Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Same-Day ART Initiation and Associated Factors Among People Living with HIV on Lifelong Therapy at Nekemte Specialized Hospital, Western Ethiopia
Authors Bayisa L , Bayisa D , Turi E , Mulisa D , Tolossa T , Akuma AO , Bokora MC , Rundasa DT
Received 2 November 2022
Accepted for publication 13 January 2023
Published 24 January 2023 Volume 2023:15 Pages 11—22
DOI https://doi.org/10.2147/HIV.S395238
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Lami Bayisa,1 Diriba Bayisa,2 Ebisa Turi,3 Diriba Mulisa,1 Tadesse Tolossa,3 Adugna Olani Akuma,1 Merga Chala Bokora,2 Dawit Tesfaye Rundasa1
1Department of Nursing, School of Nursing and Midwifery, Wollega University, Nekemte, Ethiopia; 2Department of Midwifery, School of Nursing and Midwifery, Wollega University, Nekemte, Ethiopia; 3Department of Public Health, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
Correspondence: Lami Bayisa, Department of Nursing, School of Nursing and Midwifery, Wollega University, P.O.Box: 395, Nekemte, Ethiopia, Tel +251 924318135, Email [email protected]
Background: The test-and-treat approach recommends early ART initiation (same day). Early ART start has double the benefits as treatment and as prevention. However, there is limited information regarding same-day ART initiation in Ethiopia. Hence, this study aimed to assess the magnitude and factors of same-day ART initiation among people living with HIV (PLHIV) on ART at Nekemte specialized hospital, in Western Ethiopia.
Methods: A cross-sectional study was conducted among 483 PLHIV from January 10 to February 15, 2021. Data were collected using an investigator-administered questionnaire. Epi Data 3.1 and STATA 14.0 were used for data entry and analysis, respectively. Variables with P-value < 0.25 from bivariable analysis were included in the multivariable analysis. AOR with 95% CI and P-value < 0.05 were used to declare statistical significance.
Results: A total of 483 study subjects participated and gave a 100% response rate. Two thirds (65%) of them started ART on the same day with a 95% CI [60.2– 68.8]. Urban dwellers (AOR = 3.93 (95% 1.96– 7.87)), with no OIs (AOR = 4.02 (95% CI: 1.54– 10.47)), not screened for TB (AOR = 6.02 (95% CI: 1.71– 21.15)), tested via VCT (AOR = 2.32 (95% CI: 1.37– 3.26)), who have not used CPT (AOR = 1.88 (95% CI: 1.10– 3.23)), who have not used IPT (AOR = 2.36 (95% CI: 1.0– 5.57)), who were tested in 2019/20 (AOR = 2.37 (95% CI: 1.08– 5.518)), and with BMI ≥ 25 kg/m2 (AOR = 2.18 (95% CI: 1.05– 4.52)) were significantly associated with same-day ART initiation.
Conclusion: Two thirds of study subjects initiated ART on the same day as HIV diagnosis. Voluntary testing and immediate referral to HIV care, advocating test-and-treat, and intensive counseling should be strengthened and reinforced for newly diagnosed HIV-positive people. Given that, high attention should be paid to individuals from urban residence, not screened for TB, who have not used CPT and IPT prophylaxis.
Keywords: antiretroviral therapy, ART initiation, same day
Introduction
Human immunodeficiency virus (HIV) infection remains a major public health concern in the world. Starting from the day it was declared a pandemic, it has claimed the lives of about 36.3 million people.1 In the last couple of decades, antiretroviral therapy (ART) has significantly improved the inhibition of virus multiplication and regeneration of immunity in HIV-infected individuals. However, worldwide, the spread of HIV has not been managed according to the best global interest. Yearly around 1.8 million new HIV infections are being diagnosed.2 To manage the wide spread of HIV infection successfully, sub-Saharan African countries (SSA) are struggling to diagnose 95% of HIV infections, initiate and retain 95% of HIV-diagnosed persons on ART, and reach reduced viral load of 95% for those who started receiving ART by customizing the Joint United Nation Program on HIV/AIDS (UNAIDS) goals of 90–90–90.3 The test and treat approach is currently implemented in all World Health Organization (WHO) member state countries including SSA. In the test and treat strategy, WHO recommended the immediate initiation of ART after a confirmed positive HIV test result regardless of the individual’s clinical and immunological status.4
Initiation of ART is categorized as early if started within 7 days and delayed if started after 7 days of confirmed diagnosis of positive HIV test result. Given that, immediate (same-day) ART initiation is when confirmed HIV infected individuals begin lifelong therapy immediately after diagnosis as swiftly as possible if there are no contraindications4,5
Same-day ART initiation was defined as acceptance of lifelong therapy on the day of HIV diagnosis and return to home with prescribed highly active antiretroviral therapy (HAART).5 Immediate ART treatment is believed to play a paramount role in realizing the ambitious plan of ending new HIV infections by 2030 that has been set by UNAIDS through providing health-related quality of life to people living with HIV (PLHIV).5 Furthermore, immediate ART initiation (same-day) after a confirmed HIV positive test result accelerates viral load suppression and in turn prevents the onward transmission of HIV via sexual route in particular.4 It improves the equity and accessibility of ART for people who are at risk of being lost to follow-up before initiating ART.6–9 Immediate ART initiation also reduces HIV-related morbidity and mortality among PLHIV.9 The immediate initiation of ART demands strict implementation of test and treat strategy, strong post-test counseling and proper referral of HIV infected individuals to ART units.
Despite the advantages of immediate (same-day) ART initiation, its uptake is poor in both developed and resource-limited settings including Ethiopia.10 For instance, in South Africa, the same-day initiation of ART was 40.1% from 2017 to 2018,11 in Taiwan, rapid initiation of ART was 68.3% in 2017.7 Similarly, in San Diego, 26% and 48% of newly diagnosed HIV-positive individuals started ART on the same day as diagnosis and within a week respectively.12
Patient’s decision, long time duration of settlement, expensive transport because of long distance from health institution, social discrimination, and worry of disclosure are factors of same-day ART initiation reported by previous studies.9–12
Other reasons for delayed ART uptake are staff scarcity, long waiting times, fear of drug adverse effects, being male, immature age, and the need to take time off work.13,14 Factors like juvenile age at diagnosis, lack of education, alternative ways of healing rather than ART drug use, acquiring HIV due to having different sexual partner, and feeling better are also associated with delayed ART initiation.10,15
In Ethiopia, several actions have been taken to strengthen the uptake of immediate (same-day) ART initiation for all newly diagnosed HIV infected individuals through providing empathy and care, continued counseling after test while delivering home advice, or social-worker’s attendance.16–18 However, there is limited information regarding same-day ART initiation among PLHIV in Ethiopia. Hence, this study aimed to assess the magnitude and determinants of same-day ART initiation among PLHIV who have initiated ART at Nekemte specialized hospital, in Western Ethiopia.
Methods
Study Design and Study Period
A facility-based cross-sectional study was conducted at Nekemte Specialized Hospital, Western Ethiopia from January 10 to February 15, 2021.
Study Area
The Nekemte Specialized Hospital is located in Nekemte town. Nekemte town is the capital city of East Wollega Zone that is 328 Km from Addis Ababa in a Western direction. The hospital started to provide ART services in 2005 G.C and currently, it is providing HIV-related services to more than 3000 adult HIV-positive individuals. Including the integrated ART services, the hospital is providing services to a catchment population of greater than three million people. The “test and treat” policy has been implemented in the hospital since our country Ethiopia subscribed to it in 2017 G.C and the HIV treatment cascade was adopted from the WHO which outlines early initiation of ART including the same day as confirmed HIV diagnosis.
Study Subjects
The HIV-positive individuals on ART who were being follow-up at Nekemte Specialized Hospital were the source population. The study population was the HIV-positive individuals on ART aged 18 years and above, who initiated ART since the test and treat strategy was applied in the hospital. The individuals with an unrecorded HIV diagnosis and ART initiation date were excluded from the study.
Study Variables
Dependent variable: same-day ART initiation.
Independent variables: 1) socio-demographic characteristics included: age, sex, religion, educational status, occupational status, and residence; 2) baseline clinical characteristics included: baseline CD4, WHO clinical stage, functional status, baseline viral load, BMI; 3) facility and structure related characteristics included: HIV test approach, year tested for HIV, site tested for HIV, use baseline CPT, use baseline IPT, and residing within catchment area; 4) personal and family-related characteristics included: HIV disclosure status, having regular partner, partner’s HIV status, and presence of <15 children in the family.
Sample Size and Sampling Procedure
The sample size was calculated using a single population proportion formula with the assumption of a 95% confidence interval, 5% margin of error, taking 41.9%10,15 magnitude of same-day ART initiation from a previous study conducted at Bahr Dar and considering 20% no response rate. The systematic sampling method was used to recruit 483 study participants. The medical registration number of the study participants given for their routine follow-up was used as a sampling frame. Accordingly, about 1447 study participants had registered to have follow-up during study period. Given that, we recruited the study participants using every third person (k=3) method while the first participant was selected with lottery method.
Data Collection Instrument and Procedure
The data were collected through an investigator-administered pre-designed questionnaire. The questionnaire was prepared in English, translated into Afaan Oromoo for data collection, and then re-translated back into English to maintain consistency. Medical records were reviewed to obtain relevant medical history and laboratory parameters from the HIV intake form and ART follow-up format. Participants were interviewed to obtain socio-demographic data. One supervisor (BSc in public health), and two data collectors (clinical nurses) participated in the data collection process. Quality of data was maintained throughout; a pre-test was done on 5% of the determined sample size and the necessary amendment was conducted based on the result, two days of training were given for data collectors and supervisors. Principal investigators checked the completeness of data on a daily basis.
Data Management and Analysis
Data were entered into a computer using EPI data software version 3.01 statistical programs. Data were cleaned and exported to STATA windows version 14.0 for further analysis. The Hosmer and Lemeshow goodness-of-fit was used to check the model fitness (P>0.05) and we used the receiver operating characteristics curves (ROC) to check the model accuracy. Furthermore, we checked for the existence of multi-collinearity through variance inflation factor (VIF), and then the highly correlated variables were identified via correlation matrix, and removed to solve the problem. The participants’ characteristics were reported as a count or percentages for categorical variables, and mean with standard deviation for continuous variables. Both bivariable and multivariable logistic regression analyses were performed to identify potential variables associated with same-day ART initiation. Those variables with a P-value of <0.25 in the bivariable analysis were included into multivariable analysis to control the possible effects of confounders. Adjusted odds ratio (AOR) with 95% CI and P-value of <0.05 were used to declare and report the statistical significance of variables associated with the outcome variable.
Ethical Consideration
Ethical clearance was obtained from the institutional review board (IRB) of the Institute of Health Sciences, Wollega University. A formal letter of permission was obtained from Nekemte Specialized Hospital medical director. Study participants were recruited only after informed written consent was obtained from each of them. All the data obtained were treated confidentially.
Results
Socio-Demographic Characteristics
In this research more than half of the participants, 265 (54.87%), were female; three out of five participants, 296 (61.28%), were married. Seventy-two participants (14.91%) had an educational level of more than college and above. The majority of study participants, 419 (86.75%), were urban dwellers (Table 1).
 |
Table 1 Socio-Demographic Characteristics of HIV-Infected People Who Have Initiated ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Stages of HIV/AIDS
To recognize the stage and progress of HIV/AIDS among the study participants at the time of ART initiation, the World Health Organization (WHO) clinical stage was used. Accordingly, nearly three fourths of the study participants, 372 (77.02%), were WHO clinical stage I. While a sizeable number of the study participants, 14.08% and 8.91%, were WHO clinical stage II and III/IV respectively (Figure 1).
 |
Figure 1 WHO HIV/AIDS clinical stage among patients who initiated ART at Nekemte specialized hospital, Ethiopia, 2021. |
Baseline Clinical and Hematological Characteristics
The majority of the participants, 320 (66.25%), had CD4 cell count of <500 cells/mm. A few participants, 42 (8.70%), had a viral load of ≥1000 copies/mL. Most of the study participants, 446 (92.34%), were diagnosed with working functional status. A few participants, 39 (8.07%), had a history of baseline OIs. Almost all participants, 460 (95.24%), were screened for TB (Table 2).
 |
Table 2 Baseline Clinical and Hematological Characteristics of HIV-Positive People Who Have Initiated ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Hospital Departments where Patients were Referred to the ART Unit
In the hospital, HIV testing is done at several departments. For instance, nearly one third of the study participants, 166 (34.37%), were screened at and referred to ART from OPD. In addition, a significant number of the study participants, 13.46% and 3.11%, were screened for HIV and referred to the ART unit from the TB clinic and STI clinic respectively (Figure 2).
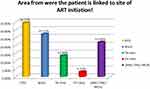 |
Figure 2 Department from which the patient was referred to the site of ART initiation among patients receiving ART at Nekemte specialized hospital, Western Ethiopia, 2021. |
Facility and Structure Related Characteristics
Regarding HIV test approaches, the majority of participants, 349 (72.26%), were tested via VCT. One hundred and thirty-two participants (27.33%) were tested in the year 2018. The majority of 429 (88.82%) participants were tested at the hospital. Fifty-four participants (11.18%) were from outside of the ART catchment area (Table 3).
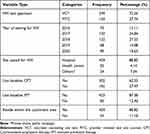 |
Table 3 Facility and Structure Related Characteristics of HIV-Positive People Who Have Initiated ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Personal and Family-Related Characteristics
The current study revealed that almost all participants, 465 (96.27%), had disclosed their HIV serostatus; of which more than half of the disclosure, 259 (55.46%), was to the spouse. Most, 436 (90.27), of the participants had a regular sexual partner. Nearly half [217 (49.89%)] of the study participants’ partners’ HIV status was positive. About two thirds, 316 (64.80%), of the study participants had less than five children in the family (Table 4).
 |
Table 4 Personal and Family-Related Characteristics of HIV Positive People Who Have Initiated ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Same-Day ART Initiation
Nearly two thirds (64.6%) of the study participants started ART on the same day as confirmed positive HIV test with 95% CI [60.2–68.8] (Figure 3).
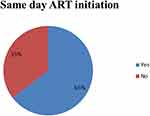 |
Figure 3 Magnitude of same-day ART initiation among HIV-positive people on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021. |
Factors Associated with Same-Day ART Initiation
Both binary and multiple logistic regressions were computed. From the bivariable logistic regression model, ten (10) variables were transferred into the multivariable logistic regression model. Then, seven (7) variables remained in the multivariable logistic regression analysis being independently and significantly associated with the outcome variable at the p-value of <0.05.
Accordingly, participants from an urban area revealed 4-fold higher odds of initiating ART on the same day as compared to those from a rural area (AOR= 3.93 (95% 1.96–7.87)). Also, odds for the same-day ART initiation were 4-fold higher in participants without baseline OIs (AOR=4.02 (95% CI 1.54–10.47)) as compared to those with baseline OIs. As well, the odds for same-day ART initiation were 6-fold higher in participants who did not screen for TB (AOR=6.02 (95% CI1.71–21.15)) as compared to their counterparts. Participants who tested via VCT showed odds of ART initiation on the same day of nearly 2-fold higher (AOR = 2.32 (95% CI: 1.37–3.26)) as compared to those tested via PITC. In addition, the odds for same-day ART initiation were 2-fold higher in participants who did not use baseline CPT (AOR= 1.88 (95% CI1.10–3.23)) as compared to those who used it. Furthermore, odds for same-day ART initiation were 2-fold higher in subjects who did not use IPT (AOR=2.36 (95%1.0–5.57)) as compared to their counterparts. Moreover, odds for same-day ART initiation were 2-fold higher in subjects tested for HIV in 2019/20 (AOR= 2.37 (95% CI1.08–5.518)) as compared to participants tested in 2016. Additionally, odds for same-day ART initiation were two fold higher in individuals with obese nutritional status (BMI ≥25 kg/m2) (AOR=2.18 (95% CI (2.18 (1.05–4.52)) as compared to underweight subjects (BMI ≤17.99 kg/m2) (Table 5).
Discussion
Same-day ART initiation is the ideal program that increases the number of people starting ART and it is an entry point for successful treatment outcome. The current study found that the prevalence of same-day ART initiation was 64.6% (95% CI, 60.2–68.8). This figure indicates the improvement of immediate lifelong therapy commencement uptake in the study area. Surprisingly, more than three out of four newly diagnosed HIV infected individuals initiated the ART within a week of confirmed positive HIV test result. This finding highlights the feasibility of same-day ART initiation in the study area and it is supported by the study conducted in Estawin: 63%.19
However, this finding is higher than that of a prospective study done in North Ethiopia which reported a same-day ART initiation of 40.9%,10 multi-national research conducted in Africa,20 and studies conducted in South Africa which reported a magnitude of same-day ART initiation of 36%,21 40.4%,11 and 20.2%22 respectively. The discrepancy might be due to the difference in the study period; the previous studies were conducted earlier when the test and treat approach guideline was being developed and there might have been resistance to its implementation. However, the current study was conducted after a couple of strategies and policies had been developed to retain patients on lifelong therapy. In addition, patients’ uptake of the same-day ART initiation increased over time due to improved readiness of the health system in providing education and counseling regarding the advantage of initiating ART as early as possible. Accordingly, to scale up the same-day ART initiation, different training has been provided to healthcare providers advocating the importance of early ART initiation for HIV-infected individuals regardless of their clinical and immunological status.
Likewise, the finding of this study is lower than that of a prospective study conducted among pregnant women in South Africa in which the magnitude of same-day ART initiation was reported as 73%.23 The difference might be due to the study population variation. The previous study was conducted among pregnant women under universal ART treatment. Pregnant women under Option B+ eliminates the need for CD4 enumeration and identification of the WHO clinical stage of the disease which may increase the chance of HIV-infected pregnant women starting lifelong therapy on the day of their first ANC visit – “same-day” ART initiation.
Regarding the factors influencing same-day ART initiation, this study revealed that the likelihood of initiating ART on the same day as confirmed HIV-positive diagnosis was four fold higher among patients who were urban dwellers than their counterparts. This finding is supported by a study conducted in the USA.24 The possible reason for the late initiation of ART for rural dwellers might be due to low access to information and health facilities, the long distance of health facilities from their home which is related to the cost of transportation process,25 and fear of stigma.
Furthermore, the odds of same-day ART initiation were 4 times higher among patients without opportunistic infection as compared to patients with opportunistic infection. This is in line with previous studies conducted in Ethiopia10 and South Africa11 in which patients who presented with advanced clinical features were less likely to initiate ART on the day of HIV diagnosis. However, this finding is in contrast with qualitative studies conducted in Ethiopia26 and Kampala,25 in which asymptomatic clients refused to initiate ART immediately following HIV-positive test results. The finding of the previous study pointed out that the reason for refusal of treatment on the day of HIV diagnosis was fear of the adverse psychological effect of treatment, mistrust of the HIV test result, and they prefer to use holy water and traditional medicine as an alternative treatment.
Again, in this study, those who had not been screened for tuberculosis were six times more likely to initiate ART during the first day of confirmed HIV-positive diagnosis than their counterparts. The delay of ART initiation among patients screened for TB could be explained by the fact that ART may be briefly delayed while investigating to identify people who should be either accelerated for TB diagnosis or given preventive TB therapy. Regarding TB/HIV co-infection, the WHO recommends that TB treatment should be initiated first, followed by ART.4
Furthermore, this research finding revealed that those who did not take IPT on the first day were nearly 2 times more likely to initiate ART on the same day as confirmed HIV-positive diagnosis than their counterparts. Patients who are taking IPT may take some time to start ART initiation due to the necessity of conducting a different investigation to screen for active TB disease before initiation of TB preventive therapy to avoid giving one anti-tuberculosis drug to patients with TB disease who require a full treatment regimen.27
The result from this finding showed that those who recently tested HIV positive were two times more likely to initiate ART on the first day as compared with those who tested HIV positive in 2016. The increment in same-day ART initiation among patients diagnosed recently could be due to a new recommendation that all HIV-infected people should start ART irrespective of their clinical or immune status endorsed by WHO in 2014, which Ethiopia subscribed to and has been following since 2016 (its national guideline).28
Regarding body mass index, participants with BMI ≥25 kg/m2 are two times more likely to initiate ART on the first day of confirmed positive test than their counterparts. Relatively, being obese is a major risk factor for developing type II diabetes which may impair immune response. Therefore, obese HIV patients are encouraged to start ART the same day, as healthcare providers may give special consideration and push obese HIV patients to start ART treatment immediately due to the fear of HIV infection and obesity compounding the risk of morbidity and mortality.
Limitations of the Study
Social desirability bias may have affected this study due to the persistent nature of HIV and stigma linkage in the community. The inclusion of participants with OIs in this study may have underestimated the magnitude of same-day ART initiation. Moreover, this study investigated factors only from the patient’s side and facility characteristics though the healthcare providers’ perspective on same-day ART initiation remained unexplained. Thus, further study is recommended to identify providers’ related factors to same-day ART initiation.
Conclusion and Recommendation
In the current study, two thirds of study subjects initiated ART on the same day as HIV diagnosis in the study area. Voluntary testing, immediate referral to HIV care, advocating test-and-treat, and intensive counseling should be strengthened, and reinforced for newly diagnosed HIV-positive people. Given that, high attention should be paid to individuals from urban residence, not screened for TB, who have not used CPT and IPT prophylaxis.
Data Sharing Statement
All produced and analyzed data are included in this manuscript.
Ethical Approval and Consent from the Participants
Ethical clearance was obtained from the institutional review board (IRB) of the Institute of Health Sciences, Wollega University. A formal letter of permission was obtained from Nekemte Specialized Hospital medical director. Study participants were recruited only after informed written consent was obtained from each of them. All the data were obtained anonymously and treated confidentially. All the procedures of data collection were conducted according to the principles of the Helsinki Declaration.
Acknowledgment
We are thankful to the data collectors, supervisors, and study participants; it was due to them that this study was completed successfully.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. World Health Organization. World Health Organization HIV/AIDS fact sheet; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
2. Peter E, Kamath R, Andrews T, et al. Psychosocial determinants of health-related quality of life of people living with HIV/AIDS on antiretroviral therapy at Udupi District, Southern India. Int J Prev Med. 2014;5(2):203.
3. World Health Organization. WHO Guidelines Approved by the Guidelines Review Committee, in Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach. Geneva: World Health Organization Copyright © World Health Organization; 2016.
4. World Health Organization. Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy, July 2017; 2017.
5. Boyd M, Boffito M, Castagna A, et al. Rapid initiation of antiretroviral therapy at HIV diagnosis: definition, process, knowledge gaps. HIV Med. 2019;20:3–11. doi:10.1111/hiv.12708
6. Rodger AJ, Cambiano V, Bruun T, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet. 2019;393(10189):2428–2438. doi:10.1016/S0140-6736(19)30418-0
7. Huang Y-C, Sun H-Y, Chuang Y-C, et al. Short-term outcomes of rapid initiation of antiretroviral therapy among HIV-positive patients: real-world experience from a single-center retrospective cohort in Taiwan. BMJ Open. 2019;9(9):e033246. doi:10.1136/bmjopen-2019-033246
8. Bacon O, Chin JC, Hsu L, Cohen S, Sachdev D, Havlir D. The rapid ART program initiative for HIV diagnoses (RAPID) in San Francisco.
9. Zhao Y, Wu Z, McGoogan JM, et al. Immediate antiretroviral therapy decreases mortality among patients with high CD4 counts in China: a nationwide, retrospective cohort study. Clin Infect Dis. 2018;66(5):727–734. doi:10.1093/cid/cix878
10. Moges NA, Adesina OA, Okunlola MA, et al. Same-day antiretroviral treatment (ART) initiation and associated factors among HIV positive people in Northwest Ethiopia: baseline characteristics of a prospective cohort. Arch Public Health. 2020;78(1):1–13. doi:10.1186/s13690-020-00473-4
11. Lilian RR, Rees K, McIntyre JA, et al. Same-day antiretroviral therapy initiation for HIV-infected adults in South Africa: analysis of routine data. PLoS One. 2020;15(1):e0227572. doi:10.1371/journal.pone.0227572
12. Hoenig M, Marchetti L, Parlanti P, et al. Rapid HIV viral load suppression in those initiating antiretroviral therapy at the first visit after HIV diagnosis. Sci Rep. 2016;6(1):1–5. doi:10.1038/s41598-016-0001-8
13. Lee MJ, Venturelli S, McKenna W, et al. Reasons for delayed antiretroviral therapy (ART) initiation in the era of early ART initiation guidelines: a retrospective service evaluation. Int J STD AIDS. 2019;30(4):415–418. doi:10.1177/0956462418814985
14. Govindasamy D, Ford N, Kranzer K. Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: a systematic review. AIDS. 2012;26(16):2059–2067. doi:10.1097/QAD.0b013e3283578b9b
15. Croxford S, Yin Z, Burns F, et al. Linkage to HIV care following diagnosis in the WHO European Region: a systematic review and meta-analysis, 2006–2017. PLoS One. 2018;13(2):e0192403. doi:10.1371/journal.pone.0192403
16. Wynberg E, Cooke G, Shroufi A, et al. Impact of point‐of‐care CD4 testing on linkage to HIV care: a systematic review. J Int AIDS Soc. 2014;17(1):18809. doi:10.7448/IAS.17.1.18809
17. Kohler PK, Chung MH, McGrath CJ, et al. Implementation of free cotrimoxazole prophylaxis improves clinic retention among antiretroviral therapy-ineligible clients in Kenya. AIDS. 2011;25(13):1657. doi:10.1097/QAD.0b013e32834957fd
18. Cantrell RA, Sinkala M, Megazinni K, et al. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2008;49(2):190–195. doi:10.1097/QAI.0b013e31818455d2
19. Kerschberger B, Boulle A, Kuwengwa R, et al. The impact of same-day antiretroviral therapy initiation under the World Health Organization treat-all policy. Am J Epidemiol. 2021;190(8):1519–1532. doi:10.1093/aje/kwab032
20. Boeke CE, Joseph J, Wang M, et al. Point‐of‐care testing can achieve a same‐day diagnosis for infants and rapid ART initiation: results from government programs across six African countries. J Int AIDS Soc. 2021;24(3):e25677. doi:10.1002/jia2.25677
21. Joseph Davey D, Kehoe K, Serrao C, et al. Same‐day antiretroviral therapy is associated with increased loss to follow‐up in South African public health facilities: a prospective cohort study of patients diagnosed with HIV. J Int AIDS Soc. 2020;23(6):e25529. doi:10.1002/jia2.25529
22. Onoya D, Sineke T, Hendrickson C, et al. Impact of the test and treat policy on delays in antiretroviral therapy initiation among adult HIV positive patients from six clinics in Johannesburg, South Africa: results from a prospective cohort study. BMJ Open. 2020;10(3):e030228. doi:10.1136/bmjopen-2019-030228
23. Langwenya N, Phillips TK, Brittain K, et al. Same‐day antiretroviral therapy (ART) initiation in pregnancy is not associated with viral suppression or engagement in care: a cohort study. J Int AIDS Soc. 2018;21(6):e25133. doi:10.1002/jia2.25133
24. Lopes BL, Eron JJ, Mugavero MJ, et al. HIV care initiation delay among rural residents in the Southeastern United States, 1996 to 2012. J Acquir Immune Defic Syndr. 2017;76(2):171. doi:10.1097/QAI.0000000000001483
25. Lankowski AJ, Siedner MJ, Bangsberg DR, et al. Impact of geographic and transportation-related barriers on HIV outcomes in sub-Saharan Africa: a systematic review. AIDS Behav. 2014;18(7):1199–1223. doi:10.1007/s10461-014-0729-8
26. Moges NA, Adesina OA, Okunlola MA, et al. Barriers and facilitators of same-day antiretroviral therapy initiation among people newly diagnosed with HIV in Ethiopia: qualitative study using the transtheoretical model of behavioral change. J Multidiscip Healthc. 2020;13:1801. doi:10.2147/JMDH.S282116
27. Ethiopia, F.M.o.H.o. Implementation Guideline for TB/HIV Collaborative Activities in Ethiopia. Federal Ministry of Health Addis Ababa; 2007.
28. Ethiopia, F.M.o.H. National Consolidated Guidelines for Comprehensive HIV Prevention, Care and Treatment. FMOH Ethiopia Addis Ababa; 2018.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

