Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Self-care Related Knowledge, Attitude, and Practice and Associated Factors Among Patients with Type 2 Diabetes in JMC, Ethiopia
Authors Mekonnen Y , Hussien N
Received 11 December 2020
Accepted for publication 22 January 2021
Published 5 February 2021 Volume 2021:14 Pages 535—546
DOI https://doi.org/10.2147/DMSO.S296112
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ming-Hui Zou
Yimer Mekonnen, Nezif Hussien
Department of Pharmacy, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Yimer Mekonnen
Department of Pharmacy, Institute of Health, Jimma University, Jimma, Ethiopia
Email [email protected]
Background: A patient’s knowledge, attitude and practice toward diabetes self-care is found to be imperative for them to attain the desired treatment targets and contribute meaningfully in the management of their disease.
Objective: To assess the knowledge, attitude and practice towards diabetes self-care with the associated factors among patients with type 2 diabetes mellitus (T2DM) in Jimma Medical Center, Ethiopia.
Methods: A cross-sectional study was conducted to determine knowledge, attitude, and practice toward diabetes self-care. Three hundred and seventy-one T2DM patients attending Jimma Medical Center from March 30 to June 1, 2019 were included in this study and an interviewer-administered questionnaire was used to collect the data. SPSS version 20 was used for descriptive and logistic regression analysis. Odds ratios and their 95% confidence intervals together with p-value < 0.05 were used to declare statistical significance.
Results: Out of 371 patients, 201 (54.2%) were male. Of the total, 235 (63.3%) had good knowledge, 221 (59.6%) had positive attitude, and 201 (54.2%) had good self-care practice toward diabetes. Primary educational level (AOR=1.895) was associated with poor knowledge of diabetes, while urban living (AOR=0.570) was protective for low knowledge of diabetes. Monthly income < 1000 Ethiopian birr (ETB); (AOR=2.723) and 1000– 3000 ETB; (AOR=1.126), illiterate (AOR=2.3), and duration of diabetes mellitus (DM) < 5 years (AOR=2.242) were significantly associated with negative attitude. Having other comorbidities (AOR=0.602) was less likely to have negative attitude towards diabetes. Patients age, 41– 50 years (AOR=2.256), and 51– 60 years (AOR=2.677), education: being illiterate (AOR=4.372), primary level (AOR=4.514), and earning monthly income < 1000 ETB (AOR=4.229) were significantly associated with poor self-care practice. On the contrary, being male (AOR=0.198) was less likely to have a poor self-care practice.
Conclusion: The knowledge level, attitude status and self-care practice among T2DM patients were found to be optimal.
Keywords: knowledge, attitude, self-care practice, type 2 diabetes mellitus, Jimma, Ethiopia
Background
Diabetes mellitus (DM) is a metabolic disorder characterized by a persistently elevated blood glucose associated with absent or inadequate pancreatic insulin secretion, with or without concurrent impairment of insulin action.1 It is associated with abnormalities in carbohydrate, fat, and protein metabolism, which results in chronic complications, including microvascular, macrovascular, and neuropathic disorders.2 There are two main types of diabetes, type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM). According to the latest report of the International Diabetes Federation (IDF) there are more than 463 million people living with diabetes worldwide.3 T2DM is the most common form of DM, which accounts for 90% to 95% of all persons with diabetes4 and is expected to increase to 439 million by 2030.5
Formerly, diabetes has been a disease affecting developed countries and wealthy people. However, recently, it became a health problem in all populations worldwide, particularly developing countries.6 In the last few decades, the prevalence of diabetes increased alarmingly reaching epidemic level, affecting people in all age groups in both urban and rural settings.7,8 According to the latest report of the IDF, it was estimated that 19 million people (20–79 years of age) are living with diabetes in Africa and this figure is estimated to increase to 47 million by 2045.3 In Ethiopia, according to a WHO report of 2016, the overall prevalence of DM is estimated to be 3.8%9
DM is a chronic disease, requiring a multipronged approach for its management, wherein the patient has an important role to play.9 Patient knowledge about the disease and self-care practices is very important for patients to attain the desired treatment goal and contribute significantly in the management of their disease.10 The chronic nature of diabetes and handling of the majority of the day to day care of the patient in ambulatory care necessitate promoting and strengthening self-care practices among all patients with diabetes.10,11 However, qualitative research done in different parts of Ethiopia indicated that self-care practice is still low, in the range of 25% to 63.8%.12–17
Although the prevalence of diabetes mellitus is high in the Jimma area, patients’ knowledge, attitude and practice toward diabetes self-care with their associated factors is not well studied. Therefore, this study was conducted to evaluate the levels of knowledge, attitude, and practice toward diabetes self-care with associated factors among T2DM patients attending the diabetic clinic of Jimma University Medical Center (JMC).
Methods
Study Design and Area
An institutional-based cross-sectional prospective study design was conducted from March 30 to June 1, 2019, in the diabetic clinic of Jimma Medical Center (JMC). JMC is located in Jimma town, about 355 km from the capital of Ethiopia, Addis Ababa. It is currently the only teaching and specialized hospital in the southwest part of the country. The hospital serves as a referral site and provides specialized care for the southwest region with a catchment population of more than 15 million.
Study Population
The study population was all sampled adult T2DM patients who visited the diabetic clinic of JMC at the time of data collection period and fulfilling the inclusion criteria.
Inclusion Criteria
The inclusion criteria were: diagnosed with T2DM; able to participate without a mental disability that could affect his/her decisions; no physical disability affecting self-care; and being over 18 years of age.
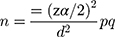
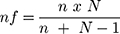
Sample Size Determination
The sample size was determined using a single population proportion formula. The proportion of DM self-care practice from the previous study (50.8%),18 with the assumption of 5% marginal error and 95%CI, the sample size was calculated as follows:
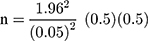
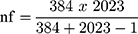
Since the total number of T2DM patients at the diabetic clinic of JMC is 2023, which is less than 10,000, the following correctional formula was used.
By adding 10% contingency value and 5% nonresponse rate, the final sample size was calculated to be 371.
Sampling Technique
In the diabetic clinic of JMC, each person with diabetes visits their doctor at least once every two months. The total number of persons with diabetes having a follow-up at the diabetic clinic is 2023. To get representative sample, every fifth person with diabetes was selected by using a systematic random sampling technique.
Data Collection Tool and Procedure
The data collection tool was developed based on previous similar studies12,19–21 and patient follow-up charts. It was originally prepared in English then translated to local languages (Afan Oromo and Amharic), and back translated to English by independent language experts. The questionnaire was evaluated for face validity by experts dealing with persons with diabetes and the content validity of the questionnaire was done after several meetings with other experts working in the diabetic clinic of JMC (two physicians, a dietician, a nurse, a psychologist). The reliability of the questionnaire was assessed by calculating Cronbach’s alpha. The score was 0.55 upon removal of three questions with poor reliability scores. In addition, the questionnaire was administered to five randomly selected individuals with no history of DM to improve the clarity of questions. Finally, considering comments of the experts, a pilot study was conducted on 37 patients (10% of the sample size), based on which the final version of the questionnaire was used for this study.
The tools consisted of five parts: part one assessed the sociodemographic information of the study participants (ie, age, sex, residence, religion, educational status, marital status, and average monthly income); part two contained disease and treatment-related questions (ie, how long since diagnosed with DM, duration on antidiabetic medication, current medication taken and other comorbidities present); parts three, four, and five included questions related to knowledge, attitude and diabetes self-care practice, respectively. Data were collected through direct interview by three trained nurses and one supervisor.
Knowledge Attitude and Practice (KAP) Scoring
A total of 11 items were included in the knowledge section which assessed patient’s awareness about diabetes self-care (importance and frequency of foot care, importance and frequency of eye clinic visit and physical activity). For the 11-item knowledge questions, the maximum attainable score was “11“ and the minimum score was “0”.
Likewise, in the attitude section, a total of seven items were included which consisted of respondents attitude toward diabetes self-care in a five-point Likert scale response options (strongly disagree, disagree, neutral, agree, and strongly agree) scored from one to five. Each scale response were summed and divided by the total number of items (seven) to generate subscale scores. Respondents with subscale score above or equal to the average were considered to have a positive attitude.
In the same fashion, 11 self-care practice-related questions covering diet, physical activity, blood glucose testing, foot care, medication, smoking, and alcohol consumption were provided to patients. Responses were Yes/No with maximum attainable score of 11 and the minimum score of 0. The combined level of knowledge, attitude and practice (KAP) was classified according to each respondent’s score. Good knowledge, positive attitude, and good self-care practice corresponded to a score greater than or equal to the mean of each variables, while Poor knowledge, negative attitude and poor self care practice corresponded to a score less than the mean of each variables.
Data Quality Assurance
The quality of data was assured by properly designing the tool, and the questionnaire was pretested in JMC, and important modifications were made prior to the actual data collection. A two-day training was provided to the data collectors on the data collection tool, how to ask questions, and the way of approaching respondents. The collected data were checked carefully on a daily basis for completeness, accuracy, and clarity by a supervisor, and the principal investigators monitored the overall activities of data collection.
Data Analysis
Data was coded, entered and analyzed using SPSS version 20. Binomial and multivariate logistic regression analysis was done to identify factors affecting knowledge, attitude and practice of self-care. In all analyses a p-value of <0.05 (two-tailed test) was considered as criterion of statistical significance.
Variables
Dependent Variables
Knowledge level, attitude and practice status toward diabetes self-care
Independent Variables
Demographic characteristics: age, sex, religion, educational status, marital status, residential place and monthly income. Clinical characteristic: duration of DM, comorbidity and treatment modalities
Results
Demographic Characteristics of Participants
Sociodemographic characteristics of the study participants are depicted in Table 1. All of the 371 T2DM patients selected for the interviews were willing, giving a response rate of 100%. More than half, 201 (54.2%) of the study participants were male. Most of the respondents 131 (35.31%) were in the age group of above 60 years. More than half, 203 (54.7%) of the study participants were Muslim religion followers and the majority were married, 253 (68.2%). With regard to education status, one-third of the study participants 124 (33.4%) had primary education, while one quarter, 93 (25.10%) had no formal education and nearly half, 171 (46.09%) of them secure an average monthly income of 1000–3000 ETB.
 |
Table 1 Demographic Characteristics of Participants with T2DM on Follow-up at JMC, 2019 (n=371) |
Knowledge Regarding Diabetes Mellitus
The mean (±SD) of knowledge score for the study participants was found to be 5.94±1.98 (range: 1–11) with a maximum possible score of 11. A total of 235 (63.3%) participants had good knowledge about DM. In the majority of participants, 285 (76.8%) had good knowledge about the frequency of eye clinic visits, and 268 (72.2%) had knowledge on signs and symptoms of hypoglycemia. However, only 79 (21.3%) participants were known to have knowledge on hypoglycemia management (Table 2).
 |
Table 2 Knowledge Towards Diabetes Self-care Among T2DM Patients on Follow-up at JMC, 2019 (n=371) |
Attitude Status Toward Diabetic Self-care
The mean ±SD of attitude score for the study participants was found to be 4.087±0.56 (range: 2–5). More than half, 221 (59.6%) of the study participants had attitude score greater than the mean, indicating they had positive attitude toward diabetes self-care. The majority 350 (94.34%) of the respondents reported that if there was a problem in my feet, I report to my health-care provider immediately, and regular self-care practice is important for diabetes patients 341 (91.9%). Furthermore, 317 (85.44%) of the participants thought that self-care practice is as effective as medication for their condition if followed, while about 293 (79.0%) of the participants agreed that support from family and friends is important in diabetes self-care practice (Table 3).
 |
Table 3 Attitude Towards Self-care Practice Among T2DM Patients on Follow-up at JMC, 2019 (n=371) |
Self-care Practice Toward Diabetes
The mean ±SD of self-care practice score for the participants was 5.23±1.76 (range: 1–10). More than half, 201 (54.2%) of the study participants had good self-care practice. Self-care practices that were best followed were adherence to no smoking, 328 (88.4%), adherence to medication, 305 (82.21%), and adherence to no alcohol intake 253 (68.20%). Among the self-care practices, it was seen that adherence for testing of blood glucose, 40 (10.8%) was not followed by the majority of the study participants (Table 4).
 |
Table 4 Frequency Distribution of Self-care Practice Among T2DM Patients on Follow-up at JMC, 2019 (n=371) |
Predictors of Knowledge, Attitude and Self-care Practice Among the Study Participants
Table 5 shows results of the binary and multinomial regression analysis of factors associated with knowledge of diabetes. The analysis showed significant association of patients’ knowledge with residence and educational level (p<0.05). There were no significant association of patients’ knowledge with sex, age, religion, marital status, monthly income, and other clinical status of the patients (p>0.05). High level of knowledge of diabetes self-care was the reference group. Respondents who are at primary education level (adjusted odd ratio, AOR=1.89, 95%CI: 1.02–3.52) were more likely to have poor knowledge than those with tertiary education. Urban residents were 43% (AOR=0.57, 95%CI: 0.36–0.91) more likely to have a good knowledge when compared to rural residents.
 |
Table 5 Multinomial Logistic Regression Analyses Findings of Factors Associated with Knowledge on Diabetes Self-care Among T2DM Patients on Follow-up at JMC, 2019 (n=371) |
Results from multiple logistic regressions for attitude showed that illiterate participants were 2.3 times (AOR=2.3; 95%CI: 1.181–4.501) more likely to have a negative attitude than participants with a higher educational level. Income was a factor that negatively affected attitude toward diabetes. Participants with monthly income less than 1000 ETB were 2.7 times (AOR=2.723, 95%CI: 1.443–5.137) and 1000–3000 ETB were 1.13 times (AOR=1.126, 95%CI: 0.623–2.034) more likely to have a negative attitude compared to those earned more than 3000 ETB. Participants having other comorbidities were 0.6 times (AOR=0.602, 95%CI: 0.372–0.974) less likely to have a negative attitude towards diabetes self-care compared to those with no comorbidities. In terms of duration of DM, participants with duration of less than five years were 2.24 times (AOR=2.242, 95%CI: 1.188–4.231) more likely to have a negative attitude than those with a duration of more than 10 years (Table 6).
 |
Table 6 Multinomial Logistic Regression Analyses Findings of Factors Associated with Attitude Toward Diabetes Self-care Among T2DM Patients on Follow-up at JMC, 2019 (n=371) |
Male patients were 80.2% (AOR=0.198, 95%CI: 0.115–0.344) more likely to have a good self-care practice when compared to female patients. On the contrary, patients in the age range of 41–50 were 2.3 times (AOR=2.256, 95%CI: 1.115, 4.563), and 51–60 were 2.7 times (AOR=2.677, 95%CI: 1.105–6.481) less likely to have good self-care practice. Similarly, illiterate patients were 4.4 times (AOR=4.372, 95%CI: 1.988–9.616), and patients with primary level education were 4.5 (AOR=4.514, 0.95%CI: 2.196–9.276) more likely to have poor self-care practice when compared to patients attending tertiary education level. With regard to monthly income, patients who earned less 1000 ETB were prone to poor self-care practice (AOR=4.229, 95%CI: 2.061–8.675) compared to patients earned more than 3000 ETB (Table 7).
 |
Table 7 Multinomial Logistic Regression Analyses Findings of Factors Associated with Self-care Practice Among T2DM Patients on Follow-up at JMC, 2019 (n=371) |
Discussion
In this study, 63.3% of patients had good knowledge about diabetes self-care. This finding was higher than the study done in India (24.3%),22 Nepal (12.3%),19 Jordan (53.3%),23 Egypt 52.3%,24 and Malaysia (41.9),25 and almost similar to studies done in Oman (61.4%)26 and Iran (61.41%).20 The discrepancy may be attributed to the difference in the study population. In our study, the participants were hospital-based and they have better health education access. When we compare patients at primary level of education with those who attained tertiary education level, a significant difference in knowledge level of diabetes self-care was observed. A cross-sectional study in Bangkok and other central provinces of Thailand showed educational and age level brought diabetes knowledge differences.27 This may not be amazing as knowledge is achieved through education. Patients from urban areas had a good knowledge level of diabetes self-care compared to patients from rural areas. The result was in line with study done in Ayder comprehensive specialized hospital, North Ethiopia.12 Higher level knowledge of urban residents could be due to the reality that urban residents are more likely to have access to information regarding the disease through mass media, books, and the internet.
This study showed that 59.6% of patients had a positive attitude toward diabetes self-care practices. This finding was higher compared to other studies done in Debre Tabor town, Northwest Ethiopia (39.5%),21 Bangladesh (18%),28 Kenya (48%),29 and India (17.6%).30 This might be due to study setting differences; studies done in Kenya and India were from rural areas, but our study enrolled both urban and rural residents and they have better access to a health education that leads to attitude change toward diabetes self-care practices. On the contrary, the finding was lower when compared with studies done in Ayder comprehensive specialized hospital, North Ethiopia (70.4%)12 and Adama, Ethiopia (81.9%).31 The variation might be due to the use of different data collection tools and difference in the study population. Positive attitude towards diabetes self-care was high in patients who earned a higher monthly income than their counterparts. The finding was consistent with the study conducted in Bale, Ethiopia.32 This might be because of having a higher monthly income will help to access and afford necessary information related to diabetes that resulted in behavioral change among the patients. Patients having other comorbidities had a better attitude than those with no comorbidity. This might be because of Patients with other comorbidities had repetitive communication with health-care providers. Furthermore, taking insulin injection alone, being diabetic for less than five years and being illiterate were associated with a negative attitude toward diabetes self-care. This is because patients taking insulin injection alone may have a negative attitude due to injection associated pain and patients with low academic status have low awareness about diabetes self-care.
More than half (54.2%) of the participants had good self-care practice. Self-care practice reported in this study is consistent with studies done in Benishangul Gumuz Regional State Public Hospitals, Western Ethiopia (54.3%),15 Hadiya Zone health institutions, Southern Ethiopia (52.3%),33 Harari, Eastern Ethiopia (50.9%),34 and Iran (52.23%).20 However, it is higher than studies conducted in Bahir Dar, Northwest Ethiopia (28.4%)35 and Egypt (37%).36 The possible reasons for this difference could be the difference in the sources of information, sociocultural variation, inadequate health education toward self-care practice and educational level of the study participants. In the present study, those who were illiterate and at aprimary educational level were more likely to have poor self-care practice than those who attained tertiary educational level. This finding is similar to the result of previous studies in Benishangul Gumuz Regional State Public Hospitals, Western Ethiopia15 and Harari,34 and indicates how education and its application are crucial for diabetic management.37 Earning a monthly income less than 1000 ETB was associated with poor self-care practice. This finding was consistent with study conducted in Debre Tabor town, Northwest Ethiopia.21 This might be explained patients who had low income cannot have sustained lifestyle modification or behavioral change and lack of resources could be a barrier for self-care practice. Patients aged 41–60 years were more likely to have poor self-care practice than patients older than 60 years. This suggests that as age increase, individuals become conscious and aware of their health and adjust their lifestyle. However, being male was found to be protective against poor self-care practice. The possible reason for this may be that relatively higher percentages of males (64.68%) were knowledgeable and their knowledge resulted in good self-care practice.
Limitation of the Study
The study was carried out in a hospital setting at a single place (JMC), so it may be difficult to generalize to the entire country. In addition, the findings are based on self-reported data from participants which limits the validity of the data.
Conclusion
The findings of this study showed that the level of knowledge, attitude and practice toward diabetes self-care among T2DM patients were found to be optimal. Factors associated with good knowledge of diabetes self-care were living in urban and attaining tertiary education level. Earning higher monthly income and presence of other comorbidities were associated with positive attitude toward diabetes self-care. Being male was associated with good self-care practice. This study identified the existence of knowledge level difference between urban and rural residents. It also indicated self-care practice difference between male and female patients. Clinicians should pay great attention for these affected groups in order to empower them to diabetes self-care.
Abbreviations
AOR, adjusted odds ratio; COR, crude odds ratio; DM, diabetes mellitus; IDF, International Diabetes Federation; IRB, Institutional Review Board; JMC, Jimma Medical center; KAP, knowledge, attitude, practice; SPSS, Statistical Program for the Social Sciences; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
Ethics Approval and Consent to Participate
The study was approved by Institutional Review Board (IRB) of Jimma University on January 17, 2019. The principal investigator and data collectors briefed the aim of the study to the patients and signed informed consent was taken from all participants. During data collection, confidentiality was ensured and for this reason, name and address of the patient was not recorded in the data collection check list. The study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
We are grateful to Jimma University for funding this research through SRS. We are also thankful for the staff of JMC for their cooperation in collecting the data and the patients who willingly participated in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Faten MRI, Neime A. Diabetic patients knowledge, attitude and practice toward oral health. JEP. 2013;4(20):19–25.
2. Diabetes CJ. Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome [Internet]; 2018. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29650080.
3. Tripathi BK, Srivastava AK. Diabetes mellitus: complications and therapeutics. Med Sci Monit. 2006;12(7):RA130–47.
4. Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus-present and future perspectives. Nat Rev Endocrinol. 2011;8(4):228–236. doi:10.1038/nrendo.2011.183
5. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi:10.2337/diacare.27.1047
6. International diabetes federation. IDF Diabetes Atlas.
7. International diabetes federation. IDF Diabetes Atlas.
8. International diabetes federation. IDF Diabetes Atlas.
9. Raithatha SJ, Shankar SU, Dinesh K. Self-care practices among diabetic patients in Anand district of Gujarat. ISRN Family Med. 2014;2014:1–6. doi:10.1155/2014/743791
10. Okonta HI, Ikombele JB, Ogunbanjo GA. Knowledge, attitude and practice regarding lifestyle modification in type 2 diabetic patients. Afr J Prim Health Care Fam Med. 2014;6(1):2–7. doi:10.4102/phcfm.v6i1.655
11. Heisler M, Piette JD, Spencer M, Kiefer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care. 2005;28(4):816–822. doi:10.2337/diacare.28.4.816
12. Niguse H, Belay G, Fisseha G, Desale T, Gebremedhn G. Self-care related knowledge, attitude, practice and associated factors among patients with diabetes in ayder comprehensive specialized hospital, North Ethiopia. BMC Res Notes. 2019;12(1). doi:10.1186/s13104-019-4072-z
13. Asmare G, Biftu G, Tadesse A, Agenehu B, Zeleke A, Biresaw W. Self- care practices and associated factors among adult diabetic patients in public hospitals of Dire Dawa administration, Eastern Ethiopia. BMC Public Health. 2020;20(1):1232. doi:10.1186/s12889-020-09338-5
14. Andualem Y, Mezgebu Y, Amare M, Telake A. Self-care practice and associated factors among patients with diabetes mellitus on follow up at university of gondar referral hospital, Gondar, Northwest Ethiopia. BMC Res Notes. 2019;12(591). doi:10.1186/s13104-019-4630-4
15. Segni W, Mohammed H, Addisu T. self-care practice and associated factors among diabetes mellitus patients on follow up in benishangul gumuz regional state public hospitals, western Ethiopia: a cross-sectional study. BMC Res Notes. 2018;11(1):833. doi:10.1186/s13104-018-3939-8
16. Melat M, Meaza D. Self care practice and its associated factors among diabetic patients in Addis Ababa public hospitals: across sectional study. J Diabetes Metab. 2016;7(6). doi:10.4172/2155-6156.C1.046
17. Tesfaye M, Ebrahim M, Taklo S, Kefale B. Predictors of diabetes self-care practice among patients with type 2 diabetes in public hospitals in northeastern Ethiopia: a facility-based cross-sectional study. Diabetes Metab Syndr Obes. 2020;13:3137–3147. doi:10.2147/DMSO.S273682
18. Tefera K, Hailay G, Lillian M, Tesfahun E. Diabetes related knowledge, self-care behaviours and adherence to medications among diabetic patients in Southwest Ethiopia: a cross-sectional survey. BMC Endocr Disord. 2016;16(1):28. doi:10.1186/s12902-016-0114-x
19. Gautam A, Bhatta DN, Aryal UR. Diabetes related health knowledge, attitude and practice among diabetic patients in Nepal. BMC Endocr Disord. 2015;15(1). doi:10.1186/s12902-015-0021-6
20. Niroomand M, Ghasemi SN, Karimi-Sari H, Kazempour-Ardebili S, Amiri P, Khosravi MH. Diabetes knowledge, attitude and practice (KAP) study among Iranian in-patients with type-2 diabetes: a cross-sectional study. Diabetes Metab Syndr. 2015;10(1):114–119. doi:10.1016/j.dsx.2015.10.006
21. Asmamaw A, Asres G, Negese D, Fekadu A. Knowledge and attitude about diabetes mellitus and its associated factors among people in DebreTabor Town, Northwest Ethiopia: cross sectional study. Sci J Public Health. 2015;3(2):199–209. doi:10.11648/j.sjph.20150302.17
22. Dinesh PV, Kulkarni AG, Gangadhar NK. Knowledge and self-care practices regarding diabetes among patients with type 2 diabetes in Rural Sullia, Karnataka: a community based cross-sectional study. J Family Med Prim Care. 2016;5(4):847–852. doi:10.4103/2249-4863.201176
23. Alsous M, Abdel Jalil M, Odeh M, Al Kurdi R, Alnan M, Bryner RW. Public knowledge, attitudes and practices toward diabetes mellitus: a cross sectional study from Jordan. PLoS One. 2019;14(3):e0214479. doi:10.1371/journal.pone.0214479
24. Khawaga GE, Wahab FA. Knowledge, attitudes, practice and compliance of diabetic patients in dakahlia, Egypt. Eur J Med Res. 2015;3(1).
25. Minhat HS, Hamedon TR. Understanding towards diabetes mellitus among rural adult community in Malaysia. World J Med Sci. 2014;11(2):217–221.
26. Bimani AL, Khan SA, David P. Evaluation of T2DM related knowledge, attitude and practices of Omani patients. Saudi Pharm J. 2015;23(1):22–27. doi:10.1016/J.JSPS.2013.12.006
27. Pongmesa T, Li SC, Wee HL. A comparison of diabetes knowledge among residents in Bangkok and other central provinces of Thailand. Value Health. 2008;11(6):A517. doi:10.1016/S1098-3015(10)66713-7
28. Islam M, Chakrabart R, Dirani M, et al. Knowledge, attitudes and practice of diabetes in rural Bangladesh: the Bangladesh population based diabetes and eye study. PLoS One. 2014;9(10):e110368. doi:10.1371/journal.pone.0110368
29. Maina K, Ndegwa Z, Njenga E, Muchemi E. Knowledge, attitude and practices related to diabetes among community members in four provinces in Kenya: a cross-sectional study. Pan Afr Med J. 2010;7(2).
30. Rathod GB, Rathod S, Parmar P, Parikh A. Study of knowledge, attitude and practice of general population of Waghodia towards diabetes mellitus. Int J Curr Res. 2014;6(1).
31. Adem AM, Gebremariam ET, Gelaw BK, Ahmed M, Fromsaseifu M, Thirumurugan DG. Assessment of knowledge, attitude and practices regarding life style modification among type 2 diabetic mellitus patients attending adama hospital medical college, Oromia Region, Ethiopia. Glob J Med Res. 2014;14(7):37–48.
32. Chanyalew W, Alemayehu G. Knowledge, attitude, practices and their associated factors towards diabetes mellitus among non diabetes community members of Bale Zone administrative towns, South East Ethiopia. A cross-sectional study. PLoS One. 2016;12(2):e0170040. doi:10.1371/journal.pone.0170040
33. Tesfaye FG, Yilima CD, Biruk WT. Predictors of diabetes self-care practice and associated factors among patient on follow up at Hadiya zone, health institutions southern Ethiopia, using health belief model, cross-sectional study design. EC Endocrinol Metab Res. 2019;4(10):1–17.
34. Ayele K, Tesfa B, Abebe L, Tilahun T, Girma E, Bacurau RFP. Self-care behaviour among patients with diabetes in Harari, Eastern Ethiopia: the health belief model perspective. PLoS One. 2012;7(4):e35515. doi:10.1371/journal.pone.0035515
35. Abate T, Tareke M, Tirfie M. Self-care practices and associated factors among diabetes patients attending the outpatient department in Bahir Dar, Northwest Ethiopia. BMC Res Notes. 2018;11(1):800. doi:10.1186/s13104-018-3874-8
36. Maged M, Alghazaly G, Alshora A. Knowledge, practice and barriers of foot self-care among diabetic patients at tanta university hospitals, Egypt. Egypt J Med. 2018;36(4).
37. Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12(14). doi:10.1186/2251-6581-12-14
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.