Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
SAPHO Syndrome with Palmoplantar Pustulosis as the First Manifestation Successfully Treated with Adalimumab
Authors Yang Q, Xiang T, Wu Y, Ye E, He B, Bu Z
Received 30 July 2022
Accepted for publication 17 November 2022
Published 28 November 2022 Volume 2022:15 Pages 2547—2554
DOI https://doi.org/10.2147/CCID.S384346
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Qingyun Yang,1,* Tingkai Xiang,1,* Yangfan Wu,1,* Enyi Ye,1,* Beilei He,1,* Zhangyu Bu2,*
1Department of The Fourth School of Clinical Medicine, Zhejiang Chinese Medical University, Hangzhou, Zhejiang, 310006 People’s Republic of China; 2Department of Dermatology, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou, 310006, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhangyu Bu, Department of The Fourth School of Clinical Medicine, Zhejiang University School of Medicine, No. 261, Huansha Road, Hangzhou, Zhejiang, 310006, People’s Republic of China, Fax +8657156006617, Email [email protected]
Introduction: Synovitis-acne-pustulosis-hyperostosis-osteitis (SAPHO) syndrome is an acronym for synovitis, pustulosis, acne, hyperostosis, and osteitis, and clinically manifests as dermatological and musculoskeletal damage. Two major manifestations that co-occur in a single patient are rare.
Methods/Results: This literature describes a 44-year-old male affected by SAPHO syndrome, whose first manifestation was palmoplantar pustulosis (PPP). Symptomatic treatments such as anti-inflammatory and analgesics did not work well for him. Adalimumab provided noteworthy improvement in the neck and thoracic back pain improvement after two weeks. The palmoplantar pustules were alleviated after four weeks.
Conclusion: The literature on SAPHO syndrome therapy is increasing. Thus, adalimumab is a novel therapeutic agent. This report demonstrates the efficiency of adalimumab in SAPHO syndrome.
Keywords: synovitis, acne, psoriasis, bone hypertrophy, osteitis, psoriasis arthritis, adalimumab
Introduction
Synovitis-acne-pustulosis-hyperostosis-osteitis (SAPHO) syndrome is an acronym for synovitis, pustulosis, acne, hyperostosis, and osteitis, and it clinically manifests as dermatological and musculoskeletal damage. The skin manifestations of the disease are vairy. Palmoplantar pustulosis (PPP) is the most common manifestation in SAPHO, only 63.5% of patients present with typical lesions,1 which can lead to misdiagnosis when patients present with atypical lesions. We recommend biological treatment for patients with SAPHO, especially those with PPP.2 A few cases have reported the successful use of TNF-α for SAPHO syndrome.3–5 Compared to traditional treatments, adalimumab is a novel therapeutic option. We report the case of an adult patient with SAPHO syndrome whose first manifestation was PPP successfully treated with adalimumab. The relevant literatures are also reviewed.
Case Presentation
A 44-year-old male patient presented with palmoplantar pustules in the first clinical presentation. He presented with erythematous pustules on both hands and feet for six months, with no itching or pain. The patient was previously healthy and had no history of underlying diseases or psoriasis.
Dermatological Examination
The patient developed scattered patchy erythema and pustules on the palms of both hands and the soles (Figure 1).
 |
Figure 1 Scattered patchy erythema and pustules on the palms of both hands and the soles (A). The palmoplantar pustules were alleviated after treatment (B). |
Orthopedic examination: The patient felt pain in the right thoracic vertebra joint under pressure, and it was hard for him to lift both upper limbs.
Laboratory Tests
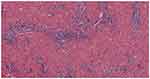
The results showed that the CRP level was 19 mg/L (0–8 mg/L), ESR was 62 mm/h (0–15 mm/h), and PLT was 369*10^9/L (100–350*10^9/L). Besides, WBC count, neutrophil count, lymphocyte count, RBC count, Hb, ALT, AST, RF, tumor markers and thyroid function, immune function, and routine urine test results were all normal. Moreover, the anti-CCP antibody profile, ANA profile, HLA-B27, PPD test, and T-SPOT results were negative. Skin biopsy pathology of the left hand revealed that the patient suffered from hyperkeratosis of the skin, with a few focal purulent exudates, epidermal hyperplasia, hypertrophy of the spinous layer, and hyperplasia of the epithelium of the epidermis with lymphocytic infiltration (Figure 2).
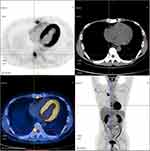
On the second day after admission, the patient complained of unbearable neck and thoracic back pain and difficulty lifting both upper extremities. Whole-body imaging was then performed. Specifically, the cervical and thoracic MRI revealed abnormal signal foci in the 5th, 8th, 9th, and 10th thoracic vertebra (T5, T8, T9, and T10) and some body parts (Figure 3). Later, PET-CT was performed, which showed abnormal glucose metabolism with bone alteration in the 1st right sternocostal joint, sternal body, the T5, T8, T9, and T10, and the 4th lumbar vertebra (L4), with a high possibility of malignant lesion (Figure 4). Furthermore, ECT revealed radiologically distributed thickening in the 1st anterior right rib, right sternoclavicular joint, and right upper tibia (Figure 5).
 |
Figure 3 MRI of the thoracic spine shows abnormal signal lesions in the 5th, 8th, 9th, and 10th thoracic spine (T5, T8, T9, and T10). |
 |
Figure 5 ECT showed that radiologically distributed thickening appeared in the 1st anterior right rib, right sternoclavicular joint, and right upper tibia (Figure 1F). |
The patient was referred for an orthopedic consultation. He was diagnosed with bone tumor metastases by the Department of Orthopedics, and a vertebral puncture was recommended. However, the patient’s vertebral biopsy pathology report did not suggest tumor cells; however, it showed T9 and L4 bone tissues with few broken bones, sequestrums, bone marrow, and focal plasma cell hyperplasia (Figure 6). Immunohistochemical findings revealed a few scattered Mum-1 [+] CD38 [+] CD138 [+]. The day after the vertebral puncture, the patient developed a folliculitis-like lesion on the anterior chest and back (Figure 7). Based on the patient’s clinical symptoms, imaging manifestations, and pathological findings from bone and skin biopsies, a bone tumor was excluded, and the patient was diagnosed with SAPHO syndrome.
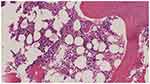 |
Figure 6 The patient’s vertebral biopsy pathology report did not suggest tumor cells, but only a few broken bones, sequestrums, and bone marrow. |
 |
Figure 7 Pustular lesion on the anterior chest and back. |
Treatment
The patient underwent routine symptomatic anti-inflammatory treatment; however, there was no significant improvement. On 5/15/2020, the patient received adalimumab subcutaneously at the first dose of 80 mg, followed by 40 mg every two weeks (q2w). Two weeks after the treatment, the joint symptoms were significantly relieved. And the palmoplantar pustules were alleviated after four weeks (Figure 1). The patient has been treated for more than two years and is still undergoing treatment. In the present follow-up, all the symptoms disappeared.
Discussion
SAPHO syndrome is a rare chronic autoimmune disease with major clinical manifestations, including bone hypertrophy, osteomyelitis, acne, pustulosis, and synovitis.1 There are no uniform diagnostic criteria for SAPHO syndrome, and the diagnostic criteria proposed by Benhamou et al are more commonly used: (1) acne + osteoarthritic manifestations; (2) palmoplantar pustulosis + osteoarthritic manifestations; (3) hyperostosis (anterior chest wall, limb or spine) with or without cutaneous manifestations; (4) and chronic recurrent multifocal osteomyelitis involving the mesial or peripheral bones with or without cutaneous manifestations. Patients with one of the above manifestations and no infectious diseases or bone tumors can be definitively diagnosed with SAPHO syndrome. In the present case, the disease in the patient was first manifested as palmoplantar pustules, and six months later, he developed pain in the right sternocostal and right knee joint. After admission, multiple folliculitis-like lesions appeared on the anterior chest and back, and imaging suggested abnormal signal foci in the 1st right sternocostal joint, which met three of the above diagnostic criteria. The patient had no infectious diseases or bone tumors, so the diagnosis of SAPHO syndrome was confirmed.
The two typical manifestations of the disease are skin damage and bone and joint involvement. These two characteristic manifestations occur in an irregular order, with cutaneous manifestations appearing earlier, later, or simultaneously with osteoarticular symptoms. Skin involvement can manifest in various forms, such as palmoplantar pustulosis, pustular psoriasis, severe acne, common psoriasis, and Sweet’s syndrome.
Bone and skin biopsies of SAPHO syndrome are non-specific and cannot be used to confirm the disease but primarily to exclude other diseases.6 Skin histopathology shows aseptic inflammation and pseudo-abscesses infiltrated by neutrophils, and bacterial cultures are usually negative.7 WBC count, ESR, and CRP levels may be elevated during serological examination, and rheumatoid factor and antinuclear antibodies are mostly negative. X-ray, CT, MRI, PET/CT, and ECT are currently the most prominent methods for diagnosing SAPHO syndrome, but not every patient has typical manifestations.8,9 SAPHO syndrome frequently arises in the bilateral sternoclavicular joints, the 1st sternocostal joint, and the sternal stalk, similar to the “bull’s head”. In the present case, the patient lacked the typical “bull’s head” sign, and only the 1st sternocostal joint and sternal body were involved.
The patient in this study had palmoplantar pustulosis and pain in the sternoclavicular area in succession, which should be differentiated from pustular psoriasis (PP) and psoriasis arthritis (PsA). European Rare and Severe Expert Network (ERASPEN) considered PPP a variant of PP.10 In patients with PPP, the prevalence of psoriasis arthritis has been reported to range from 8.6 to 26%,11 and nail involvement (nail psoriasis) is 30 to 76%. PsA has a longer course, and chronic changes in the nail usually occur before osteoarthritic changes. Joint symptoms worsen or diminish in parallel with cutaneous symptoms, with joint symptoms aggravating while imaging shows the opposite. Psoriasis arthritis is more common in small peripheral joints such as the hand, wrist, and foot joints, with the end of the finger (toe) joints showing hypertrophy of the joint edges. Some scholars argue that PPP should be classified as a form of PP, the associated arthritis is part of psoriatic arthropathy, and SAPHO syndrome may be a subtype of psoriatic arthritis.11,12
The pathogenesis of SAPHO syndrome has not been completely elucidated, and it is probably connected with genetic susceptibility factors and dysregulation of innate immunity with overexpression of proinflammatory cytokines, especially interleukin (IL)-1, IL-17, and tumor necrosis factor-alpha (TNF-a).13
SAPHO syndrome is mainly treated symptomatically with NSAIDs or NSAIDs combined with anti-rheumatic drugs. Biological agents are more common and effective, including 1) IL-1 receptor antagonist, anakinra; 2) TNF-α antagonists, including adalimumab, etanercept, and infliximab. Some studies have found a high expression of TNF-α in the biopsies of diseased bone tissues with SAPHO syndrome14 and abnormal expressions of IL-8 and IL-18 in serum, which are inflammatory factors that enhance the expression of TNF-α and its related products, which can be used as solid evidence for the efficacy of TNF-α antagonists in the treatment of SAPHO syndrome.4,5 There are data on a small number of cases accepting adalimumab treatment in SAPHO patients. The treatment was well tolerated, and the improvement of skin and joint symptoms was observed.3–5 Although there have been sporadic case report that using anti-TNF-α therapy can lead to skin manifestations, such as psoriasiform lesions, as adverse effects,15–17 adalimumab is still an effective choice.
Conclusion
SAPHO syndrome has diverse clinical and imaging presentations with atypical and rare early symptoms. When patients have atypical skin lesions, dermatologists may miss the diagnosis because they are unaware of the disease. Therefore, dermatologists should pay attention to patients with pustular lesions or eruptive acne in combination with persistent bone and joint damage to reduce misdiagnosis. Our case confirms the literature data3–5 reporting the efficacy of adalimumab in SAPHO syndrome.
Abbreviations
SAPHO, synovitis-acne-pustulosis-hyperostosis-osteitis; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; PLT, platelet; WBC, white blood cell; RBC, red blood cell; Hb, hemoglobin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; RF, rheumatoid factor; CCP, cyclic citrullinated peptide; ANA, antinuclear antibody; HLA-B27, human leukocyte antigen B27; PPD, purified protein derivative; T-SPOT, T cell spot test of tuberculosis infection; MRI, magnetic resonance imaging; CT, computed tomography; PET-CT, positron emission tomography-computed tomography; ECT, emission computed tomography; PP, pustular psoriasis; PsA, psoriasis arthritis; ERASPEN, The European Rare and Severe Expert Network; PPP, pustulosis palmaris plantaris; NSAIDs, nonsteroidal anti-inflammatory drugs.
Ethics Approval
Our institution did not require ethical approval for reporting individual cases. We thank the patient for providing written informed consent for all types of accompanying images to be published in this article.
Acknowledgments
We thank the patient for providing written informed consent for the publication of all types of accompanying images and case details. Institutional approval does not apply to this case publication.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Hangzhou Science and Technology Committee Grant numbers: 20191203B94, Medical Science and Technology Project of Zhejiang Province Grant numbers: 2020RC095, Zhejiang Province Public Welfare Technology Application Research Project Grant numbers: LGF19H110001, Medical Science and Technology Project of Zhejiang Province Grant numbers: 2018KY578.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Firinu D, Garcia-Larsen V, Manconi PE, et al. SAPHO syndrome: current developments and approaches to clinical treatment. Curr Rheumatol Rep. 2016;18(6):35. doi:10.1007/s11926-016-0583-y
2. Ji Q, Wang Q, Pan W, et al. Exceptional response of skin symptoms to secukinumab treatment in a patient with SAPHO syndrome: case report and literature review. Medicine. 2022;101(33):e30065. doi:10.1097/MD.0000000000030065
3. Vekic DA, Woods J, Lin P, et al. SAPHO syndrome associated with hidradenitis suppurativa and pyoderma gangrenosum successfully treated with Adalimumab and methotrexate: a case report and review of the literature. Int J Dermatol. 2018;57(1):10–18. doi:10.1111/ijd.13740
4. Castellví I, Bonet M, Narváez JA, et al. Successful treatment of SAPHO syndrome with Adalimumab: a case report. Clin Rheumatol. 2010;29(10):1205–1207. doi:10.1007/s10067-010-1476-5
5. Crowley EL, O’Toole A, Gooderham MJ. Hidradenitis suppurativa with SAPHO syndrome maintained effectively with Adalimumab, methotrexate, and intralesional corticosteroid injections. SAGE Open Med Case Rep. 2018;6:2050313x18778723. doi:10.1177/2050313X18778723
6. Kahn MF, Hayem F, Hayem G, et al. Is diffuse sclerosing osteomyelitis of the mandible part of the synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome? Analysis of seven cases. Oral Surg Oral Med Oral Pathol. 1994;78(5):594–598. doi:10.1016/0030-4220(94)90170-8
7. Marzano AV, Genovese G, Moltrasio C, et al. Whole-exome sequencing in 10 unrelated patients with syndromic hidradenitis suppurativa: a preliminary step for a genotype-phenotype correlation. Dermatology. 2022;238(5):860–869. doi:10.1159/000521263
8. Colina M, Govoni M, Orzincolo C, et al. Clinical and radiologic evolution of synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome: a single center study of a cohort of 71 subjects. Arthritis Rheum. 2009;61(6):813–821. doi:10.1002/art.24540
9. Depasquale R, Kumar N, Lalam RK, et al. SAPHO: what radiologists should know. Clin Radiol. 2012;67(3):195–206. doi:10.1016/j.crad.2011.08.014
10. Brunasso AMG, Massone C. Recent advances in palmoplantar pustulosis. Fac Rev. 2021;10:62. doi:10.12703/r/10-62
11. Kim M, Yang S, Kim BR, et al. Nail involvement features in palmoplantar pustulosis. J Dermatol. 2021;48(3):360–365. doi:10.1111/1346-8138.15716
12. Chen W, Ito T, Lin S-H, et al. Does SAPHO syndrome exist in dermatology? J Eur Acad Dermatol Venereol. 2022;36(9):1501–1506. doi:10.1111/jdv.18172
13. Genovese G, Caorsi R, Moltrasio C, et al. Successful treatment of co-existent SAPHO syndrome and hidradenitis suppurativa with Adalimumab and methotrexate. J Eur Acad Dermatol Venereol. 2019;33(Suppl 6):40–41. doi:10.1111/jdv.15849
14. Wagner AD, Andresen J, Jendro MC, et al. Sustained response to tumor necrosis factor alpha-blocking agents in two patients with SAPHO syndrome. Arthritis Rheum. 2002;46(7):1965–1968. doi:10.1002/art.10539
15. Massara A, Cavazzini PL, Trotta F. In SAPHO syndrome anti-TNF-alpha therapy may induce persistent amelioration of osteoarticular complaints, but may exacerbate cutaneous manifestations. Rheumatology. 2006;45(6):730–733. doi:10.1093/rheumatology/kei221
16. Ben Abdelghani K, Dran DG, Gottenberg J-E, et al. Tumor necrosis factor-alpha blockers in SAPHO syndrome. J Rheumatol. 2010;37(8):1699–1704. doi:10.3899/jrheum.091086
17. Burgemeister LT, Baeten DL, Tas SW. Biologics for rare inflammatory diseases: TNF blockade in the SA PHO syndrome. Neth J Med. 2012;70(10):444–449.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.