Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Sanders type 3–4 calcaneal fractures fixed with locking plate: does tri-cortical iliac bone autograft provide extra benefit for stabilization?
Authors Bulut T, Gursoy M, Ozturk T, Ozcan C, Sener M
Received 15 July 2017
Accepted for publication 15 April 2018
Published 11 September 2018 Volume 2018:14 Pages 1665—1670
DOI https://doi.org/10.2147/TCRM.S146530
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh

Tugrul Bulut,1 Merve Gursoy,2 Tahir Ozturk,1 Cem Ozcan,1 Muhittin Sener1
1Department of Orthopaedics and Traumatology, Ataturk Training and Research Hospital, Izmir Katip Celebi University, Izmir, Turkey; 2Department of Radiology, Ataturk Training and Research Hospital, Izmir Katip Celebi University, Izmir, Turkey
Objective: The aim of this study was to determine whether tri-cortical iliac bone autografting provided extra benefit for the stabilization in Sanders Type 3–4 calcaneal fractures fixed with locking plate.
Materials and methods: The study included 29 calcaneal fractures (Sanders Type 3/4=15/14). All fractures were fixed with locking plate using the extended lateral approach. Bone grafts were used in 16 (Group A; Sanders Type 3/4=7/9) and not used in 13 (Group B; Sanders Type 3/4=8/5) calcaneal fractures. As a grafting material, only tri-cortical iliac crest bone autograft was used. All operations were performed by the same surgeon. The same locking plate was used in all fractures. Calcaneal height and angle of Bohler and Gissane were measured in early postoperative and final control radiographs in both groups. Clinical evaluations were performed using the American Orthopedic Foot and Ankle Society ankle hind foot scale.
Results: There was no difference between the groups in terms of clinical results. Radiologically, the degree of change in Bohler’s angle, Gissane’s angle, and calcaneal height was not different between the groups.
Conclusion: Bone grafting does not affect the clinical and radiologic outcomes in Sanders Type 3–4 calcaneal fractures fixed with locking plate, and they provide no extra benefit to the stabilization. We think that fixation using locking plate is adequate and there is no need for bone grafting.
Keywords: calcaneal fractures, Sanders Type 3–4, locking plate, bone autograft
Introduction
Calcaneus fractures are the most frequently seen tarsal bone fractures. Approximately 75% of all calcaneus fractures are intra-articular fractures.1,2 Displaced intra-articular calcaneus fractures occur as a result of impaction of the talus, and these are generally high-energy injuries.3,4 Impaction of the talus causes collapse and fragmentation in the posterior facet of the calcaneus, which can be seen clearly on computed tomography (CT). Sanders et al5 classified calcaneus fractures according to the number of fragments in the posterior facet. This classification has a prognostic importance.6 Sanders Type 3 and 4 fractures have a worse prognosis than other types.
Calcaneus fractures have long been recognized as having various complications and poor functional results. In comparison with other orthopedic injuries and other health problems such as myocardial infarct and organ transplant, displaced intra-articular calcaneus fractures have not currently reached the expected level with respect to function.7 Sanders Type 3 and 4 fractures in particular continue to be a significant reason for labor force loss and socioeconomic problems.
Surgical treatment is usually recommended for displaced intra-articular calcaneal fractures.8,9 One of the main aims of surgical treatment is anatomic reduction of the posterior facet. Spongeous bone defects occur following reduction of collapse in the posterior facet. Grafting is a method frequently applied to the defects that form. In the literature, there are different views on the subject of the necessity for and the efficacy of these grafts used.9–12
The aim of this study was to investigate whether tri-cortical iliac crest bone autograft made an additional contribution to protecting the stability of Sanders Type 3 and 4 fractures fixed using a locking plate. The clinical and radiological results of tri-cortical iliac crest bone autograft were also evaluated.
Materials and methods
This retrospective study was approved by the Institutional Review Board of our hospital (Izmir Katip Celebi University Non-interventional Clinical Studies Institutional Review Board; IRB: 177). Due to the retrospective nature of the study, informed consent by patients and providers was not required. Patient consent to review medical records was not required, as all data were deidentified. All methods were conducted in accordance with the approved guidelines.
This study was made on Sanders Type 3 and 4 displaced intra-articular calcaneus fractures, which were fixed using locking plate with an extended lateral approach between 2013 and 2016. Patients were excluded if they were aged <18 years or the follow-up period was <6 months. This retrospective study included 29 fractures of 27 patients comprising 4 females and 23 males, with a mean age of 41.48±11.33 (range, 22–59) years, with Sanders Type 3 (n=15) and Type 4 (n=14) fractures (posterior articular facet step-off >2 mm, loss of calcaneus height, and decreased Bohler’s angle). Bilateral calcaneus fracture was determined in 2 patients.
All the fractures were operated on by the same surgeon, and the same type of locking plate (Lowprofile Calcaneus Interlocking Plate, TST, Istanbul, Turkey) was used in all cases (Figure 1). Graft was used in 16 calcaneus fractures (Sanders Type 3/4=7/9) and not used in 13 fractures (Sanders Type 3/4=8/5). As grafting material, only tri-cortical iliac crest bone autograft was used. No donor site complications were observed in any case. The fractures where graft was used were called as Group A and those without graft as Group B.
All the patients were followed up according to the standard postoperative follow-up protocol established in our clinic for calcaneus fracture surgery. In accordance with this, all patients were immobilized for 2 weeks postoperatively with a short-leg brace. After the brace was removed, active and passive ankle joint range of movement exercises were started. Mobilization was started with partial weight-bearing in the 6th week, and in the 12th week, full weight-bearing was permitted.
No necrosis was observed in the flap of any patient. Superficial infection developed in 1 case (1/29=3.5%), which completely recovered with oral antibiotic therapy. Deep infection developed in 1 case (1/29=3.5%) and as there was no improvement with antibiotic therapy, the plate was removed in the postoperative 10th month. As there was bone union of this fracture, no additional fixation was made after the plate was removed. The 2 patients who developed infections were both in the group where graft had been used (2/16=12.5%).
In all patients, measurements were taken of Bohler’s angle, the crucial angle of Gissane, and calcaneal height in early postoperative radiographs (postop day 0 or 1) and at the final follow-up examination (at the earliest 3 months after the start of full weight-bearing, ≥6 months). By comparing these 2 values, any change in the angles and height values after the start of full weight-bearing were recorded, if present. By comparing the amount of loss in the final measurement values of the 2 groups, it was determined whether the use of tri-cortical iliac crest bone autografts made any additional contribution to the protection of the stability of Sanders Type 3 and 4 calcaneus fractures fixed with locking plate.
The clinical evaluations at the final follow-up examinations were done using the American Orthopedic Foot and Ankle Society (AOFAS) ankle hind foot scale. In this 100 point AOFAS scoring system, a score of ≥90 points is evaluated as excellent, 80–89 points as good, 70–79 points as fair, and a score of ≤69 points as poor.13,14
All the radiological measurements were made by an independent radiology specialist, and all the clinical evaluations by an independent orthopedics specialist.
Statistical analysis
Data analyses were performed using IBM SPSS Statistics Version 24.0 software (IBM Corporation, Armonk, NY, USA). According to the groups, age distribution was analyzed with the Mann–Whitney U-test, infection rate and gender distribution by the Fisher’s Exact test, affected side (right/left) and Sanders fracture type by Pearson χ2 analysis, and the clinical results according to the AOFAS score by χ2 trend analysis. The early- and late-stage radiological measurement results of the groups, AOFAS scores, and postoperative follow-up time were compared using Mann–Whitney U analysis. A value of p<0.05 was accepted as statistically significant.
Results
No statistically significant difference was determined between the groups with respect to age, gender, side (right/left), and Sanders fracture type (p>0.05) (Tables 1–3) were observed.
  | Table 1 Age distribution of the groups |
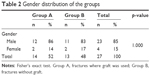  | Table 2 Gender distribution of the groups |
The postoperative follow-up period was determined as 12.25±4.58 months in Group A and 11.38±5.47 months in Group B, with no statistically significant difference between the groups (p>0.05) (Table 4).
According to the AOFAS scores, excellent and good results were obtained in 62.5% (10/16) of the graft group and in 69.3% (9/13) of the nongraft group. The mean AOFAS score was 83.63±10.26 in Group A and 87.54±10.6 in Group B, with no statistically significant difference between the groups (p>0.05) (Tables 3 and 4).
No difference was found in early and late Bohler’s angle and calcaneal height values of the groups (p>0.05). The early and late stage Gissane’s angle values of the Group A were lower than that of the Group B (p<0.05) (Table 4).
When the amount of change in the Bohler’s angle, Gissane’s angle, and calcaneal height values at the final follow-up examination were examined, the loss of Bohler’s angle had a mean of 1.54°±1.48° (range, 0°–6.5°) in Group A and 1.38°±1.02° (range, 0°–4.1°) in Group B, the change in the Gissane angle had mean of 1.86°±1.4° (range, 0°–6.8°) in Group A and 1.79°±0.85° (range, 1.2°–4.2°) in Group B, and the loss of calcaneal height had a mean of 0.98±0.92 (range, 0.03–3.6) mm in Group A and 0.81±0.63 (range, 0–2.2) mm in Group B. No statistically significant difference was determined between the groups at the final follow-up examination with respect to the amount of change in the angles and height values (p>0.05) (Table 4).
Infection was developed in 2 cases (2/16=12.5%) in Group A, and there was no infection case in Group B. This difference was not statistically significant (p>0.05).
Discussion
There is no full consensus in literature on the treatment of displaced intra-articular calcaneus fractures.11,15–17 The search for a new treatment, which may be an alternative, is still continuing.18,19 Open reduction and internal fixation (ORIF) is currently accepted by many authors as the primary treatment for displaced intra-articular calcaneus fractures.8,20 Although which technique should be used for ORIF is debatable, the basic aim of all the methods is the anatomic reduction of the posterior facet and the anatomic restoration of the height, width, and length of the calcaneus. In the literature, the advantages and effectiveness of locking plates are very clear.21–23 However, the necessity for and effectiveness of grafting is still a controversial issue.9–12
In addition to the effects of filling defects, grafting also has the effect of providing mechanical support and promoting bone healing. Therefore, while some authors have advocated the necessity of frequent use of grafting, others have stated that the use is always necessary.24–27 In some recent studies, grafting has been reported to have no positive effects on functional and radiological results.8,12,28
Duymus et al9 investigated the need for cancellous allogenic bone graft in calcaneus fracture surgery, and Singh and Viney10 reported on the need for cancellous iliac bone autograft. In these 2 studies, comparisons were made of the clinical and radiological results of patients with and without graft for Sanders Type 2–4 displaced intra-articular calcaneus fractures. No difference was determined between the groups with respect to functional results in either study, but more satisfactory radiological results were obtained with grafting. Therefore, Duymus et al9 reported that the use of bone grafts could be recommended and Singh and Viney10 reported that grafting of large cavities formed after reduction should be considered among the treatment options. Longino and Buckley12 investigated the effect on reduction quality of autologous bone supplementation. In that study, both Sanders Type 2 and Sanders Type 3 and 4 displaced intra-articular calcaneus fractures were evaluated, and it was reported that no objective radiological or functional benefit could be determined from bone graft supplementation.12 In contrast to these more recent studies, Leung et al24,25 stated that ORIF applied using bone graft was the treatment method that should be the primary preference for calcaneus fractures. While in the older studies the use of graft was keenly recommended, in the recent studies the efficiency and necessity of grafts in calcaneal fractures became controversial. We think that this contrasting view may occur as a result of the currently more widespread use of perioperative imaging methods, established surgical principles, and developed implant technologies. There is also a need for further studies to be made on calcaneus fractures with more homogenized groups. Sanders Type 2 and 4 fractures should not be included in the same cohort. The ideal evaluation method would be to make comparisons within the group for each type of fracture.
In the current study, only Sanders Type 3 and Type 4 displaced intra-articular calcaneus fractures were evaluated. By providing mechanical support with tri-cortical iliac crest bone autograft, it was investigated whether or not there was any additional contribution to stability. No difference was found between the groups in terms of clinical results. Radiologically, the degree of change in Bohler’s angle, Gissane’s angle and calcaneal height was not significantly different between the groups. These results indicate that graft does not provide additional stability. Although, no difference was found in early and late Bohler’s angle and calcaneal height values of the groups, only the early and late Gissane’s angle values of the Group A were lower than that of the Group B. We think that this finding is not relevant with our hypothesis but indicates the quality of the fracture reduction so does not affect the conclusions of our study. If these grafts made additional contributions to a level that would affect the clinical and radiological results, the loss of Bohler angle and height in the nongraft group after full weight-bearing should have been at a higher significant level. However, the results of this study showed no difference between patients where graft was and was not used with respect to the rates of loss in the final measurement values. This can be interpreted as the tri-cortical iliac crest bone autografts having made no additional contribution to the protection of stability in Sanders Type 3 and 4 calcaneus fractures fixed with locking plate. Thus it can be considered that following appropriate reduction, fixation made using a locking plate is sufficient.
There have been studies in the literature where grafts have been associated with higher infection rates.29–31 Benirschke and Kramer32 declared a 1.8% and Sanders et al5 declared a 2% deep infection rate after ORIF. Duymus et al9 reported a 12.5% superficial infection rate after ORIF. Superficial infection developed in 1 case (1/29=3.5%) and deep infection developed in 1 case (1/29=3.5%) in our study. The 2 cases which developed infections were both in the group where graft had been used (2/16=12.5%). Although there was no statistically significant difference, the infection rate was greater in the group with graft. If we had had a bigger sample size, this difference might have become clear. The procedure of bone autograft harvesting may increase the operative time in calcaneal fractures, and thus this situation may increase the infection rate.
The strengths of this study are that all the operations were performed by the same surgeon, the same type of locking plate was used for all fractures, only tri-cortical iliac bone autograft was used, and evaluation of the clinical and radiological results was made by an independent observer. However the weak points of this study were that it was made on a cohort which could be considered to be extremely homogenous, it was retrospective and so there was no specific randomization method for the decision of performing a bone graft, the number of patients was low, and the follow-up period was relatively short. We think that there is a need for further studies which have more extensive and homogenous series (only Sanders Type 3, only Sanders Type 4).
Conclusion
As there was no additional positive contribution to the clinical and radiological results, thus iliac bone autografts should not be considered necessary in calcaneus fracture surgery. Fixation applied with locking plate is sufficient. When the potential complications have been considered, we think that autografts are not essential.
Disclosure
The authors report no conflicts of interest in this work.
References
Bajammal S, Tornetta P 3rd, Sanders D, Bhandari M. Displaced intra-articular calcaneal fractures. J Orthop Trauma. 2005;19(5):360–364. | ||
Mitchell MJ, McKinley JC, Robinson CM. The epidemiology of calcaneal fractures. Foot (Edinb). 2009;19(4):197–200. | ||
Sanders RW, Clare MP. Fractures of the calcaneus. In: Bucholz RW, Heckman JD, Court-Brown CM, Tornetta P, editors. Rockwood and Green’s Fractures in Adults. 8th ed. Vol. 2. Philadelphia, PA: Lippincott Williams and Wilkins; 2006:2293–2336. | ||
Al-Ashhab ME. Treatment for calcaneal malunion. Eur J Orthop Surg Traumatol. 2013;23(8):961–966. | ||
Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87–95. | ||
Sanders R, Vaupel ZM, Erdogan M, Downes K. Operative treatment of displaced intraarticular calcaneal fractures: long-term (10–20 years) results in 108 fractures using a prognostic CT classification. J Orthop Trauma. 2014;28(10):551–563. | ||
van Tetering EA, Buckley RE. Functional outcome (SF-36) of patients with displaced calcaneal fractures compared to SF-36 normative data. Foot Ankle Int. 2004;25(10):733–738. | ||
Khorbi A, Chebil M, Ben Maitigue M, et al. [Screw fixation without bone graft of calcaneal joint fractures: 35 cases]. Rev Chir Orthop Reparatrice Appar Mot. 2006;92(1):45–51. French. | ||
Duymus TM, Mutlu S, Mutlu H, Ozel O, Guler O, Mahirogullari M. Need for bone grafts in the surgical treatment of displaced intra-articular calcaneal fractures. J Foot Ankle Surg. 2017;56(1):54–58. | ||
Singh AK, Vinay K. Surgical treatment of displaced intra-articular calcaneal fractures: is bone grafting necessary? J Orthop Traumatol. 2013;14(4):299–305. | ||
Yang Y, Zhao H, Zhou J, Yu G. Treatment of displaced intraarticular calcaneal fractures with or without bone grafts: a systematic review of the literature. Indian J Orthop. 2012;46(2):130–137. | ||
Longino D, Buckley RE. Bone graft in the operative treatment of displaced intraarticular calcaneal fractures: is it helpful? J Orthop Trauma. 2001;15(4):280–286. | ||
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. | ||
Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg. 2007;46(2):65–74. | ||
Silva LC, Heck JM, Guerra MT. Surgical treatment of intraarticular fractures of the calcaneus: comparison between flat plate and calcaneal plate. Rev Bras Ortop. 2016;52(1):29–34. | ||
Chen CH, Hung C, Hsu YC, Chen CS, Chiang CC. Biomechanical evaluation of reconstruction plates with locking, nonlocking, and hybrid screws configurations in calcaneal fracture: a finite element model study. Med Biol Eng Comput. 2017;55(10):1799–1807. | ||
Zhang F, Tian H, Li S, et al. Meta-analysis of two surgical approaches for calcaneal fractures: sinus tarsi versus extensile lateral approach. ANZ J Surg. 2017;87(3):126–131. | ||
Falis M, Pyszel K. Treatment of displaced intra-articular calcaneal fractures by intramedullary nail. Preliminary report. Ortop Traumatol Rehabil. 2016;18(2):141–147. | ||
El-Desouky II, Abu Senna W. The outcome of super-cutaneous locked plate fixation with percutaneous reduction of displaced intra-articular calcaneal fractures. Injury. 2017;48(2):525–530. | ||
Lian K, Lu H, Guo X, Cui F, Qiu Z, Xu S. The mineralized collagen for the reconstruction of intra-articular calcaneal fractures with trabecular defects. Biomatter. 2013;3(4):pii: e27250. | ||
Stoffel K, Booth G, Rohrl SM, Kuster M. A comparison of conventional versus locking plates in intraarticular calcaneus fractures: a biomechanical study in human cadavers. Clin Biomech (Bristol, Avon). 2007;22(1):100–105. | ||
Richter M, Gosling T, Zech S, et al. A comparison of plates with and without locking screws in a calcaneal fracture model. Foot Ankle Int. 2005;26(4):309–319. | ||
Kayali C, Altay T, Kement Z, Citak C, Yagdi S. The effect of early weight-bearing on comminuted calcaneal fractures treated with locking plates. Eklem Hastalik Cerrahisi. 2014;25(2):85–90. | ||
Leung KS, Yuen KM, Chan WS. Operative treatment of displaced intra articular fractures of the calcaneus. Medium-term results. J Bone Joint Surg Br. 1993;75(2):196–201. | ||
Leung KS, Chan WS, Shen WY, Pak PL, So WS, Leung PC. Operative treatment of intra-articular fractures of the os calcis-the role of rigid internal fixation and primary bone grafting: preliminary results. J Orthop Trauma. 1989;3(3):232–240. | ||
Di Schino M, Bensaida M, Vandenbussche E, Augereau B, Nich C. Results of open reduction and cortico-cancellous autograft of intra-articular calcaneal fractures according to Palmer. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8):e8–e16. | ||
Elsner A, Jubel A, Prokop A, Koebke J, Rehm KE, Andermahr J. Augmentation of intraarticular calcaneal fractures with injectable calcium phosphate cement: densitometry, histology, and functional outcome of 18 patients. J Foot Ankle Surg. 2005;44(5):390–395. | ||
Gusic N, Fedel I, Darabos N, et al. Operative treatment of intraarticular calcaneal fractures: anatomical and functional outcome of three different operative techniques. Injury. 2015;46(Suppl 6):S130–S133. | ||
Calori GM, Mazza E, Colombo M, Ripamonti C. The use of bone-graft substitutes in large bone defects: any specific needs? Injury. 2011;42(Suppl 2):S56–S63. | ||
Gupta AR, Shah NR, Patel TC, Grauer JR. Perioperative and long-term complications of iliac crest bone graft harvesting for spinal surgery: a quantitative review of the literature. Intern Med J. 2001;8(3):163–166. | ||
Laurie SW, Kaban LB, Mulliken JB, Murray JE. Donor-site morbidity after harvesting rib and iliac bone. Plast Reconstr Surg. 1984;73(6):933–938. | ||
Benirschke SK, Kramer PA. Wound healing complications in closed and open calcaneal fractures. J Orthop Trauma. 2004;18(1):1–6. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



