Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 12
Rural Vaccination Coverage Among Children Aged 12–23 Months Was Higher Than the Urban Counterparts: A Comparative Cross-Sectional Study in Pawi District, Ethiopia
Authors Gelaye SS Snr , Yenit MK , Baraki AG
Received 24 December 2020
Accepted for publication 1 March 2021
Published 19 March 2021 Volume 2021:12 Pages 119—127
DOI https://doi.org/10.2147/PHMT.S299064
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Roosy Aulakh
Smeneh Sintayehu Gelaye Snr,1 Melaku Kindie Yenit,2 Adhanom Gebreegziabher Baraki2
1Department of Maternal and Child Health, BenshangulGumuz Health Office, BenshangulGumuz, Ethiopia; 2Department of Epidemiology and Biostatistics, College of Medicine and Health Sciences, Institute of Public Health, University of Gondar, Gondar, Ethiopia
Correspondence: Adhanom Gebreegziabher Baraki Tel +251918068580
Email [email protected]
Background: In developing countries like Ethiopia, about 3 million children’s deaths are attributed to vaccine-preventable diseases. Studies especially that try to explain the urban to rural vaccination coverage discrepancy are limited in the study area. This study aimed to assess full vaccination coverage and associated factors among children aged 12– 23 months in rural and urban kebeles of Pawi district.
Methods: A community-based comparative cross-sectional study among urban and rural kebeles was conducted. A multistage sampling method was used to select 456 rural and 229 urban. Data were collected from mothers/caregivers using interviewer-administered questionnaires and vaccination cards. Full vaccination coverage was estimated for both urban and rural kebeles. Multivariable logistic regression analysis was used to identify factors associated with full vaccination. Adjusted Odds Ratio with a 95% confidence interval was reported.
Results: Full vaccination coverage was 67% (95% CI 63% − 71%) and 60% (95% CI: 54% − 66%) among rural and urban residents, respectively. Educational status of the father (AOR=2.69; 95% CI, 1.61– 4.48), using postnatal care (PNC) (AOR=2.60; 95% CI, 1.58– 4.29), discussion on side effect and contraindications of vaccines (AOR=1.82 95% CI, 1.16– 2.88), and Institutional delivery (AOR=4.39, 95% CI 2.17– 8.87) were factors significantly associated with full vaccination among rural children, whereas using Knowledge on immunization schedules (AOR=1.92 95% CI, 1.03– 3.60), PNC (AOR=3.19; 95% CI, 1.57– 6.47), discussion on side effects and contraindications of vaccines (AOR=2.75; 95% CI, 1.4– 5.3) were notably associated with full vaccination among urban children.
Conclusion: The study reveals vaccination coverage was higher in rural compared to urban kebeles but it is still far below the WHO recommended target. Therefore interventions shall be made to improve the coverage especially by using the identified factors like improving PNC service and promoting institutional delivery and health education.
Keywords: full vaccination, associated factors, comparative cross-sectional, Ethiopia
Background
Vaccine-preventable diseases are major public health problems causing a high burden of child morbidity and mortality. Vaccination is an effective public health intervention that protects children from vaccine-preventable diseases.1 Immunization has eradicated smallpox, lowered the global incidence of polio by 99%, and achieved dramatic reductions in illness, disability, and death from vaccine-preventable diseases.2 Immunization is key to reduce deaths among children under 5 years old.3 Globally estimated 2–3 million deaths are averted each year through immunization.4
However, more than 3 million people still die of vaccine-preventable diseases each year and approximately 1.5 million of these deaths are in children less than 5 years.5 A large proportion of these deaths are also in sub-Saharan Africa.6
Ethiopia is aiming to achieve vaccination coverage of ≥90% nationally and ≥80% in every district by the year 2020,7 but reports indicated that the percentage of children who are fully vaccinated remains far below the goal set.8 Frequent measles outbreaks and high childhood morbidity and mortality in the country are among the consequences of low immunization coverage.9 The Ethiopian demographic and health survey of 2016 showed that the full vaccination coverage in the country was 39% and has a high discrepancy between urban (65%) and rural areas (35%).10
Full vaccination status can be affected by several factors like sex7,11 age of the mother, literacy of the mother10,12–14 residence7 ANC follow up10,15 Place of delivery,15–17 knowledge about vaccination18–20 Distance from vaccination sites,11,21 and the number of children in the household.19,22
Pawi, where this study was conducted is one of the districts in BenshangulGumuz region, Ethiopia is mainly affected by vaccine-preventable diseases.23 Even though vaccine-preventable diseases are one of the major public health problems in the study area, studies on immunization coverage and associated factors are lacking besides the available studies in the country used a simple cross-sectional study. Therefore, this study was done to fill the information and methodological gap by determining the prevalence and identify factors using comparative cross-sectional design among urban and rural settings.
Methods
Study Design and Period
Community based comparative cross-sectional study was conducted from April to August 2018.
Study Area and Population
Pawidistrict is located at a distance of 588 km from Addis Ababa the capital city of Ethiopia. The district is administratively subdivided into 17 rural and three urban kebeles. The district has a total population of 61,902 people of which 39,864 (64.4%) are from rural and 22,038 (35.6%) are from urban. Concerning education, 39.86% of the population is considered literate. All mothers/caregivers of children aged 12 to 23 months who lived in the selected kebeles for at least 1 year were included in the study.
Sample Size Determination and Sampling Procedure
The sample size was calculated using double population proportions formula with the assumption of P=15% for rural and 32% for the urban,24 5% level of significance, power of 90%, the urban to the rural ratio of 1 to 2, design effect of 2 and 10% non-response rate. The total sample size was 685 which is 456 for rural and 229 urban residents.
A multi-stage sampling method was used to select study participants. Primarily kebeles were stratified into urban and rural kebeles and then eight kebeles were selected from 17 rural kebeles and two kebeles were selected from three urban kebeles. A sampling frame of households with children aged 12–23 months was prepared after a census of households with target children was carried out, and then by using simple random sampling technique households were selected from each kebeles. If eligible participants were not available for two visits the next household was included in the study.
Variables of the Study
A child is considered fully vaccinated if he or she took at least one dose of BCG vaccine, three doses of Diphtheria-Pertussis-Tetanus-Hepatitis B and Haemophilus influenza type B (DPT-HepB-Hib), three doses of the polio vaccine and one dose of measles vaccine.25 A child who missed at least one dose of the recommended vaccine is considered as not fully vaccinated.24
Data were collected about age, sex, marital status of mother, religion, number of children, monthly family income, occupation, educational status, place of residence, birth order, place of birth for index child, distance from health service, postnatal care usage of mothers, knowledge of mother or caretaker about vaccination schedule, and discussion about side-effects and contraindications of vaccines.
Data Collection, Tool, and Quality Assurance
Data were collected by face-to-face interviews and from vaccination cards using a structured questionnaire. The questionnaire was first prepared in English and translated to Amharic the local language, and then it was again translated back to English. A total of 10 data collectors and 2 supervisors who are health professionals were assigned to the data collection.
Training was given for both data collectors and supervisors for 2 days. Every day after data collection, questionnaires were reviewed and checked for completeness by the supervisors and principal investigator, and the necessary feedback was offered to the data collector the next morning.
Data Processing and Analysis
Data were entered using Epi-info version 7 and analyzed by SPSS version 20. To identify factors associated with full vaccination, Binary logistic regression, and multivariable logistic regression analysis were used. In Binary logistic regression analysis variables with a p-value ≤0.2 were included in multivariable analysis. Adjusted Odds Ratios (AOR) with the corresponding 95% Confidence Interval for variables with P-value <0.05 were used to show the strength and direction of the association. To assess the goodness fit of the modelHosmer Lemeshow goodness of fit test was used.
Results
Socio-Demographic Characteristics of the Study Participants
A total of 685 mothers/caretakers, 456 from rural and 229 from urban, were interviewed making the response rate 100%. The mean age with standard deviation (SD) of the mothers and their children were 28 (±5) years and 17 (±4) months, respectively. Two hundred thirty-nine (52%) and 116 (51%) of the index children were male in rural and urban residents, respectively. Most of the respondents, 432 (94.7%) of rural and 223 (97.4%) of urban mothers, were married. Most participants in rural 297 (65%) and urban 156 (68%) were orthodox Christians. Four hundred (88%) of the rural and 225 (98%) of the urban deliveries were institutional (Table 1).
 |
Table 1 Baseline Characteristics of the Respondent in Pawi District, 2018 |
Vaccination Coverage Among 12–23 Months Aged Children
Vaccination status of 514 (75%) children was assessed by using immunization cards while the remaining 25% were assessed by asking mothers/caregivers verbally. From those who showed the vaccination card of their child majority, 348 (67.7%), were from rural and the rest 166 (32.3%) were from urban. The overall vaccination coverage was64.5% (95% CI: 61% - 68.2%). There was a significant difference between rural and urban residents, which is 67% (95% CI 63% −71%) and 60% (54–66%) respectively.
Factors Associated with Overall Full Vaccination Coverage in Pawi District
Children who live in rural were 1.5 times more likely to be fully vaccinated as compared to urban children[AOR=1.5, 95% CI: (1.1, 2.3)]. Children whose father are able to read and write were 1.7 times more likely to be fully vaccinated than who are unable to read and write[AOR=1.7, 95% CI (1.2, 2.6)]. Children born first were 1.8 times more likely to be fully vaccinated compared with being second and above [AOR=1.8, 95% CI: (1.2, 2.7)]. Children born from mothers who received postnatal service were 2.9 times more likely to be fully vaccinated than their counterparts [AOR=2.9, 95% CI: (2.0, 4.3)]. Children born in health institutions were 3.2 times more likely to be fully vaccinated than those born at home [AOR=3.2, 95% CI: (1.6, 6.3)]. Children born from mother who gets advice on side effects and contraindications of vaccines were two times more likely to be fully vaccinated as compared with their counterparts [AOR=2.0, 95% CI: (1.4, 2.9)] (Table 2).
 |
Table 2 Factor Associated with Overall Full Vaccination Coverage in Pawi District, 2018 |
Factors Associated with Full Vaccination Coverage in Rural Children
Educational status of the father (AOR=2.69; 95% CI, 1.61–4.48), receiving PNC service (AOR=2.60; 95% CI, 1.58–4.29), discussion on side effect and contraindications of vaccines (AOR=1.82 95% CI, 1.16–2.88), and institutional delivery (AOR=4.39, 95% CI 2.17–8.87) were significantly associated with full vaccination among children in the rural setting (Table 3).
 |
Table 3 Factor Associated with Full Vaccination Coverage in the Rural Area of Pawi District, 2018 |
Factors Associated with Full Vaccination Coverage in Urban Children in Pawi District
In the multivariable logistic regression analysis, PNC visit (AOR=3.19; 95% CI, 1.57–6.47), discussion on side effects and contraindications of vaccines (AOR=2.75; 95% CI, 1.4–5.3), and Knowledge on immunization schedules (AOR=1.92 95% CI, 1.03–3.60) were found to be significantly associated predictors of full vaccination in urban areas (Table 4).
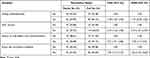 |
Table 4 Factors Associated with Full Vaccination Coverage in Urban Areas of Pawi District, 2018 |
Discussion
The overall full vaccination status among children aged 12–23 months was 65% whereas in rural and urban residents it was 67%and 60% respectively. Factors that affect the overall full vaccination coverage were residence, father’s educational status, being the first child, postnatal service utilization, Institutional delivery, advice on side effect, and contraindication of vaccines. In urban setting PNC visit, discussion on side effects and contraindication of vaccines, and Knowledge on immunization schedules were found to be significantly associated with full vaccination whereas the educational status of the father, receiving PNC service, discussion on side effect and contraindications of vaccines, and Institutional delivery were significantly associated with full vaccination among children in the rural setting.
The overall coverage (65%) is below the WHO recommended coverage of 90%.26 This was similar to many results in different parts of Ethiopia.6,10,24 A significant difference in vaccination coverage between urban and rural children was found. This result was in line with a study conducted in the Tselemti district that showed full vaccination coverage to be higher in rural (80%) than in urban areas (67.5%).14 Similarly, a study conducted in Ambo district central Ethiopia indicated that full vaccination coverage was higher among rural children than that of the urban, 21%, and 15%, respectively.9 The full vaccination coverage among rural residents was higher when compared to a study conducted in rural Nigeria27 but it was low when compared to a study from Istanbul.28
The odds of full vaccination among rural children were nearly two times higher than urban children. This finding was consistent with findings in Burkinafaso and the rural District of Ethiopia,10,14 but it is against studies conducted in Lay Armachiho and Jigjiga Districts.7,23 The higher coverage in rural areas might be due to the health extension program which is mainly focused on improving rural health programs.29
Children whose father can read and write were more likely to be fully vaccinated than children whose father is not able to read and write. This association was observed in the overall model and for the rural residents but it was not significant among the urban residents. This result was consistent with the study conducted at Mizan Aman Town, Sinana district, and Nigeria.8,16,27 Those who read and write could have better information about vaccine-preventable diseases and the use of vaccination which they get from written sources and other sources.
Birth order of children showed a significant association with full vaccination status, being the first child in the family had nearly two times higher odds of full vaccination than being the second and above. This is in line with finding in Ethiopia, Kenya, and Zimbabwe.19,22,30 The first child in many cultures is the favourite one this helps them get a better attention and time which enables him/her complete full course of vaccination.
The odds of full vaccination among children born to mothers who had PNC follow-up was higher as compared to their counterparts. This holds true in all the three models; the overall, rural and urban settings. This finding agrees with studies conducted in the Amibara district in Ethiopia and rural Nigeria.15,27 This shows provision of health education for the mother and vaccination service for the baby during postnatal visits play a significant role in increasing the full vaccination coverage.31
Institutional delivery was found to increase the odds of full vaccination compared to home delivery in the overall and rural settings but it was not significant among urban residents. This result is in line with previous studies in Ethiopia and Nigeria.10,13,27 The reason behind could be due to the fact that after delivery health workers provide advice for mothers on the benefit of vaccination and some of the vaccinations are started on the first day of the baby.
The odds of full vaccination for children whose mother ever discussed side effect and contraindication of vaccines with health workers was higher in all settings as compared to their counterparts. This result was similar to the study conducted in the Arbegona district of southern Ethiopia.19 This could be due to the reassurance of health care providers about the possible side-effects and the available interventions that makes the mothers comfortable to get their children vaccinated.
Children born from mothers who had knowledge of immunization schedules were nearly two times more likely to be fully vaccinated than their counterparts in the urban setting. This result was consistent with other studies in Ethiopia9,19 and Kenya.30 This greatly reduces missing vaccination doses due to not availing themselves in the vaccination dates thus increases the odds of getting the full vaccines.
Since it is a cross-sectional study and the data collected are not exclusively from the vaccination cards recall bias cannot be ruled out. Since the study was also done in a single district in Ethiopia, it may not reflect the whole picture of vaccination coverage in the whole country.
Conclusions
This study reveals vaccination coverage to be higher in rural compared to urban kebeles but it was far below the WHO recommended target. Factors that affect the overall full vaccination coverage were residence, father’s educational status, being the first child, postnatal service utilization, Institutional delivery, advice on side effect, and contraindication of vaccination. In urban setting PNC visit, discussion on side effects and contraindication, and Knowledge on immunization schedules were found to be significantly associated with full vaccination whereas the educational status of the father, receiving PNC service, discussion on side effect and contraindication, and Institutional delivery were significantly associated with full vaccination among children in the rural setting.
Therefore, interventions shall be made to improve the coverage especially by using the identified factors like improving PNC service, promoting institutional delivery, advising, and reassuring mothers on the side effects of vaccinations.
Abbreviations
ANC, Antenatal Care; AOR, Adjusted Odds Ratio; CI, Confidence Interval; PNC, Postnatal care; SD, Standard Deviation; WHO, World Health Organization.
Data Sharing Statement
The data upon which the results are based could be accessed based on a reasonable request made to the corresponding author.
Ethical Consideration
Ethical approval was obtained from the research ethics review committee of the University of Gondar and permission was obtained from the BenshangulGumuz regional health bureau and from the district health office. Verbal informed consent which was accepted according to the ethical review committee was obtained from participants after a complete clarification of the purpose and procedure per the Declaration of Helsinki. All the information from this interview was kept confidential and used only for the study. Personal identifications were not collected.
Author Contributions
All authors made a significant contribution to the work reported in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Disclosure
All authors declared that they have no competing interests.
References
1. World Health Organization. State of the World’s Vaccines and Immunization; 2009.
2. Bilous J, Eggers R, Jarrett S, et al. A new global immunisation vision and strategy. Lancet. 2006;367(9521):0140–6736. doi:10.1016/S0140-6736(06)68625-X
3. Udessa G. Vaccination status and factors associated with it among children aged 12–23 months in Wadera District, South East Ethiopia. Health Care Curr Rev. 2018;6(2):222.
4. World Health Organizaion. Assessment report of the global vaccine action plan strategic advisory group of experts on immunization. [Internet]. Geneva, Switzerland; 2017.
5. Mindra G. All children should enjoy the benefits of immunization. South Sudan Med J. 2016;9(4):75.
6. Hussen M. Assessment of child immunization coverage and associated factors in Kombolcha Woreda Eastern Ethiopia; 2013.
7. Kassahun MB, Biks GA, Teferra AS. Level of immunization coverage and associated factors among children aged 12–23 months in Lay Armachiho District, North Gondar Zone, Northwest Ethiopia: a community based cross sectional study. BMC Res Notes. 2015;8:239. doi:10.1186/s13104-015-1192-y
8. Legesse E, Dechasa W. An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia. BMC Pediatr. 2015;15:31. doi:10.1186/s12887-015-0345-4
9. Etana B, Deressa W. Factors associated with complete immunization coverage in children aged 12–23 months in Ambo Woreda, Central Ethiopia. BMC Public Health. 2012;12:566. doi:10.1186/1471-2458-12-566
10. Animaw W, Taye W, Merdekios B, Tilahun M, Ayele G. Expanded program of immunization coverage and associated factors among children age 12–23 months in Arba Minch town and Zuria District, Southern Ethiopia, 2013. BMC Public Health. 2014;14(1):464.
11. Gualu T, Dilie A. Vaccination coverage and associated factors among children aged 12–23 months in Debre Markos Town, Amhara Regional State, Ethiopia. Adv Public Health. 2017;2017:1–6. doi:10.1155/2017/5352847
12. Salmon DA, Smith PJ, Pan WK, Navar AM, Omer SB, Halsey NA. Disparities in preschool immunization coverage associated with maternal age. Human vaccines. 2009 Aug 1;5(8):557–561.
13. Mbengue MAS, Sarr M, Faye A, et al. Determinants of complete immunization among Senegalese children aged 12–23 months: evidence from the demographic and health survey. BMC Public Health. 2017;17(1):630. doi:10.1186/s12889-017-4493-3
14. Kidane T, Tekie M. Factors influencing child immunization coverage in a rural district of Ethiopia, 2000. Ethiop J Health Dev. 2003;17(2):105–110.
15. Samuel Mebrahtom YB. Magnitude and determinants of childhood vaccination among pastoral community in Amibara District, Afar Regional State, Ethiopia. Res J Med Sci Public Health. 2013;1(No. 3).
16. Meleko A, Geremew M, Birhanu F. Assessment of child immunization coverage and associated factors with full vaccination among children aged 12–23 months at Mizan Aman Town, Bench Maji Zone, Southwest Ethiopia. Int J Pediatr. 2017;2017:1–11. doi:10.1155/2017/7976587
17. Awino OJ. Determinants of immunization coverage among children aged 12–23 months in Kenya; 2013.
18. Elizabeth KGK, Raphael N, Moses E. Factors influencing low immunization coverage among children between 12–23 months in East Pokot, Baringo Country, Kenya. Int J Vaccines. 2015;1(2):00012.
19. Negussie A, Kassahun W, Assegid S, Hagan AK. Factors associated with incomplete childhood immunization in Arbegona district, southern Ethiopia: a case–control study. BMC Public Health. 2016;16:27. doi:10.1186/s12889-015-2678-1
20. Yenit MK, Gelaw YA, Shiferaw AM. Mothers’ health service utilization and attitude were the main predictors of incomplete childhood vaccination in east-central Ethiopia: a case-control study. Arch Public Health. 2018;76(1). doi:10.1186/s13690-018-0261-9
21. Russo G, Miglietta A, Pezzotti P, et al. Vaccine coverage and determinants of incomplete vaccination in children aged 12–23 months in Dschang, West Region, Cameroon: a cross-sectional survey during a polio outbreak. BMC Public Health. 2015;15:630. doi:10.1186/s12889-015-2000-2
22. Mukungwa T. Factors Associated with full Immunization Coverage amongst children aged 12 – 23 months in Zimbabwe. Afr Pop Stud. 2015;29(No. 2). doi:10.11564/29-2-745
23. Mohamud AN, Feleke A, Worku W, Kifle M, Sharma HR. Immunization coverage of 12–23 months old children and associated factors in Jigjiga District, Somali National Regional State, Ethiopia. BMC Public Health. 2014;14:865. doi:10.1186/1471-2458-14-865
24. Mohamud AN. Immunization coverage of 12–23 months old children and associated factors in Jigjiga District, Somali National Regional State, Ethiopia. BMC Public Health. 2014;14(1):1–9.
25. EDHS E. Demographic and health survey 2016: key indicators report. The DHS Program ICF; 2016.
26. WHO. Immunization, vaccines and biologicals; 2014. Available from: https://www.who.int/immunization/newsroom/press/immunization_coverage_july2014/en/.
27. Odusanya OO, Alufohai EF, Meurice FP, Ahonkhai VI. Determinants of vaccination coverage in rural Nigeria. BMC Public Health. 2008;8. doi:10.1186/1471-2458-8-381
28. Torun SD, Bakırcı N. Vaccination coverage and reasons for non-vaccination in a district of Istanbul. BMC Public Health. 2006;6(1):125. doi:10.1186/1471-2458-6-125
29. Workie NW, Ramana GN. The health extension program in Ethiopia; 2013.
30. Kawakatsu Y, Honda S. Individual-, family-and community-level determinants of full vaccination coverage among children aged 12–23 months in western Kenya. Vaccine. 2012;30(52):7588–7593. doi:10.1016/j.vaccine.2012.10.037
31. Anjum Q, Omair A, Inam S, Ahmed Y, Usman Y, Shaikh S. Improving vaccination status of children under five through health education. J Pak Med Assoc. 2004;54(12):610–613.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
