Back to Journals » Patient Preference and Adherence » Volume 16
Role of Rituximab in the Treatment of Pemphigus Vulgaris: Patient Selection and Acceptability
Authors Ciolfi C , Sernicola A , Alaibac M
Received 29 July 2022
Accepted for publication 29 October 2022
Published 7 November 2022 Volume 2022:16 Pages 3035—3043
DOI https://doi.org/10.2147/PPA.S350756
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Christian Ciolfi *, Alvise Sernicola *, Mauro Alaibac
Dermatology Unit, Department of Medicine (DIMED), University of Padua, Padua, Italy
*These authors contributed equally to this work
Correspondence: Alvise Sernicola, Dermatology Unit, Department of Medicine (DIMED), University of Padua, Via Vincenzo Gallucci, 4, Padua, 35121, Italy, Tel/Fax +39 049 821 2924, Email [email protected]
Abstract: Anti-CD20 monoclonal antibody rituximab is an approved adjuvant treatment, in combination with oral corticosteroids, for patients with pemphigus vulgaris, a severe and potentially life-threatening autoimmune blistering skin disorder. Updated approaches to the management of pemphigus vulgaris support rituximab as a first-line adjuvant treatment to induce remission early in the course of disease; however, its feasibility in the clinical setting is often reduced by a series of limitations, including high cost of this biological drug, physician and patient concern for the risk of adverse reactions, and uncertainty regarding the optimum dosing and schedule of administration. The standard approved rituximab dosages, which are derived from lymphoma protocols, have been recognized to exceed the effective dose required for inducing B cell depletion, since the B cell burden in pemphigus vulgaris is much lower than in lymphoproliferative disorders. To overcome these limitations, recent research has investigated alternative regimens of rituximab, using lower doses of the drug. Moreover, differences in patient and disease characteristics that are highlighted in the literature strongly suggest that therapy should be tailored individually on a case-by-case basis: personalized treatment schedules may be necessary to optimize response to treatment and tolerability in different subjects, with the possibility of repeated infusions for severe forms and in case of relapse. Finally, low-dose regimens of rituximab were suggested to be favorable during the COVID-19 pandemic by providing a lesser degree of immune cell depletion while retaining a sufficient response. In conclusion, the current literature suggests that lower-dose regimens of rituximab are not only tolerable and cost-effective but may also be associated with a positive response in pemphigus vulgaris, comparable to that achieved with higher doses especially in early disease. Further evidence from rigorous clinical trials will be required to optimize lower-dose regimens of RTX and establish their position within the treatment scenario of pemphigus vulgaris.
Keywords: pemphigus, rituximab, low dose, patient acceptability, treatment acceptability
Introduction
Rituximab (RTX) is an anti-CD20 monoclonal antibody, first approved by the Food and Drug Administration (FDA) in 1997 for a non-Hodgkin lymphoma orphan indication. Its subsequent approval for other conditions provided a significant advancement in the management of several lymphoproliferative and immune-mediated diseases. This chimeric murine/human antibody is produced in Chinese hamster ovary suspension cultures and is purified by affinity and ion-exchange chromatography, followed by inactivation of any containing viruses. Currently, the FDA has approved three RTX biosimilars, while patients throughout Europe have access to five RTX biosimilars: the development of biosimilars may improve patient access to RTX by lowering the cost of the drug.1–3
The aim of this article is to review current knowledge on RTX in the treatment of pemphigus vulgaris (PV). However, rather than extensively reporting results of published studies in this context – that have been covered in depth by recent reviews4 – the authors specifically focused on issues concerning patient selection and on the treatment protocols that may be associated to improved acceptability. The latter include first-line treatment with RTX – as “first adjunctive immunosuppressive agent” – and lower-dose regimens of the drug.
Review
Pemphigus
Pemphigus refers to a group of autoimmune blistering dermatoses characterized by intraepidermal acantholysis and consequent formation of blisters and erosions due to circulating pathogenic autoantibodies. Target antigens are desmosomal transmembrane glycoproteins desmogleins 1 and 3, which are key contributors to interkeratinocyte adhesion. Pemphigus is recognized as a prototype of antibody-mediated autoimmunity; however, there is strong evidence supporting the role of abnormal T cell subpopulations in autoimmune bullous skin disorders. Specifically, Th2 cells and T follicular helper cells promote the survival of self-reactive B cells and their production of autoantibodies, while Th17 cells support the inflammatory response following skin damage. Moreover, an imbalance of regulatory T cells leads to the spontaneous activation of autoreactive CD4+ T cells, which further promotes autoantibody production.5,6
Different clinical subtypes of pemphigus with variable cutaneous and mucous involvement are recognized; these include PV, pemphigus foliaceus, IgA pemphigus, pemphigus herpetiformis, and paraneoplastic pemphigus. PV is the prevalent subtype in this group and features flaccid blisters on any area of the cutaneous surface, associated with painful mucous membrane erosions which can be the presenting sign of the disease.7,8
The epidemiology of PV is variable according to geographic and ethnical factors. The disease is most common in individuals of Ashkenazi ethnicity and in those of Mediterranean descent. Moreover, hereditary associations have been seldom reported in the literature and may be relevant to specific populations; the association with certain HLA haplotypes and alleles has been reported in Brazilian subjects with pemphigus9,10 and in family studies conducted in Brazil and in Italy.11,12 Such genetic associations hint at a possible genetic predisposition that may underlie susceptibility to PV and to other autoimmune disorders. In this regard, there is scant and preliminary evidence linking PV to autoimmune comorbidities; the most commonly reported in the literature are autoimmune thyroid diseases, rheumatoid arthritis, type 1 diabetes mellitus, Sjogren’s syndrome, systemic lupus erythematosus, inflammatory bowel diseases, and alopecia areata. These autoimmune disorders have been additionally observed with higher frequencies in first-degree relatives of patients with pemphigus compared to unrelated controls.8,13 Future studies are needed to elucidate whether these are sporadic associations or the expression of a predisposition to autoimmunity, which might potentially be relevant to the response to B cell depleting therapies in pemphigus.
Rituximab
RTX targets CD20, a 33–37 kDa transmembrane surface molecule belonging to the membrane-spanning 4-domain family A (MS4A) protein family. CD20 is expressed as homodimers or homo-tetramers by pre-B lymphocytes and B lymphocytes, but its expression is lost once these develop into plasma cells.14,15
Although its natural ligand still eludes detection and mice carrying a CD20 gene disruption display an almost normal B cell differentiation,16 the association of CD20 with B cell receptor (BCR) suggests a role in the BCR pathway; specifically, there is evidence of CD20 acting as a calcium channel during BCR signaling.17 CD20 is an intriguing molecule to target in lymphoproliferative and immune-mediated diseases. As a matter of fact, it is expressed on most of B cell malignancies, but not on pre-B hematopoietic stem cells and terminally differentiated plasma cells, which grants tumor specificity, B cell reconstitution after treatment, and maintenance of pre-existing plasmatic IgG levels. Moreover, CD20 does not seem to have a natural ligand, therefore RTX has no known endogenous binding competitors. Also, CD20 is highly expressed by B lineage cells and is neither modulated nor shed from the cell surface after RTX binding.15,18 Several mechanisms of action are described for RTX: complement-dependent cytotoxicity, consequent to C1q binding to RTX-opsonized B cells; antibody-dependent cell-mediated cytotoxicity, dependent on natural killer cell activation mediated by the interaction between the Fc portion of RTX with their FcγIIIa receptor; antibody-dependent cellular phagocytosis, consequent to monocytes binding to RTX-opsonized B cells through their Fcγ receptor; and direct induction of apoptosis, through the activation of the caspase cascade. Moreover, RTX indirectly downregulates autoreactive CD4+ Th cells by disrupting the antigen-presenting role of B lymphocytes.14,19,20 In autoimmune diseases like pemphigus, RTX depletes B cells and lymphoid resident memory B cells, with a consequent decrease of circulating pathogenic anti-desmoglein autoantibodies; however, RTX is thought to also modulate both humoral and acquired immune function deeply in pemphigus. This hypothesis is supported by the duration of disease remission that is frequently longer than the time to B cell reconstitution in the peripheral blood. Patients with long-lasting remission display a high naïve/memory B cell ratio, with increased regulatory B cells and T cells; in contrast, patients with short-lasting remission display a low naïve/memory B cell ratio, with early reappearance of autoreactive CD4+ Th cells. Factors for predicting the duration of response are still not identified.21
Indications and Dosing of Rituximab
Currently, RTX is approved by the FDA for the treatment of CD20-positive non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, microscopic polyangiitis, and PV. Moreover, it has orphan designation for Rasmussen encephalitis and immune thrombocytopenic purpura, and has been substantially used off-label for other immune-mediated conditions, including neurologic, hematologic, dermatologic, oncologic, and autoimmune diseases.22 In 2018, RTX was approved by the FDA for the treatment of PV in adult patients with moderate-to-severe disease as a steroid-sparing immunosuppressant in adjunction to corticosteroids. However, there is still uncertainty regarding the optimal RTX regimen to adopt in PV. Originally, patients had been treated with the lymphoma protocol (4 weekly infusions of 375 mg/m2 RTX).23,24 Nowadays, the induction regimen recommended by European and American guidelines consists of 2 infusions of 1000 mg RTX at a 2-week interval with a tapering course of glucocorticoids. As for the maintenance regimen, European guidelines recommend infusions of 500 mg RTX at months 12 and 18, and then every six months thereafter according to the clinical conditions of patients; American guidelines, instead, recommend infusions of 500 mg RTX at month 12 and then every six months thereafter according to the clinical conditions of patients.25,26
Lower-Dose Regimens of Rituximab
The optimal RTX regimen for PV has not been established yet. Dose-finding trials for RTX in PV and other non-malignant conditions are missing, and the standard protocols exceed the effective dose required for inducing B cell depletion according to pharmacological data provided by a 2018 study performed on healthy volunteers, the results of which are summarized in Table 1.27 Compared to lymphoproliferative disorders, the B cell burden is lower in autoimmune disease28,29 and specifically in PV,30 where short-lived plasma cells responsible for the production of pathogenic autoantibodies are continuously replenished. On this basis, a linear correlation between B cell depletion and therapeutic effect cannot be hypothesized, and clinical studies have been proposed to investigate the response to lower dosages of RTX in PV.31 A 2021 review collected published evidence on the use of low-dose RTX for the treatment of PV: nine studies were included, with RTX dosages varying between modified dose (3 × 375 mg/m2 or 3 × 500 mg), low dose (2 × 375 mg/m2 or 2 × 500 mg), and ultra-low dose (≤500 mg for a cycle, either single or multiple infusions).32–40 The authors of the review suggested that low-dose and ultra-low-dose protocols should be used to induce the remission in patients with mild-to-moderate PV, with the possibility of repeated infusions for more severe forms.41 These data confirmed the results of a 2015 systematic review and meta-analysis, comparing different RTX regimens in the treatment of PV. The authors found no superiority of high-dose (near or ≥2000 mg/cycle) over low-dose protocols (<1500 mg/cycle) in terms of complete remission, time to disease control and complete remission, and relapse rates; however, the high-dose RTX regimen was associated with longer maintenance of complete remission.42 Specifically, a study on 27 subjects highlighted decreased time to complete remission and rate of relapse associated to high-dose RTX,32 while a trial on 22 subjects with PV reported no difference in complete remission and time to disease control.37 An additional study involving 23 patients showed comparable clinical outcomes between high and low doses in severe PV.35 Finally, a pilot study by the authors of the present review enrolled 8 patients with PV (diagnosed according to suggestive clinical presentation and histology and confirmed by positive direct immunofluorescence) that received a single infusion of RTX 200 mg: complete remission was achieved by 5 subjects and partial response by an additional 3. At the end of the follow-up period only one subject was off corticosteroid therapy and another patient had relapsed.40 High-quality randomized control trials and large-scale prospective studies are currently missing and needed to provide robust evidence supporting the efficacy of low and ultra-low RTX in PV. The severity of PV and the concomitant use of systemic steroids constitute predictable confounding factors that should be taken into account by future investigations. Moreover, low-dose RTX protocols have also been successfully adopted for several off-label indications.43 However, further studies are required to establish the optimal RTX regimen for immunobullous diseases like PV.
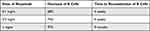 |
Table 1 Effect of Increasing Doses of Rituximab on B Cells |
Patient Selection
PV is a prototypical antibody-mediated autoimmune disease owing to the clear definition of its major antigen and the extensive demonstration of the pathogenicity of circulating antigen-specific autoantibodies. Such level of understanding of the pathogenesis is rare in the field of autoimmunity and has supported the shift from broad immunosuppression to the introduction of pathogenesis-based approaches. Traditional treatment armamentarium for PV is based on systemic corticosteroids which are often combined with a steroid-sparing adjuvant. PV is a severe dermatological condition with potentially devastating consequences and requires high doses of systemic steroids, in the range of 1–1.5 mg/kg/d of prednisone. An adjuvant immunosuppressor is usually added to spare the dose of prednisone: azathioprine, mycophenolate mofetil, and methotrexate are widely employed, while cyclophosphamide is generally considered as a further line owing to its high burden of toxicity.44–47 Although the use of these agents is common in the clinical practice and widely described in the literature, the lack of high-quality evidence derived from randomized controlled trials has prevented the formulation of univocal treatment recommendations for a standardized treatment approach.48 Moreover, standardization is still lacking when measuring disease severity, and systematic use of the Pemphigus Disease Area Index (PDAI) by clinicians needs to be further encouraged.
Subjects receiving high-dose corticosteroids and traditional immunosuppressive drugs, as well as those receiving biologic agents, need to be thoroughly screened for malignancies and current infections according to the comprehensive screening work-up proposed in the literature.49 Considering the potential risk of infections during immune-modulating treatments, it is generally recommended that patients receive available vaccinations, especially against respiratory tract infectious agents. Ideally, immunization should be administered prior to initiation of these regimens as certain live vaccines are contraindicated during iatrogenic immunosuppression.44 The issue of vaccination has highly concerned both patients and physicians during the COVID-19 pandemic, since efforts for mass immunization privileged fragile subjects with chronic immune-mediated conditions receiving immune modulators, especially in the first phases.
Within this established treatment scenario, interventions aimed at pathogenic autoantibodies or autoreactive immune cells are regarded as second-line options reserved for refractory cases or when high-dose corticosteroids are contraindicated.50 Apart from RTX, these interventions include high-dose intravenous autoantibodies, immunoadsorption, and other novel approaches that are outside the scope of this review.51 However, the development of pathogenesis-based approaches in PV led to challenge this sequential approach and to suggest a potential benefit from the early introduction of targeted approaches as first-line therapy. In the prospective, multicenter, parallel-group, open-label randomized RITUX3 trial, first-line use of RTX combined with short-term prednisone was assessed in patients with newly diagnosed pemphigus; early introduction of RTX resulted in greater efficacy and safety compared to prednisone alone.52 Specifically, the rationale for early introduction of RTX is derived by experimental evidence in vivo that B cell epitopes do not change during the course of PV as epitope spreading is an exceptional event53 and that autoreactive plasma cells in PV are short-lived.20 Further studies have highlighted, however, that clones of autoreactive B cells are able to persist over time and become responsible for clinical relapses that follow periods of remission.54 These long-lived plasma cells are thought to reside within the bone marrow or peripheral sites of inflammation and are being investigated as therapeutic targets in certain autoimmune disorders.55,56 It is at present speculative whether these could become potential targets for future treatments of PV. Though we do not advocate the measurement of anti-desmoglein 3 autoantibodies as a substitute for the clinical evidence of disease remission, its decline in the serum has been generally reported in parallel with clinical improvement, further supporting the notion that RTX abolishes disease-specific autoreactive plasma cells.20
While an updated approach to the management of PV may support RTX as a first-line adjuvant treatment,57 the optimum dosing and schedule of administration are still inconclusively defined. Moreover, personalized treatment schedules may be necessary to optimize response to treatment and tolerability in different subjects.
Acceptability of the Treatment Protocol
Response to both high and low doses of RTX has been documented by several studies in the literature (Table 2).31–40,58,59 Compared to steroid-only therapy, regimens containing RTX achieve a three-fold higher chance of complete remission.52,60 However, rates of response after administration of different doses of RTX are not easily comparable considering potential confounders such as the extreme variability of the cumulative dosing of corticosteroids administered. Standardized outcomes of clinical response are also lacking, but it must be noted that a significant difference in the quality of life, assessed through DLQI and Skindex scores, has been reported with different regimens of RTX compared to steroid-only treatment.37,52 Moreover, differences in patient and disease characteristics that are highlighted in the literature strongly suggest that therapy should be tailored individually on a case-by-case basis.41 Early treatment with RTX, that is a short duration of disease ≤6 months, has been associated with higher complete remission and also with shorter time to remission and longer duration of remission.61
 |
Table 2 Low-Dose Rituximab Regimens for the Treatment of Pemphigus Vulgaris |
In contrast, relapse of disease commonly occurs in PV subjects that previously received RTX, with reported frequencies up to 81% after a follow-up of 79 months.62 Relapse is reported following both high- and low-dose regimens of RTX, though certain studies showed that high-dose RTX may achieve longer duration of remission.42 While some studies report remission after a single cycle of RTX,21,63 other authors suggested repeated doses to consolidate remission.52 Moreover, the timing of additional doses of RTX is uncertain and may be affected by concurrent immunosuppressor use, which is heterogeneous among studies.21,64 However, the observation of relapse even after high doses of RTX hints at disease mechanisms, potentially involving persistent memory B cell clones, that are not susceptible to the action of the drug.
Different regimens of RTX might be preferred according to the severity of disease; however, inconsistent definitions of severity and response among studies make direct comparisons unfeasible and will require further investigation in the future.42,57 In this regard, there is growing evidence that early RTX may be the appropriate treatment for patients with moderate-to-severe PV: patients undergoing RTX as first-line therapy show a better response and tolerability if compared to patients receiving previous conventional adjuvant therapies.61,65,66 Finally, concerns on the safety of RTX may limit its utility in the clinical practice and its acceptability by patients. The adverse effects of RTX are potentially severe and life-threatening conditions which may occur early during infusion or at later times. Early reactions include flu-like symptoms and cardiovascular effects that have been generally controlled by slowing the rate of infusion or by stopping it entirely.35,36 Moreover, hypersensitivity reactions have been reported in up to 25% of subjects requiring interruption of infusion, which in practice equals to administration of a low dose of RTX.34 Delayed complications of RTX are mainly related to the risk of infection, which is increased by the concurrent prednisone use in virtually all subjects.
Recently, the management of immune-mediated skin disorders has been revised in response to the threat of COVID-19. Current clinical practice guidelines support continuation of immunosuppressive therapies in patients with chronic diseases who require them, with the exception of high-dose glucocorticoids, which were associated with worse COVID-19 outcomes.67,68 A retrospective cohort study investigated whether patients undergoing immunosuppressive therapies for solid organ transplantations, cancers, or rheumatological disorders were at higher risk for mechanical ventilation or in-hospital death due to COVID-19 compared to non-immunosuppressed individuals. The authors found that only RTX negatively impacted COVID-19 outcomes.69 Therefore, low-dose regimens of RTX may prove favorable in this context by providing a lesser degree of immune cell depletion while retaining a sufficient response, especially in early disease.41
Overall, while a better safety profile may be theoretically achieved by low-dose RTX regimens, the literature suggests a similar tolerability of both high-dose and low-dose RTX.1,41
Conclusion
Further clinical studies with rigorous design are needed to characterize the efficacy and safety of a first-line ultra-low-dose RTX. Additionally, in vitro studies are required to investigate the cellular mechanisms underlying long-term remission in PV patients. An in-depth understanding of these mechanisms might enable us to overcome the current main limitation of treatments targeting B cells, which is the risk of relapse.51 PV is a prototypical disorder within the field of autoimmunity owing to the clear pathogenicity of serum autoantibodies produced by specific B cell clones, and as such the results of research in this disease may be similarly relevant for other autoimmune conditions in the skin or other organs that are still less defined. The notion that the B cell burden in PV is dramatically lower compared to that in lymphoproliferative disorders provides a theoretical justification for the use of an ultra-low dose of RTX in the treatment of PV.31 Moreover, a major concern from both the clinician’s and the patient’s perspective is immediate and delayed adverse reactions to RTX: while the former are generally managed or prevented by stopping the infusion which equals to administering a low dose, the latter may also benefit from a lower cumulative dose of RTX. The ultra-low dose of RTX is not only tolerable but has also been associated with a positive response of PV, comparable to that achieved with high doses, especially in early disease.
Finally, a significant limitation to the feasibility of the full-dose regimen of RTX in the clinical setting is the high cost of this biological drug: this may be overcome by ultra-low-dose protocols that could prove cost-effective in inducing remission and that may be readministered in case of relapse.
Funding
This research received no external funding.
Disclosure
Christian Ciolfi and Alvise Sernicola are co-first authors for this study. The authors declare no conflicts of interest in this work.
References
1. Kaegi C, Wuest B, Schreiner J, et al. Systematic review of safety and efficacy of rituximab in treating immune-mediated disorders. Front Immunol. 2019;10:1990. doi:10.3389/fimmu.2019.01990
2. Cheesman S. Introduction of biosimilar rituximab: a hospital perspective. Hemasphere. 2020;5(1):e515. doi:10.1097/HS9.0000000000000515
3. How the U.S. compares to Europe on biosimilar approvals and products in the pipeline Updated March 14, 2022. JD Supra. Available from: https://www.jdsupra.com/legalnews/how-The-u-s-compares-to-europe-on-7635750./.
4. Kridin K, Ahmed AR. The evolving role of rituximab in the treatment of pemphigus vulgaris: a comprehensive state-of-The-art review. Expert Opin Biol Ther. 2021;21(4):443–454. doi:10.1080/14712598.2021.1874915
5. Fang H, Li Q, Wang G. The role of T cells in pemphigus vulgaris and bullous pemphigoid. Autoimmun Rev. 2020;19(11):102661. doi:10.1016/j.autrev.2020.102661
6. Amber KT, Staropoli P, Shiman MI, Elgart GW, Hertl M. Autoreactive T cells in the immune pathogenesis of pemphigus vulgaris. Exp Dermatol. 2013;22(11):699–704. doi:10.1111/exd.12229
7. Malik AM, Tupchong S, Huang S, Are A, Hsu S, Motaparthi K. An updated review of pemphigus diseases. Medicina. 2021;57(10):1080. doi:10.3390/medicina57101080
8. Kridin K. Pemphigus group: overview, epidemiology, mortality, and comorbidities. Immunol Res. 2018;66(2):255–270. doi:10.1007/s12026-018-8986-7
9. Brochado MJF, Nascimento DF, Campos W, Deghaide NHS, Donadi EA, Roselino AM. Differential HLA class I and class II associations in pemphigus foliaceus and pemphigus vulgaris patients from a prevalent Southeastern Brazilian region. J Autoimmun. 2016;72:19–24. doi:10.1016/j.jaut.2016.04.007
10. Walsh P, Brochado MJF, Vernal S, et al. Relationship between pemphigus and American tegumentary leishmaniasis: insights from serological and genetic profiles. Trans R Soc Trop Med Hyg. 2017;111(8):345–353. doi:10.1093/trstmh/trx065
11. Salathiel AM, Brochado MJF, Kim O, Deghaide NHS, Donadi EA, Roselino AM. Family study of monozygotic twins affected by pemphigus vulgaris. Hum Immunol. 2016;77(7):600–604. doi:10.1016/j.humimm.2016.05.005
12. Fania L, Moro F, De Paolis E, et al. Pemphigus vulgaris in two pairs of siblings from two unrelated Italian families: human leukocyte antigen genotypes, ST18 mutation and immunological profile. J Dermatol. 2021;48(2):211–214. doi:10.1111/1346-8138.15656
13. Parameswaran A, Attwood K, Sato R, Seiffert-Sinha K, Sinha AA. Identification of a new disease cluster of pemphigus vulgaris with autoimmune thyroid disease, rheumatoid arthritis and type I diabetes. Br J Dermatol. 2015;172(3):729–738. doi:10.1111/bjd.13433
14. Pavlasova G, Mraz M. The regulation and function of CD20: an “enigma” of B-cell biology and targeted therapy. Haematologica. 2020;105(6):1494–1506. doi:10.3324/haematol.2019.243543
15. Cragg MS, Walshe CA, Ivanov AO, Glennie MJ. The biology of CD20 and its potential as a target for mAb therapy. Curr Dir Autoimmun. 2005;8:140–174. doi:10.1159/000082102
16. O’Keefe TL, Williams GT, Davies SL, Neuberger MS. Mice carrying a CD20 gene disruption. Immunogenetics. 1998;48(2):125–132. doi:10.1007/s002510050412
17. Li H, Ayer LM, Lytton J, Deans JP. Store-operated cation entry mediated by CD20 in membrane rafts. J Biol Chem. 2003;278(43):42427–42434. doi:10.1074/jbc.M308802200
18. Casan JML, Wong J, Northcott MJ, Opat S. Anti-CD20 monoclonal antibodies: reviewing a revolution. Hum Vaccin Immunother. 2018;14(12):2820–2841. doi:10.1080/21645515.2018.1508624
19. Abulayha A, Bredan A, El Enshasy H, Daniels I. Rituximab: modes of action, remaining dispute and future perspective. Future Oncol. 2014;10(15):2481–2492. doi:10.2217/fon.14.146
20. Eming R, Nagel A, Wolff-Franke S, Podstawa E, Debus D, Hertl M. Rituximab exerts a dual effect in pemphigus vulgaris. J Invest Dermatol. 2008;128(12):2850–2858. doi:10.1038/jid.2008.172
21. Didona D, Maglie R, Eming R, Hertl M. Pemphigus: current and Future Therapeutic Strategies. Front Immunol. 2019;10:1418. doi:10.3389/fimmu.2019.01418
22. Delate T, Hansen ML, Gutierrez AC, Le KN. Indications for rituximab use in an integrated health care delivery system. J Manag Care Spec Pharm. 2020;26(7):832–838. doi:10.18553/jmcp.2020.26.7.832
23. Craythorne E, du Viver A, Mufti GJ, Warnakulasuriya S. Rituximab for the treatment of corticosteroid-refractory pemphigus vulgaris with oral and skin manifestations. J Oral Pathol Med. 2011;40(8):616–620. doi:10.1111/j.1600-0714.2011.01017.x
24. Fortuna G, Calabria E, Ruoppo E, et al. The use of rituximab as an adjuvant in the treatment of oral pemphigus vulgaris. J Oral Pathol Med. 2020;49(1):91–95. doi:10.1111/jop.12951
25. EMA MabThera. European medicines agency; September 17, 2018.Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/mabthera.
26. Genentech. Rituxan® (rituximab [Oncology]). Information for healthcare providers. Available from: https://www.gene.com/medical-professionals/medicines/rituxan-oncology.
27. Schoergenhofer C, Schwameis M, Firbas C, et al. Single, very low rituximab doses in healthy volunteers - a pilot and a randomized trial: implications for dosing and biosimilarity testing. Sci Rep. 2018;8(1):124. doi:10.1038/s41598-017-17934-6
28. Hale M, Rawlings DJ, Jackson SW. The long and the short of it: insights into the cellular source of autoantibodies as revealed by B cell depletion therapy. Curr Opin Immunol. 2018;55:81–88. doi:10.1016/j.coi.2018.10.008
29. Hoyer BF, Moser K, Hauser AE, et al. Short-lived plasmablasts and long-lived plasma cells contribute to chronic humoral autoimmunity in NZB/W mice. J Exp Med. 2004;199(11):1577–1584. doi:10.1084/jem.20040168
30. Mouquet H, Musette P, Gougeon ML, et al. B-cell depletion immunotherapy in pemphigus: effects on cellular and humoral immune responses. J Invest Dermatol. 2008;128(12):2859–2869. doi:10.1038/jid.2008.178
31. Alaibac M. Ultra-low dosage regimen of rituximab in autoimmune blistering skin conditions. Front Immunol. 2018;9:810. doi:10.3389/fimmu.2018.00810
32. Kim JH, Kim YH, Kim MR, Kim SC. Clinical efficacy of different doses of rituximab in the treatment of pemphigus: a retrospective study of 27 patients. Br J Dermatol. 2011;165(3):646–651. doi:10.1111/j.1365-2133.2011.10411.x
33. Horváth B, Huizinga J, Pas HH, Mulder AB, Jonkman MF. Low-dose rituximab is effective in pemphigus. Br J Dermatol. 2012;166(2):405–412. doi:10.1111/j.1365-2133.2011.10663.x
34. Chay J, Donovan P, Cummins L, Kubler P, Pillans P. Experience with low-dose rituximab in off-label indications at two tertiary hospitals. Intern Med J. 2013;43(8):871–882. doi:10.1111/imj.12207
35. Cho HH, Jin SP, Chung JH. Clinical experiences of different dosing schedules of rituximab in pemphigus with various disease severities. J Eur Acad Dermatol Venereol. 2014;28(2):186–191. doi:10.1111/jdv.12080
36. Londhe PJ, Kalyanpad Y, Khopkar US. Intermediate doses of rituximab used as adjuvant therapy in refractory pemphigus. Indian J Dermatol Venereol Leprol. 2014;80(4):300–305. doi:10.4103/0378-6323.136832
37. Kanwar AJ, Vinay K, Sawatkar GU, et al. Clinical and immunological outcomes of high- and low-dose rituximab treatments in patients with pemphigus: a randomized, comparative, observer-blinded study. Br J Dermatol. 2014;170(6):1341–1349. doi:10.1111/bjd.12972
38. Gupta J, Raval RC, Shah AN, et al. Low-dose rituximab as an adjuvant therapy in pemphigus. Indian J Dermatol Venereol Leprol. 2017;83(3):317–325. doi:10.4103/ijdvl.IJDVL_1078_14
39. Robinson AJ, Vu M, Unglik GA, Varigos GA, Scardamaglia L. Low-dose rituximab and concurrent adjuvant therapy for pemphigus: protocol and single-centre long-term review of nine patients. Australas J Dermatol. 2018;59(1):e47–e52. doi:10.1111/ajd.12571
40. Russo I, Miotto S, Saponeri A, Alaibac M. Ultra-low dose rituximab for refractory pemghigus vulgaris: a pilot study. Expert Opin Biol Ther. 2020;20(6):673–678. doi:10.1080/14712598.2020.1727440
41. Tavakolpour S, Aryanian Z, Seirafianpour F, et al. A systematic review on efficacy, safety, and treatment-durability of low-dose rituximab for the treatment of Pemphigus: special focus on COVID-19 pandemic concerns. Immunopharmacol Immunotoxicol. 2021;43(5):507–518. doi:10.1080/08923973.2021.1953063
42. Wang HH, Liu CW, Li YC, Huang YC. Efficacy of rituximab for pemphigus: a systematic review and meta-analysis of different regimens. Acta Derm Venereol. 2015;95(8):928–932. doi:10.2340/00015555-2116
43. Fernandez-Martinez M, Esterlich E, Vallano A, Danés I, Agustí A. Off-label uses of low-dose Rituximab: a systematic review of the Literature. Clin Ther. 2015;37(8):e117–e118. doi:10.1016/j.clinthera.2015.05.336
44. Hertl M, Jedlickova H, Karpati S, et al. Pemphigus. S2 Guideline for diagnosis and treatment--guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV). J Eur Acad Dermatol Venereol. 2015;29(3):405–414. doi:10.1111/jdv.12772
45. Beissert S, Werfel T, Frieling U, et al. A comparison of oral methylprednisolone plus azathioprine or mycophenolate mofetil for the treatment of pemphigus. Arch Dermatol. 2006;142(11):1447–1454. doi:10.1001/archderm.142.11.1447
46. Beissert S, Mimouni D, Kanwar AJ, Solomons N, Kalia V, Anhalt GJ. Treating pemphigus vulgaris with prednisone and mycophenolate mofetil: a multicenter, randomized, placebo-controlled trial. J Invest Dermatol. 2010;130(8):2041–2048. doi:10.1038/jid.2010.91
47. Chams-Davatchi C, Mortazavizadeh A, Daneshpazhooh M, et al. Randomized double blind trial of prednisolone and azathioprine, vs. prednisolone and placebo, in the treatment of pemphigus vulgaris. J Eur Acad Dermatol Venereol. 2013;27(10):1285–1292. doi:10.1111/j.1468-3083.2012.04717.x
48. Zhao CY, Murrell DF. Pemphigus vulgaris: an evidence-based treatment update. Drugs. 2015;75(3):271–284. doi:10.1007/s40265-015-0353-6
49. Calabria E, Fortuna G, Aria M, Mignogna MD. Autoimmune mucocutaneous blistering diseases in the south of Italy: a 25-year retrospective study on 169 patients. J Oral Pathol Med. 2020;49(7):672–680. doi:10.1111/jop.13059
50. Enk AH, Hadaschik EN, Eming R, et al. European Guidelines (S1) on the use of high-dose intravenous immunoglobulin in dermatology. J Eur Acad Dermatol Venereol. 2016;30(10):1657–1669. doi:10.1111/jdv.13725
51. Pollmann R, Schmidt T, Eming R, Hertl M. Pemphigus: a comprehensive review on pathogenesis, clinical presentation and novel therapeutic approaches. Clin Rev Allergy Immunol. 2018;54(1):1–25. doi:10.1007/s12016-017-8662-z
52. Joly P, Maho-Vaillant M, Prost-Squarcioni C, et al. First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial. Lancet. 2017;389(10083):2031–2040. doi:10.1016/S0140-6736(17)30070-3
53. Ohyama B, Nishifuji K, Chan PT, et al. Epitope spreading is rarely found in pemphigus vulgaris by large-scale longitudinal study using desmoglein 2-based swapped molecules. J Invest Dermatol. 2012;132(4):1158–1168. doi:10.1038/jid.2011.448
54. Hammers CM, Chen J, Lin C, et al. Persistence of anti-desmoglein 3 IgG(+) B-cell clones in pemphigus patients over years. J Invest Dermatol. 2015;135(3):742–749. doi:10.1038/jid.2014.291
55. Alexander T, Sarfert R, Klotsche J, et al. The proteasome inhibitior bortezomib depletes plasma cells and ameliorates clinical manifestations of refractory systemic lupus erythematosus. Ann Rheum Dis. 2015;74(7):1474–1478. doi:10.1136/annrheumdis-2014-206016
56. Hiepe F, Radbruch A. Plasma cells as an innovative target in autoimmune disease with renal manifestations. Nat Rev Nephrol. 2016;12(4):232–240. doi:10.1038/nrneph.2016.20
57. Vinay K, Cazzaniga S, Amber KT, Feldmeyer L, Naldi L, Borradori L. Rituximab as first-line adjuvant therapy for pemphigus: retrospective analysis of long-term outcomes at a single center. J Am Acad Dermatol. 2018;78(4):806–808. doi:10.1016/j.jaad.2017.11.024
58. Yancey KB. Commentary regarding clinical and immunological outcomes of high- and low-dose rituximab treatments in patients with pemphigus: a randomized, comparative, observer-blinded study. Dermatol Ther. 2015;28(3):174–175. doi:10.1111/dth.12198
59. Keeley JM, Bevans SL, Jaleel T, Sami N. Rituximab and low dose oral immune modulating treatment to maintain a sustained response in severe pemphigus patients. J Dermatolog Treat. 2019;30(4):340–345. doi:10.1080/09546634.2018.1510173
60. Alaeen H, Toosi R, Mahmoudi H, et al. Short-term clinical and serological follow-up with conventional and conformational anti-desmoglein antibodies in treatment-naïve and previously treated patients with pemphigus vulgaris after receiving rituximab. Int J Womens Dermatol. 2019;5(5):372–377. doi:10.1016/j.ijwd.2019.05.008
61. Balighi K, Daneshpazhooh M, Mahmoudi H, et al. Comparing early and late treatments with rituximab in pemphigus vulgaris: which one is better? Arch Dermatol Res. 2019;311(1):63–69. doi:10.1007/s00403-018-1881-1
62. Colliou N, Picard D, Caillot F, et al. Long-term remissions of severe pemphigus after rituximab therapy are associated with prolonged failure of desmoglein B cell response. Sci Transl Med. 2013;5(175):175ra30. doi:10.1126/scitranslmed.3005166
63. Hebert V, Joly P. Rituximab in pemphigus. Immunotherapy. 2018;10(1):27–37. doi:10.2217/imt-2017-0104
64. Murrell DF, Peña S, Joly P, et al. Diagnosis and management of pemphigus: recommendations of an international panel of experts. J Am Acad Dermatol. 2020;82(3):575–585.e1. doi:10.1016/j.jaad.2018.02.021
65. Aryanian Z, Balighi K, Daneshpazhooh M, et al. Rituximab exhibits a better safety profile when used as a first line of treatment for pemphigus vulgaris: a retrospective study. Int Immunopharmacol. 2021;96:107755. doi:10.1016/j.intimp.2021.107755
66. Nosrati A, Mimouni T, Hodak E, et al. Early rituximab treatment is associated with increased and sustained remission in pemphigus patients: a retrospective cohort of 99 patients. Dermatol Ther. 2022;35(5):e15397. doi:10.1111/dth.15397
67. Thng ZX, De Smet MD, Lee CS, et al. COVID-19 and immunosuppression: a review of current clinical experiences and implications for ophthalmology patients taking immunosuppressive drugs. Br J Ophthalmol. 2021;105(3):306–310. doi:10.1136/bjophthalmol-2020-316586
68. Cheng GS, Evans SE. The paradox of immunosuppressants and COVID-19. Eur Respir J. 2022;59(4):2102828. doi:10.1183/13993003.02828-2021
69. Andersen KM, Bates BA, Rashidi ES, et al. Long-term use of immunosuppressive medicines and in-hospital COVID-19 outcomes: a retrospective cohort study using data from the National COVID cohort collaborative. Lancet Rheumatol. 2022;4(1):e33–e41. doi:10.1016/S2665-9913(21)00325-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
