Back to Journals » Clinical Ophthalmology » Volume 16
Safety and Efficacy of Hypersonic Vitrectomy for Retinal Reattachment Surgery in Proliferative Vitreoretinopathies
Authors Deuchler S , Scholtz J, Knoch T, Seitz B , Koch FH
Received 19 August 2022
Accepted for publication 31 October 2022
Published 11 November 2022 Volume 2022:16 Pages 3711—3720
DOI https://doi.org/10.2147/OPTH.S386014
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Supplementary video of "Hypersonic vitrectomy for retinal reattachment in PVR" [ID 386014].
Views: 229
Svenja Deuchler,1– 3 Julia Scholtz,1 Timo Knoch,4 Berthold Seitz,2 Frank H Koch1,3
1Study Centre, Augenzentrum Frankfurt, Frankfurt am Main, Hessen, Germany; 2Department of Ophthalmology, Saarland University Medical Center, Homburg, Saarland, Germany; 3Department of Ophthalmology, University Hospital of the Goethe University Frankfurt/Main, Frankfurt am Main, Hessen, Germany; 4Bausch + Lomb GmbH, Berlin, Germany
Correspondence: Svenja Deuchler, Email [email protected]
Introduction: To investigate the safety and efficacy of the Vitesse hypersonic vitrectomy device for retinal reattachment surgery in proliferative vitreoretinopathy (PVR) or proliferative diabetic vitreoretinopathy (PDVR) cases. The Vitesse device utilizes hypersonic technology to liquefy instead of cutting the vitreous, providing an alternative to the traditional pneumatic guillotine cutter.
Material and Methods: A prospective, one-armed, non-comparative, open-label study was performed. Sixteen patients with a diagnosis of PVR or PDVR that required retinal reattachment surgery were included. Severity of disease was classified using the Retina Society 1983 classification and Kroll Classification from 2007. Patient data was collected preoperatively, 2 days postoperatively, 1 month postoperatively, and 3 months postoperatively. Efficacy of hypersonic vitrectomy was evaluated, both subjectively using a questionnaire and objectively by means of Supplementary Video documentation, device settings, and data collection of the patients’ medical history.
Results: In all 16 cases, retinal reattachment surgery could be performed with Vitesse without conversion to a guillotine cutter. The vitreous could be separated from the detached retina completely with no iatrogenic tissue damage. Vitreous traction was documented in one case. In 6 cases, shaving of the vitreous base was performed after early fluid–air exchange with hypersonic vitrectomy without any complications. No adverse events suspected to be related to hypersonic vitrectomy were documented in the follow-up visits.
Conclusion: The Vitesse has potential advantages including reduced vacuum volumes with limited amount of turbulence and avoidance vitreoretinal traction. Liquefaction directly in front of the probe entrance allows for continuous unrestricted fluid flow. These factors of hypersonic technology allow to carry out retinal reattachment surgery in PVR or PDVR cases successfully.
Keywords: retinal detachment, hypersonic vitrectomy, proliferative vitreoretinopathy, proliferative diabetic vitreoretinopathy
Introduction
Retinal detachment has always been a difficult pathology to manage.1,2 Though it is a relatively rare disease with an incidence of 1 in 10,000, it is a sight-threatening condition. In tertiary care facilities, the occurrence of retinal detachments accounts for a large proportion of the operative effort.3 The three main techniques for the treatment of a retinal detachment are scleral buckling,4–9 pars plana vitrectomy (PPV)10–12 and pneumatic retinopexy.13 Vitrectomy should be favored for retinal reattachment surgery if there is vitreous traction like in PVR14 or PDVR15 cases.16,17
The Vitesse vitrector is a novel device from Bausch + Lomb GmbH (St. Louis, MO, USA) that uses hypersonic technology instead of traditional pneumatic guillotine cutting for vitreous removal.18 In 2017, the first in-human study using Vitesse was conducted in India and delivered promising results.19 Soon after, the device was approved by the FDA and CE and select surgeons began to operate with the device and collect further clinical experiences.
The main objective of this study was to evaluate the safety and efficacy of the Vitesse hypersonic vitrectomy device for retinal reattachment surgery in proliferative vitreoretinopathy (PVR) or proliferative diabetic vitreoretinopathy (PDVR) cases.
Materials and Methods
This prospective, one-armed, non-comparative, open-label study was approved by the Ethic Committee of the University Hospital Frankfurt (E115/20) and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. It was registered in the German Clinical Trials Register (DRKS00026046).
The University Hospital Department of Ophthalmology in Frankfurt was given the opportunity to be the first in Germany to conduct a clinical study using Vitesse. Two vitreoretinal surgeons – a primary surgeon and an assistant surgeon – completed all cases together, viewing through stereoscopic observation systems of the microscope. They were required to complete an online training prior to operating with Vitesse. The background, machine settings and surgical techniques were discussed. Each case was performed together with a Clinical & Application Specialist from Bausch + Lomb to find optimal machine settings for each requirement.
Vitesse is used in conjunction with plastic cannulas instead of standard titanium cannulas because the hypersonic technology prevents the device from being used with metal cannulas. Overall, lower vacuum volumes of vitreous are necessary when using Vitesse (0–150 mmHg) compared to traditional vitrectomy (200–600 mmHg). A vibrating single lumen needle (0–60 micrometers at 28.5 kHz) shears the vitreous body at the edge of the continuously open port and the liquified material is extracted. This is in opposite to traditional gold-standard guillotine systems that contain a double lumen system for cutting and aspirating and therefore have to aspirate vitreous into the lumen where the cutting takes place. Figure 1 shows the Vitesse device in use.
 |
Figure 1 Vitesse device in use, as seen in the right hand of the surgeon. |
Here, we focus on the 16 cases where hypersonic vitrectomy was used for reattachment of detached retina in patients with proliferative vitreoretinopathy (PVR) or proliferative diabetic vitreoretinopathy (PDVR) in an inpatient setting. All patients were informed about the study, and written informed consent was obtained prior to inclusion.
The efficacy of the Vitesse liquefaction technique was recorded both subjectively using a questionnaire, which the surgeon filled out after each case, and objectively by means of Supplementary Video documentation of the operation with an evaluation of the duration of the operation, the method of vitrectomy (eg, if performed using early fluid–air exchange to complete vitreous removal under air), the safety of the procedure (as defined by the complication rate, incarceration of vitreous, and excessive retinal traction), and the device settings.
All study patients were seen for follow-up postoperatively. The first follow-up visit was completed 2 days after surgery date and prior to discharge. All patients were scheduled for a 1-month follow-up visit. As standard procedure, patients who received a silicone oil tamponade were scheduled for oil removal 2 months postoperatively, with the exception of those who due to their clinical picture required prolonged oil tamponade. All patients were scheduled for a 3-month follow-up visit.
Results
Sixteen patients with retinal detachment due to either PVR or PDVR underwent pars plana vitrectomy and all procedures were performed by 2 retinal surgeons together. Patients were classified according to disease severity using the classification system of the Retina Society 1983 and the Kroll Classification from 2007.14,15,20 Please see Table 1.
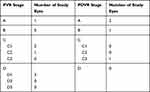 |
Table 1 Patient Classification Using the Retina Society 1983 Classification and Kroll Classification from 2007 |
Vitesse Technology and Machine Settings in Retinal Reattachment Surgery
Table 2 displays the typical machine settings chosen for retinal reattachment surgery based on our case experiences so far. Regarding stroke length, for primary core vitrectomy, it was useful to work with a stroke of approximately 60 µm. If the vitreous was still attached and a PVD was required, stroke was reduced. It was advised by the surgeons to start with zero stroke and increase it up to 60 µm if necessary. Regarding vacuum pressure, in most retinal detachment scenarios a vacuum pressure around 100–120 mmHg was used. If the patient was young or had a pathological adherent vitreous (for example, in PVR cases in rhegmatogenous retinal detachment) we found it to be adventitious to reduce the vacuum pressure to about 40 mmHg. Finally, regarding fluid–air exchange, a vacuum of approximately 120 mmHg was required to be as effective with Vitesse as with a guillotine cutter.
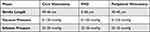 |
Table 2 Typical Vitesse Machine Parameters in Our Setting with a Dual Linear Foot Pedal for Retinal Reattachment Surgery |
In Figure 2 and Supplementary Video, examples of retinal reattachment surgery with Vitesse are presented. In the upper right-hand corner of both Figure 2 and Supplementary Video, parameters and device settings are listed.
 |
Figure 2 Removal of residual vitreous (before silicone oil fill) under air using the Vitesse device. |
Results of the Postoperative Questionnaire
The case-specific results of the postoperative questionnaire completed by surgeons are displayed in Table 3. Out of 16 cases, 3 complications were noted. All were related to the instability of the plastic cannulas, as described in Limitations and Complications. Vitreous traction was observed in one case (PVR D1) due to inability to cut vitreous but without any associated retinal injury or break. After performing a fluid–air exchange, the surgeon was able to complete the vitrectomy successfully. In 7 of 16 cases, surgeons reported on the postsurgical questionnaire that using Vitesse felt more time-consuming than the procedure would have been with a guillotine cutter. Average case time was 1 hour 20 minutes, and the time varied depending on the difficulty of the case (min 0:40 and max 2:54).
 |
Table 3 Results from Case-Specific Postoperative Questionnaire |
Air fill in eyes with incomplete vitreous removal was helpful for better visualization and for stabilization of mobile retina. Therefore, in 6 of 16 cases, early fluid–air exchange was performed and removal of the vitreous base was completed without any collapse of the eye or choroidal or retinal bleeding. All cases were performed using hypersonic vitrectomy, and surgeons did not have to switch to a guillotine cutter to finish the procedure in any cases.
Staining of the transparent vitreous either from previously existing bleeding or from triamcinolone crystals injected into the vitreous cavity was helpful for a more adequate assessment of the progress of vitreous liquefaction.
With Vitesse, trimming back of necrotic tissue at the edge of a retinal tear as well as the targeted removal of a tear flap was managed in all cases without the risk of uncontrolled and/or extensive tissue reduction. The maneuver had to be adjusted based on specific tissue density: subretinal fluid was drained with a stroke length of 0, soft swollen retina required stroke length between 20 and 40 µm, and dense fibrovascular tissue was removed with stroke length between 40 and 60 µm. This was combined with a vacuum level of 40–120 mmHg.
Accidental iatrogenic enlargement of a retinal tear was not detected in any of our cases. In one case, a larger retinectomy was required. This could be performed precisely with Vitesse by liquefying the retina with a stroke length between 20 and 40 µm and a vacuum level of 20–120mmHg without unintentional removal of healthy tissue.
Postoperative Follow-Up
Dependent on the PVR/PDVR staging and the amount of efforts to reattach the retina, a gas tamponade could be used as vitreous tamponade in 3 eyes (one case with PDVR A, one with PDVR B and one with PVR A). These patients all had ophthalmologic findings within normal limits at the 1-month follow-up visit. The other 13 received silicone oil tamponade. Out of the 13 patients who received silicone oil tamponade, 9 oil removal postoperatively. For these patients, at the initial 1-month follow-up visit, no adverse events as iatrogenic retinal holes and retinal redetachment related to the Vitesse procedure18 were noted and oil removal was performed at 2-months postoperatively. At a 3-month follow-up post initial surgery, all eyes were stable. The other 4 patient eyes that initially received silicone oil required prolonged silicone oil tamponade due to their disease severity.
None of the patients had an eye pressure increase or hypotony after surgery in the first follow-up visit before discharge. At the 1-month follow-up visit, 3 patients had a slightly elevated intraocular pressure, which could be managed with topical anti-glaucoma therapy. After these 3 patients underwent silicone oil removal, their intraocular pressure decreased back to normal levels without additional therapy. None of the patients developed any signs of inflammation or endophthalmitis postoperatively. None of the adverse events noted were suspected to be related to hypersonic vitrectomy.
Limitations and Challenges of Hypersonic Vitrectomy
Due to the hypersonic technique, plastic cannulas are necessary to avoid friction metal (handpiece) to metal (trocar).18 One observation noted early on in the study was the lack of stability of the plastic cannulas. In 3 cases, this instability was especially highlighted in the postoperative questionnaire completed by the surgeon. In 2 cases, 1 cannula was extruded and had to be re-inserted into the eye. In the other case, the cannula was only partially extruded and could be replaced. After these 3 initial instances of instability, our center received a new shipment of cannulas with a new lot number. With the new cannulas, one additional case of instability was experienced during a surgery in an eye with a deep eye socket.
Regarding the Vitesse device, out of 16 cases, there was only one instance of clinically relevant traction, but it was without secondary complications (eg, retinal tear).
Vitesse had the potential to create unwanted vitreous pearls (dehydrated vitreous strands) in front of the target as a result of a non-optimized combination of aspiration and stroke. In our cases, this could be resolved by adjusting the aspiration-stroke-setup to the specific tissue density as described above. Table 4 includes a summary of the limitations, advantages, and possible solutions of the use of Vitesse for hypersonic vitrectomy.
 |
Table 4 Advantages and Limitations of Hypersonic Vitrectomy for Retinal Reattachment Surgery |
Discussion
Hypersonic vitrectomy is a novel innovation in the field of vitreoretinal surgery and provides an alternative to the traditional pneumatic guillotine cutter method. Prior research on the use of hypersonic vitrectomy with Vitesse has shown similar promising results regarding the safety and efficiency of the device.19,21,22 Stanga et al19 published the first human study using Vitesse on 20 patient eyes in India. In this study, surgeons were able to successfully perform peripheral vitrectomy in 18 of 20 patient eyes using hypersonic vitrectomy. In one of the two unsuccessful attempts, the surgeon switched to a guillotine cutter device to complete the surgery. Blinder et al21 published a case series in the United States including 64 human eyes that underwent hypersonic vitrectomy. This study reported that in 9 of 64 cases, vitrectomy could not be completed entirely using the Vitesse device and that the surgeon switched to a pneumatic guillotine cutter during the procedure. Romano et al22 performed a prospective, multicentric, interventional study on 50 eyes using hypersonic vitrectomy. In this study, 70% of the cases could be finished using hypersonic energy exclusively, in 30% the vitrectomy was finished switching to a guillotine cutter.
We were able to utilize Vitesse for retinal reattachment surgery in PVR or PDVR cases for the entirety of all 16 cases and at no point required conversion to the pneumatic guillotine cutter. In 1 out of 16 cases, there was an instance of clinically relevant traction seen by the surgeon, but without secondary complications. Stanga et al reported 2 retinal tears19 and 1 out of 64 cases developed an iatrogenic retinal break in Blinder’s study.21 In Romano’s study two iatrogenic retinal breaks appeared.22 Stanga et al performed no retinal reattachment surgeries with Vitesse and Blinder reported 23 cases. In this case, all retinal detachments could be successfully reattached with hypersonic vitrectomy and repeat PPV was required for recurrent retinal detachment in 2 patients. Romano et al performed surgery on 4 retinal detachments out of 50 cases.
In Blinder’s postoperative questionnaire, surgeons reported for 52% of cases that hypersonic vitrectomy was more advantageous relative to the pneumatic guillotine cutter, and also highlighted its ability to perform smooth peripheral shaving at the vitreous base.
Stanga et al reported in the first clinical cases that vitreous strands were present in the majority of cases.19 This was better managed in Blinder’s and Romano’s study, which reported difficulties in cutting the vitreous and the presence of vitreous strands in only 13%21 respectively in 10%22 of cases. With ongoing further clinical studies and machine parameter adaptations, this issue may be minimized.
As described above, the Vitesse device is safe to use for vitrectomy. In 43.8% of cases with vitreous traction, surgeons noted in their postoperative surveys that it seemed to be more time-consuming to use for a complete vitrectomy than the guillotine cutter. The average time of procedure was 1 hour 20 min. Due to variations in case severity, procedure length could not be objectively verified. There are two possible reasons for this potentially lengthier process. First, the process might indeed take longer or second, and the action of liquifying is smoother in a way such that not all responses are visible to the surgeon or observer.
A fluid–air exchange can be performed with Vitesse at any point during the liquefaction procedure once there is a core cavity created. Hypersonic vitrectomy technology makes a vitrectomy under air in the vitreous both efficient and safe simultaneously. In 37.5% of all cases, a vitrectomy under air with Vitesse was performed. All of these cases ran smoothly and resulted in no complications (eg, bleeding or eye collapse).
Complete vitrectomy is crucial for retinal reattachment surgery, especially in more cumbersome cases with PVR/PDVR activity. Here, well-defined retinotomies, relaxing incisions, and retinectomies have to be performed precisely. Additionally, adequate vitreous base shaving is a requirement prior to performing a temporary silicone oil fill, which helps to prevent recurrence of PVR. Therefore, the safety and efficacy profile for dissecting vitreous and necrotic retinal tissue from vital retina using Vitesse will play a pronounced role.
With more experience using Vitesse, the user is able to finesse the correct combination of low aspiration and adapted stroke length parameters to the tissue. This allows the surgeon to complete the vitreous liquefaction more completely and with less complications. However, the user must be aware that in retinal detachment cases with dense, tractive vitreous, the complete removal of the vitreous could be more time-consuming. The tip of the Vitesse device continues to be refined for efficiency and optimal outcomes based on feedback from surgeons using the device.
Overall, the use of hypersonic technology allows to approach many procedural steps in retinal reattachment surgery in a modified way adjusted to the individual pathology. As use and research pertaining to Vitesse continues, this hypersonic technology has the potential to become more widely used in vitreous surgery, especially if the safety profile increases while maintaining or improving efficiency.
Data Sharing Statement
The authors confirm that the data supporting the findings of this study are available within the article (Tables and Figures) and its Supplementary Video.
Acknowledgments
The abstract of this paper was presented at the ARVO Annual Meeting 2022 as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Investigative Ophthalmology & Visual Science Vol. 63, No.7 (June 2022) https://iovs.arvojournals.org/article.aspx?articleid=2780991.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
Svenja Deuchler, Julia Scholtz, and Berthold Seitz declare that there is no conflict of interest regarding the publication of this paper. Timo Knoch is employed by Bausch + Lomb as Clinical Trainer & Application Specialist Retina. Prof. Dr. Frank H Koch reports non-financial support from B&L Company, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Dellaporta AN. Retinal detachment surgery: historical notes. Documenta Ophthalmologica. 1999;99:259–272. doi:10.1023/A:1002668925562
2. Van de Put MAJ, Hooymans JMM, Los LI; Dutch Rhegmatogenous Retinal Detachment Study Group. The incidence of rhegmatogenous retinal detachment in The Netherlands. Ophthalmology. 2013;120(3):616–622. doi:10.1016/j.ophtha.2012.09.001
3. Unlue N, Kocaoglan H, Acar MA, Sargin M, Aslan BS, Duman S. Outcome of complex retinal detachment surgery after silicone oil removal. Int Ophthalmol. 2004;25:33–36. doi:10.1023/b:inte.0000018545.62455.ff
4. Flindall RJ, Norton EW, Curtin VT, Gass JD. Reduction of extrusion and infection following episcleral silicone implants and cryopexy in retinal detachment surgery. Am J Ophthalmol. 1971;71:835–837. doi:10.1016/0002-9394(71)90250-9
5. Domniz Y, Cahana M, Avni I. Corneal surface changes after pars plana vitrectomy and scleral buckling surgery. J Cataract Refract Surg. 2001;27:868–872. doi:10.1016/S0886-3350(00)00755-0
6. Hanneken AM, Michels RG. Vitrectomy and scleral buckling methods for proliferative vitreoretinopathy. Opthalmology. 1988;95:865–869. doi:10.1016/S0161-6420(88)33081-2
7. Hayashi H, Hayashi K, Nakao F, Hayashi F. Corneal shape changes after scleral buckling surgery. Ophthalmology. 1997;104:831–837. doi:10.1016/S0161-6420(97)30226-7
8. Kwartz J, Charles S, McCormack P, Jackson A, Lavin M. Anterior segment ischaemia following segmental scleral buckling. Br J Ophthalmol. 1994;78:409–410. doi:10.1136/bjo.78.5.409
9. Yoshida A, Feke GT, Green GJ, et al. Retinal circulatory changes after scleral buckling procedures. Am J Ophthalmol. 1983;95:182–188. doi:10.1016/0002-9394(83)90012-0
10. Johansson K, Malmsjö M, Ghosh F. Tailored vitrectomy and laser photocoagulation without scleral buckling for all primary rhegmatogenous retinal detachments. Br J Ophthalmol. 2006;90:1286–1291. doi:10.1136/bjo.2006.098202
11. Oyagi T, Emi K. Vitrectomy without scleral buckling for proliferative vitreoretinopathy. Retina. 2004;24:215–218. doi:10.1097/00006982-200404000-00004
12. Siqueira RC, Gomes CV, Dalloul C, Jorge R. Vitrectomy with and without scleral buckling for retinal detachment. Arq Bras Oftalmol. 2007;70(2):298–302. doi:10.1590/S0004-27492007000200020
13. Chan CK, Lin SG, Nuthi AS, Salib DM. Pneumatic retinopexy for the repair of retinal detachments: a comprehensive review (1986–2007). Surv Ophthalmol. 2008;53(5):443–478. doi:10.1016/j.survophthal.2008.06.008
14. Hilton G, Machemer R, Michels R, Okun E, Schepens C, Schwartz A. The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology. 1983;90(2):121–125. doi:10.1016/s0161-6420(83)34588-7
15. Kroll P, Rodrigues EB, Hoerle S. Pathogenesis and classification of proliferative diabetic vitreoretinopathy. Ophthalmologica. 2007;221(2):78–94. doi:10.1159/000098253
16. Heimann H, Hellmich M, Bornfeld N, Bartz-Schmidt KU, Hilgers RD, Foerster MH. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment (SPR Study): design issues and implications. Graefes Arch Clin Exp Ophthalmol. 2001;239:567–574. doi:10.1007/s004170100319
17. Heimann H, Zou X, Jandeck C, et al. Primary vitrectomy for rhegmatogenous retinal detachment: an analysis of 512 cases. Graefes Arch Clin Exp Ophthalmol. 2006;244:69–78. doi:10.1007/s00417-005-0026-3
18. Deuchler S, Knoch T, Papour A, Kohnen T, Koch F. Pars plana vitrectomy-from suction cutting systems to ultrasound technology. Ophthalmologe. 2021;118(7):741–746. German. doi:10.1007/s00347-021-01377-6
19. Stanga PE, Williams JI, Shaarawy SA, et al. First-in-human clinical study to investigate the effectiveness and safety of pars plana vitrectomy surgery using a new hypersonic technology. Retina. 2020;40(1):16–23. doi:10.1097/IAE.0000000000002365
20. Machemer R, Aaberg TM, Freeman HM, Irvine AR, Lean JS, Michels RM. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1991;112:159–165. doi:10.1016/S0002-9394(14)76695-4
21. Blinder KJ, Awh CC, Tewari A, Garg SJ, Srivastava SK, Kolesnitchenko V. Introduction to hypersonic vitrectomy. Curr Opin Ophthalmol. 2019;30(3):133–137. doi:10.1097/ICU.0000000000000563
22. Romano MR, Caretti L, Ferrara M, et al. Twenty-three-gauge hypersonic vitrectomy: real-world surgical evidence. Retina. 2021;41(12):2523–2530. doi:10.1097/IAE.0000000000003215
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
