Back to Journals » Local and Regional Anesthesia » Volume 16
Safety of Cubital Tunnel Release Under General versus Regional Anesthesia
Authors Carlson Strother CR, Dittman LE, Rizzo M, Moran SL, Rhee PC
Received 16 February 2023
Accepted for publication 1 June 2023
Published 7 July 2023 Volume 2023:16 Pages 91—98
DOI https://doi.org/10.2147/LRA.S389011
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Courtney R Carlson Strother,1 Lauren E Dittman,1 Marco Rizzo,1 Steven L Moran,2 Peter C Rhee1
1Department of Orthopedic Surgery, Mayo Clinic, Rochester, MN, USA; 2Department of Plastic Surgery, Mayo Clinic, Rochester, MN, USA
Correspondence: Peter C Rhee, Department of Orthopedic Surgery, Mayo Clinic, 200 1st Street SW, Rochester, MN, USA, 55905, Tel +1 507-284-3422, Fax +1 507-266-2533, Email [email protected]
Purpose: The aim of this study was to evaluate the occurrence of early (< 6 weeks) post-operative complications following ulnar nerve decompressions at the cubital tunnel performed under regional anesthesia compared to those performed under general anesthesia.
Methods: In situ ulnar nerve decompressions at the cubital tunnel performed at a single institution from 2012 through 2019 were retrospectively reviewed. Post-operative complications were compared between subjects who underwent the procedure with regional versus general anesthesia.
Results: Ninety-one ulnar nerve in situ decompressions were included in the study, which were performed under regional anesthesia in 55 and general anesthesia in 36 cases. The occurrence of post-operative complications was not significantly different between patients who received regional (n = 7) anesthesia and general (n = 8) anesthesia. None of the complications were directly attributed to the type of anesthesia administered. The change in pre- and post-operative McGowan scores were not significantly different between anesthesia groups (p = 0.81).
Conclusion: In situ ulnar nerve decompression at the cubital tunnel under regional anesthesia does not result in increased post-operative complications compared to those surgeries performed under general anesthesia. In situ ulnar nerve decompression performed under regional anesthesia is a safe and reliable option for patients who wish to avoid general anesthesia.
Level of Evidence: III.
Keywords: cubital tunnel, regional anesthesia, ulnar neuropathy
Plain Language Summary
The goal of this study was to compare the safety of general anesthesia or a nerve block that makes the arm numb in patients (otherwise known as regional anesthesia) who have their ulnar nerve released near their elbow. After comparing the outcomes in patients who had their ulnar nerve released at their elbow, we did not find any difference in complications between the two different types of anesthesia. Nerve blocks to the arm is a safe and reliable option of anesthesia to have for ulnar nerve release surgery for patients wishing to avoid general anesthesia.
Introduction
Cubital tunnel syndrome is the second most common upper extremity compressive neuropathy.1 In patients that have failed conservative management, surgical options include in situ decompression, medial epicondylectomy, and various forms of ulnar nerve anterior transpositions at the elbow.2 A recent meta-analysis demonstrated open in situ ulnar nerve decompressions to have the best outcomes and lowest incidence of complications in treatment of primary cubital tunnel syndrome. In situ ulnar nerve decompressions have increased in the United States in recent decades, which can be performed under local, regional, or general anesthesia.3,4
The choice of anesthesia for upper extremity procedures is a complex decision that must be discussed between the patient, surgeon, and anesthesiologist. Regional anesthesia and general anesthesia have their own risks and benefits that must be individualized to each patient. General anesthesia requires intubation, stresses the cardiovascular system, and can cause post-operative nausea and vomiting.5 Conversely, regional anesthesia avoids intubation but requires patient cooperation and some patients require unexpected conversion to general anesthesia if the block does not provide adequate analgesia.5 In addition, while rare, reports of perioperative nerve injury from peripheral nerve blocks raise a concern for their use in select patients by some anesthesiologists.6,7 In particular, patients with preexisting peripheral neuropathy are thought to theoretically be at a higher risk of suffering new or worsening neurologic symptoms or dysfunction. This is derived from the “double crush” or “double hit” phenomenon, where nerves compressed in one region are thought to be more susceptible to impaired function if compressed or injured in a second location within the same nerve.8
The appropriateness and efficacy of ulnar nerve in situ decompression under regional anesthesia or peripheral nerve blocks has not been reported. Therefore, the purpose of this study was to compare the safety of in situ ulnar nerve decompression performed under regional anesthesia compared to general anesthesia.
Materials and Methods
Following institutional review board approval and in compliance with the Declaration of Helsinki, ulnar nerve in situ decompressions at the cubital tunnel performed at a single institution from 2012 through 2019 were retrospectively reviewed. Due to the retrospective nature of the review, written informed consent requirement was waived by the Mayo Clinic institutional review board. Data was maintained with confidentiality. Two hundred and twenty adult (age 18 years and older) patients were initially identified based on CPT codes and ICD-9/ICD-10 codes. Patients with a clinical diagnosis of ulnar neuropathy, defined by history and physical exam of numbness and/or weakness in the ulnar nerve distribution with or without evidence of ulnar neuropathy on electrodiagnostic studies (nerve conduction velocity and electromyography), were included. Patients who had prior ulnar nerve surgery (n = 50) or those who underwent ulnar nerve transposition or medial epicondylectomy (n = 67) were excluded. Additionally, patients who underwent ulnar nerve decompression following trauma (n = 6), in conjunction with elbow oncologic procedures (n = 4), or in the setting of elbow arthroplasty were excluded (n = 1).
In situ ulnar nerve decompressions were performed in 92 surgeries on 80 patients by three senior hand surgeons at a single institution (S.L.M., M.R., P.C.R.). One patient’s surgery was performed under local anesthetic with moderate sedation and was excluded from the analysis. In total, 91 cases were included in this study, and an in-depth chart review was performed on each subject. Investigated variables included method of anesthesia (regional versus general), pre- and post-operative McGowan scores,9 and post-operative complications occurring within 6 weeks after surgery in parallel to the American College of Surgeons National Surgery Quality Improvement Project (NSQIP) which reports complications and adverse events up to 30 days post-operative.10 Complications were defined as any outcome that required additional care related to the patient’s surgery beyond the expected postoperative recovery, including additional patient phone calls, clinical visits, or emergency department visits. In addition, administration of an adjuvant intraoperative local block, conversion from regional to general anesthesia, and concomitant Guyon’s canal release were evaluated. Medical records were reviewed to obtain demographic information including age, gender, body mass index (BMI), comorbidities, pre-operative electrodiagnostic testing results when available, and duration of tourniquet inflation. Primary outcome measures included any post-operative complications and pre- to post-operative change in McGowan scores. The postoperative complication of severe swelling was defined by patient reporting marked and bothersome increase in size of their operative extremity relative to the unoperated arm.
A chi-squared test was used to compare the rates of post-operative complications between patients who underwent in situ ulnar nerve decompression with regional versus general anesthesia and to evaluate the change in pre- to post-operative McGowan scores between the two groups. Statistical significance was set at p<0.05. Patient’s cohort was dependent on the initial planned form of anesthesia. For example, patients who received regional anesthesia who failed to have adequate analgesia and were subsequently intubated for the procedure were still analyzed as part of the regional anesthesia group.
Results
Of the 91 included elbows, 55 in situ ulnar nerve decompressions were performed under regional anesthesia and 36 under general anesthesia. Demographic information is shown in Table 1. A tourniquet was used in all but one case in the regional anesthesia group and two cases in the general anesthesia group. Among those who underwent regional anesthesia, five subjects received supplemental intra-operative local anesthetic injections (9.1%) at the surgical site, and eleven subjects in the general anesthesia cohort received supplemental intra-operative local anesthetic injections (30.6%). This was the only characteristic that was significantly different between anesthesia groups (p = 0.008). Concomitant Guyon’s canal release was performed in 5 (9.1%) and 5 (13.9%) cases under regional and general anesthesia, respectively. One (1.8%) patient in the regional anesthesia cohort and 2 (5.6%) subjects in the general anesthesia cohort spent one night in the hospital post-operatively for pain control.
 |
Table 1 Baseline Characteristics |
Within the regional anesthesia group, supraclavicular nerve blocks were most commonly utilized (n = 30, 54.6%), followed by axillary (19, 34.6%) and infraclavicular blocks (6, 10.9%). The type of local anesthetic used for the block was reported in 53 patients (96.4%) and included lidocaine, bupivacaine, and mepivacaine with or without epinephrine. Six patients (10.9%) required conversion to general anesthesia due to inadequate intra-operative pain control. Characteristics of these 6 patients are further described in Table 2. In addition, 5 (9.1%) patients in the regional anesthesia group discharged to home with an in-dwelling continuous anesthetic delivery nerve catheter for 1–2 days post-operative.
 |
Table 2 Characteristics of Failed Brachial Plexus Blocks |
Post-operative complications were not significantly different between the regional (7 patients, 12.7%) and general anesthesia (8 subjects, 22.2%) groups (p = 0.233) (Table 3). Three patients had more than one complication in the regional anesthesia cohort, and one patient had multiple complications in the general anesthesia cohort—all of these cases consisted of pain and severe swelling in the operative extremity. Worsening pain was attributed to the post-operative dressing in 5 of the 9 cases with full resolution after dressing modification or removal. One patient in the general anesthesia cohort experienced post-operative neuropathic pain within the distribution of the ulnar nerve. None of the patients in this study required a return to the operating room for complications regarding their cubital tunnel surgery in the initial six-week follow-up period. One patient in the regional anesthetic group passed away in six weeks following surgery due to medical causes unrelated to the procedure.
 |
Table 3 Complications |
The pre- to post-operative change in McGowan scores was not significantly different between anesthesia groups (p = 0.81) (Table 4). The majority of patients had no change in McGowan scores at 6 weeks post-operatively when performed under regional anesthesia (n = 33, 60%) and general anesthesia (24, 66.7%). No patient’s McGowan score worsened at 6 weeks follow-up.
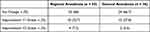 |
Table 4 Postoperative Change in McGowan Score |
Subgroup analysis in the regional anesthesia cohort for patients with (n = 10) and without (n = 45) cervical radiculopathy was performed. There were no incidences of worsening peripheral neuropathy following regional anesthesia in these patients, and there was no difference between complication rates in patients with (n = 2, 20%) and without cervical radiculopathy (n = 5, 11.1%) (p = 0.59). There was no difference in pre- to post-operative change in McGowan scores in patients with and without cervical radiculopathy (p = 0.55).
Discussion
There was no significant difference in the occurrence of complications or outcomes at 6 weeks post-operative in patients who underwent in situ ulnar nerve decompression under general versus regional anesthesia. Specifically, no patient experienced worsening ulnar neuropathy or a brachial neuritis after receiving a peripheral nerve block. Similarly, Hebl et al found no significant increase in post-operative complications or worsening ulnar neuropathy following various forms of ulnar nerve anterior transposition in patients with cubital tunnel syndrome compared between those who received axillary blocks (6 complications, 6%) versus general anesthesia (n = 15, 6%).11 Disproportionate nerve irritation during block placement and preexisting neurologic disease were not risk factors for regional anesthesia associated nerve injury.11 Conversely, one multicenter review of regional anesthesia complications for a wide variety of surgeries in the body found pain or paresthesias during needle placement or anesthetic injection was associated with an increased risk of neurologic injury.6
The incidence of neurologic injury following peripheral nerve block ranges from 0.02% to 0.3%,6,12,13 with transient nerve deficits reported up to 8% in some studies.12–14 Additional reported complications of peripheral nerve blocks, while rare, include systemic toxicity from the local anesthetic15 and phrenic nerve palsy with hemidiaphragm paralysis, specifically in supraclavicular and interscalene blocks.16–18 Given the rarity of peripheral nerve injuries following peripheral nerve blocks, the underlying cause of injury is often unclear.6,7,14,19,20 The implementation of ultrasound guided and/or nerve stimulator assisted peripheral nerve block is considered to have improved outcomes, though this has yet to be shown in the literature.13 Patients with underlying upper or lower motor neuron pathology within the distribution of the targeted nerve are thought to be at higher risk for neurologic injuries after nerve blocks due to the nerve’s increased sensitivity to local anesthetics or decreased neural blood supply, though this has not been confirmed nor disproved in the literature.13,21
Additionally, it is postulated that patients with cervical radiculopathy are considered to have increased susceptibility to further progression of nerve injury following regional anesthesia which is extrapolated from the “double crush” theory.8 A study of malpractice claims related to peripheral nerve blocks found that 26% of claims had a preexisting injury or radiculopathy, and the majority of claims were for “permanent minor injuries.”14 However, neither the current study nor that performed by Hebl et al11 reported higher rates of neurologic injury following the use of peripheral nerve blocks in patients undergoing surgery for ulnar nerve compressive neuropathy. Additionally, adverse outcomes were not associated with the presence of underlying neurologic diseases or cervical radiculopathy. This suggests that regional anesthesia for ulnar nerve in situ decompression does not place the ulnar nerve at a higher risk for developing a new or worsening nerve deficit.
Multiple studies have compared general versus regional anesthesia in various orthopedic procedures.22–25 Regional anesthesia has been associated with less postoperative nausea, pain, cardiovascular events, and shorter hospital stays in hip fractures, arthroplasty, and rotator cuff repairs.22–25 A study by Rundgren et al reported decreased post-operative pain, nausea and vomiting, and shorter total peri-operative time in patients undergoing surgical treatment of distal radius fractures with peripheral nerve blocks compared to general anesthesia.26 Of note, 7 of the 45 patients (15.6%) in their study required conversion to general anesthesia due to inadequate anesthesia provided by the peripheral nerve block. This is similar to the results presented in this study, which found that 10.9% of patients required conversion to general anesthesia following unsuccessful regional anesthesia. This is a known risk following peripheral nerve blocks and must be discussed with the patient prior to surgery.13 A study by Roussel and Thirkannad did not find a significant difference in failure of upper extremity brachial plexus nerve blocks to produce adequate pain control during in situ cubital tunnel release between axillary (6 of 30), infraclavicular (6 of 30), and supraclavicular (10 of 30) nerve blocks.27 Our study also had failure of axillary, infraclavicular, and supraclavicular nerve blocks during in situ cubital tunnel release. Further evolution in the safe and efficacious delivery of peripheral nerve blocks may improve their efficacy in the future.
Limitations of this study include the retrospective nature of the review, which may not have captured all adverse events after surgery and may be subject to confounding factors. A selection bias between patients who had general versus regional anesthesia is likely present in this retrospective comparative study; however, there was no difference in patient demographics between the two cohorts. Furthermore, nerve injuries following peripheral nerve blocks are extremely rare, and larger prospective studies may be required to better identify risk factors for development of these complications. Although our study is underpowered to accurately detect any differences in nerve injuries between anesthesia cohorts, it provides an important initial investigation into the complex decision-making regarding the choice of anesthesia for surgical procedures involving the ulnar nerve. Further studies on the safety of regional anesthesia in ulnar nerve transpositions or revision cubital tunnel surgeries are also warranted, as these patients often differ in the severity of ulnar neuropathy.
Despite the theoretic increased risk of peripheral nerve injury following brachial plexus blocks in patients undergoing in situ ulnar nerve decompression for the treatment of cubital tunnel syndrome, the current study found no evidence to support these concerns. However, further studies are necessary to determine if the method of anesthesia performed at the time of in situ ulnar nerve decompression affects clinical outcomes.
Acknowledgments
This abstract was previously presented at the 2021 Mid-America Orthopaedic Association Conference and the 2020 American Society for Surgery of the Hand Conference.
Funding
The authors have no sources of funding to declare for this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Latinovic R, Gulliford MC, Hughes RA. Incidence of common compressive neuropathies in primary care. J Neurol Neurosurg Psych. 2006;77(2):263–265. doi:10.1136/jnnp.2005.066696
2. Staples JR, Calfee R. Cubital tunnel syndrome: current concepts. J Am Acad Orthop Surg. 2017;25(10):e215–e224. doi:10.5435/JAAOS-D-15-00261
3. Soltani AM, Best MJ, Francis CS, Allan BJ, Panthaki ZJ. Trends in the surgical treatment of cubital tunnel syndrome: an analysis of the national survey of ambulatory surgery database. J Hand Surg. 2013;38(8):1551–1556. doi:10.1016/j.jhsa.2013.04.044
4. Huq NS, Ahmed N, Razeghi M. Cubital tunnel release using local anesthesia. Clin Plast Surg. 2013;40(4):557–565. doi:10.1016/j.cps.2013.08.003
5. Whitlock EL, Pardo MC. Choice of anesthetic technique. In: Basics of Anesthesia.
6. Auroy Y, Narchi P, Messiah A, Litt L, Rouvier B, Samii K. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthes. 1997;87(3):479–486. doi:10.1097/00000542-199709000-00005
7. Hussain N, Goldar G, Ragina N, Banfield L, Laffey JG, Abdallah FW. Suprascapular and interscalene nerve block for shoulder surgery: a systematic review and meta-analysis. Anesthes. 2017;127(6):998–1013. doi:10.1097/ALN.0000000000001894
8. Upton AR, McComas AJ. The double crush in nerve entrapment syndromes. Lancet. 1973;2(7825):359–362. doi:10.1016/S0140-6736(73)93196-6
9. Mc GA. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br. 1950;32(3):293–301. doi:10.1302/0301-620X.32B3.293
10. Maggard-Gibbons M. The use of report cards and outcome measurements to improve the safety of surgical care: the American college of surgeons national surgical quality improvement program. BMJ Qual Saf. 2014;23(7):589–599. doi:10.1136/bmjqs-2013-002223
11. Hebl JR, Horlocker TT, Sorenson EJ, Schroeder DR. Regional anesthesia does not increase the risk of postoperative neuropathy in patients undergoing ulnar nerve transposition. Anesth Analg. 2001;93(6):1606–1611. doi:10.1097/00000539-200112000-00058
12. Wulf H. Nervenschäden bei Regionalanästhesie – Eine Komplikation und viele mögliche Ursachen [Nerve damage in regional anesthesia - A complication and many possible causes]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2012;47(5):318–319. German. doi:10.1055/s-0032-1313569
13. Jeng CL, Torrillo TM, Rosenblatt MA. Complications of peripheral nerve blocks. Br J Anaesth. 2010;105(Suppl 1):i97–i107. doi:10.1093/bja/aeq273
14. Saba R, Brovman EY, Kang D, Greenberg P, Kaye AD, Urman RD. A contemporary medicolegal analysis of injury related to peripheral nerve blocks. Pain Physician. 2019;22(4):389–400.
15. Rubin DS, Matsumoto MM, Weinberg G, Roth S. Local anesthetic systemic toxicity in total joint arthroplasty: incidence and risk factors in the United States from the national inpatient sample 1998–2013. Reg Anesth Pain Med. 2018;43(2):131–137. doi:10.1097/AAP.0000000000000684
16. Chiaghana CO, Awoniyi CA. Delayed onset and long-lasting hemidiaphragmatic paralysis and cranial nerve deficit after interscalene nerve block for rotator cuff repair in beach chair position. J Clin Anesth. 2016;34:571–576. doi:10.1016/j.jclinane.2016.06.026
17. Kot Baixauli P, Rodriguez Gimillo P, Baldo Gosalvez J, de Andres Ibanez J. Usefulness of diaphragmatic ultrasound in the early diagnosis of phrenic nerve palsy after shoulder surgery in the prevention of post-operative respiratory complications. Rev Esp Anestesiol Reanim. 2018;65(10):593–596. doi:10.1016/j.redar.2018.05.008
18. Shinn HK, Kim BG, Jung JK, Kwon HU, Yang C, Won J. Prolonged hemidiaphragmatic paresis following continuous interscalene brachial plexus block: a case report. Med. 2016;95(24):e3891. doi:10.1097/MD.0000000000003891
19. Cheney FW, Domino KB, Caplan RA, Posner KL. Nerve injury associated with anesthesia: a closed claims analysis. Anesthes. 1999;90(4):1062–1069. doi:10.1097/00000542-199904000-00020
20. Lee LA, Posner KL, Kent CD, Domino KB. Complications associated with peripheral nerve blocks: lessons from the ASA closed claims project. Int Anes Clin. 2011;49(3):56–67. doi:10.1097/AIA.0b013e31821a0294
21. Neal JM, Gerancher JC, Hebl JR, et al. Upper extremity regional anesthesia: essentials of our current understanding, 2008. Reg Anes Pain Med. 2009;34:134–170.
22. Kreutziger J, Hirschi D, Fischer S, Herzog RF, Zbinden S, Honigmann P. Comparison of interscalene block, general anesthesia, and intravenous analgesia for out-patient shoulder reduction. J Anesth. 2019;33(2):279–286. doi:10.1007/s00540-019-02624-6
23. Matharu GS, Garriga C, Rangan A, Judge A. Does regional anesthesia reduce complications following total hip and knee replacement compared with general anesthesia? An analysis from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. J Arthroplasty. 2020;35(6):1521–1528. doi:10.1016/j.arth.2020.02.003
24. Gulur P, Nishimori M, Ballantyne JC. Regional anaesthesia versus general anaesthesia, morbidity and mortality. Best Pract Res Clin Anaesthesiol. 2006;20(2):249–263. doi:10.1016/j.bpa.2005.10.002
25. Danninger T, Stundner O, Rasul R, et al. Factors associated with hospital admission after rotator cuff repair: the role of peripheral nerve blockade. J Clin Anesth. 2015;27(7):566–573. doi:10.1016/j.jclinane.2015.07.008
26. Rundgren J, Mellstrand Navarro C, Ponzer S, Regberg A, Serenius S, Enocson A. Regional or general anesthesia in the surgical treatment of distal radial fractures: a randomized clinical trial. J Bone Joint Surg Am. 2019;101(13):1168–1176. doi:10.2106/JBJS.18.00984
27. Roussel J, Thirkannad S. Comparison of 3 ultrasound-guided brachial plexus block approaches for cubital tunnel release surgery in 120 ambulatory patients. AANA J. 2014;82(2):121–126.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
