Back to Journals » Clinical Ophthalmology » Volume 16
Selection Criteria for Air Tamponade During Vitrectomy for Rhegmatogenous Retinal Detachment
Authors Nakamura M, Nishi K , Nishitsuka K
Received 25 January 2022
Accepted for publication 23 March 2022
Published 30 March 2022 Volume 2022:16 Pages 981—986
DOI https://doi.org/10.2147/OPTH.S359936
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Madoka Nakamura, Katsuhiro Nishi, Koichi Nishitsuka
Department of Ophthalmology and Visual Sciences, Yamagata University Faculty of Medicine, Yamagata, Japan
Correspondence: Koichi Nishitsuka, Department of Ophthalmology and Visual Sciences, Yamagata University Faculty of Medicine, Yamagata, Japan, Tel +81 23-628-5374, Fax + 81 23-528-5377, Email [email protected]
Purpose: To compare air tamponade and sulfur hexafluoride (SF6) gas tamponade during vitrectomy for the treatment of rhegmatogenous retinal detachment (RRD).
Methods: We reviewed 294 eyes with RRD treated with 25-gauge vitrectomy by a single surgeon between June 2011 and April 2018 retrospectively. The exclusion criteria for the proposed air tamponade selection were more than 2 weeks since onset, giant retinal tears, history of complications following cataract surgery, high myopia, and proliferative vitreoretinopathy classified as grade C or higher. We examined the differences in the therapeutic effect between the air group and SF6 group at 6-month follow-up.
Results: A total of 294 eyes were included in the study, 156 eyes in the air group and 138 eyes in the SF6 group. No difference was observed in the primary anatomical success rates between the air group (99.4%; 155/156 eyes) and the SF6 group (96.5%; 135/138 eyes; P = 0.102). Postoperative intraocular gas half-life was shorter in the air group (3.97 ± 0.87 days) compared with the that in the SF6 group (8.67 ± 1.47 days; P = 0.0001). The incidence of postoperative ocular hypertension was lower in the air group (19.9%; 31/156 eyes) than in the SF6 group (62.3% 86 /138 eyes; P = 0.0001).
Conclusion: We compared the criteria for proper selection between air and SF6 gas tamponade during vitrectomy for the treatment of RRD. Air tamponade was able to reduce the period of prone position and the risk of ocular hypertension without reducing the therapeutic effect.
Keywords: air tamponade, rhegmatogenous retinal detachment, sulfur hexafluoride gas tamponade, vitrectomy
Introduction
Rhegmatogenous retinal detachment (RRD) is a serious retinal disorder that can lead to blindness. The best treatment technique has been debated by ophthalmologists. Because RRD treatment had changed continuously, these changes need to be frequently evaluated. Several studies have reported an increase in the uses of pars plana vitrectomy (PPV) for treating eyes with RRD.1–4 The Japan Retinal Detachment Registry revealed that in 2016 and 2017, vitrectomy was employed for RRD treatment in 77.8% of cases.5,6
However, PPV for RRD treatment has some disadvantages, including limitations in its day-to-day use due to gas tamponade. Typically, long-acting gases (LAGs), such as sulfur hexafluoride (SF6) and octafluoropropane (C3F8), have been chosen for tamponade. However, several studies have demonstrated the effectiveness of room air tamponade for RRD treatment for reducing patient discomfort.7–10 Although air tamponade has advantages, such as early discharge, surgeons are sometimes hesitant to use it due to the lack of patient selection criteria.
In the European Vitreo-Retinal Society Retinal Detachment study, RRD was classified as complicated retinal detachment (RD) and uncomplicated RD according to the degree of severity.11–14 The choice of tamponade for RD should be individualized based on the location and characteristics of RD, expected patient compliance with postoperative positioning requirements, and other factors.15 We considered that it is easy for surgeons to select air tamponade for cases with RD that is relatively mildly severe. Moreover, we created an air tamponade selection criterion. The purpose of this study was to investigate the proper use of tamponade by comparing the effectiveness of both air tamponade and SF6 gas tamponade during vitrectomy for treating RRD in our proposed criteria.
Materials and Methods
Between June 2011 and April 2018, 907 RRD eyes were treated by a single surgeon at Yamagata University Hospital. Of these, 359 RRD eyes were treated with scleral buckling and 548 RRD eyes were treated with pars plana vitrectomy. In this study, relatively mildly severe RRD cases were defined as follows: less than 2 weeks since onset, no giant retinal tears, no history of complications following cataract surgery, no high myopia, and no proliferative vitreoretinopathy classified as grade C or higher. These were the inclusion criteria aimed at the proposed air tamponade selection. Of the 548 RRD eyes treated with vitrectomy, we conducted a retrospective analysis of 294 RRD eyes met this inclusion criteria. Figure 1 is shown the flow of patients through the study. Enrolled patients were divided into two groups: the air group comprised patients on whom air tamponade was used, and the SF6 group comprised patients on whom SF6 gas tamponade was used.
 |
Figure 1 Flow of patients through the study. Abbreviations: RRD, rhegmatogenous retinal detachment; SB, scleral buckling; PPV, pars plana vitrectomy. |
All patients were treated by hospitalization, and all work was approved by the institutional review board of Yamagata University Faculty of Medicine. The procedure conformed to the tenets of the Declaration of Helsinki. All data were fully anonymized before we accessed them, and the institutional review board waived the requirement for informed consent. Patients or the public were not involved in the design, or conduct, or reporting, or dissemination of our research.
The following variables were analyzed: sex, age, number of retinal breaks, location of retinal breaks, number of quadrants involved, presence or absence of macular detachment, lens status, time course changes in postoperative intraocular gas half-life, presence or absence of postoperative ocular hypertension by measuring intraocular pressure (IOP), primary anatomical success rate, and final anatomical success rate. Primary success was defined as having no additional surgery by 6 months. Final success was defined as the retina being repositioned at 6 months. The half-life was defined as the number of days until the gas interface reached the center of the optic disc in a fundus examination conducted daily. Postoperative IOP was measured every day during the hospital stay. Postoperative ocular hypertension was defined as an IOP of ≥22 mmHg. Lower breaks were defined as retinal breaks located between four and eight o’clock in the detached retina.
Surgical Procedure
Retrobulbar anesthesia was administered using 6 mL of mixed 2% lidocaine and 0.5% levobupivacaine. We used the 25GPPV wide-angle noncontact viewing system (Resight®; Carl Zeiss Meditec AG, Jena, Germany) with the Constellation Vision System (Alcon Laboratories, Inc., Fort Worth, TX, USA) or EVA vitrectomy system (DORC, Zuidland, The Netherlands). We created three cannulas with conjunctival displacement and oblique-angled sclerotomies in the inferotemporal, superotemporal, and superonasal quadrants 3.0 to 4.0 mm posterior to the limbus. Before vitrectomy, all phakic eyes underwent phacoemulsification and intraocular lens implantation (PEA + IOL) with sclerocorneal incision using the same machine. After core vitrectomy, vitreous gel was visualized with an injection of triamcinolone acetonide (MaQaid, Wakamoto Pharmaceutical, Tokyo, Japan) during mid peripheral vitrectomy. The peripheral vitreous gel was then carefully shaved for 360° with scleral indentation. Peripheral vitreous shaving was performed up to the vitreoretinal angle formed by the retina and peripheral posterior vitreous detachment near the vitreous base.16–18 In all the cases, internal drainage of subretinal fluid was performed through a pre-existing retinal break. Internal drainage retinotomy was not performed. All RDs were restored intraoperatively. To completely surround all retinal breaks, we applied retinal photocoagulation. At the end of the surgery, the eyes of the SF6 group were flushed with prepared 50-mL nonexpansile 18% SF6 gas syringe to ensure complete exchange. All sclerotomy sites were closed with 8–0 Vicryl suture to prevent postoperative hypotony. All patients were treated by hospitalization and had a daily fundus examination after the surgery. We encouraged all patients to assume a prone position following surgery and to remain prone until the intraocular gas concentration was reduced in half. Subsequently, all patients were permitted to assume any position, except for the supine position, until the intraocular gas disappeared.
Statistical Analyses
We used Fisher’s exact test and Mann–Whitney U-test for the statistical analysis. Statistical significance was set at P <0.05 for all analyses. Analyses were conducted using PASW Statistics 18 (SPSS Inc., Chicago, IL, USA).
Results
A total of 294 eyes were included in the study, 156 eyes from the air group and 138 eyes from the SF6 group. The patient characteristics are presented Table 1. There were 51 women in the air group and 37 women in the SF6 group (P = 0.308). The mean ± standard deviation (SD) age was 61.3 ± 8.1 years in the air group and 63.6 ± 9.8 years in the SF6 group (P = 0.0114). The mean ± SD number of retinal breaks was 1.6 ± 1.0 in the air group and 1.7 ± 1.0 in the SF6 group (P = 0.1615). A total of 29 eyes (18.6%) in the air group and 45 eyes (32.6%) in the SF6 group involved lower breaks (P = 0.007). The mean ± SD quadrant of RD was 1.6 ± 0.6 in the air group and 1.9 ± 0.8 in the SF6 group (P = 0.00076). A total of 57 eyes (36.5%) in the air group and 75 eyes (54.3%) in the SF6 group involved macular detachment (P = 0.0023). There were 137 phakic eyes (87.8%) in the air group and 95 phakic eyes (68.8%) in the SF6 group (P = 0.0001). The primary success rates were similar between the air group (99.4%; 155/156 eyes) and SF6 group (96.5%; 135/138 eyes; P = 0.102). The postoperative intraocular gas half-life was shorter in the air group (3.97 ± 0.87 days) than in the SF6 group (8.67 ± 1.47 days; P = 0.0001). The incidence of postoperative ocular hypertension was lower in the air group (19.9%; 31/156 eyes) than in the SF6 group (62.3%; 86/138 eyes). Table 2 shows the primary success rate depending on the location of the break, lens status and quadrant of RD. No difference was observed in the primary success rate between the air group and the SF6 group depending on the location of the break, lens status, and quadrant of RD. Figure 2 presents the distribution of intraocular gas half-life in both the air group and SF6 group. The median half-life was 4 days in the air group and 7 days in the SF6 group. The final success rates were 100% in both the air group and SF6 group.
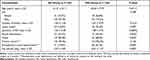 |
Table 1 Patient Characteristics and Results |
 |
Table 2 Primary Success Rate Depending on the Location of the Break, Lens Status and Quadrant of RD |
 |
Figure 2 Distribution of postoperative intraocular gas half-life (day) following vitrectomy for RRD between the air group and sulfur hexafluoride (SF6) group. |
Discussion
In the tamponade selection for general RD, LAGs, including SF6/C3F8 and silicone oil, are commonly chosen for severe cases and inferior break.15 Advances in vitreous surgery have resulted in attempts to select air tamponade over LAG for repositioning the retina as well as alleviating patient discomfort.7–10 In 2013, Tan et al7 reported the effectiveness of air tamponade for upper retinal breaks, and in 2015, Zhou et al8 demonstrated the effectiveness of air tamponade for lower retinal breaks. However, the primary anatomical success rate in these studies ranged from 78% to 85%,7,8 and it seems that the subjects included in the study were severe cases with some serious factors.
In this study, we focused on patients with RD that is relatively mildly severe. Moreover, we retrospectively validated the use of air tamponade selection criteria. We believe that the selection criteria, which were found to be successful in this study, could easily be used in routine RD treatment. In addition, one of the advantages of this study was the verified number of cases, which was more than twice the number included in recent reports of air tamponade.9,10 In the air tamponade selection criteria proposed in this study, including less than 2 weeks since onset, no giant retinal tears, no history of complications of cataract surgery, no high myopia, and no proliferative vitreoretinopathy classified as grade C or higher, air tamponade and SF6 gas tamponade had the same therapeutic effects. Recent studies of good therapeutic outcomes reported primary anatomical success rates of 94.3% to 94.4%,9,10 but the air selection criteria might have included more severe cases of RD, as compared with our criteria. In addition, because the treatment in our study was performed during hospitalization, it is possible that the patients’ ability to maintain a rest level was more advantageous than with 1-day surgery. Taking all these factors into consideration, future studies should review the selection criteria for air tamponade.
In this study, we were able to verify in detail that elevated IOP is a complication of air tamponade or SF6 gas tamponade. Generally, it is believed that tamponade with room air has a lower probability of increased IOP compared with LAGs, such as SF6 and C3F8.19 This study also revealed that the incidence of postoperative ocular hypertension was lower in the air group. Although LAG is advantageous for the treatment of RRD due to long-term filling in the eye, we demonstrated once again that it was disadvantageous to the air tamponade for increasing IOP. Postoperative ocular hypertension was observed not only the day after surgery but also several days after (data not shown). Because IOP was measured daily, we could collect the details of the occurrence of IOP. Ocular hypertension was transitory and treated only with anti-glaucoma eye drops. It is an important clinical point to note that in this study, the use of tamponade in the eye caused an increase in IOP of about 20% in air and about 60% in SF6. The results of this study indicate that the risk of increased IOP can be greatly reduced by selecting air.
The half-life of the tamponade was about 4 days in the air and approximately 8 days for the SF6 gas. Thompson et al19 reported an air half-life of 1.6 days and SF6 half-life of 2.8 days, which is shorter than the values reported in our results. Our results suggest that the half-life of air and SF6 was long because vitreous shaving was performed as much as possible and the three ports were sutured in all cases to prevent eye collapse. The results of longer half-life of air and SF6 may also be due to the fact that all the eyes in this study had phacoemulsification of the lens; therefore lens removal increased the volume of space to hold the air or gas. In this study, regardless of the location of the retinal breaks or the state of RD, the patients maintained the prone position until the intraocular gas concentration was reduced in half by the uniform half-life. In addition, the nurse continually checked the patient’s position during hospitalization. Based on the criteria of this study, the therapeutic effect is sufficient when the prone position is continued for about 4 days. Even if the patient does not know whether he or she can properly maintain a prone position during surgery, it is necessary to verify whether the air tamponade is effective. In addition, we hope that attempts will be made to shorten the period of prone position.20,21
This study has several limitations. Pneumatic retinopexy is rarely performed in Japan, and we could not obtain data on it. Due to the retrospective nature of the present study, some items, including the location of the retinal break, quadrants of RD, lens status, and macular status, differed between the air group and the SF6 group. Future prospective studies based on the results of the present research should provide further validation of the effectiveness of the air tamponade.
In summary, we proposed the criteria for properly selecting between air tamponade or SF6 gas tamponade during vitrectomy for the treatment of RRD. We found no differences in the therapeutic effect exhibited by air tamponade and SF6 gas tamponade based on the proposed selection criteria for air tamponade. Furthermore, the incidence of elevated IOP was lower with air tamponade than with SF6 gas tamponade. Future prospective studies should be conducted to verify the therapeutic effect of air tamponade.
Acknowledgments
This work was supported by JSPS KAKENHI (grant JP25462704). Meeting presentation: American Academy of Ophthalmology, 2019.
Funding
There is no funding to report.
Disclosure
Koichi Nishitsuka reports personal fees from Santen, HOYA, Alcon, NOVARTIS, SENJU, KOWA, and Otsuka, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Ho JD, Liou SW, Tsai CY, Tsai RJ, Lin HC. Trends and outcomes of treatment for primary rhegmatogenous retinal detachment: a 9-year nationwide population-based study. Eye. 2009;23(3):669–675. doi:10.1038/sj.eye.6703105
2. Wong CW, Wong WL, Yeo IY, et al. Trends and factors related to outcomes for primary rhegmatogenous retinal detachment surgery in a large asian tertiary eye center. Retina. 2014;34(4):684–692. doi:10.1097/IAE.0b013e3182a48900
3. Smretschnig E, Falkner-Radler CI, Sporl J, Kivaranovic D, Binder S, Krepler K. Primary retinal detachment surgery: changes in treatment and outcome in an Austrian tertiary eye center. Ophthalmologica. 2017;237(1):55–62. doi:10.1159/000454889
4. Reeves MG, Pershing S, Afshar AR. Choice of primary rhegmatogenous retinal detachment repair method in US commercially insured and medicare advantage patients, 2003–2016. Am J Ophthalmol. 2018;196:82–90. doi:10.1016/j.ajo.2018.08.024
5. Sakamoto T, Kawano S, Kawasaki R, et al. Japan-Retinal Detachment Registry Report I: preoperative findings in eyes with primary retinal detachment. Jpn J Ophthalmol. 2020;64(1):1–12. doi:10.1007/s10384-019-00702-6
6. Nishitsuka K, Kawasaki R, Yamakiri K, et al. Preoperative factors to select vitrectomy or scleral buckling for retinal detachment in microincision vitrectomy era. Graefes Arch Clin Exp Ophthalmol. 2020;258(9):1871–1880. doi:10.1007/s00417-020-04744-2
7. Tan HS, Oberstein SY, Mura M, Bijl HM. Air versus gas tamponade in retinal detachment surgery. Br J Ophthalmol. 2013;97(1):80–82. doi:10.1136/bjophthalmol-2012-302140
8. Zhou C, Qiu Q, Zheng Z. Air versus gas tamponade in rhegmatogenous retinal detachment with inferior breaks after 23-gauge pars plana vitrectomy: a prospective, randomized comparative interventional study. Retina. 2015;35(5):886–891. doi:10.1097/IAE.0000000000000416
9. Pak KY, Lee SJ, Kwon HJ, Park SW, Byon IS, Lee JE. Exclusive use of air as gas tamponade in rhegmatogenous retinal detachment. J Ophthalmol. 2017;2017. doi:10.1155/2017/1341948.
10. Tetsumoto A, Imai H, Hayashida M, et al. The comparison of the surgical outcome of 27-gauge pars plana vitrectomy for primary rhegmatogenous retinal detachment between air and SF6 gas tamponade. Eye (Lond). 2020;34(2):299–306. doi:10.1038/s41433-019-0726-2
11. Adelman RA, Parnes AJ, Ducournau D; European Vitreo-Retinal Society Retinal Detachment Study Group. Strategy for the management of uncomplicated retinal detachments: the European vitreo-retinal society retinal detachment study report 1. Ophthalmology. 2013;120(9):1804–1808. doi:10.1016/j.ophtha.2013.01.070
12. Adelman RA, Parnes AJ, Sipperley JO, Ducournau D; European Vitreo-Retinal Society Retinal Detachment Study Group. Strategy for the management of complex retinal detachments: the European vitreo-retinal society retinal detachment study report 2. Ophthalmology. 2013;120(9):1809–1813. doi:10.1016/j.ophtha.2013.01.056
13. Michalewska Z, Ducournau D, Adelman RA. How do vitrectomy parameters influence the results of rhegmatogenous retinal detachments repair? EVRS RD Study No. 3. Acta Ophthalmol. 2014;92(5):e416–e417. doi:10.1111/aos.12318
14. Adelman RA, Parnes AJ, Michalewska Z, Ducournau D; European Vitreo-Retinal Society Retinal Detachment Study Group. Clinical variables associated with failure of retinal detachment repair: the European vitreo-retinal society retinal detachment study report number 4. Ophthalmology. 2014;121(9):1715–1719. doi:10.1016/j.ophtha.2014.03.012
15. Vaziri K, Schwartz SG, Kishor KS, Flynn HW. Tamponade in the surgical management of retinal detachment. Clin Ophthalmol. 2016;10:471–476. doi:10.2147/OPTH.S98529
16. Nishitsuka K, Nishi K, Namba H, Kaneko Y, Yamashita H. Intraoperative optical coherence tomography imaging of the peripheral vitreous and retina. Retina. 2018;38(3):e20–e22. doi:10.1097/IAE.0000000000001979
17. Nishitsuka K, Nishi K, Namba H, Kaneko Y, Yamashita H. Quantification of the peripheral vitreous after vitreous shaving using intraoperative optical coherence tomography. BMJ Open Ophthalmol. 2021;6(1):e000605. doi:10.1136/bmjophth-2020-000605
18. Nishitsuka K, Nakamura M, Nishi K, Namba H, Kaneko Y, Yamashita H. Surgical outcomes of rhegmatogenous retinal detachment with different peripheral vitreous-shaving procedures. Clin Ophthalmol. 2021;15:2197–2202. doi:10.2147/OPTH.S310789
19. Thompson JT. Kinetics of intraocular gases. Disappearance of air, sulfur hexafluoride, and perfluoropropane after pars plana vitrectomy. Arch Ophthalmol. 1989;107(5):687–691. doi:10.1001/archopht.1989.01070010705031
20. Xia S, Zhao XY, Wang EQ, Chen YX. Comparison of face-down posturing with nonsupine posturing after macular hole surgery: a meta-analysis. BMC Ophthalmol. 2019;19(1):34. doi:10.1186/s12886-019-1047-8
21. Shiraki N, Sakimoto S, Sakaguchi H, Nishida K, Nishida K, Kamei M. Vitrectomy without prone positioning for rhegmatogenous retinal detachments in eyes with inferior retinal breaks. PLoS One. 2018;13(1):e0191531. doi:10.1371/journal.pone.0191531
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
