Back to Journals » Patient Preference and Adherence » Volume 14
Self-Medication Practice and Associated Factors Among University of Gondar College of Medicine and Health Sciences Students: A Cross-Sectional Study
Authors Zeru N, Fetene D, Geberu DM , Melesse AW , Atnafu A
Received 4 August 2020
Accepted for publication 15 September 2020
Published 1 October 2020 Volume 2020:14 Pages 1779—1790
DOI https://doi.org/10.2147/PPA.S274634
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Nuhamin Zeru,1 Destaw Fetene,2 Demiss Mulatu Geberu,3 Alemakef Wagnew Melesse,2 Asmamaw Atnafu3
1University of Gondar Comprehensive Specialized Hospital, Gondar, Ethiopia; 2Department of Epidemiology and Biostatistics, University of Gondar, Gondar, Ethiopia; 3Department of Health Systems and Policy, University of Gondar, Gondar, Ethiopia
Correspondence: Asmamaw Atnafu
University of Gondar, P.O. Box 196, Gondar, Ethiopia
Tel +251-918776945
Email [email protected]
Purpose: Self-medication is the use of medicines by individuals to treat self-recognized illnesses or symptoms without any medical supervision. Such practices may cause antimicrobial resistance, which causes treatment failure, economic loss, serious health hazards, missed diagnosis, delayed appropriate treatment, drug dependency, and adverse drug effects. However, empirical evidence is limited to the current status of its practices and associated factors among university students. Thus, the aim of this study was to assess the magnitude and associated factors of self-medication practices among medicine and health science students at the University of Gondar.
Methods: An institution-based cross-sectional study was employed from February to March 2017. A total of 792 randomly selected students were surveyed with a self-administered structured questionnaire. Epi Info version 7 and SPSS version 20 were used for data entry and analysis, respectively. Binary logistic regression analysis was performed. In multivariable analysis, P-value < 0.05 and adjusted odds ratio (AOR) with 95% confidence interval (CI) were used to identify associated factors.
Results: Self-medication practice was found to be 52.4% (95% CI: (49%, 56%)) among university students. For most students, the major reason for using self-medication was taking the illness as less serious (71.1%). Females (AOR: 1.48; 95% CI: 1.08– 2.01), income category (USD 44.01– 175.87) (AOR: 0.47; 95% CI: 0.29– 0.78), sixth year students (AOR: 8.71; 95% CI: 4.04– 18.77) and health officer students (AOR: 2.36; 95% CI: 1.20– 4.63) were found to be significantly associated with self-medication practice.
Conclusion: More than half of the students practiced self-medication, which is moderately higher than other findings. Gender, income, year of study, and field of study were the major factors that affected self-medication. Therefore, interventions that can halt the high magnitude of self-medication and factors associated with it are crucial. Special attention should be given to students who stay in the university for longer years.
Keywords: self-medication, university students, College of Medicine and Health Science
Introduction
Having access to effective and efficient healthcare system in a community is unquestionable, as good health is the fundamental requirement of life. However, in developing countries, is very limited or almost no access to modern healthcare infrastructures and appropriate and affordable medication.1,2 Due to this situation, most episodes of illness are treated by self-medication (S.M.). Self-medication is the selection and use of medicines by individuals to treat self-recognized illnesses or symptoms without professional supervision regarding indication, dosage, and duration of treatment.3,4 Additionally, it is the intermittent or continued use of drugs prescribed by a licensed health professional for chronic or recurring disease conditions.3
In most developing countries such as Ethiopia, many drugs are dispensed over the counter (OTC), and the majority of the medical conditions, nearly 12.1–62.9%, are treated through self-medication at optional and cheaper costs.5–7 However, there is a clear difference between the practices of self-medication with OTC drugs and the way of purchasing and using prescription-only medicines without a doctor’s order. This means that the rule of OTC medicines is violated in developing countries, particularly in our setup since many prescription-only drugs are purchased and used at OTC corners. This is potentially a dangerous kind of self-prescription, and such type of practice is common in many developing countries such as Ethiopia. This facilitates the emergence of antimicrobial resistance.8 Hence, the national drug regulatory authority needs to evaluate, approve, and list drugs that are safe for self-medication.
Evidence from different studies showed that the practices of self-medication have been used to treat different perceived disease conditions like headache,5,7,9–17 common cold,5–7,11,12,15,16,18,19 fever,6,18,19 cough5,6,12,16 and respiratory tract infections.11,12,20 Moreover, these practices were attributed to different reasons such as previous experience,7,13,15,16,21–25 mildness of disease,6,9,14–16,22,24–27 lack of time to consult health professionals1,13,16,28,29 and cost-effectiveness.16
If self-medication is not guided by reliable medical information, it will directly or indirectly lead to irrational or misuse of medicines, which was 7.3% to 99.4% prevalent in different global studies. In this regard, the availability of reliable information about proper handling and utilization of self-medication is inadequate in many developing countries.21,30 Furthermore, the readily available wide range of drugs without the prescription of a registered prescriber is the major problem responsible for the irrational use of medicines as self-medication, and this has impacts on different health-related conditions31 such as antimicrobial resistance, which causes treatment failure, economic loss, increased load of morbidity and mortality in addition to wastage of efforts and resources, missed diagnosis, delayed appropriate treatment, drug dependency, and adverse drug effects.5,31–33 To clarify one of the aforementioned impacts of self-medication, a study conducted in Ghana, for example, revealed that there were an immense practice of self-medication (70%) and high percentage (35%) of treatment failure on these self-medicated students. Besides, this same study showed that the utilized drugs caused a high rate (72–83%) of resistance by many common disease-causing etiologies.1 As a result, a high percentage of treatment failure, which was highly associated with self-reported medication, was partly explained by this drug resistance.1,2 Another study also indicated that drug resistance has direct correlation to the non-prescribed use of antibiotics.23 Moreover, infections due to resistant bacteria cause not only high mortality and poor quality of life of infected patients but it also increases the strain on health systems and the risk of such infections dissemination.2
Self-medication is widely practiced both in developed and developing countries, and its prevalence ranges from 12.1% to 92.8%, respectively.6,34 The prevalence of SM among university students ranges from 64.8% to 77.2% in the Middle East,11,22 71.7% to 95.3% in Asia,12,13 24% to 91.4% in Africa and 38.55% to 77.1% in Ethiopia.14,21,23,32,35 The literature reviewed on various works and the meta-analysis revealed that 67% (with an interval of 55–81%) of Iranian students had self-medication.36
Several studies revealed a range of factors that affect self-medication practice. Accordingly, the socio-demographic factors include sex,1,5,7,11,14,28,32,34,37 age,18,23,32,34,37 monthly income,14,23,29,37 level of education,32,37 residence,15,34 religion,15 marital status,7,29,34,38 year of study,5,10–12,32,38,39 and field of study.1,5,11,12,14,23 Moreover, the source of drugs for self-medication such as community pharmacies,6,15,23,29,32 drug stores,16,32 unused drugs stored at home,11,40 friends and relatives5 are repeatedly reported in numerous relevant literatures. Such sources of drugs greatly influence, contribute and facilitate the occurrence of SM practice. Largely, self-medication has a strong relationship with sources of information such as pharmacists,15,21,24 physicians/nurses, but without prescriptions,21 friends or relatives, different readings, and reading materials.12,15
Different works in the literature showed that self-medication is widely practiced both in developed and developing countries around the globe, and its magnitude is variably increasing. To the best of researcher’s knowledge and the literature reviewed, there are, however, few empirical evidence in Ethiopia, particularly in the study setting where there is only one study35 which was conducted before seven years. This study did not assess the associated factors of self-medication and its prevalence, which is the area to be addressed in the current study. Previous studies did not also simultaneously address factors affecting S.M., reasons of S.M., and perceived disease conditions that lead to S.M., the source of the drugs, and sources of information. Thus, within its global burden and impact, knowing its magnitude and associated factors at a university level is essential and has a pivotal role in devising appropriate educational, regulatory, and administrative measures. Hence, this study assessed the magnitude and factors associated with self-medication practices among Medicine and Health Sciences students at the University of Gondar.
Materials and Methods
Study Design and Setting
An institution-based cross-sectional study was conducted from February to March 2017. The study was conducted in the College of Medicine and Health Science, University of Gondar (UoG), located in Gondar town, which is found Northwest of Addis Ababa and 741 km away from it. The university was established in 1954 as a Public Health College and Training Center. Nowadays, it is one of the highest rank universities in Ethiopia. University of Gondar encompasses five colleges, and one of which is the College of Medicine and Health Sciences and comprehensive specialized hospital, which is comprised of one institute and five schools. The college is expanding the scope of its activities. Currently, it is providing training to students in areas of Medicine, Health officer, Pharmacy, Nursing, Midwifery, Environmental & Occupational Health & Safety, Physiotherapy, Medical Laboratory Technology, Optometry, Anesthesia, Psychiatry, and Health Informatics. The college has a total of 4359 regular undergraduate students; of which 2812 are males and attending regular programs at different levels of year of study. The students receive healthcare services mainly from University of Gondar Comprehensive Specialized Hospital, which is one of the tertiary level and teaching Hospitals in Amhara region, and various private and governmental healthcare settings.
Source and Study Population
All regular undergraduate students of the College of Medicine and Health Sciences at the University of Gondar who attended their class in the 2016/2017 academic year were the source population. Whereas all regular undergraduate students of the selected departments of the College of Medicine and Health Sciences in the 2016/2017 academic year were the study population.
Sample Size Determination and Sampling Procedures
The sample size was calculated based on the single population proportion, by taking P= 38.5%, which is the proportion of students with self-medication practice taken from a study conducted in 2010 in Gondar, Ethiopia,13 and by assuming d as the margin of error (0.05), 95% confidence level at Z/2 (α = 0.05) = 1.96 and design effect =2. Finally, by adding a 10% non-response rate, the final sample size was 801.
by taking P= 38.5%, which is the proportion of students with self-medication practice taken from a study conducted in 2010 in Gondar, Ethiopia,13 and by assuming d as the margin of error (0.05), 95% confidence level at Z/2 (α = 0.05) = 1.96 and design effect =2. Finally, by adding a 10% non-response rate, the final sample size was 801.
A stratified multistage sampling technique was employed based on the field of study and years of study. Accordingly, out of 12 departments that have undergraduate students in the College of Medicine and Health Sciences, four of them were selected by simple random sampling. Then, the sample was proportionally allocated for all the selected four departments based on the respective total number of regular undergraduate students. Additionally, the selected departments were again stratified into different years of study, and the proportional allocation of the sample was done accordingly. Finally, the required number of study participants were selected by using simple random sampling technique.
Inclusion and Exclusion Criteria
All regular undergraduate students from the selected departments of the College of Medicine and Health Science during 2016/17 academic year were included. Those who had a serious illness and had been hospitalized during the data collection period were excluded.
Data Collection Tool and Procedure
Data were collected through a pretested structured self-administered questionnaire adapted from similar previous studies based on the objectives of this study. One supervisor and three data collectors who are diploma pharmacy technicians were hired.
During data collection, the representatives of each class were communicated to inform the students to stay in their classes until the data collectors meet them. After explaining the purpose of the study, the sample students were requested to sign a written consent. Then, these students filled the required data in the self-administered questionnaire. When the randomly selected students were absent during the data collection time, students who were next to the absent students were requested to replace them. Similarly, during this collection process, students who expressed their refusal to participate in the study or were unable to finish the questionnaire were counted as non-respondents.
The questionnaire was prepared in English and translated into Amharic and was back-translated into English to check its consistency. To assure the content validity of the prepared questionnaire, it was reviewed by three subject experts in addition to the investigators. The questionnaire included socio-demographic variables (age, sex, marital status, the field of study, year of study, monthly pocket money, and drug expenditure), general information on self-treatment with medication, and other associated conditions such as perceived illness (headache, respiratory tract infection, G.I. disease, fever, Eye diseases), sources of drugs (pharmacies, medicines stored at home, friends and family members, herbalists), sources of information on medication (received no advice, red label or leaflet, advised by relatives, from internet, advised by health workers but without a prescription), and reasons for self-prescribing of medication (disease is not serious, emergency use, for prevention of disease, prior experience about the drug, less expensive in terms of time/money).
Data Quality Control
Data quality issues were assured by conducting a pretest on 40 students (5% of total sample size) from the non-selected departments in the College of Medicine and Health Science. Necessary corrections, as well as amendments, were made on the tool before the actual data collection. Additionally, a one-day-long training was also given to the three data collectors and the supervisor about the data collection tools and the sampling techniques. Moreover, the data were checked daily for completeness, consistency and when problems faced, they were corrected with regular supervision during the data collection period.
Operational Definition
Self-Medication
It is the selection and use of medicines by individuals, within three months, to treat at least one self-recognized illness or symptoms without professional prescription and supervision regarding indication, dosage, and duration of treatment.14,38
Data Processing and Analysis
The completed data were checked, cleaned, coded, and entered into Epi Info version 7 and then exported to SPSS version 20 for analysis. Text narration, tabulation, and descriptive statistics, like frequencies, percentages, means, and standard deviation were used to present the descriptive result. Whereas binary logistic regression was used to explain factors associated with self-medication practice. In the bi-variable analysis, variables with a P-value of less than 0.2 were entered into the multivariable analysis. Variables that have a P-value less than 0.05 in the multivariable logistic regression analysis were taken as statistically significant factors for the dependent variable. The strength of the association was presented by adjusted odds ratio and 95% Confidence interval.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Institutional Research Review Board of the Institute of Public Health, CMHS, the University of Gondar, which approved the procedure, and a support letter was obtained from the student dean of CMHS, University of Gondar. Written informed consent was obtained from each participant after the purpose, and the objectives of the study were made clear. The confidentiality of respondents was maintained by using anonymity. Finally, the research was conducted in accordance with the declaration of Helsinki.
Results
Socio-Demographic Characteristics of Study Participants
A total of 792 study participants (students) answered the questionnaire with a response rate of 98.8%. More than half (54.5%) of the participants were between 21 and 23 years old with a mean age of 21.35 years and a standard deviation of ±1.69 years. Sixty-one percent of the respondents were males, and 98.5% of the participants were single. The majority (63.1%) of the students were Amhara, followed by Oromo (24.1%). Among the total study participants, 65.7% were from medicine, and 13.9% were from the Health officer department. Almost 25% of the participants were 2nd-year students, and 65% were Orthodox Christian by religion (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Study Participants (Students), CMHS, University of Gondar, Gondar, Ethiopia, May 2017 (n=792) |
Illness/Symptoms for Self-Medication and Duration of Illness Before Self-Medication
Most (86.5%) self-medicated students had a history of headache followed by 53% respiratory tract infection and 47.9% gastrointestinal disease. Regarding the duration of illness before using self-medication, 55.9% of self-medicated respondents had used the medicine within 24 hours of the illness, whereas 3.1% of the respondents used the medicine after 5 to 12 weeks of the illness duration (Table 2).
 |
Table 2 Illness/Symptoms for Self-Medication and Illness Before Self-Medication at Students of CMHS, University of Gondar, Gondar, Ethiopia, May 2017 (N= 415) |
Reason, Source of Drugs and Information for Self-Medication, Type of Requested Drug, and Outcome of Treatment
Among the total 415 respondents that used self-medication, 76.1% of them reported that they used self-medication due to the fact that the disease was not serious and 59% of them used it for Emergency. Analgesic/antipyretic that is used for mild to moderate pain relief without losing consciousness (71.8%) and Antimicrobial (57.3%) were the major requested types of drugs. Ninety-five percent of the source of drugs for self-medication were purchased from pharmacies, followed by 24.8% of unused drugs stored at home.
Regarding the source of information for self-medication, more than half of the participants (52%) reported that they did not receive advice, followed by 41.2% of the respondents read labels or leaflets and 35.6% of them were advised by doctors, nurses, health workers but without prescription. Two hundred seventy-five (66.6%) of the respondents claimed that they had successfully cured from the illness, and 59.2% of the respondents reported that as they showed improvement from the illness (Table 3).
 |
Table 3 Reason, Source of Drugs and Information for Self-Medication, Type of Requested Drug and Outcome of Treatment at Students of CMHS, University of Gondar, Gondar, Ethiopia, May 2017 (n=415) |
Prevalence of Self-Medication
In this study, the magnitude of self-medication practice among students was 415 (52.4%) with (95% CI: (49%, 56%)) (Figure 1).
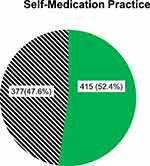 |
Figure 1 Magnitude of self-medication practice among University of Gondar, CMHS students, Gondar, Ethiopia, May 2017. |
Factors Associated with Self-Medication Practice
All the covariates had been checked for crude association with self-medication practice among the study participants in a bi-variable analysis at binary logistic regression. Of all covariates, sex, age, income, marital status, year of study, and field of study were found to have an association with self-medication practice at p-value < 0.2. These variables were entered into multivariable logistic regression so as to determine the statistically significant association of variables with self-medication practice. After performing multivariable logistic regression, sex, income, field of study, and year of study had statistically significant association with self-medication practice at p-value <0.05.
Accordingly, female respondents were 1.5 times (AOR: 1.48; 95% CI: 1.08–2.01), more likely to use self-medication than male students. Respondents who had USD 44.01–175.87 category of income per month were 53% (AOR: 0.47; 95% CI: 0.29–0.78) less likely to use self-medication than those who had USD 22 or less.
Regarding the respondent’s year of study and department, sixth-year students were 8.7 times (AOR: 8.71; 95% CI: 4.04–18.77) more likely to use self-medication than first-year students. Respondents who belonged to the health officer department were 2.3 times (AOR: 2.36; 95% CI: 1.20–4.63), more likely to use self-medication than those students who belonged to the psychiatry department (Table 4).
 |
Table 4 Bi-Variable and Multivariable Logistic Regression Analysis of Self-Medication Practice at Students of CMHS, University of Gondar, Gondar, Ethiopia, May 2017 (n=792) |
Discussion
The aim of this study was to assess the prevalence and associated factors of self-medication among students of college of medicine and health science at the University of Gondar. The current study revealed that the prevalence of self-medication practice among the participants was found to be 52.4% with (95% CI: (49%, 56%)). This finding is almost similar to the studies conducted at King Soud University (50.9%)16 and the University of Damman city (49.3%)24 in Saudi Arabia. Whereas our study finding was higher than those studies conducted in Rwanda (12.1%),6 Spain (12.7%),34 Tabuk city/KSA (43.24%),41 New Delhi, India (44.5%)42 and China (47.8%).23 This difference might be due to the respondents’ cultural difference, healthcare systems, infrastructures, and socio-demographic characteristics. For example, the well-established healthcare systems and infrastructures in developed countries might create suitable conditions for clients to consult their healthcare professionals and use drugs ordered by these professionals. As a result, their self-medication practice would be lower than the result of our study. Additionally, respondents from Spain, India and China countries could get strong health education about the risk factors of self-medication and its negative effect on health and life, so this leads them to lower self-medication practices.
On the other hand, the finding of this study was lower than those studies carried out in Egypt (62.9%),7 Saudi Arabia (64.8%),11 Pakistan (66%),29 Ghana (70%),1 Nagpur India (71.7%),12 Iran (72%),9 Khartoum state, Sudan (73.9%),37 University students of Karachi (76%),17 Arsi University, Ethiopia (77.1%),14 United Arab Emirates (77.2%),43 South India (80.4%),27 Iran (81%),44 University of Karachi, Pakistan (81.28%),13 Southern Nigeria (91.4%),32 West Bengal (92%)26 and India (92.39%). This difference might be due to the variation in socio-demographic and economic profiles, geographical and study time variation in which self-medication practice was assessed, and availability of drugs on over the counter.
In the case of the factors associated with self-medication, female respondents were more likely to use self-medication. This finding is in agreement with studies conducted in Ghana,1 Mekele and Jimma Universities, Ethiopia,5,45 Taibah University, Saudi Arabia,11 South India,28 South Western Nigeria,32 Spain,34 and Khartoum state, Sudan.37 The possible reason might be female students faced recurrent disease conditions more than their male counterparts related to their relatively low immunity and continuous menstrual cycle due to hormonal effect. This monthly menstrual cycle is strongly associated with anti-pain drugs like Ibuprofen, which may result in gradually adapting drugs and make them hesitant not to visit healthcare organizations that finally leads them to a high magnitude of self-medication.1
In this study, those respondents who had higher income per month were less likely to use self-medication than who had lower income. This finding is in line with studies carried out in Arsi University, Ethiopia.14 The possible justification might be students who have lower income might not be able to afford to visit healthcare institutions and to consult licensed health professionals. So, they might be urged to buy drugs with the lower cost from over the counter centers without prescription which, in turn, leads to high self-medication practice. However, this finding is in contrast with studies conducted in Southern China23 and Pakistan.29 These studies revealed that income and self-medication practices have direct relationship and justified that students who have lower income might visit the school health clinic that delivers free service, or they might ignore miner disease conditions like the common cold.
The other associated factor in the present study was the students’ year of study. Likewise, the sixth year students were more likely to use self-medication than first-year students. This finding is comparable with studies carried out in Mekelle University, Ethiopia,5 Taibah University, Saudi Arabia,11 Nagpur India,12 North India,38 and Pakistan.39 This could be as the students’ year of study increases, they take more practical-oriented courses. Hence, their knowledge and understanding about drugs and diseases would also increase, which resulted in high uptake and purchase of medication without prescription since the regulatory system is loose.23
The field of study has a statistically significant association with self-medication in this study. Accordingly, students of the health officer department were more likely to use self-medication than psychiatry department students. This finding is in agreement with the studies done in Mekelle University, Ethiopia,5 Southern China,23 and Nagpur India.12 This might be due to health officer students had taken more courses about disease conditions as well as the drugs that can treat the disease, and this led them to have higher knowledge. This knowledge, in turn, had led health officer students to a false sense of confidence in self-diagnosis and management.23 Nevertheless, the finding of this study is in contrast with the studies carried out in Arsi University, Ethiopia,14 and Ghana.1 In this regard, a study conducted in Ghana tried to reason out that the low practice in medically inclined students was the effect of policies as health education about self-medication and its risks are the basic mechanism to minimize irrational use of drugs through self-medication.1 Furthermore, the possible justification for the difference between our study and these two studies could probably be explained by geographical and cultural variations of factors of self-medication.
In the present study, most (86.5%) self-medicated students had a history of headache as a perceived disease condition. This finding is consistent with studies carried out in Mekele University, Ethiopia,5 Southern Ethiopia,46 Peshawar,47 Jimma, Ethiopia,45 Taibah University, Saudi Arabia,11 University of Karachi, Pakistan,13 Arsi University, Ethiopia,14 Mekelle University (Adi-haqi campus), Ethiopia15 and Punjab, Pakistan.48 The most common reasons for using self-medication were due to disease was not serious/mildness of the illness/316 (71.1%). This finding is in line with those studies conducted in Arsi University, Ethiopia,14 United Arab Emirates,22 public-sector University in Damman city, Saudi Arabia,24 Khartoum, Sudan,25 West Bengal,26 South India.27 On the other hand, other studies revealed that the most common reason for self-medication was previous experience,7,13,15,16,21–25 lack of time to consult health professionals1,13,16,28,29 and to be cost-effective.16
Regarding drug type, most of the self-medicated students requested Analgesic/antipyretic (71.8%) followed by Antimicrobial (57.3%). Varies studies also reported these drug types, i.e. Analgesic/antipyretic8,10,11,16,17,31,44 and Antimicrobial11,31 as the most commonly requested type of drugs. Most (95.4%) of the drugs were purchased from community pharmacies as a source of drugs for self-medication. This finding is in line with studies carried out in Mekelle University (Adi-haqi campus), Ethiopia,15 Southern China,23 Karachi, Pakistan,29 and Southwestern Nigeria.32 Conversely, the other studies showed that the source of drugs for self-medication were drug stores16,32 and unused drugs stored at home.20,40 Regarding the source of information for self-medication, more than half (52%) of the respondents received no advice/sources of information. This finding is not comparable with findings from Mekele, Ethiopia, Indonesia and Damman city, Saudi Arabia15,21,24 which these studies revealed that pharmacists were the most common sources of information.
Limitation of the Study
This study assessed the selection and use of medicines in the last three months before the data collection period. Therefore, there might be a recall bias. Besides, the data collection method of this study was a self-administered questionnaire, which may introduce bias from the respondents’ side based on their behavior. Moreover, this study did not differentiate the self-medication practices towards antibiotics, most of them are prescription-only drugs, instead, it generically assessed for all drugs. Therefore, this condition might result in a higher magnitude of self-medication because some of the components of antiviral and antifungal drugs in the antimicrobial group can be given as over the counter medications.
Conclusion
Assessing students’ self-medication practice and associated factors are very important to different stakeholders to intervene in drug misuse and overcome its impacts. The current study revealed that the prevalence of self-medication practice among university students was high. And the most common disease condition was a headache, and the primary requested drug was Analgesics. Community pharmacies were the most common source of drugs for self-medication, and more than half of the participants did not receive any information for this practice. Gender, high students’ monthly income, the sixth year of study, and field of study were the factors that affected self-medication practices. Therefore, by taking into account the high magnitude, its impact, and the associated factors, it requires great attention especially when students stay longer in university for attending education. Moreover, strict drug prescription by health professionals and creating awareness of drug regulation to the students are essential.
Abbreviations
CMHS, College of Medicine and Health Science; NDP, National Drug Policy; OTC, over the counter; S.M., self-medication; SMP, self-medication practice; UOG, University of Gondar; WHO, World Health Organization.
Data Sharing Statements
All the data supporting the findings are within the manuscript. Additional detailed information and raw data are available from the corresponding author on reasonable request.
Acknowledgments
The authors would like to express our gratitude to the University of Gondar College of Medicine and Health Sciences Institute of Public Health for ethical approval. We also would like to thank the supervisors and all respondents for their willingness to participate in the study.
Author Contributions
All authors contributed to the design, acquisition, analysis, and interpretation of data; drafting and revising of the article; have agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Donkor ES, Tetteh-Quarcoo PB, Nartey P, Agyeman IO. Self-medication practices with antibiotics among tertiary level students in Accra, Ghana: a cross-sectional study. Int J Environ Res Public Health. 2012;9(10):3519–3529. doi:10.3390/ijerph9103519
2. WHO. Community-Based Surveillance of Antimicrobial Use and Resistance in ResourceConstrained Settings. World Health Organization; 2009.
3. Organization W.H. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication. Geneva: World Health Organization; 2000.
4. WSMI. The story of self care and self medication. The World Self-Medication Industry; 2010. Available from: http://wwwwsmiorg/pdf/fippdf.
5. Gutema GB, Gadisa DA, Kidanemariam ZA, et al. Self-medication practices among health sciences students: the case of Mekelle University. J Appl Pharm Sci. 2011;1(10):183.
6. Tuyishimire J, Okoya F, Adebayo AY, Humura F, Lucero-Prisno III DE. Assessment of self-medication practices with antibiotics among undergraduate university students in Rwanda. Pan Afr Med J. 2019;33.
7. Helal R, Abou-ElWafa H. Self-medication in university students from the city of Mansoura, Egypt. J Environ Public Health. 2017;2017.
8. Hussain SMF, Ashfaq KM, Malik F, et al. Prevalence of self-medication and health-seeking behavior in a developing country. Afri J Pharm Pharm. 2011;5:972–978.
9. Niroomand N, Bayati M, Seif M, Delavari S, Delavari S. Self-medication pattern and prevalence among Iranian medical sciences students. Curr Drug Saf. 2020;15(1):45–52. doi:10.2174/1574886314666191022095058
10. Tesfaye ZT, Ergena AE, Yimer BT. Self-medication among medical and nonmedical students at the University of Gondar, Northwest Ethiopia: a cross-sectional study. Scientifica. 2020;2020:1–5. doi:10.1155/2020/4021586
11. Aljaouni ME, Hafiz AA, Alalawi HH, Alahmadi GM, AlKhawaja I. Self-medication practice among medical and non-medical students at Taibah University, Madinah, Saudi Arabia. Int J Acad Sci Res. 2015;3(4):54–65.
12. Kasulkar AA, Gupta M. Self medication practices among medical students of a private institute. Indian J Pharm Sci. 2014;77(2):178–182. doi:10.4103/0250-474X.156569
13. Shoaib MH, Yousuf RI, Anjum F, et al. Survey based study on the use of non-prescription drugs among pharmacists and non-pharmacists. Afri J Pharm Pharm. 2013;7(38):2652–2656. doi:10.5897/AJPP2013.3821
14. Bekele SA, Argaw MD, Yalew AW. Magnitude and factors associated with self-medication practices among university students: the case of Arsi University, College of Health Science, Asella, Ethiopia: cross-sectional survey based study. Open Access Lib J. 2016;3(06):1.
15. Eticha T, Araya H, Alemayehu A, Solomon G, Ali D. Prevalence and predictors of self-medication with antibiotics among Adi-haqi Campus students of Mekelle University, Ethiopia. Internet J Pharma Sci Res. 2014;5:678–684.
16. AlRaddadi KK, Barakeh RM, AlRefaie SM, AlYahya LS, Adosary MA, Alyahya KI. Determinants of self medication among undergraduate students at King Saud University: knowledge, attitude and practice. J Health Spec. 2017;5(2):95–101. doi:10.4103/2468-6360.205078
17. Zafar SN, Syed R, Waqar S, et al. Self-medication amongst university students of Karachi: prevalence, knowledge and attitudes. J Pak Med Assoc. 2008;58(4):214.
18. Kumar VMA, Yadav G, Raut D, Singh S, Singh S. Prevalence and pattern of self-medication practices in an urban area of Delhi, India. Med J DY Patil Univ. 2015;8:16–20. doi:10.4103/0975-2870.148828
19. Parakh R. Self -medication practice among engineering students in an engineering college in North India. J Phytopharmacol. 2013;4(2):30–36.
20. Jassim AM. In-home drug storage and self-medication with antimicrobial drugs in Basrah, Iraq. Oman Med J. 2010;25.
21. Widayati A, Suryawati S, de Crespigny C, Hiller JE. Self medication with antibiotics in Yogyakarta City Indonesia. BMC Res. 2011;(4):491.
22. Shehnaz SI, Sreedharan J, Khan N, Issa KJ, Arifulla M. Factors associated with self-medication among expatriate high school students: a cross-sectional survey in United Arab Emirates. Epidemiol Biostat Public Health. 2013;10(4).
23. Pan H, Cui B, Zhang D. Prior knowledge, older age, and higher allowance are risk factors for self-medication with antibiotics among University Students in Southern China. PLoS One. 2012;7:e41314. doi:10.1371/journal.pone.0041314
24. Albusalih FA, Ahmad R, Ahmad N, Ahmad N. Prevalence of self-medication among students of pharmacy and medicine colleges of a public sector university in Dammam City, Saudi Arabia. J Pharm. 2017;5(4):51. doi:10.3390/pharmacy5030051
25. Furreh FH, Eltayeb AAM, Hamza M, et al. Self-medication practice among health science students in International University Of Africa (Iua), Khartoum, Sudan. World J Pharm Res. 2016;5(5):61–69.
26. Banerjee I, Bhadury T. Self-medication practice among undergraduate medical students in a tertiary care medical college, West Bengal. J Postgrad Med. 2012;58(2):127. doi:10.4103/0022-3859.97175
27. Badiger S, Kundapur R, Jain A, et al. Self-medication patterns among medical students in South India. Australas Med J. 2012;5(4):217. doi:10.4066/AMJ.2012.1007
28. Kumar N, Kanchan T, Unnikrishnan B, et al. Perceptions and practices of self-medication among medical students in coastal South India. PLoS One. 2013;8(8):e72247. doi:10.1371/journal.pone.0072247
29. Limaye D, Farah-Saeed AM, Pitani RS, Fortwengel G, Fortwengel G. Self-medication practices among university students from Karachi, Pakistan. Int J Community Med Public Health. 2017;4(9):3076–3081. doi:10.18203/2394-6040.ijcmph20173635
30. Arikpo G, Eja M, Enyi-Idoh K. Self medication in Rural Africa: the Nigerian experience. Internet J Health. 2009;11(1).
31. Sherazi B, Mahmood K, Amin F, Zaka M, Riaz M, Javed A. Prevalence and measure of self medication: a review. J Pharm Sci Res. 2012;4(3):1774–1778.
32. Osemene K, Lamikanra A. A study of the prevalence of self-medication practice among university students in Southwestern Nigeria. Trop J Pharm Res. 2012;11(4):683–689. doi:10.4314/tjpr.v11i4.21
33. WHO. Self-medication. Sudan J Ration Use Med. 2014;(6)
34. Figueiras A, Caamano F, Gestal-Otero JJ. Gestal-Otero Sociodemographic factors related to self-medication in Spain. Eur J Epidemiol. 2000;16(1):19–26. doi:10.1023/A:1007608702063
35. Abay S, Amelo W. Assessment of self-medication practices among medical, pharmacy, health science students in Gondar University, Ethiopia. J Young Pharm. 2010;2(3):306–310. doi:10.4103/0975-1483.66798
36. Azami-Aghdash S, Mohseni M, Etemadi M, Royani S, Moosavi A, Nakhaee M. Prevalence and cause of self-medication in Iran: a systematic review and meta-analysis article. Iran J Public Health. 2015;44(12):1580.
37. Awad A, EI Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Appl Pharm Sci. 2005;(8):326–331.
38. Aditya S, Rattan A. Self-medication among dental undergraduate students with antibiotics: looking beyond the known. Asian J Pharm Clin Res. 2013;6(Suppl 4):132–135.
39. Fatima S, Akash S, Azhar S, Muhammad D, Bashir S. Medical students perception and practice of self-medication: vision of future practitioner in Pakistan. Br J Pharm Res. 2017;17(1):1–8. doi:10.9734/BJPR/2017/32524
40. Wakgari Deressa AA, Enqusellassie F. Self-treatment of malaria in rural communities, Butajira, southern Ethiopia. Bull World Health Organ. 2003;81(4).
41. Alzhahrani OM, Aloqbi HS A descriptive study of self-medication practices among patients in a public health care system in Tabuk City. 2015.
42. Yadav S, Rawal G. Self-medication practice in low income countries. Int J Pharm Chem Anal. 2015;2(3):139–142.
43. Johnson D, Sekhar HS, Alex T, Kumaraswamy M, Chopra RS. Self medication practice among medical, pharmacy and nursing students. Int J Pharm Pharm Sci. 2016;8(7).
44. Haghighi S, Ashrafizadeh H, Sayadi N. Self-medication and related factors among university students in Iran. J Nurs Midwifery Sci. 2016;3(2):47–51. doi:10.18869/acadpub.jnms.3.2.47
45. Worku S. Practice of Self-medication in Jimma Town. Ethiop J Health Dev. 2003;17(2):111–116.
46. Wabe NT, Ahmed D, Angamo MT. Self-medication with antibiotics and antimalarials in the community of Silte zone, South Ethiopia. TAF Prev Med Bull. 2012;11(5):529–536. doi:10.5455/pmb.1-1314892446
47. Khan SJ, Khan S, Shah N. Self-medication with antibiotics in urban areas of Peshawar. Gomal J Med Sci. 2010;9(1).
48. Conditions, frequencies, and socio-demographic factors leading self medication practice in Sargodha Area of Punjab Pakistan. J Appl Pharm. 2013;5(4):819–826.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
