Back to Journals » Patient Preference and Adherence » Volume 14
Satisfaction of Pregnant Women with Antenatal Care Services at Women and Children Hospital in South Okkalapa, Myanmar: A Facility-Based Cross-Sectional Study Triangulated with Qualitative Study
Authors Hsai NM, Matsui M , Ng CFS, Khaing CT, Imoto A , Sayed AM, Huy NT , Kamiya Y, Moji K
Received 12 June 2020
Accepted for publication 23 October 2020
Published 18 December 2020 Volume 2020:14 Pages 2489—2499
DOI https://doi.org/10.2147/PPA.S266916
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Nang Mon Hsai,1,2 Mitsuaki Matsui,1 Chris Fook Sheng Ng,1 Cho Thet Khaing,3 Atsuko Imoto,1 Ahmed M Sayed,4,5 Nguyen Tien Huy,1 Yasuhiko Kamiya,1 Kazuhiko Moji1
1School of Tropical Medicine and Global Health, Nagasaki University, Nagasaki 852-8523, Japan; 2Social Security Board, Ministry of Labour, Immigration and Population, Nay Pyi Taw, Myanmar; 3Department of Epidemiology, University of Public Health, Yangon, Myanmar; 4School of Pharmacy, Al-Azhar University, Cairo, Egypt; 5Online Research Club, Nagasaki 852-8523, Japan
Correspondence: Kazuhiko Moji; Nguyen Tien Huy
Graduate School of Tropical Medicine and Global Health, Nagasaki University, Nagasaki, Japan
Email [email protected]; [email protected]
Background: While patients’ satisfaction is a barometer for healthcare quality, Myanmar did not do enough to assess the antenatal care (ANC) satisfaction.
Objective: In this study, we aim to assess the satisfaction level of pregnant women with ANC services provided by a public hospital in Myanmar.
Methods: A cross-sectional study was conducted with 125 women in the quantitative and 27 in the qualitative study at South Okkalapa Women and Children Hospital in Myanmar. Satisfaction was measured by using a five-point Likert scale with 25-item services. Statistical software SPSS version 16 was used for quantitative data analysis. Qualitative data were manually analyzed by thematic analysis.
Results: The proportion of pregnant women who were satisfied with healthcare services ranged from 18% to 35%. Provider’s service yielded satisfaction ranging between 25% and 35%; meanwhile, facilities in the waiting area had the lowest mean score (2.78) for satisfaction. Laboratory service and waiting time at the antenatal clinic were major sources of dissatisfaction. Overall, 48% of the pregnant women were in high satisfaction with ANC services. Out of 25 items, cleanliness of ANC clinic, the process of ANC procedure, drug supply by the hospital, ventilation, and lighting in the waiting area, waiting time to see doctors, and working hours (availability of services) showed significant association with overall satisfaction.
Conclusion: Nearly half of the pregnant women in the study were very satisfied with the total healthcare services they received. Facilities in the waiting area, laboratory service, and waiting time to see doctors were dissatisfied services and need to be upgraded.
Keywords: antenatal care, satisfaction, dissatisfaction, antenatal services, pregnant women
Background
The world is losing almost 800 women every single day due to pregnancy-related complications, with the highest rate in the low- and middle-income countries (LMICs).1 Using the proper antenatal care before, during, and after delivery has shown improvement in the pregnancy outcomes and diminishes the number of unnecessary mortalities.2 As long as antenatal care (ANC) is considered necessary support for the mother and fetus, the risks of pregnant-comorbidities or mortalities will come to an end. The justification is that ANC is a primary barometer for maternal mortality and a necessary component of maternal healthcare especially in developing nations.3
While more than 200 million women become pregnant every year, about 15% of them encountered problems that are preventable by proper obstetric care.4 Previously, WHO recommended four ANC visits – as a minimum – for one pregnancy to assure an optimal birth outcome and to reduce maternal risks, especially for developing countries.5 Globally, 85% of the pregnant women can access ANC services in addition to a skilled birth at least once. In contrast, only 58% get the WHO recommended minimum requirement of four ANC visits.6 In Sub-Saharan African and South Asian countries, the highest rate of maternal mortality ratio (MMR), they have low antenatal coverage, which is about 49% and 42% for four visits, respectively. In 2016, the WHO introduced a new model for ANC visits in which every pregnant woman should have at least eight contacts for one pregnancy, in addition to, the initial contact that begins during the first trimester of pregnancy.5
Antenatal care is an admission point for a mother to get access to medical services like monitoring of the fetal condition, prevention of anaemia, deworming, vaccinations such as tetanus, and screening for sexually transmitted infections (HIV and syphilis). These screenings lead to early diagnosis of any potential complications.7 By receiving proper care, pregnant women can increase their awareness of signs and symptoms of pregnancy-related complications and prepare their bodies for safe delivery.
MMR in Myanmar improved to 130/100,000 live births in 2015, while the infant mortality rate was 26.6/1000 live births in 2011. This may be due to the national coverage of ANC and delivery care in Myanmar that has improved during these years.8 The ANC coverage had risen from 63.1% in 2005 to be 86.1% in 2016. According to Myanmar Demographic Health Survey 2015–16; 81% of the pregnant women received ANC from a skilled provider at least once, also, 59% of the women had four or more ANC visits.9 Unfortunately, about 1300 women died due to pregnancy-related complications among the average 1–1.2 million deliveries (DOH, 2010). MMR is still high compared to other LMICs. Thirty-four percent of total births were taking place at home provided by SBA. Although ANC coverage has been increasing during these years, there has been inadequate and late initiation of ANC.
For the last two decades, the increased awareness of women using healthcare services has increased the need for healthcare service delivery in public health. Ultimately, patients’ satisfaction is used as an indicator of medical care quality, which is a considerable factor in the service assessment. Interpersonal relationship with care providers and their efficiency also improves patient satisfaction.10 Comfort to care resulted in patients’ compliance (to follow advice from health professionals, adhere to treatment regimens, and remain in a coordinated system of care). which leads to good maternal and fetal outcomes. Patients’ recognition was considered for improvement of health outcomes, continuity of care, compliance to treatment, and courtesy care of providers.11 The feature of the healthcare facility can be relatively assessed by measuring the level of patients’ acceptance.12 Thus, our research question is to analyze the satisfaction level of pregnant women with antenatal care services provided by one of the public hospitals located in the suburban area of Myanmar and to identify which services were satisfied by the pregnant women.
Methods
Study Design
A facility-based cross-sectional study was conducted in the ANC clinic of South Okkalapa Women and Children Hospital in Yangon, Myanmar. A quantitative and qualitative mixed method of sequential explanatory design was applied.13 This study was conducted from October to December 2017. The development of our questionnaire was formed in three cycles; the first cycle was to form the questionnaire according to the PSQ-18.14 Nevertheless, we edited the questionnaire to be more convenient and easier for the patients. Therefore, points related to the doctors’ service, time to wait, cost, and quality of care, accessibility are the same as the PSQ. While points like registration, ultrasound and laboratory services, drug supply, facilities in the antenatal clinic, privacy with confidentiality, and nurses’ services are different from the PSQ. Then, the first author and the ethical team translated the manuscript for the local language. The third cycle included a pre-test for the questionnaire and its questions to ensure the simplicity and palatability of the questionnaire to have the last version (Supplementary 1). Internal consistency (Cronbach’s alpha) for the study was 0.9.
Sample Size
The sample size for the quantitative study was calculated based on a single population proportion formula by assuming a prevalence of satisfaction among pregnant women attending the antenatal clinic of SOWCH with quality of ANC service was assumed as 60% with a marginal error of 10% between sample and population at 95% confident interval:
The following formula was applied in calculating the sample size:
n=z2 p (1-p)/d2 =95
n=required minimum sample size
z=number of standard errors from the mean (for 95% confidence level, z=1.96)
p=prevalence of satisfaction (60%)
d=precision (10%)
The required minimum sample size was 95 pregnant women. In the study, 125 respondents out of 140 were analyzed because of withdrawal.
For the qualitative study, four focus group discussions (FGDs) were conducted and a total of 27 pregnant women with 6–8 women in each group participated. A convenience sampling technique was employed to select the participants for FGDs.
Recruitment Method
Our sample was chosen from the daily registers at the ANC clinic, where their participants were randomly selected. A simple random sampling technique was used to draw a sample population. Participants for FGDs were selected through the time we made the study and after their acceptance. A convenience sampling technique is implemented in our investigation.
Variables and Method of Data Collection
The questionnaire consisted of 47 items that were related to the obstetric profile of pregnant women, their perception of ANC services, and satisfaction with services of the hospital and socio-demographic characteristics. Service satisfaction was measured by the 25-items instrument which had a high internal consistency (Cronbach’s alpha 0.93). Outcome variable satisfaction was measured by using a five-point Likert scale (totally satisfied: 4 marks, satisfied: 3 marks, neutral–do not know: 2 marks, dissatisfied-somewhat dissatisfied: 1 mark, strongly dissatisfied: 0 marks).
The women were classified into two levels of satisfaction; “Low Satisfaction (≤75th percentile)” and “High Satisfaction (>75th percentile)”.15 For each question, only if the response of pregnant women was a score of 3, they were satisfied with this specific service. So, the cutoff point was set at a score of 3 for each question in the scoring of service. For each group of satisfaction, cut-off points were calculated based on their satisfaction scores. Prior to actual data collection, a pilot survey for the pre-test of the questionnaire was performed in a non-sample area to assess the validity of the questionnaire.
Data Analysis
Collected data were coded and then entered into Microsoft Excel (Microsoft Co. WA, USA). The data were analyzed using SPSS (version 16.0) software (IBM Co, NY, USA). Descriptive statistics and binary logistic regression analyses were performed. In binary logistic regression, both binary and multivariable analyses were carried out to identify the factors affecting the level of satisfaction. The outcome variable is a satisfaction to health service delivery while explanatory variables are socio-demographic and healthcare-related. P-value <0.05 is considered as statistically significance. Adjusted odds ratios were found to prove the strong association. For a qualitative study, concepts were explored from themes and presented to support the quantitative results.
In multivariable logistic regression analysis, the significant variables and those with p-value <0.25 in the crude analysis were entered into a multivariable logistic model to control the confounding.13
Ethical Consideration
The study was approved by ethical committees of Nagasaki University, School of Tropical Medicine, and Global Health and Ethical Review Committee of Department of Medical Research, Myanmar by ‘Approval Number: Ethics/DMR/2017/129ʹ. Written informed consent was taken from each participant or their parental/legal guardian if they are under 18 and confidentiality was assured. We affirm that this study in all its stages was compiled with the Declaration of Helsinki.16
Results
Socio-Demographic Characteristics
The socio-demographic characteristics of the respondents are represented in Table 1. Our respondents’ ages ranged from 16 to 39 years, with the majority of them (93%) between 20 and 39 years, leaving about 7% as pregnant women under 20. About half of our included respondents were housewives, while the other half was divided between working for the government/private sector or stated their occupation as “others”. While the highest percentage of respondents were at the high school level (40%), it should be noted that about 10% of our respondents were in primary school. Only 18% had university qualifications; however, there were no illiterate women in our sample. Notably, up to 60% of our respondents’ families were composed of three members, while the rest comosed more than three. And, 36.8% stated that their monthly income was less than 133 USD, while only 29% of the families get over 200 USD. Besides, 28% of our respondents lived in remote areas, while the rest lived in the borders of 10 km of towns.
 |
Table 1 Socio-Demographic Characteristics of the Respondents, Pregnant Women (N=125) |
Obstetric Characteristics of Respondents
Our sample showed that more than one-third (38%) of respondents visited the antenatal clinic five or more times, and 25% of them visited the ANC only twice (Table 2). Besides, the prevailing state of current pregnancy was the primigravida in about 60% of the respondents. We found that half of the respondents (51%) were between the 28 and the 36 gestational weeks, while 14% were less than 24 weeks of gestation at the enrollment. Additionally, the first ANC visit before 12 weeks of gestation accounted for 26% of the respondents, where nearly one-third of respondents 32% started at 19−24 weeks of gestation. Concerning the type of pregnancy, we noticed that nearly two-thirds (66%) of pregnancies were planned and expected.
 |
Table 2 Obstetric Characteristics of the Respondents (N=125) |
The levels of satisfaction of our respondents of pregnant women with the services introduced by the hospitals are presented in Table 3. The principal items, included for investigating patients’ satisfaction, were the general facilities, general services, registration services, and providers’ services. The majority of our included women (68%) were satisfied with the general facility (including waiting area, antenatal clinic, medical records, and privacy), while the one-fifth of them were satisfied with the mentioned items. The general services, also proved close results, with about 63% of our cases were satisfied with the services mentioned in the table, while the quarter of them was satisfied. Furthermore, the included sample stated that the biggest part of them (66%) were satisfied with the registration services, while about a quarter of them was totally satisfied. Coming to the evaluation of providers, the participants showed that 65% of the respondents were satisfied with the services, while the third part of them was totally satisfied.
 |
Table 3 The Satisfaction of Pregnant Women with Services of the Hospital |
Associated Factors with Total Satisfaction
The principal factors that participated in the dissatisfaction with the healthcare services were estimated. Our analysis revealed that the monthly income was significantly associated with the dissatisfaction of the three areas of service, among all included factors as presented in Table 4.
 |
Table 4 Adjusted Odds Ratios for an Association of Each Characteristic with the Area of Services |
Interestingly, families with income less than 200 001 kyats showed a statistically significant association with the dissatisfaction of general facility (Adjusted Odd Ratio (AOR)=0.34, 95% CI 0.13–0.94). Besides, the families with income between 200 001 and 300 000 kyats stated they were dissatisfied with the general facility (AOR=0.29, 95% CI 0.11–0.82), general services (AOR=0.34, 95% CI 0.13–0.89) or registration services (AOR=0.36, 95% CI 0.13–0.96).
Among the four service groups of satisfaction; the providers’ services had the highest satisfaction score (48%), while the general facilities had the lowest satisfaction score (73%) (Table 5). In conclusion, the greatest proportion of dissatisfaction was noticed in the general facilities of the hospital followed by registration service. Overall, half of our sample were highly satisfied with the total services (48%), where the other half (52%) were accounted for a low satisfaction score (Figure 1).
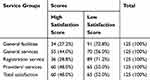 |
Table 5 Distribution of Respondents by Different Service Groups |
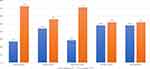 |
Figure 1 Frequency distribution of respondents’ satisfaction level with different services. |
Notably, there is a statistically significant association between the overall satisfaction and the six elements; waiting time to see doctors, ventilation and lighting in waiting area, drug supply, the process of ANC procedure, cleanliness, and working hours of ANC clinic in Table 6. Also, there is a significant association between each of those services and the overall dissatisfaction.
 |
Table 6 Ranking of Factors That Received Low Satisfaction Among Those Who Were Dissatisfied Overall (N=65), The Ranking of Factors That Received Dissatisfaction |
In the qualitative findings; we have found some explanations for these results. For instance; the reduced costs along with the good services were the connection between the hospital and the pregnant women. Women who delivered the first child at this hospital mentioned that they were satisfied with the services; therefore, they returned back. The pregnant women needed to pay between 4000 and 20,000 kyats (estimated 4–20 USD) to reach the hospital for each visit. Also, they have to pay for the ultrasound service between 1000 and 3000 kyats, added to, the blood test which costs 2000 kyats. The main obstacle was transportation costs which were high for ANC. Most of the women were dissatisfied with toilet facilities in the ANC clinic as they stated that toilets in the clinic were not sufficient for attended women.
Discussion
We investigated the patients’ satisfaction in different aspects for each service; general facilities, general services, registration service, and providers’ service.10 We could reveal, in this study, that only 6/25 services (ventilation and lighting in the waiting area, waiting time to see doctors, drug supply, ANC procedure, cleanliness of the clinic, and working hours) were significantly linked with the overall satisfaction. This study is paralleled with the findings of similar studies from different countries such as India, Malaysia, and Pakistan.17–19
In the present study, satisfaction levels of pregnant women did not vary regarding their ages or occupations. This finding is not compatible with Adeyinka et al and Das et al where their statistics showed a link between the employment state and the dissatisfaction.20,21 They dated their findings back to the lost time of the working women in the care or their accumulated experience more than the unemployed women. The contradiction may be due to the sample size or the distance between the women and the facility; as in Adeyinka et al, for instance, they investigated cases in rural places with limited access to the healthcare settings. In our study, we run a facility-based investigation where respondents already have access to clinical care.
Coming to the general facilities and providers’ services; highly educated women had slightly higher satisfaction more than the low-educated women; nevertheless, the differences were not statistically significant. This insignificance is partly tied to the small number of women in low education levels in our sample. In the meanwhile, Nabbuye-Sekandi et al proved that women with higher education were more satisfied in the outpatient clinics in Uganda.22
In our study, we have figured that women living near to catchment areas were more satisfied, with general services, registration, and providers’ services, than those from the remote area; however, the statistics were not significant. Notably, this result is different from Melese et al where remote-habitants women were happier with the services.10,23 On the other hand, our data are consistent with the finding of a study in Ghana determining consumer satisfaction of health care.23 This variation in results may be stemmed back to the difference of socio-demographic properties which cannot be consistent through different studies.
Furthermore, many studies stated that pregnant women with higher family incomes tend to be less satisfied compared to the low-income group.2,13 However, this study found that pregnant women with higher family income were more likely to be satisfied with all four service dimensions, statistically significant in the general facility, general services, and registration service. The possible explanation for greater satisfaction could be that women with high incomes were able to pay more to get more and better services but they chose this hospital’s services by their own choice. Another possible justification was that low-income women were less satisfied with services due to payment for some (laboratory and ultrasound) services. In addition, this study observed that non-primigravida women had higher satisfaction with general facility services than primigravida. This finding indicated that they chose this facility since they already had a good experience with this hospital during previous pregnancies. We noticed that most of the multipara women (52%) delivered their previous children at this hospital. This finding is similar to a study done in Sri Lanka which determined factors for client satisfaction in hospitals.24
In the meantime, pregnant women with frequent ANC visits had higher satisfaction than that with few visits. Surprisingly, pregnant women with many visits were more likely to have complied with information for regular follow-up meanwhile they were satisfied. Perhaps the justification was that pregnant women with frequent visits were familiar with the hospital environment and care providers.
The women with expected pregnancy were more likely to be satisfied with all groups of services except registration services. A similar finding was reported in a study conducted in Ethiopia by Tayelgn and his colleagues in 2011.25,26 A systemic review reported that unexpected pregnancy was associated with postponement of ANC or inadequate ANC visits in both developing and developed countries.27
With regard to general services, pregnant women were less satisfied with laboratory service with a mean score of 2.98 out of 4. This concurred with the finding of a study in East Kazakhstan, which found that laboratory test services were not dissatisfied by the women.26 This may be reasoned by the insufficient information about blood tests and costs for testing.
In our analysis, most of the pregnant women were satisfied with the medical expenses incurred at the clinic for the service they received, which is in accord with different findings in studies in Pakistan and Malaysia.19,28 Besides, women were satisfied with the availability of ultrasound service that is coming in an accord with Soliman’s study in Egypt,19 in which pregnant women were unsatisfied with the unavailability of equipment especially ultrasound.
For the waiting time, it had the lowest mean score among other services, and it led to lower satisfaction overall. FGDs’ participants mentioned that they had 2–3 hours waiting time, also, the first visit was even longer. Waiting time is the major problem in service delivery of ANC setting, which influenced, negatively, the decision of newly pregnant women to start antenatal care.
For the communication; satisfaction patterns were different between the type of providers, with a higher satisfaction for nurses than doctors. This was in line with previous researches done in Sri Lanka and India.24,29 The possible explanation for this finding was the low social experience for doctors compared to nurses. In fact, pregnant women were familiar with nurses during health education sessions where nurses alleviated their anxiety.
Facilities in the waiting area, laboratory service, and long waiting time to see doctors were the services that caused low satisfaction based on the total dissatisfied score. The findings on areas of dissatisfaction were supported by qualitative findings. Pregnant women were highly satisfied with the examination done by doctors, working hours, and health education. According to the results, hospital authorities should pay attention to the six services that are significantly associated with overall satisfaction to be a better environment for their patients. We should inquire about the weakness of laboratory service and put effort to cover this weakness. The hospital should focus on the improvement of facilities to increase overall satisfaction like toilets, waiting for space, and infrastructure. Advantages of services that attained a high satisfaction score should be maintained alongside desired improvements in other services.
Limitations
The study presented interesting results, but those results were limited by some factors. For instance, our sample size was limited to identifying all factors associated with the satisfaction of pregnant women with antenatal care services. Also, the limitation inherent to satisfaction studies was the tendency of respondents to reply to positive answers to questions concerning satisfaction because of their reluctance to blame care providers. In order to minimize this bias, we conducted an interview and FGDs in a separate room by using non-hospital staff as research members.
Conclusion
Nearly half of pregnant women in the study were very satisfied with the total healthcare services they received. Our analysis exculpated that majority of the socio-demographic and obstetric characteristics of pregnant women were not significantly influencing the satisfaction with ANC services. In addition, the satisfaction level of respondents varied by the services they received. Among the four areas of service; providers’ services had the highest satisfaction score, and high dissatisfaction was found in general facilities. In general, facilities in the waiting area, laboratory service, and waiting time to see doctors were dissatisfied services. We recommend that healthcare authorities should upgrade the facilities in the waiting area and increase the workforce to counteract the overcrowding. This study explored many challenges in the provision of healthcare services which indicated the need to improve the public facilities in the Myanmar context.
Strengths and limitations of This Study
- This study is empowered by the use of techniques to minimize the risk of bias.
- Our results are limited by the sample size; which hindered explicating all the factors.
- The tendency of respondents to reply positively may frame a limitation.
Abbreviations
ANC, antenatal care; FGDs, focus group discussions; LB, live births; MOHS, Ministry of Health and Sports; PSQ, Patient Satisfaction Questionnaire; SOWCH, South Okkalapa Women and Children Hospital; WHO, World Health Organization.
Acknowledgments
We greatly acknowledge Priya Raju (American University of the Caribbean, Cupecoy, Saint Maarten, Netherland Antilles) for her editing our manuscript.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare no potential conflicts of interest.
References
1. Gidey G, Hailu B, Nigus K, et al. Timing of first focused antenatal care booking and associated factors among pregnant mothers who attend antenatal care in Central Zone, Tigray, Ethiopia. BMC Res Notes. 2017;10(1):608. doi:10.1186/s13104-017-2938-5
2. Yaser AA, Hussein AFA. Assessment of antenatal care services among pregnant women’s in Al-Hilla City. Kufa J Nurs Sci. 2015;5(3):192–200.
3. Kabir R, Khan H. Utilization of antenatal care among pregnant women of Urban Slums of Dhaka City, Bangladesh. IOSR J Nurs Health Sci. 2013;2(2).
4. Thompson A. Poor, and pregnant in Africa: safe motherhood and human rights. Midwifery. 1999;15(3):146–153. doi:10.1016/S0266-6138(99)90059-1
5. Organization WH. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. World Health Organization; 2016.
6. Lincetto O, Gomez P, Munjanja S. Antenatal care. Opportunities for Africa’s newborns: practical data, policy, and programmatic support for newborn care in Africa. World Health Organisation; 2006:55–62.
7. Paudel YR, Jha T, Mehata S. Timing of first antenatal care (ANC) and inequalities in early initiation of ANC in Nepal. Front Public Health. 2017;5:242. doi:10.3389/fpubh.2017.00242
8. Aung SH. Myanmar needs to strengthen smokeless tobacco control policies. Southeast Asia J Public Health. 2016;6(2):1–2.
9. Health, M.o. and I. Sports. Myanmar demographic and health survey 2015–16. 2017.
10. Melese T, Gebrehiwot Y, Bisetegne D, et al. Assessment of client satisfaction in labor and delivery services at a maternity referral hospital in Ethiopia. Pan Afr Med J. 2014;17. doi:10.11604/pamj.2014.17.76.3189
11. Galle A, Van Parys A-S, Roelens K, et al. Expectations and satisfaction with antenatal care among pregnant women with a focus on vulnerable groups: a descriptive study in Ghent. BMC Women’s Health. 2015;15(1):112. doi:10.1186/s12905-015-0266-2
12. Win AH, Panza A. Clients’ satisfaction towards health care services at outpatient department, Pinlon Hospital, Yangon, Myanmar. J Health Res. 2010;24(Suppl 2):15–20.
13. Chemir F, Alemseged F, Workneh D. Satisfaction with focused antenatal care service and associated factors among pregnant women attending focused antenatal care at health centers in Jimma town, Jimma zone, South West Ethiopia; a facility-based cross-sectional study triangulated with a qualitative study. BMC Res Notes. 2014;7(1):164.
14. Marshall GN, Hays RD. The Patient Satisfaction Questionnaire Short-Form (PSQ-18). Rand Santa Monica, CA; 1994.
15. Ajayi DT, Adedokun BO, Owoeye DO, et al. Treatment satisfaction and medication adherence among hypertensive patients seeking care in selected hospitals in Ibadan, Nigeria. Arch Basic Appl Med. 2018;6(1):67.
16. General Assembly of the World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81(3):14.
17. Dhahi ZK, Issa SS, Hameed LA. A study on pregnant women’s satisfaction with primary health care services in Basra. Int J Res Humanit Arts Lit. 2015;3:7–19.
18. Majrooh MA, Hasnain S, Akram J, et al. Coverage and quality of antenatal care provided at primary health care facilities in the ‘Punjab’province of ‘Pakistan’. PLoS One. 2014;9(11):e113390. doi:10.1371/journal.pone.0113390
19. Pitaloka DS, Rizal A. Patient’s satisfaction in antenatal clinic hospital Universiti Kebangsaan Malaysia. Jurnal Kesihatan Masyarakat (Malaysia). 2006;12(1):1–10.
20. Adeyinka O, Jukic AM, McGarvey ST, et al. Predictors of prenatal care satisfaction among pregnant women in American Samoa. BMC Pregnancy Childbirth. 2017;17(1):381. doi:10.1186/s12884-017-1563-6
21. Pal R, Das P, Basu M, et al. Client satisfaction on maternal and child health services in rural Bengal. Indian J Community Med. 2010;35(4):478. doi:10.4103/0970-0218.74344
22. Nabbuye-Sekandi J, Makumbi FE, Kasangaki A, et al. Patient satisfaction with services in outpatient clinics at Mulago hospital, Uganda. Int J Qual Health Care. 2011;23(5):516–523. doi:10.1093/intqhc/mzr040
23. Nketiah-Amponsah E, Hiemenz U. Determinants of consumer satisfaction of health care in Ghana: does the choice of health care provider matter? Glob J Health Sci. 2009;1(2):50. doi:10.5539/gjhs.v1n2p50
24. Senarath U, Fernando DN, Rodrigo I. Factors determining client satisfaction with hospital‐based perinatal care in Sri Lanka. Trop Med Int Health. 2006;11(9):1442–1451. doi:10.1111/j.1365-3156.2006.01698.x
25. Tayelgn A, Zegeye DT, Kebede Y. Mothers’ satisfaction with referral hospital delivery service in Amhara Region, Ethiopia. BMC Pregnancy Childbirth. 2011;11(1):78. doi:10.1186/1471-2393-11-78
26. Dauletyarova M, Semenova Y, Kaylubaeva G, et al. Are Kazakhstani women satisfied with antenatal care? Implementing the WHO tool to assess the quality of antenatal services. Int J Environ Res Public Health. 2018;15(2):325. doi:10.3390/ijerph15020325
27. Hajizadeh S, Ramezani Tehrani F, Simbar M, et al. Factors influencing the use of prenatal care: a systematic review. J Midwifery Reproductive Health. 2016;4(1):544–557.
28. Ashraf M, Ashraf F, Rahman A, et al. Assessing women’s satisfaction level with maternity services: evidence from Pakistan. Int J Collab Res Intern Med Public Health. 2012;4(11):1841.
29. Pricilla RA, David K, Siva R, et al. Satisfaction of antenatal mothers with the care provided by nurse-midwives in an urban secondary care unit. J Family Med Prim Care. 2016;5(2):420. doi:10.4103/2249-4863.192359
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
