Back to Journals » Substance Abuse and Rehabilitation » Volume 13
Services Available at United States Addiction Treatment Facilities That Offer Medications versus Behavioral Treatment Only: A Cross-Sectional, Observational Analysis
Authors Weber A , Miskle B, Lynch A, Arndt S, Acion L
Received 17 January 2022
Accepted for publication 19 August 2022
Published 7 September 2022 Volume 2022:13 Pages 57—64
DOI https://doi.org/10.2147/SAR.S356131
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Justinn Cochran
Andrea Weber,1 Benjamin Miskle,1 Alison Lynch,1 Stephan Arndt,1,2 Laura Acion3
1Department of Psychiatry, University of Iowa Health Care, Iowa City, IA, USA; 2Department of Biostatistics, University of Iowa, Iowa City, IA, USA; 3Universidad de Buenos Aires – CONICET, Instituto de Cálculo, Ciudad Autónoma de Buenos Aires, Argentina
Correspondence: Andrea Weber, Department of Psychiatry, University of Iowa Health Care, 500 Newton Road, Iowa City, IA, 52242, USA, Tel +1 319 384 8014, Fax +1 319 384 7467, Email [email protected]
Purpose: Substance use disorders (SUDs) are widespread and cause significant morbidity and mortality, yet most people in the United States with a SUD do not receive treatment. Recommendations call for widespread use of pharmacotherapy, including medications for opioid use disorder (MOUD). However, many facilities do not offer a full array of medication treatments. This study aims to characterize programs that do and do not offer pharmacotherapy as part of addiction treatment services. We hypothesized that the availability of pharmacotherapy would predict the existence of other recommended components of treatment.
Patients and Methods: We analyzed characteristics regarding treatment facilities (n = 15,782) recorded by the 2019 National Survey of Substance Abuse Treatment Services (N-SSATS) to determine how many SUD treatment facilities offer any pharmacotherapy. We compared facilities that offer any pharmacotherapy to facilities that offer none.
Results: We found that 65% of SUD treatment facilities that responded to the N-SSATS survey provided at least one pharmacotherapy, while 35% of SUD treatment facilities did not. The facilities that provided at least one pharmacotherapy offered, on average, 6 additional treatment options (Cohen’s d = 0.87; 95% CI: 0.84– 0.91). Psychiatric medications were the most commonly available pharmacotherapy, followed by buprenorphine/naloxone and naltrexone.
Conclusion: These results support that pharmacotherapy availability, such as MOUD, at SUD treatment facilities is associated with an increased number of recommended treatment components. Since MOUD has been shown elsewhere to reduce mortality for people with OUD, it should be universally available at SUD treatment facilities. Further efforts are needed to make pharmacotherapy more widely available.
Keywords: substance use treatment, buprenorphine, naltrexone, pharmacotherapy
Introduction
Substance use disorders (SUDs) are prevalent, costly, and treatable. According to the National Survey on Drug Use and Health (NSDUH), 20.4 million people age 12 and older in the United States (US) had a SUD, a number that has held steady for the past 4 years. 1 The number of lives lost due to overdose deaths continues to rise as the US continues to experience an epidemic of overdose deaths. After overdose deaths fell slightly in 2018, the number of deaths increased in 2019. 2 September 2020 marked the end of a 12-month period that saw the highest number of deaths due to drug overdose, most of which involved an opioid. 2
Several treatments are available to treat SUDs, including medications and behavioral interventions. Behavioral interventions including contingency management, cognitive behavior therapy, and motivational enhancement have been shown to reduce drug use.3,4 Also, the US Food and Drug Administration (FDA) has approved medications for the treatment of three SUDs: acamprosate, disulfiram, and naltrexone to treat alcohol use disorder (AUD); bupropion, nicotine replacement, and varenicline to treat tobacco use disorder (TUD); and buprenorphine, methadone, and naltrexone to treat opioid use disorder (OUD).
Medications for OUD (MOUD) improve outcomes by reducing drug use,5 associated infections,6 arrests,7 and death.8 The importance of long-term treatment was highlighted in a study of over 48,000 adults in Maryland, US, who received outpatient specialty treatment for OUD.9 The authors found that while MOUD reduced the risk of overdose death, this protective effect only lasts for the duration of treatment, and risk of overdose death increases after treatment end.
Several leading agencies have published guidelines about what constitutes high-quality treatment for SUD. The Substance Abuse and Mental Health Services Agency (SAMHSA) recommends that people seeking high-quality addiction treatment look for programs that are accredited, offer medication and evidence-based practices, incorporate family involvement, and provide ongoing recovery supports.10 The National Institute on Alcohol Abuse and Alcoholism (NIAAA) advises that people seeking treatment for AUD look for programs that are credentialed and offer a full assessment, a personalized treatment plan, provide science-based therapies, and offer continuing recovery support.11 Finally, the National Institute on Drug Abuse (NIDA) has published a list of principles of effective treatment. This list includes individualized and accessible treatment of long enough duration to achieve and maintain a stable recovery; components of behavioral therapy and pharmacotherapy; addressing of any associated medical, psychiatric, psychological, social, vocational and legal needs of the individual. However, recommendations are insufficient if programs do not offer these characteristics, or if it is too difficult to discern which programs meet these criteria.
Even though SAMHSA and NIDA specifically recommend choosing a treatment program that offers medications for OUD and AUD, many treatment programs do not provide this option. A report by Mark et al looked at trends in availability of high-quality SUD treatment components in the US between 2007 and 2017 and found that most of the recommended treatment components increased in availability from 2007 to 2017.12 Nevertheless, at the end of the study period, more than half of facilities still did not offer MOUD; mental health assessments; testing for hepatitis C, HIV, and sexually transmitted infections; self-help groups; employment assistance; and transportation assistance. In 2017, only 35.5% of SUD treatment programs offered at least one medication to treat OUD, and even fewer (16.3%) offered at least one medication to treat AUD.13 Furthermore, geographic variation in programming suggests that treatment options are heavily influenced by where the person lives rather than individual treatment preference. For example, in 2017, 10% of SUD treatment facilities in Hawaii provided MOUD, while 81% of SUD treatment facilities in Rhode Island provided MOUD.12 The percentage of SUD treatment facilities that were accredited in 2017 varied from state to state, ranging from 15% in Colorado and North Dakota to 89% in Wyoming and Alaska. Nationally, about half of all SUD treatment programs performed comprehensive mental health assessments in 2017, ranging from 20% of facilities (in Hawaii) to 74% of facilities (in Alaska).12
With much variation between treatment facilities, finding a program that is compatible with one’s treatment goals can be daunting. Several organizations, including the American Society of Addiction Medicine (ASAM), SAMHSA, and NIAAA operate web-based treatment locators to assist individuals in locating treatment programs. NIAAA’s treatment locator provides recommendations for identifying high-quality treatment programs, while SAMHSA’s treatment locator lists treatment programs that provide medications for OUD and AUD, serve specific age ranges, and provide services in different languages. ASAM’s certification program, in partnership with the Commission of Accreditation of Rehabilitation Facilities (CARF) certifies SUD treatment programs that have demonstrated the capacity to provide certain levels of care according to the ASAM Criteria. Not surprisingly, individuals seeking high-quality treatment for SUD can be overwhelmed with options yet lack clear criteria for selecting a treatment program.
In addition to receiving certification or licensure by national and state agencies, receiving government grants may be another differentiating factor between treatment facilities. It seems logical that only those facilities providing a wide array of evidence-based services would receive federal grant awards, but it is unclear if providing MOUD or other high-quality services make a treatment facility more or less likely to receive grant support.
Despite the prevalence, costs, and treatability of SUDs, many people with a SUD still do not get adequate treatment.1 Finding adequate treatment can be an overwhelming endeavor and depends on patient knowledge and attitudes, stigma, geographic availability, insurance coverage, and program capacity, among other criteria. Given that pharmacotherapy (including medications for OUD and AUD) is a recommended component of high-quality SUD treatment, carefully characterizing programs that offer any pharmacotherapy may provide information for assessing facility’s treatment quality, improve certifications, grant allocation, and, eventually, ease treatment choice. In this study, we assess the differences between SUD treatment programs that offer pharmacotherapy services versus those that do not. Although we acknowledge the importance of access to MOUD given the current overdose epidemic, we chose to look at the broader category of pharmacotherapy because we are interested in the breadth of medical management of all SUDs and co-morbid conditions, not just SUDs that have a medication therapy such as MOUD. We hypothesize that the availability of any pharmacotherapy correlates with the presence of other high-quality treatment components (such as individualized treatment plans, MOUD, medication for co-occurring conditions, and recovery supports after program completion) at the treatment facility.
Materials and Methods
SAMHSA conducts an annual national survey of all known public and private treatment facilities. The National Survey of Substance Abuse Treatment Services (N-SSATS) includes all known facilities from states, the District of Columbia, and other jurisdictions. The people responding to the survey usually are administrators or other well-informed facility staff.14 The N-SSATS is a publicly available dataset of facilities and does not include any human subjects. The 2019 wave provided data for the current study.15 The full data file has information on 15,961 facilities. Selecting only facilities that offer treatment for SUD and removing blank entries resulted in 15,782 records.
The primary variable of interest was whether the facility offered any pharmacotherapy treatment options, which for this study was coded as medication (MED). Pharmacotherapies included nicotine replacement, non-nicotine smoking/tobacco cessation medications (eg, varenicline), medications for psychiatric disorders, methadone, buprenorphine (with or without naloxone, sub-dermal implant, or extended-release injections), HIV medications, hepatitis-C medications, lofexidine, clonidine, acamprosate, naltrexone (oral or extended-release injections), or disulfiram. A facility was code as Any MED if it offered at least one pharmacotherapy and No MED if it provided none.
The survey queries facilities on the number of various available services, assessment, testing, medical, transitional, recovery support, education and counseling, ancillary, and other. Ancillary services include case management, childcare, mental health services, domestic violence, etc. Other services included treatment for gambling disorder, internet use disorder or other non-substance use disorders. Other facility characteristics, such as ownership, licensure, accreditation, and if government/public money was accepted to support SUD treatment were investigated.
Statistical Analyses
Simple frequencies, percentages, means, and standard deviations are presented for descriptive statistics. Chi-square and Mann–Whitney tests compared the Any MED and No MED groups. Confidence intervals accompany simple differences in proportions or means. Cohen’s d reflects the effect sizes for mean differences. Due to the large sample size that will result in non-clinically meaningful effects, we will only attend to moderate- or large-sized effects.
In support of using all listed medications, Cronbach’s alpha including all 16 medicines for these data was 0.90. This indicates a high degree of internal consistency, although we used this as a binary variable rather than a sum in our analyses. All analyses were done with R.16
Results
Slightly over one-third of the facilities offered No MED (35%; 5517), while nearly two-thirds provided at least one pharmacotherapy (65%; 10,265). Among the facilities that provided at least one, the mean number of medication services was 5.34 (SD = 3.8), and over 81.1% offered more than one (data not shown). The percentages of each medication appear in Table 1.
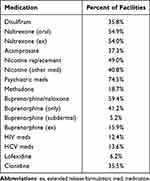 |
Table 1 Medication (MED) Services Among Facilities Offering Pharmacotherapy |
While psychiatric medications were the most frequent MED offered, MOUD were the second most popular, followed by TUD treatments. Over a third of the Any MED facilities offered pharmacotherapies for AUD. Fewer facilities had medication services for HIV or hepatitis-C.
Table 2 shows the number of services beyond pharmacotherapy offered comparing facilities that offered Any MED versus No MED. Ancillary services include case management, childcare, mental health or domestic violence services, etc. Other services included treatment for gambling disorder, internet use disorder or other non-substance use disorders.
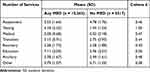 |
Table 2 Number of Services for Any MED and No MED Facilities |
There are medium to large effect sizes for most categories of service. The total number of services offered by the No MED group was 21 compared to 27, a difference of 6 services. This is a clinically and statistically significant difference (Mann–Whitney U = 41535216, p < 0.0001) and is associated with a large Cohen’s d of (0.87; 95% CI: 0.84–0.91). The separation of the facilities’ total number of services is clear in Figure 1.
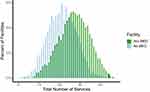 |
Figure 1 Total number of services offered by the No MED and Any MED facilities. |
Several specific services were highly distinctive contrasting the No MED and Any MED facilities. The top ten distinguishing services are shown in Table 3. While many of the services are “medical”, not all are.
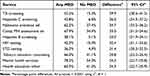 |
Table 3 Top Ten Distinguishing Individual Services |
There were several other distinguishing features that separated the facilities with and without MED. For example, the type of ownership differed between the two groups (χ2 = 132.21, df = 5, p < 0.0001). There were slightly more private for-profit facilities (42.0%) among the No MED group than the Any MED group (38.6%), but the differences were not large. The No MED facilities did offer outpatient treatment services more often than the Any MED facilities (84.1% and 81.8%; χ2 = 14.10, df = 1, p < 0.0002).
Larger differences became apparent in questions about licensing, certification, and accreditation. Only 31.0% of the No MED facilities were licensed, certified, or accredited specifically to provide SUD treatment services. In contrast, approximately two-thirds of the Any MED facilities were (66.5%; χ2 = 1816.77, df = 1, p < 0.0001). Similarly, 18.9% of the No MED facilities reported an accreditation from the CARF, while 35.4% of the Any MED were accredited by that organization (χ2 = 470.02, df = 1, p < 0.0001).
The Any MED group also tended to accept more sources of payment than the No MED facilities. Any MED programs were more likely to accept private insurance, Medicare, federal military insurance, Medicaid, state financed insurance, and cash payments (all p-values <0.0001, eg, accepts private insurance MED = 81.8%; No MED = 57.6%). Interestingly, No MED and Any MED facilities were only slightly different in their acceptance of federal or other government grants. The percentage of No MED and Any MED facilities accepting grants was 50.4% and 52.5%, respectively (χ2 = 6.29, df = 1, p < 0.0122).
Discussion
This study shows that SUD treatment facilities providing any pharmacotherapy were more likely to offer additional treatments and services compared to programs that provided no pharmacotherapy options. Almost two-thirds of treatment programs surveyed offered any pharmacotherapy, and among them the mean number of pharmacotherapies offered was about 5 out of 16 possible. Facilities offering any pharmacotherapy were more likely to also offer testing, medical evaluation and treatment, transition services, recovery supports, educational programming, and ancillary and other services, when compared to facilities that offered no pharmacotherapy. When added together, facilities that provided any pharmacotherapy offered, on average, six additional services compared to facilities that provided no pharmacotherapy. These findings support our hypothesis that the availability of any pharmacotherapy at a SUD treatment facility does predict the presence of other treatment components, which may increase the quality of the facility.
This study found clinically significant differences in more than just pharmacotherapy offerings between the facilities that offered any pharmacotherapy (“Any MED”) and those that offered no pharmacotherapy (“No MED”). Compared to No MED programs, Any MED programs were significantly more likely to offer testing for tuberculosis, hepatitis, HIV, and sexually transmitted infections with large effect sizes. Any MED facilities offered education more often than No MED facilities did, with a moderate effect size. Surprisingly, education on naloxone, a medication to reverse the effects of an opioid overdose, was offered at 62.2% of the Any MED group, compared to 27.4% of the No MED group. In 2018, the US Surgeon General released the Advisory on Naloxone and Opioid Overdose underscoring the need for increased access to naloxone.17 While more of the Any MED group facilities offered naloxone education, education on naloxone should be universally provided at all SUD treatment facilities. Assessment, medical, transition, recovery, and ancillary services were also more common in the Any MED group.
Licensing, certifications, and accreditations also differentiated both types of facilities. Any MED facilities were licensed, certified, or accredited 66.5% of the time, whereas only 31% of the No MED facilities were licensed. Facilities that offered Any MED (35.4%) were more likely to be accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF) than facilities that offered No MED (18.9%). Licensing, certification, and accreditation should be an indicator of quality or, at least, a minimum standard of care. In SUD treatment, these markers may not be held to as high a standard as in other areas. A recent study published by Beetham et al used callers posing as uninsured patients to gather information about the recruitment practices of residential SUD treatment programs.18 They found a high prevalence of concerning practices that appear to prey upon a vulnerable population at a vulnerable time in order to make a profit.
Sources of payment was another area that separated among the study groups: the Any MED group was more likely to accept additional sources of payment at their treatment facilities. Unexpectedly, however, there was no difference between the two groups in terms of grants received. Grants were received by 52.5% of the Any MED facilities, whereas 50.4% of the No MED group reported receiving grants. This trend suggests that programs offering recommended and evidence-based therapies are just as likely to receive government funds as programs that do not offer recommended or evidence-based therapies and raises the question of whether tax dollars should be spent supporting treatment programs that do not provide recommended forms of treatment.
Patient choice in treatment is crucial. While the primary focus of SUD treatment is to reduce the use of a particular substance, patient choice allows patients to have a say in their treatment plan and recovery goals. Providing treatment options allows patients to have more choice and thus more input into their treatment. This study found that programs offering Any MED provide significantly more treatment options than No MED programs.
There are some limitations with this study. As a cross-sectional study, the results are associations, but do not confer causality. While there is no evidence that offering more services in SUD treatment facilities yields better outcomes or should be considered of higher quality, it is plausible that more medical evaluation and treatment would improve overall care. Nevertheless, a limitation of this study is that actual patient outcomes were not measured. Programs that offer more services, such as testing and education, may be more likely to treat or refer patients for other comorbid disease states. By providing more education, these programs may also be able to advise patients on how to improve their overall health, and potentially decrease opioid overdose deaths, by providing more education about naloxone and other harm reduction tools. The possible benefits of more medically oriented treatment programming warrant further study.
The study is also limited because no rationale is given regarding the facilities that do not offer pharmacotherapy. For example, are No MED treatment programs simply unable to find a prescriber? Are the treatment programs insufficiently funded to offer these services? Are there philosophical reasons for not providing MED, such as a prioritizing abstinence-based recovery without medication utilization? Further research is needed to identify barriers to implementing high-quality treatments, such as MED, into specialized SUD treatment programs.
Additional limitations for this study relate to the use of the N-SSATS survey. First, this survey is administered to specialty SUD treatment programs and thus does not reflect the entire spectrum of care provided to people seeking treatment for addiction, such as those who are treated in a community mental health center or in primary care. Second, this survey is subject to recall bias and reflects what treatment programs report to offer, not what patients actually receive.
In spring 2021, the Department of Health and Human Services (HHS) issued an intention to eliminate the certified training requirement and waiver so eligible prescribers with an active DEA-license could prescribe buprenorphine for OUD in an office-based setting for up to 30 patients. Criticisms of the waiver requirement remain plentiful, including formal position statements from numerous national societies who argue that requiring such additional training is not consistent with the safety profile of buprenorphine, its Schedule III classification, and the strong evidence that buprenorphine reduces mortality in OUD.8 These criticisms have continued to grow as overdose deaths have risen significantly during the coronavirus pandemic, according to Centers for Disease Control and Prevention (CDC) data.2 It is possible that elimination of buprenorphine prescription barriers for all available prescribers (not just physicians) may further enhance the availability of buprenorphine treatment in the treatment facilities included in this study. This is especially true for rural Americans, approximately 1/3 of whom live in counties lacking any buprenorphine provider.19 Furthermore, by completely removing the buprenorphine waiver for all practitioners, it is estimated that the number of available prescribers would increase by a factor of 20. As a result, SUD treatment programs could more easily find MOUD prescribers to hire, buprenorphine could more readily be initiated while in a treatment program, and participants could be easily transitioned to outpatient prescribers upon completion of specialty substance use treatment.20
Conclusion
These results support that the availability of pharmacotherapy, such as medications for OUD and AUD, at SUD treatment facilities is associated with an increased number of recommended treatment components. Since medications such as buprenorphine/naloxone have been shown elsewhere to reduce mortality for people with OUD, they should be universally available at SUD treatment facilities. The availability of MOUD at a treatment facility may also serve as a marker of other medical services to consumers in search of specialty treatment. Having more evidence-based, recommended treatment options increases patient choice and promotes patient-centered treatment planning. Further efforts are needed to make pharmacotherapy and MOUD more widely available at specialty treatment facilities; such efforts may include reinvigorating program certification criteria to require medications for OUD and AUD, state policies that promote the incorporation of medications for OUD or AUD, and utilizing tax-dollars and other grant funding to expand availability of such services.
Disclosure
Dr. Benjamin Miskle reports stock options from Johnson & Johnson, received speaker fees at the annual meeting from Iowa Pharmacists Association, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. SAMHSA. Key substance use and mental health indicators in the United States: results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH series H-55). Available from: https://www.samhsa.gov/data/.
2. Overdose deaths accelerating during Covid-19; 2020. Available from: cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html.
3. Ainscough TS, McNeill A, Strang J, Calder R, Brose LS. Contingency management interventions for non-prescribed drug use during treatment for opiate addiction: a systematic review and meta-analysis. Drug Alcohol Depend. 2017;178:318–339. doi:10.1016/j.drugalcdep.2017.05.028
4. Dugosh K, Abraham A, Seymour B, McLoyd K, Chalk M, Festinger D. A systematic review on the use of psychosocial interventions in conjunction with medications for the treatment of opioid addiction. J Addict Med. 2016;10(2):93–103. doi:10.1097/ADM.0000000000000193
5. Rees CE, Cleland JA, Dennis A, Kelly N, Mattick K, Monrouxe LV. Supervised learning events in the foundation programme: a UK-wide narrative interview study. BMJ Open. 2014;4(10):e005980. doi:10.1136/bmjopen-2014-005980
6. Fullerton CA, Kim M, Thomas CP, et al. Medication-assisted treatment with methadone: assessing the evidence. Psychiatr Serv. 2014;65(2):146–157. doi:10.1176/appi.ps.201300235
7. Evans EA, Zhu Y, Yoo C, Huang D, Hser YI. Criminal justice outcomes over 5 years after randomization to buprenorphine-naloxone or methadone treatment for opioid use disorder. Addiction. 2019;114(8):1396–1404. doi:10.1111/add.14620
8. Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550. doi:10.1136/bmj.j1550
9. Krawczyk N, Mojtabai R, Stuart EA, et al. Opioid agonist treatment and fatal overdose risk in a state-wide US population receiving opioid use disorder services. Addiction. 2020;115(9):1683–1694. doi:10.1111/add.14991
10. SAMHSA. Finding quality treatment for substance use disorders; 2018. Available from: store.samhsa.gov/product/Finding-Quality-Treatment-for-Substance-Use-Disorders/PEP18-TREATMENT-LOC.
11. NIAAA. Step 1 - search trusted sources to find providers. Available from: alcoholtreatment.niaaa.nih.gov/how-to-find-alcohol-treatment/step-1-search-trusted-sources-to-find-providers#search-programs.
12. Mark TL, Dowd WN, Council CL. Tracking the quality of addiction treatment over time and across States: Using the federal government’s “Signs” of higher quality. tracking the quality of addiction treatment over time and across states: using the federal government’s “Signs” of higher quality. RTI Press Research Report Series. 2020.
13. Abraham AJ, Andrews CM, Harris SJ, Friedmann PD. Availability of medications for the treatment of alcohol and opioid use disorder in the USA. Neurotherapeutics. 2020;17(1):55–69. doi:10.1007/s13311-019-00814-4
14. Marynak K, VanFrank B, Tetlow S, et al. Tobacco cessation interventions and smoke-free policies in mental health and substance abuse treatment facilities - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(18):519–523. doi:10.15585/mmwr.mm6718a3
15. Substance Abuse and Mental Health Services Administration. Data from: treatment episode data set admissions (TEDS-A): 2017. 2019.
16. Team RC. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020.
17. US surgeon general’s advisory on naloxone and opioids overdose; 2020. Available from: https://www.hhs.gov/surgeongeneral/priorities/opioids-and-addiction/naloxone-advisory/index.html.
18. Beetham T, Saloner B, Gaye M, Wakeman SE, Frank RG, Barnett ML. Admission practices and cost of care for opioid use disorder at residential addiction treatment programs in the US. Health Aff. 2021;40(2):317–325. doi:10.1377/hlthaff.2020.00378
19. Andrilla CHA, Moore TE, Patterson DG, Larson EH. Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: a 5-year update. J Rural Health. 2019;35(1):108–112. doi:10.1111/jrh.12307
20. Marino R, Perrone J, Nelson LS, et al. ACMT position statement: remove the waiver requirement for prescribing buprenorphine for opioid use disorder. J Med Toxicol. 2019;15(4):307–309. doi:10.1007/s13181-019-00728-9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
