Back to Journals » Journal of Asthma and Allergy » Volume 15
SABA Overuse in Russia – Burden and Possible Causes: An Analysis of the Russian Population in the SABINA III (SABA use IN Asthma) Study
Authors Avdeev S , Voznesenskiy N , Boldina M, Ignatova G, Kostina N, Kulbaisov A, Leshchenko I , Beekman MJHI
Received 27 November 2021
Accepted for publication 24 February 2022
Published 24 March 2022 Volume 2022:15 Pages 371—379
DOI https://doi.org/10.2147/JAA.S350393
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Amrita Dosanjh
Sergey Avdeev,1 Nikolay Voznesenskiy,2 Marina Boldina,3 Galina Ignatova,4 Natalya Kostina,5 Amirzhan Kulbaisov,6 Igor Leshchenko,7 Maarten JHI Beekman8
1Department of Pulmonology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia; 2National Medical Research Center for Pulmonology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia; 3Department of Therapy and Cardiology, Privolzhsky Research Medical University, Nizhny Novgorod, Russia; 4Department of Therapy and Postgraduate Education, South Ural State Medical University, Chelyabinsk, Russia; 5Pulmonology Department, Voronezh Regional Clinical Hospital No 1, Voronezh, Russia; 6Pulmonology Department, Orenburg Regional Hospital No 2, Orenburg, Russia; 7Department of Phthisiatry and Pulmonology, Ural State Medical University, Ekaterinburg, Russia; 8LLC AstraZeneca, The Hague, The Netherlands
Correspondence: Sergey Avdeev, Email [email protected]
Background: Short-acting β 2-agonists (SABA) overuse is associated with asthma morbidity and mortality. The SABA use IN Asthma (SABINA) program aimed to describe the global use of SABA in patients with asthma. SABINA III study was a cross-sectional study covering 24 countries.
Methods: We performed statistical analysis of the Russian population (618 patients recruited in 12 centers) from the SABINA III study. In this study in patients aged ≥ 12 years, data on disease characteristics and asthma treatments were collected using real-time electronic case report forms. Patients were classified by asthma severity and control according to the 2017 GINA. All variables (asthma severity and control, number of severe exacerbations, SABA and other medications use) were analyzed descriptively only, no hypothesis was tested.
Results: Majority of the study population consisted of patients with moderate/severe asthma (78.5%), while mild asthma was seen in 21.5%. Asthma was uncontrolled in 36.1% of patients and partly controlled in 33.5%. More than 80% of patients were treated with ICS/LABA fixed-dose combination. Almost half of all patients (47.0%) had at least 1 severe exacerbation in the previous 12 months. SABA over-prescription (≥ 3 canisters per year) was seen in 37% of patients. The frequency of SABA over-prescription was similar in patients with mild (35%) and moderate/severe (38%) asthma. SABA was purchased over-the-counter (OTC) in the past 12 months by 30.1% of all patients, and 14% purchased ≥ 3 canisters of SABA per year. About 91% of patients who purchased SABA OTC already received prescriptions for SABA, of whom 59% were prescribed ≥ 3 canisters per year.
Conclusion: Russia is seeing very high level of SABA over-prescription. This is potentially associated with poor asthma control and frequent severe exacerbations. Over-prescription may serve as the main cause for SABA overuse in Russia. To reduce SABA overuse and improve overall asthma control in Russia, it is necessary to educate not just the patients but also the doctors, while actively implementing up-to-date asthma treatments.
Keywords: bronchial asthma, asthma control, short-acting β 2-agonists, SABA overuse, over-the-counter use
Background
Bronchial asthma is an inflammatory disease with fluctuating symptoms, therefore anti-inflammatory treatment with inhaled corticosteroids (ICS) serves as the cornerstone of asthma treatment.1
Short-acting β2-agonists (SABA) as-needed were prescribed for symptom relief in most asthma patients, independently of maintenance treatment.1,2 At the same time, evidence of the hazards of SABA overuse has increasingly emerged in the last decades.3–6 SABA overuse, which is often associated with underuse of ICS, was recognized as one of the causes of preventable asthma attacks and deaths.7
In parallel, clinical trials have reported the superiority of anti-inflammatory reliever therapy with as-needed low dose budesonide/formoterol versus as-needed SABA, in terms of symptom control and reduction of exacerbation risk.8–11
These data have led to major changes in the 2019 report by the Global Initiative for Asthma (GINA), where SABA monotherapy is no longer recommended at Step 1, instead, a combination of low-dose ICS/formoterol as-needed is being recommended as the preferred reliever at steps 1 and 2 for adults and adolescents.1,12 The combination of low-dose ICS/formoterol is also the preferred reliever at steps 3–5 for patients who are prescribed ICS/formoterol maintenance therapy.1
The SABA use IN Asthma (SABINA) program was initiated to describe the global extent and clinical consequences of SABA use in asthma.13 The SABINA program has three main pillars: SABINA I (a retrospective, observational database study with expanded objectives in the UK), SABINA II (a distributed harmonized set of retrospective observational database studies in Europe and Canada), and SABINA III (a cross-sectional study covering 24 countries, in which no robust databases exist).13 A fourth pillar has been recently added to include multiple design, observational Research in several countries including Poland, Romania, Switzerland, the US, with more countries to follow.
The SABINA I and II studies have shown that SABA over-prescription (defined as prescription of ≥3 canisters per year) is common across 5 European countries (Germany, Italy, Spain, Sweden and the UK) with different healthcare and reimbursement policies.14 Nevertheless, some country-specific peculiarities of SABA prescription trends were revealed.14
The SABINA III program sought to further explore the trends and differences of SABA prescription in asthma patients in 24 countries, as well as SABA over-the-counter (OTC) purchase.13
In Russia, SABA is readily available OTC, ie without a prescription. This channel of SABA possession was included in the SABINA III program. The present manuscript seeks to analyze data on the Russian subpopulation in the SABINA III program to examine SABA prescription patterns and related asthma outcomes.
Methods
The SABA in Asthma International (SABINA III) is a multi-country, cross-sectional observational study describing patterns of SABA prescriptions and its associations with patient outcomes (ClinicalTrials.gov number: NCT03857178). Retrospective data were collected electronically during the study visit, over a 1-year period (starting in March 2019) and included questions for both healthcare practitioners (HCP) and participating asthma patients from each HCP center. Sites to participate in the study were selected by purposive sampling from both Primary Care and Specialist centers across the country. These centers have had to be experienced in clinical trials in asthma and also to have appropriate flow of asthma patients in order to recruit them in the study timely.
The main objective of the SABINA III study was to describe the pattern of SABA prescriptions in asthma patients, selected in a cross-sectional manner across various countries. Specifically, the study sought to describe the demographic and clinical features of the whole group of asthma patients participating in each country, and then separately groups with mild (steps 1–2) and moderate/severe (steps 3–5) asthma according to Global Initiative for Asthma GINA 2017.
Patients ≥12 years old with a documented diagnosis of asthma for at least 12 months, who had ≥3 consultations with a HCP as of the study start-date were included in the study. All patients (or a parent or legal guardian of patients under 18 years of age) provided informed consent before the study enrollment. The exclusion criteria comprised: a diagnosis of COPD or other chronic respiratory disease, any acute or chronic condition that could limit the patient’s ability to participate in the study.
The HCPs were asked to complete electronic case report forms recording the sociodemographic (age, gender, body-mass index, smoking status) and disease characteristics: asthma duration, severity and control, number of severe exacerbations during previous 12 months. Asthma severity and control were assessed according to the 2017 GINA. Asthma severity was described as mild (GINA steps 1–2) or moderate-to-severe (GINA steps 3–5). At least partly controlled asthma (partly controlled plus well-controlled asthma) was used as the outcome of clinical relevance. Severe exacerbations in the 12 months before the study visit were defined based on the American Thoracic Society/European Respiratory Society recommendations.
SABA prescriptions in the 12 months before the study visit were categorised as none, 1–2, 3–5, 6–9, 10–12 and ≥13 canisters, and >3 SABA canister prescriptions were considered as overuse. Questions about other asthma treatments were focused on use of any anti-inflammatory medications, specifically ICS, combinations of ICS with long-acting β2-agonist (LABA), oral corticosteroids (OCS) as short course or long-term/maintenance.
No additional mandated interventions on top of the routinely performed physician visits, examinations or treatments were required.
The study was performed in accordance with ethical principles consistent with the Helsinki Declaration, ICH GCP, and the applicable legislation on non-interventional/observational studies.
We performed all statistical analyses to a full analysis set of the Russian group: ie all patients who fulfill the eligibility criteria and for whom main variables (asthma severity and control, SABA prescriptions) were completed. All variables were described as mean ± standard deviation (SD) and/or median (interquartile range) for continuous variables and absolute and relative frequencies for categorical variables. All variables were analyzed descriptively, via appropriate statistical methods: categorical variables by absolute and relative frequencies and continuous variables by sample statistics.
Results
General Characteristics of the Group
The study involved 12 Russian centers; on average, each center included 52 patients aged 17 to 74 years. There were 632 patients enrolled in the study (for whom informed consent was received). Fourteen (2.2%) subjects were excluded because they did not have a diagnosis of asthma for at least 12 months. As a result, 618 patients were included in the full analysis set.
Practically all patients (99.4%) were seen by specialists, with the vast majority of patients seen by a pulmonologist/respiratory physician (565, 91.7%). The demographic characteristics of the group are presented in Table 1. The Russian population consisted of adult patients with mean age 54.4 years (only 0.5% were adolescents), female:male ratio was 3:1.
 |
Table 1 Demographic Characteristics of the Russian Asthma Patients (n=618) |
Severity and Control of Asthma
Mild asthma (GINA steps 1–2) was present in less than a quarter of the patients (21.5%), and the majority of the study population consisted of patients with moderate-to-severe asthma (GINA steps 3–5, 78.5%) (Table 2).
 |
Table 2 Disease Characteristics of the Russian Asthma Patients (n=618) |
The level of asthma symptom control was low; in fact, asthma was uncontrolled in 36.1% of patients and partly controlled in 33.5% of patients (Table 2). Almost half of all patients (47.0%) had at least 1 severe exacerbation in the previous 12 months, and 16.3% had ≥2 severe exacerbations.
Asthma Therapy Prescriptions
Data on asthma therapy prescriptions for the previous year is presented in Table 3. SABA was prescribed as an add-on to maintenance therapy for most patients, although SABA alone was prescribed for 8.1% of patients. Maintenance monotherapy with ICS was prescribed rarely. In contrast, fixed-dose combinations of ICS with a long-acting β-agonist (LABA) were prescribed for most patients. Every third patient was prescribed at least one burst of OCS during the previous year, while 3.4% were prescribed long-term/maintenance treatment using OCS.
 |
Table 3 Asthma Treatment Prescriptions in the Russian Asthma Patients (n=618) |
SABA Prescription
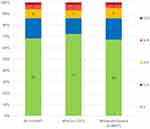
37% of patients received prescriptions for 3 or more canisters per year, which indicates SABA over-prescription. Notably, 9% of patients were prescribed 6 to 9 canisters within a year’s time, and another 9% were prescribed 10 or more canisters. The remaining 63% of all patients had prescriptions for ≤2 canisters of SABA during the year, with 19% receiving no prescriptions (Figure 1). The mean number of prescribed SABA inhalers was 4.0 ± 4.0 per patient per year; with the median at 2.0 and a range of 1–24.
The distribution of patients by the number of SABA prescriptions did not differ by asthma severity (Figure 1). Among patients with any severity of asthma who received SABA on top of maintenance therapy (including ICS), the over-prescription data did not differ from that in the general study population (37.2%).
Buying SABA without a Prescription
In the past 12 months, SABA was purchased in pharmacies, without a prescription, ie OTC by 30.1% of all patients with available data (n = 594). More than half of these patients purchased only 1–2 SABA inhalers per year, while the rest purchased OTC ≥3 canisters of SABA (Figure 2).
The distribution of patients by the quantity of SABA purchased OTC was largely unrelated to asthma severity. However, the percentage of patients purchasing ≥6 canisters per year among those with mild asthma (7%) exceeded that of those with moderate/severe asthma (5%).
Of those who acquired SABA OTC, 91% already received SABA prescriptions and 59% received prescriptions for 3 or more SABA canisters in the past year.
Discussion
In the sample of Russian patients with asthma that we reviewed, the mean number of prescribed SABA inhalers was 4.0 ± 4.0 per patient per year. The median was 2.0 (range 1–24). In this way, the average Russian patient with asthma may be classified as a potential SABA overuser merely on the basis of the number of SABA prescriptions received.
Per SABINA I–II data, in five European countries the annual number of SABA prescriptions varied from 1.6–1.9 (Germany and Sweden) to 3.1–3.3 (Italy and Spain) and 4.2 in the UK.14
The overall SABA over-prescription rate for the Russian population is 37%, which is greater than in most other European countries (9% in Italy, 16% in Germany, 29% in Spain, 30% in Sweden), and coincides with the figures for the UK (38%).14
The fact that Russia is experiencing one of the highest levels of SABA over-prescription in Europe may be explained by the low level of asthma symptom control and the high prevalence of severe exacerbations.
Real differences in SABA-over-prescription levels between Russia and other countries are further enhanced by the fact that SABA in Russia are commonly and widely obtained from a pharmacy without a prescription. What is more, every third patient in Russia has purchased SABA OTC in the past 12 months. At the same time, some 6% of patients exceeded the allowable volume of SABA use by 2–4 times only because of SABA OTC.
In Australia, where, as in Russia, SABA can be purchased OTC,15 a community pharmacy-based survey focusing exclusively on patients who requested SABA OTC was conducted.16 In this “hidden population”, 70% were classified as SABA overusers, and 73.6% were not using a preventer medication daily.16
Our analysis has shown, that among the Russian patients who purchased SABA OTC, >90% also did received SABA prescriptions and 2/3 of them got prescriptions for ≥3 canisters in the past year. Thus, most of these patients already fell into the SABA-overuse category on account of over-prescription alone.
In other words, Russian patients tend to acquire SABA independently, but not necessarily because their reliever had run out and they were not able to obtain another prescription. On the contrary, we may assume that doctors may sometimes prescribe SABA to these patients too cavalierly, not asking them about the total number of inhalers in possession.
The category of “heavy SABA overusers”, ie those patients who get ≥6 and even ≥10 inhalers annually, requires special attention from doctors. Patients fall into this category both through the purchase of SABA OTC and via over-prescription. To improve the situation, doctors should better control the SABA prescriptions, while educating patients on the safety of these drugs. Any self-reporting questionnaires about SABA flow might be helpful.
On the other hand, let us ask ourselves whether those patients who had not received a single SABA prescription in a year’s time (in Russia, that would mean every fifth patient) are doing well. A situation in which a doctor does not write a prescription for any reliever, can give patients the dangerous signal that they can choose a reliever on their own. This can lead the patient to use SABA or another bronchodilator in an uncontrolled fashion; it can even lead to off-label use of LABA in a separate inhaler (without ICS), which increases the risk of severe exacerbations of asthma.17
In Russia, the frequency of SABA over-prescription was similar in patients with mild (35%) and moderate/severe (38%) asthma. A similar picture was observed in other European countries, where SABA over-prescription was found in 9 to 32% of patients with mild asthma and in 8 to 31% of patients with moderate/severe asthma.14 An exception is the UK, where SABA over-prescription was greater for the more severe cases of asthma (58% versus 27% for mild asthma cases).14
In Russia, SABA over-prescription is observed with the highest frequency in mild asthma (35% compared to a maximum of 32% among other countries participating in the SABINA I–II program).14 This fact is well corresponding with recent data from a retrospective subanalysis of the Russian population in the SYGMA2 study,11 which showed that in Russia larger proportion of patients with mild asthma are uncontrolled (52% vs 45% in other countries) and suffered from severe asthma exacerbations in the previous year (30.1% vs 20.7%).18
The significance of these results is supported by the fact that SABA overuse is associated with an increase in the risk of various negative outcomes in asthma patients: poor asthma control, severe exacerbations, hospitalizations and mortality.19–21 Dispensing more than 12 SABA inhalers to one patient over 1 year was associated with an increased risk of asthma-related death.21 The present analysis also demonstrated possible association between SABA overuse and negative asthma outcomes revealed in this sample: high frequency of severe exacerbations and OCS burst treatment (at least once a year in every third patient).
To reduce SABA overuse and improve overall asthma control in Russia, it is necessary to educate not just the patients but also the doctors, while actively implementing up-to-date asthma treatments, including the use of anti-inflammatory relievers (low dose ICS/formoterol) instead of SABA.1,12 When educating patients and doctors, it is important to devote due attention to the use of ICS as anti-inflammatory drugs in asthma, as well as to the necessity of minimizing the use of SABA. Doctors should include the purchase of SABA OTC and its total use over a given period of time on the list of mandatory questions they discuss with patients.
The present analysis labors under several limitations, the first of which is its retrospective design. It is recognised that SABA prescriptions may not necessarily reflect actual usage, which is likely to be lower, for example in poorly resourced settings medications may being passed on to family and friends. The second limitation is due to the fact that investigators have assessed their own prescriptions with no blinding. It may lead to entering into the database “optimised”, “correct” data in cases when investigators have revealed their colleagues did not follow guidelines. Therefore, it could cause underestimation of SABA prescriptions, especially considering that almost all the investigators were specialists, mainly pulmonologists. Although it is typical for Russia that many patients with asthma (especially with more severe disease) are treated by specialists (pulmonologists or allergists), at the same time, majority of patients are regularly seen by – and, in particular, prescribed medicines free of charge by – primary care physicians. One can speculate that the level of knowledge as to the treatment of asthma in general (and of the need to restrict SABA use) may be higher among specialists than among primary care doctors. Also, almost all the centers in our study were from larger cities. In Russia, specialists from larger cities are more willing to participate in clinical trials than primary care physicians (especially from small towns/rural settings). Both facts could lead to a bias in patient selection, limiting the ability to extrapolate the findings of the study to the general Russian population of asthma patients. We may suggest that our data present a “better case scenario” and it is to be expected that SABA over-prescription may be higher in the overall Russian population as well as the number of severe exacerbations and percentage of uncontrolled patients.
The strengths of this study are its multi-center design, relatively large sample of patients across different regions of Russia, which allowed to collect data on asthma control, SABA prescription and current patterns of purchasing SABA OTC, despite lack of established databases.
Conclusions
In the Russian asthma population revealed very high level of SABA over-prescription (37% of all patients) with the mean number of prescribed SABA 4.0 canisters per year. This situation may be associated with the low level of asthma symptom control and frequent severe exacerbations. The frequency of SABA over-prescription was not related to asthma severity.
Thirty percent of the Russian group purchased SABA OTC. More than half of these were already classified as SABA overusers on account of over-prescription. Thus, the main reason for SABA overuse in Russia is over-prescription.
To reduce SABA overuse and improve overall asthma control in Russia, it is necessary to educate both patients and primary care doctors, while also actively implementing up-to-date approaches to the treatment of asthma.
Data Sharing Statement
The authors intend to share individual deidentified participant data. Any scientist can get access to deidentified database via an e-mail to corresponding author.
Disclosure
M Beekman was an employee of AstraZeneca at the time this study was conducted and reports personal fees from AstraZeneca, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
1. Global Initiative for Asthma - GINA. 2019 GINA main report. Available from: https://ginasthma.org/gina-reports/.
2. O’Byrne PM, Jenkins C, Bateman ED. The paradoxes of asthma management: time for a new approach? J Respir Eur. 2017;50(3). doi:10.1183/13993003.01103-2017
3. Stanford RH, Shah MB, D’Souza AO, Dhamane AD, Schatz M. Short-acting β-agonist use and its ability to predict future asthma-related outcomes. Ann Allergy Asthma Immunol. 2012;109(6):403–407. doi:10.1016/j.anai.2012.08.014
4. Suissa S, Ernst P, Boivin JF, et al. A cohort analysis of excess mortality in asthma and the use of inhaled β-agonists. Am J Respir Crit Care Med. 1994;149(3):604–610. doi:10.1164/ajrccm.149.3.8118625
5. Suissa S, Blais L, Ernst P. Patterns of increasing β-agonist use and the risk of fatal or near-fatal asthma. J Respir Eur. 1994;7(9):1602–1609. doi:10.1183/09031936.94.07091602
6. Nwaru BI, Ekström M, Hasvold P, Wiklund F, Telg G, Janson C. Overuse of short-acting β 2 -agonists in asthma is associated with increased risk of exacerbation and mortality: a nationwide cohort study of the global SABINA programme. J Respir Eur. 2020;55(4):1901872. doi:10.1183/13993003.01872-2019
7. Levy ML. The national review of asthma deaths: what did we learn and what needs to change? Breathe. 2015;11(1):15–24. doi:10.1183/20734735.008914
8. O’Byrne PM, Bisgaard H, Godard PP, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med. 2005;171(2):129–136. doi:10.1164/rccm.200407-884OC
9. Beasley R, Holliday M, Reddel HK, et al. Controlled trial of budesonide – formoterol as needed for mild asthma. N Engl J Med. 2019;380(21):2020–2030. doi:10.1056/nejmoa1901963
10. O’Byrne PM, FitzGerald JM, Bateman ED, et al. Inhaled combined budesonide-formoterol as needed in mild asthma. N Engl J Med. 2018;378(20):1865–1876. doi:10.1056/NEJMoa1715274
11. Bateman ED, Reddel HK, O’Byrne PM, et al. As-needed budesonide – formoterol versus maintenance budesonide in mild asthma. N Engl J Med. 2018;378(20):1877–1887. doi:10.1056/nejmoa1715275
12. Reddel HK, FitzGerald JM, Bateman ED, et al. GINA 2019: a fundamental change in asthma management: treatment of asthma with short-acting bronchodilators alone is no longer recommended for adults and adolescents. J Respir Eur. 2019;53(6):1901046. doi:10.1183/13993003.01046-2019
13. Cabrera CS, Nan C, Lindarck N, Beekman MJ, Arnetorp S, van der Valk RJP. SABINA: global programme to evaluate prescriptions and clinical outcomes related to short-acting β2 -agonist use in asthma. J Respir Eur. 2020;55(2):1901858. doi:10.1183/13993003.01858-2019
14. SABINA: an overview of short-acting β2-agonist use in asthma in European countries. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7089727/.
15. Gibson P, Henry D, Francis L, et al. Association between availability of non-prescription β2 agonist inhalers and undertreatment of asthma. J Med Br. 1993;306(6891):1514–1518. doi:10.1136/bmj.306.6891.1514
16. Azzi EA, Kritikos V, Peters MJ, et al. Understanding reliever overuse in patients purchasing over-the-counter short-acting beta2 agonists: an Australian community pharmacy-based survey. BMJ Open. 2019;9(8):e028995. doi:10.1136/bmjopen-2019-028995
17. Nelson HS, Weiss ST, Bleecker EK, Yancey SW, Dorinsky PM. The salmeterol multicenter asthma research trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. In: Chest. Vol. 129. American College of Chest Physicians;2006:15–26. doi:10.1378/chest.129.1.15
18. Aisanov Z, Avdeev S, Arkhipov V, Belevsky A. SYmbicort given as needed in mild asthma (SYGMA study): a retrospective subanalysis of the Russian population. J Asthma. 2021;1–9. doi:10.1080/02770903.2021.1892753
19. Paris J, Peterson EL, Wells K, et al. Relationship between recent short-acting β-agonist use and subsequent asthma exacerbations. Ann Allergy Asthma Immunol. 2008;101(5):482–487. doi:10.1016/S1081-1206(10)60286-4
20. Anis AH, Lynd LD, Wang XH, et al. Double trouble: impact of inappropriate use of asthma medication on the use of health care resources. CMAJ. 2001;164(5):625–631.
21. Nasser S. An imperfect “PAST” lessons learned from the National Review of Asthma Deaths (NRAD) UK. Respir Res. 2016;17(1). doi:10.1186/s12931-016-0393-9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.