Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Short- and long-term outcomes in elderly patients with locally advanced non-small-cell lung cancer treated using video-assisted thoracic surgery lobectomy
Authors Zhang L
Received 30 May 2018
Accepted for publication 26 September 2018
Published 8 November 2018 Volume 2018:14 Pages 2213—2220
DOI https://doi.org/10.2147/TCRM.S175846
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Like Zhang
Department of Thoracic Surgery, The Third Hospital of Hebei Medical University, Shijiazhuang 050051, Hebei, People’s Republic of China
Background: In recent years, video-assisted thoracic surgery (VATS) lobectomy has been used to treat locally advanced non-small-cell lung cancer (LA-NSCLC). However, VATS has not been reported in elderly patients (≥70 years) with LA-NSCLC. The purpose of this study was to compare short- and long-term outcomes of patients with LA-NSCLC aged ≥70 years and 55–69 years treated with VATS.
Patients and methods: From January 2012 to January 2018, a total of 83 patients with LA-NSCLC who were ≥55 years of age underwent VATS. Patients were divided into ≥70 years group (37 cases) and 55–69 years group (46 cases), based on their age at the time of VATS. Short- and long-term outcomes of these two groups of patients were compared.
Results: American Society of Anesthesiologists scores of ≥70 years patients were higher than those of 55–69 years patients. No significant differences were observed when comparing the general preoperative data. For short-term outcomes, there was no significant difference between the two groups of patients in length of surgery, intraoperative blood loss, conversion to thoracotomy, postoperative 30-day complication rate and severity, postoperative 30-day mortality, pathological results, compliance with adjuvant chemotherapy, or other factors. Long-term follow-up results showed that recurrence, overall survival, and disease-free survival were similar in both groups. Furthermore, multivariate analysis showed that age was not an independent predictor of overall and disease-free survival.
Conclusions: VATS in elderly patients (≥70 years) with LA-NSCLC can result in short- and long-term outcomes similar to those of 55–69 years patients with LA-NSCLC.
Keywords: lobectomy, minimally invasive surgery, locally advanced non-small-cell lung cancer, video-assisted thoracic surgery, prognosis
Introduction
Lung cancer is a common clinical malignancy.1–3 In clinical oncology, lung cancer is classified as non-small-cell lung cancer (NSCLC) and small-cell lung cancer, based on the biological characteristics and treatment methods. NSCLC accounts for approximately 85%–90% of lung cancer cases.4,5 Surgery is the mainstay treatment for patients with NSCLC.6–8 Since the first case of video-assisted thoracic surgery lobectomy (VATS) treatment for NSCLC in 1992,9 studies have shown that compared with open surgery, VATS treatment of early stage NSCLC resulted in less blood loss, faster postoperative recovery, less trauma, similar or reduced postoperative complications, and similar long-term outcomes.10–22 VATS has gradually been applied in the treatment of locally advanced NSCLC (LA-NSCLC), due to accumulation of experience and continuous improvement of surgical instruments.23–34 As life expectancy per capita increases, the occurrence of NSCLC in elderly patients has shown an increasing trend. Studies demonstrated that VATS treatment in elderly patients with early stage NSCLC can result in outcomes similar to those in nonelderly patients.35–37 However, according to our literature search, to date, there are no published reports in English on the treatment of LA-NSCLC with VATS in elderly patients. This study was aimed to investigate the clinical value of VATS for the treatment of LA-NSCLC in elderly patients, by comparing the short- and long-term outcomes of VATS in elderly and middle-aged patients with LA-NSCLC.
Patients and methods
This retrospective study complied with the tenets of the Declaration of Helsinki and was approved by the local ethics committees. The need for informed consent from all patients was waived as the study was retrospective.
From January 2012 to January 2018, a total of 106 patients with LA-NSCLC underwent VATS at our hospital. Patients who fulfilled the following inclusion criteria were enrolled in this study: 1) clinical stage of IIA–IIIA; 2) complete clinical and follow-up data available; 3) surgical approach used was VATS, including conversion to open thoracotomy; and 4) diagnosis of NSCLC. Exclusion criteria were: 1) diagnosis of SCLC; 2) patients who underwent bilobectomy or pneumonectomy; 3) patients requiring multivisceral resections due to local tumor invasion; and 4) presence of other malignant tumors. After screening, a total of 83 patients were included in the study to compare the short- and long-term outcomes (including cancer recurrence, disease-free, and overall survival) between the ≥70 years (37 cases) and 55–69 years (46 cases) groups. Preoperative chest computed tomography (CT), cardiopulmonary function testing, brain CT/magnetic resonance imaging, abdominal CT/ultrasound, bone scan, and laboratory examinations were conducted to determine clinical staging and exclude distant metastases. When mediastinal lymph node enlargement was demonstrated on chest CT, endobronchial ultrasound transbronchial needle aspiration or mediastinoscopic biopsy was performed first. Positron emission tomography/CT was not mandatory in every patient. Complete VATS without hand-assisted technique was used in this study. VATS was performed via a 4-cm utility incision at the anterior axillary line, at the fourth or fifth intercostal space, without rib spreading. A port at the eighth or seventh intercostal space, at the posterior axillary line, was used for camera visualization, and a posterior port was used for lung retraction and stapler insertion. Details of specific operations can be found in a previous literature report.29
The Clavien–Dindo criteria were used to classify the severity of postoperative 30-day complications. Minor complications were defined as Grades I–II and major complications were defined as Grades III–V.38 Postoperative 30-day mortality was defined as any death from oncological or nononcological causes within 30 days after surgery.
Patients with pathological stage greater than or equal to stage II were recommended to receive postoperative adjuvant chemotherapy, if there was no contraindication to chemotherapy.39
The permanent home address and contact information of the patients were registered at hospital discharge. Follow-up was conducted by interviews in the outpatient settings and/or through telephone interviews, home visits, or communication with family members, as well as by other means. The patients were followed up once every 3 months in the first postoperative year, once every 4 months in the second postoperative year, once every 6 months in the third postoperative year, and once a year thereafter.40 The follow-up appointments included physical examination, routine laboratory tests, and brain/chest/abdominal CT scans. Patients with suspected bone metastases underwent bone scanning.40
Patients with suspected tumor recurrence were referred to our hospital. Locoregional recurrence was defined if it occurred in 1) the bronchial stump or cut end of the lung parenchyma, 2) the ipsilateral pleura and/or chest wall, or 3) the ipsilateral hilar and/or mediastinal lymph nodes.40 Recurrence was defined as distant if it occurred in a separate lobe of the ipsilateral lung, contralateral thorax, supraclavicular lymph nodes, or in a distant organ. If distant recurrences were identified by systemic survey within a month after the detection of locoregional recurrence, these were defined as concurrent distant and locoregional recurrence.40 Overall survival was calculated from the date of radical resection to the last follow-up visit or death from any cause. Disease-free survival was assessed from the date of radical resection until the date of cancer recurrence or death from any cause.40 The latest follow-up included in this study was in March 2018.
Statistics
Categorical variables are presented as frequencies and percentages, and continuous variables are presented as median values with range. Statistical analyses were performed with the chi-squared test, Fisher’s exact test, and Mann–Whitney U test for categorical and continuous variables, respectively. Overall survival and disease-free survival rates were estimated by the Kaplan–Meier method, with differences in survival between groups compared by the log-rank test. The Cox proportional hazard model was used to identify significant predictive factors for patient survival outcomes. Results are expressed as ORs with 95% CIs. All analyses were performed using the Statistical Package for Social Sciences 13.0 for Microsoft Windows version. P<0.05 was considered to be statistically significant.
Results
Patients who were ≥70 years of age had higher American Society of Anesthesiologists scores than the 55–69 years patients (Table 1). There was no significant difference between the two groups in gender, simplified comorbidity score (SCS), tumor site, neoadjuvant chemotherapy, and tumor/node/metastasis staging (Table 1).
  | Table 1 Comparison of baseline characteristics of the two groups |
There was no significant difference between the elderly group and the middle-aged group in terms of length of surgery, intraoperative blood loss, conversion to thoracotomy, drainage time, and postoperative hospitalization time (Table 2).
  | Table 2 Comparison of surgical outcomes of the two groups |
The postoperative 30-day complications in the elderly patients were similar to those in the middle-aged group. The most common complication was prolonged air leakage. The incidence of postoperative 30-day major complications was similar in both groups. No mortality occurred intraoperatively or within 30 days postoperatively (Table 2). There were no significant differences in the pathological data between the two groups (Table 3).
  | Table 3 Comparison of pathological outcomes of the two groups |
Twenty-nine and 36 patients in the ≥70 years and 55–69 years groups, respectively, received at least one cycle of adjuvant chemotherapy. There was no significant difference in compliance with adjuvant chemotherapy between the two groups (Table 4).
  | Table 4 Comparison of chemotherapy compliance of the two groups |
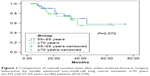
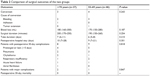
The median follow-up periods for the ≥70 years and 55–69 years groups were 35 and 38 months, respectively, and no significant difference was observed. During the follow-up period, 9 and 11 patients died in the ≥70 years and 55–69 years groups, respectively. Among the nine deaths in the ≥70 years group, eight were due to cancer recurrence, and one was due to stroke; among the eleven deaths in the 55–69 years group, ten were due to cancer recurrence and one was due to noncancer factors (Table 5). The 5-year overall survival rate in the ≥70 years and 55–69 years groups was 54% and 59%, respectively; this difference was not statistically significant (Figure 1, P=0.570). Multivariate analysis showed that the T stage, N stage, and SCS were independent predictors of overall patient survival (Table 6).
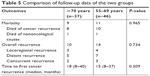  | Table 5 Comparison of follow-up data of the two groups |
  | Table 6 Univariate and multivariate analyses for predictive factors of overall survival |
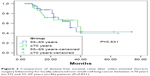
During the follow-up period, cancer recurrence was observed in 29 patients and 32 patients in the ≥70 years and 55–69 years groups, respectively. There was no significant difference between the two groups in terms of cancer recurrence rate and recurrence site. The 5-year disease-free survival rate in the ≥70 years and 55–69 years groups was 41% and 43%, respectively; this difference was not significant (Figure 2, 0.831). Multivariate analysis showed that T stage, N stage, and SCS were independent predictors of disease-free survival rate (Table 7).
  | Table 7 Univariate and multivariate analyses for predictive factors of disease-free survival |
Discussion
Compared with that of early stage NSCLC, treatment of LA-NSCLC with VATS is more difficult. The first case of VATS treatment for LA-NSCLC was reported by Petersen et al of Duke University Medical Center (USA) in 2006.34 In their study,34 Petersen et al performed VATS treatment on 12 patients with LA-NSCLC, and 1 patient was converted to thoracotomy. Compared with thoracotomy, VATS has the advantages of shorter drainage time and shorter hospitalization time. There was no significant difference in postoperative complications, postoperative mortality, and prognosis, indicating that VATS can result in outcomes similar to those of open surgery when treating LA-NSCLC.34 Subsequently, numerous studies have reported similar conclusions.23–34 In the present study, the short- and long-term outcomes of elderly patients were similar to previous reports, indicating that VATS is safe and feasible for the treatment of LA-NSCLC.
Potential treatment methods for LA-NSCLC in elderly patients include radiotherapy, radiofrequency ablation, and surgery.41 Studies have shown that the survival rate of elderly patients with LA-NSCLC who underwent surgical treatment is better than that of patients who underwent nonsurgical treatment.42 The clinical guidelines issued by the European Society for Medical Oncology also recommend surgical treatment to improve survival rate in elderly patients with LA-NSCLC with indications for surgery.43 Based on our search in available databases such as PubMed, Embase, and Chemical Abstracts, to the best of our knowledge, VATS has not been reported in the English language for the treatment of LA-NSCLC in elderly patients. This study was the first to demonstrate that elderly patients with LA-NSCLC treated by VATS can show similar long-term outcomes compared to middle-aged patients.
Elderly patients with NSCLC often present with comorbidities. Comorbidity refers to diseases that exist at the time of diagnosis of NSCLC, such as respiratory diseases and cardiovascular diseases. The impact of comorbidities on elderly patients with cancer has received increasing attention. Studies have shown that the presence of comorbidities, rather than cancer itself, is the main reason for the lower survival rate in elderly patients with NSCLC compared with nonelderly patients, making it difficult for elderly patients to tolerate surgery, radiotherapy, and chemotherapy.44 The Charlson Comorbidity Index (CCI), designed by Charlson et al in 1987, includes 19 common comorbidities, and is the most commonly used method to evaluate cancer complications in Western countries.45 It has been applied in clinical studies evaluating head and neck tumors, urinary tract cancer, and breast cancer. Most studies have shown that a higher CCI score is associated with a poorer prognosis.45–47 However, when CCI is applied in NSCLC, studies have shown that it cannot be used to assess patient prognosis.48,49 The reason for this is that CCI was derived from the study of comorbidities in patients with breast cancer. The comorbidities that affect breast cancer prognosis are very different from those of NSCLC, even though 19 common comorbidities are involved. Some comorbidities that may affect the prognosis of lung cancer, such as smoking, were not included in the score. The SCS was derived from the study of the prognostic impact of comorbidities on NSCLC, and it classified comorbidities into seven categories.50 In the SCS score, smoking accounts for a high proportion (7 points). Smoking is the leading cause of the increased incidence and mortality rate of lung cancer. A study by Tomohiro Haruki et al showed that patients with high SCS scores had poorer VATS outcomes than those with low SCS scores.51 In the present study, SCS was identified as an independent predictor of patient survival.
Clinical trials have shown that adjuvant chemotherapy can reduce the recurrence rate and improve the survival rate of patients with NSCLC.41 Clinical guidelines recommend adjuvant chemotherapy for patients with stage II and III NSCLC.41 Adjuvant chemotherapy plays a very important role in the prognosis of patients with NSCLC.41 Studies have shown that the earlier the initiation of adjuvant chemotherapy, the higher will be the tolerability and the better will be the prognosis of the patients.39–41 To our knowledge, there is no report on the effects of VATS treatment on postoperative adjuvant chemotherapy in elderly patients with NSCLC. Our study showed for the first time that elderly patients can achieve early initiation time and tolerability for postoperative adjuvant chemotherapy compared with middle-aged patients. In this study, the survival rate of elderly and middle-aged patients was similar, which may be due to improved tolerability of the procedure among elderly patients.
Conversion thoracotomy is inevitable in VATS. It has been reported that the thoracotomy conversion rate was 0%–23% when VATS was used to treat LA-NSCLC, depending on case selection and surgeon experience.23–34 In our study, we found a conversion rate of 7% and 6% in elderly and middle-aged patients, respectively, which is similar to that reported in previous studies.23–34 The vast majority of conversion thoracotomy cases in this study were due to uncontrolled bleeding, followed by tissue adhesion. To date, there is no report in the English language on the VATS conversion rate in elderly patients with LA-NSCLC. Our study showed for the first time that when VATS is used in the treatment of elderly patients with LA-NSCLC, the conversion rate is similar to that of middle-aged patients.
In this study, the long-term outcomes including cancer recurrence, overall survival, and disease-free survival were similar between groups. Previous reports on VATS treatment of patients with LA-NSCLC reported a cancer recurrence rate of 10%–30%, a 5-year overall survival rate of 50%–60%, and a 5-year disease-free survival rate of 30%–50%.23–34 The results of this study are similar to previous findings. To our knowledge, no study has reported the 5-year overall survival and 5-year disease-free survival rates in elderly patients with LA-NSCLC treated with VATS. This study demonstrates, for the first time, that elderly patients with LA-NSCLC treated with VATS can achieve similar long-term outcomes as those of nonelderly patients.
Concurrent chemoradiotherapy is a common therapeutic method for NSCLC patients with no surgical indications. However, there is debate on whether concurrent chemoradiotherapy is suitable for elderly patients. The study by Semrau et al found that elderly patients with NSCLC can tolerate concurrent chemoradiotherapy.52,53
In recent years, no notable progress has been made with respect to LA-NSCLC treatment, so new treatment strategies are urgently needed. In 2017, a randomized controlled clinical trial published in The New England Journal of Medicine showed durvalumab can reverse PD-1-mediated inhibitory signals, enhance the function of effector T-cells, and restore the cytotoxic effects of T-cells against cancer cells. Efficacy was demonstrated by the extension of progression-free survival.54
The present study has two important limitations. First, the retrospective design is associated with known risks of bias, and a prospective randomized controlled trial is needed to confirm that VATS is safe and effective for elderly patients with LA-NSCLC. Second, we examined data from a single center only, and it is possible that our findings may not generalize to other centers and/or patient groups.
In conclusion, our study suggests that VATS does not increase the incidence of postoperative complications in elderly patients with LA-NSCLC and that these patients may achieve long-term outcomes similar to 55–69 years patients. Thus, age is not a contraindication for elderly patients with LA-NSCLC to undergo VATS treatment.
Acknowledgments
The author sincerely thanks his colleagues who participated in this research.
Disclosure
The author reports no conflicts of interest in this work.
References
Naylor EC, Desani JK, Chung PK. Targeted therapy and immunotherapy for lung cancer. Surg Oncol Clin N Am. 2016;25(3):601–609. | ||
Bauer TL, Berkheim DB. Bronchoscopy: diagnostic and therapeutic for non-small cell lung cancer. Surg Oncol Clin N Am. 2016;25(3):481–491. | ||
Gamliel Z. Mediastinal staging in non-small cell lung cancer. Surg Oncol Clin N Am. 2016;25(3):493–502. | ||
Gadgeel SM, Ramalingam SS, Kalemkerian GP. Treatment of lung cancer. Radiol Clin North Am. 2012;50(5):961–974. | ||
Ginsberg MS, Grewal RK, Heelan RT. Lung cancer. Radiol Clin North Am. 2007;45(1):21–43. | ||
Harris C, Meek D, Gilligan D, Williams L, Solli P, Rintoul RC. Assessment and optimisation of lung cancer patients for treatment with curative intent. Clin Oncol. 2016;28(11):682–694. | ||
Rodriguez-Canales J, Parra-Cuentas E, Wistuba II. Diagnosis and molecular classification of lung cancer. Cancer Treat Res. 2016;170:25–46. | ||
Takahashi Y. Real-time intraoperative diagnosis of lung adenocarcinoma high risk histological features: a necessity for minimally invasive sublobar resection. Minim Invasive Surg Oncol. 2017;1(1):12–19. | ||
Roviaro G, Rebuffat C, Varoli F, Vergani C, Mariani C, Maciocco M. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc. 1992;2(3):244–247. | ||
Kirby TJ, Mack MJ, Landreneau RJ, Rice TW. Initial experience with video-assisted thoracoscopic lobectomy. Ann Thorac Surg. 1993;56(6):1248–1253. | ||
Kirby TJ, Mack MJ, Landreneau RJ, Rice TW. Lobectomy – video-assisted thoracic surgery versus muscle-sparing thoracotomy. A randomized trial. J Thorac Cardiovasc Surg. 1995;109(5):997–1002. | ||
Fang W, Ruan W. Advances in uniportal video-assisted thoracoscopic surgery for non-small cell lung cancer. Minim Invasive Surg Oncol. 2017;1(1):20–30. | ||
Abu Arab W. Video-assisted thoracoscopic surgery for non-small cell lung cancer. Minim Invasive Surg Oncol. 2017;1(1):1–11. | ||
Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol. 2016;17(6):836–844. | ||
Long H, Tan Q, Luo Q, et al. Thoracoscopic surgery versus thoracotomy for lung cancer: short-term outcomes of a randomized trial. Ann Thorac Surg. 2018;105(2):386–392. | ||
Scott WJ, Allen MS, Darling G, et al. Video-assisted thoracic surgery versus open lobectomy for lung cancer: a secondary analysis of data from the American College of Surgeons Oncology Group Z0030 randomized clinical trial. J Thorac Cardiovasc Surg. 2010;139(4):976–983. | ||
Liu Z, Yang R, Shao F. Anastomosis using complete continuous suture in uniportal video-assisted thoracoscopic bronchial sleeve lobectomy. Minim Invasive Surg Oncol. 2017;1(1):31–42. | ||
Jing X, Lin Y, Zhang B, Zhang G. Video-assisted thoracoscopic lobectomy mitigates adverse oncological effects of delayed adjuvant chemotherapy for nonsmall cell lung cancer patients. J BUON. 2016;21(6):1524–1529. | ||
Yuan J, Dai G, Kong F. Long-term outcomes of video-assisted thoracoscopic versus open lobectomy for non-small-cell lung cancer with propensity score matching. Int J Clin Exp Med. 2016;9(2):3572–3578. | ||
Yu J, Yang R, Wang J, Shao F. Equivalency of oncological outcomes during lobectomy by video-assisted thoracoscopic surgery versus thoracotomy. Int J Clin Exp Med. 2016;9(2):3505–3512. | ||
Xu J, Xiaoqiang, Tian J, Yan J. Video-assisted thoracoscopic lobectomy versus open lobectomy for clinical stage I non small cell lung cancer: a case-control study. Int J Clin Exp Med. 2016;9(2):3537–3543. | ||
Zhao H, Liu G, Wei S, Liu H. Short- and long-term outcomes of minimally invasive esophagectomy in elderly patients with esophageal squamous cell carcinoma. J BUON. 2017;22(6):1540–1546. | ||
Gonfiotti A, Bongiolatti S, Bertolaccini L, et al. Thoracoscopic lobectomy for locally advanced-stage non-small cell lung cancer is a feasible and safe approach: analysis from multi-institutional national database. J Vis Surg. 2017;3:160. | ||
Sanchez-Lorente D, Guzman R, Boada M, Carriel N, Guirao A, Molins L. Is it appropriate to perform video-assisted thoracoscopic surgery for advanced lung cancer? Future Oncol. 2018;14(6s):29–31. | ||
Mollberg NM, Mulligan MS. Video-assisted thoracoscopic (VATS) lobectomy after induction therapy. Thorac Surg Clin. 2014;24(4):465–470. | ||
Huang J, Xu X, Chen H, et al. Feasibility of complete video-assisted thoracoscopic surgery following neoadjuvant therapy for locally advanced non-small cell lung cancer. J Thorac Dis. 2013;5(Suppl 3):S267–S273. | ||
Gonzalez-Rivas D, Fieira E, Delgado M, Mendez L, Fernandez R, de La Torre M. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis. 2014;6(6):641–648. | ||
Park BJ, Yang HX, Woo KM, Sima CS. Minimally invasive (robotic assisted thoracic surgery and video-assisted thoracic surgery) lobectomy for the treatment of locally advanced non-small cell lung cancer. J Thorac Dis. 2016;8(Suppl 4):S406–S413. | ||
Chen K, Wang X, Yang F, et al. Propensity-matched comparison of video-assisted thoracoscopic with thoracotomy lobectomy for locally advanced non-small cell lung cancer. J Thorac Cardiovasc Surg. 2017;153(4):967–976. | ||
Fan J, Yao J, Wang Q, Chang Z. Safety and feasibility of uniportal video-assisted thoracoscopic surgery for locally advanced non-small cell lung cancer. J Thorac Dis. 2016;8(12):3543–3550. | ||
Shao W, Liu J, Liang W, et al. Safety and feasibility of video-assisted thoracoscopic surgery for stage IIIA lung cancer. Chin J Cancer Res. 2014;26(4):418–422. | ||
Hennon M, Sahai RK, Yendamuri S, Tan W, Demmy TL, Nwogu C. Safety of thoracoscopic lobectomy in locally advanced lung cancer. Ann Surg Oncol. 2011;18(13):3732–3736. | ||
Nakanishi R, Fujino Y, Yamashita T, Shinohara S, Oyama T. Thoracoscopic anatomic pulmonary resection for locally advanced non-small cell lung cancer. Ann Thorac Surg. 2014;97(3):980–985. | ||
Petersen RP, Pham D, Toloza EM, et al. Thoracoscopic lobectomy: a safe and effective strategy for patients receiving induction therapy for non-small cell lung cancer. Ann Thorac Surg. 2006;82(1):214–219. | ||
Deng Z, Cai Y, Huang J. Short- and long-term outcomes of patients aged ≥70 years undergoing video-assisted thoracoscopic surgery for non-small cell lung cancer. Int J Clin Exp Med. 2017;10(6):9432–9439. | ||
Wang Y, Chen C. Survival following video-assisted thoracoscopic versus open esophagectomy for esophageal carcinoma. J BUON. 2016;21(2):427–433. | ||
Liu K, Zhao J, Zhang W, Tan J, Ma J, Pei Y. Video-assisted thoracoscopic surgery for non-small-cell lung cancer in elderly patients: a single-center, case-matched study. Int J Clin Exp Med. 2015;8(7):11738–11745. | ||
Grigor EJM, Ivanovic J, Anstee C, et al. Impact of adverse events and length of stay on patient experience after lung cancer resection. Ann Thorac Surg. 2017;104(2):382–388. | ||
Naylor EC. Adjuvant therapy for Stage I and II non-small cell lung cancer. Surg Oncol Clin N Am. 2016;25(3):585–599. | ||
Vansteenkiste J, de Ruysscher D, Eberhardt WE, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(Suppl 6):vi89–vi98. | ||
Reck M, Rabe KF. Precision diagnosis and treatment for advanced non-small-cell lung cancer. N Engl J Med. 2017;377(9):849–861. | ||
Speicher PJ, Englum BR, Ganapathi AM, Onaitis MW, D’Amico TA, Berry MF. Outcomes after treatment of 17,378 patients with locally advanced (T3N0-2) non-small-cell lung cancer. Eur J Cardiothorac Surg. 2015;47(4):636–641. | ||
Eberhardt WE, de Ruysscher D, Weder W, et al. 2nd ESMO Consensus Conference in Lung Cancer: locally advanced stage III non-small-cell lung cancer. Ann Oncol. 2015;26(8):1573–1588. | ||
Ahn DH, Mehta N, Yorio JT, Xie Y, Yan J, Gerber DE. Influence of medical comorbidities on the presentation and outcomes of stage I–III non-small-cell lung cancer. Clin Lung Cancer. 2013;14(6):644–650. | ||
Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE. Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc. 2014;62(2):342–346. | ||
Chan TC, Luk JK, Chu LW, Chan FH. Validation study of Charlson Comorbidity Index in predicting mortality in Chinese older adults. Geriatr Gerontol Int. 2014;14(2):452–457. | ||
Grose D, Morrison DS, Devereux G, et al. The impact of comorbidity upon determinants of outcome in patients with lung cancer. Lung Cancer. 2015;87(2):186–192. | ||
Singh N, Singh PS, Aggarwal AN, Behera D. Comorbidity assessment using Charlson Comorbidity Index and simplified comorbidity score and its association with clinical outcomes during first-line chemotherapy for lung cancer. Clin Lung Cancer. 2016;17(3):205–213. | ||
Gironés R, Torregrosa D, Gómez-Codina J, Maestu I, Tenias JM, Rosell R. Prognostic impact of comorbidity in elderly lung cancer patients: use and comparison of two scores. Lung Cancer. 2011;72(1):108–113. | ||
Wang S, Wong ML, Hamilton N, Davoren JB, Jahan TM, Walter LC. Impact of age and comorbidity on non-small-cell lung cancer treatment in older veterans. J Clin Oncol. 2012;30(13):1447–1455. | ||
Haruki T, Yurugi Y, Wakahara M, et al. Simplified comorbidity score for elderly patients undergoing thoracoscopic surgery for lung cancer. Surg Today. 2017;47(6):718–725. | ||
Semrau S, Zettl H, Hildebrandt G, Klautke G, Fietkau R. Older patients with inoperable non-small cell lung cancer: long-term survival after concurrent chemoradiotherapy. Strahlenther Onkol. 2014;190(12):1125–1132. | ||
Elsayad K, Samhouri L, Scobioala S, Haverkamp U, Eich HT. Is tumor volume reduction during radiotherapy prognostic relevant in patients with stage III non-small cell lung cancer? J Cancer Res Clin Oncol. 2018;144(6):1165–1171. | ||
Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377(20):1919–1929. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.