Back to Journals » Open Access Emergency Medicine » Volume 15
Risks of Early Mortality and Associated Factors at Adult Emergency Department of Jimma University Medical Center
Authors Abebe F , Habtamu A , Workina A
Received 13 June 2023
Accepted for publication 30 August 2023
Published 7 September 2023 Volume 2023:15 Pages 293—302
DOI https://doi.org/10.2147/OAEM.S420660
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Fikadu Abebe,1 Asaminew Habtamu,2 Abdata Workina2
1Midwifery School, Jimma University, Jimma, Ethiopia; 2Nursing School, Jimma University, Jimma, Ethiopia
Correspondence: Fikadu Abebe, Midwifery School, Jimma University, P.O. Box-378, Jimma, Oromia Region, Ethiopia, Tel +251 917551121, Email [email protected]
Introduction: Mortality in the emergency department is still high in developing countries with resources scarce. Most of emergency department mortality occurred within the first three days; the majority of these deaths are avoidable with proper intervention. Therefore, the purpose of this study was to assess the mortality risks and therapeutic benefits of early and late death.
Methods: Case-control study approach with 87 cases and 174 controls (case to control ratio of 1:2) was used on 261 study participants. Data were extracted from the patient charts using a pretested extraction tool. Then, checked data were entered into Epi-data manager 4.6 versions and analyzed using SPSS 25 versions. Binary logistic regression was used to construct bivariate and multivariable analyses following the descriptive analysis. Finally, a predictor variable in the multivariate logistic regression was deemed to have a significant association if its P-value was less than 0.05 at a 95% confidence level.
Results: Patients who were triaged into the red zone had a 2.3-fold greater risk of dying early than those who were placed in another triage category [(AOR=2.3; 95% CI: 1.10, 5.55) P=0.001]. Besides, having cardiovascular disease (AOR=4.79; 95% CI: 1.73, 13.27), age ≥ 65 years [(AOR=3.2; 95% CI: 1.74, 7.23) P=0.003)], having rural residency (AOR=6.57; 95% CI: 1.39, 31.13), and having been diagnosed with respiratory failure [(AOR=3.2; 95% CI: 1.04, 7.69), P=0.013)] were associated with early mortality.
Conclusion: The common causes of early mortality were respiratory failure, cardiovascular disease, and road traffic accident. Being aged, having rural residence, being triaged into red zone, and diagnosed for respiratory failure and cardiac failure increase early mortality compared with late death.
Keywords: early death, resuscitation, late mortality, comorbidity
Graphical Abstract:
Introduction
The emergency department provides services for patients with conditions that are life-threatening or potentially life-threatening over 24 hours.1 During these service provisions death or improvement is an outcome, and the death can be early (within the first 72 hours of emergency department presentation) or late (after 72 hours of patient’s emergency department presentation).2,3
Causes of mortality at ED are considered to be multifactorial, which embraces the burden of trauma, medical diseases, limited emergency healthcare services, and constraints of medical services with trained health personnel.4,5 Even though geographical variation is a determinant factor, the majority of this mortality occurred due to cardiac disease, RTA, and malignancy, covering 15–60% of early mortality.6–8 Clinical treatments similar to those that are standard at emergency trauma center practices have already been demonstrated to lower mortality in high- and middle-income nations, but emergency departments of low-income countries have not been thoroughly studied.7,9
The impact of emergency department death on the individual, society, and the overall health system is significant. It is quickly rising to the top of the list of fatalities in hospitals. It accounts for 15–16% of all hospital deaths worldwide. In sub-Saharan Africa’s low- and middle-income countries (LMICS), particularly in the Central East and Western regions, the value is significantly higher at 5.1% than in high-income nations.10,11
In the Ethiopian hospitals’ emergency departments, mortality from traumatic injuries and medical diseases was mostly uncharacterized, but the causes were thought to be multifactorial, covering a substantial burden of trauma, diseases, and lack of access to quality healthcare services, as well as limited access to high-quality resources, including skilled medical personnel.12
Even though it is believed that increasing the accessibility of emergency care services will have better patient outcome, there is insufficient scientific research to support this assertion.
Until now, only few cross-sectional retrospective chart review studies have been carried out in the resource-limited African regions on emergency medical care services and factors which affect late or early emergency department death.13 Therefore, the purpose of this study was to assess the mortality risks and therapeutic benefits of early and late death.
Patients and Methods
Study Design and Setting
A case-control study was employed to review the charts of patients who died at the adult emergency department of Jimma University Medical Centre from January 11, 2020, to November 29, 2022. Jimma University Medical Centre is the largest referral hospital found in the south western part of Ethiopia; it delivers healthcare for more than 20 million clients and patients. Around 17,000 inpatients, 200,000 outpatients, and 12,000 emergency cases are served at the institution per year. Moreover, the JUMC conducts healthcare research and is the only teaching hospital found in the Southwest of Ethiopia.14 The adult emergency department of JUMC has 66 beds and provides diagnostic testing and treatment for patients requiring emergency care.15
Study Population
Charts of selected patients who died at the adult ED of Jimma University Medical Centre, from January 1, 2020, to 2022 were reviewed.
Eligibility Criteria
Patients who died at the adult emergency department were included, while those who were dead on arrival were excluded from the study.
Operational Definitions
Early mortality: The death of the patient during the service provision or improvement is an outcome, and the death can be early (within the first 72 hours of emergency department presentation).
Late mortality: The death of the patient occurred after 72 hours of the patient’s emergency department presentation.
Sample Size Determination and Sampling Procedure
Epi-info version 7.2 was used to determine the sample by deeming HIV as a determinant variable from literature.2 Confidence level was 95%, power of study 80 at 95% confidence level, odds ratio of 2.32, and proportion of diabetes mellitus among controls was 16.87%. A total of 261 patients were included into study, 174 controls and 87 cases (1:2 cases to controls). Controls were selected by systematic random sampling following purposive selection of cases.
Data Collection Procedure and Quality Control
A pilot-tested extraction checklist tool was developed from previous studies,1,16–19 containing sociodemographic characteristics, traumatic and medical causes of ED visit, immediate cause of death, comorbidities, and related variables. The calculated Cronbach’s alpha from the pilot test was 0.86. Data were collected by five BSc nurses and two senior BSc nurses who were supervised after training was given to them on the data collection tool.
Data Processing and Analysis
Following the data collection, data were rechecked for completeness and were entered into Epidata manager version 4.6. Then a cleaned data set was transferred to SPSS versions 25 for analysis. Frequency and percentages were calculated for categorical variables. Bivariate logistic regression was performed for dependent variables (early mortality and late mortality) to identify the association between predictor variables. In the bivariate logistic regression, predictor variables having a P-value less than 0.25 at 95% confidence level were transferred into multivariate logistic regression to compute adjusted odds ratio. The model fitness was checked by Hosmer–Lemeshow goodness of model fitness test. Predictors having P-value <0.05 in the multivariate logistic regression were deemed significant associations at 95% CI.
Ethical Considerations
The ethical approval letter was obtained from Jimma University Institutional Review Board, and a support letter was given to the CEO of the Jimma University Medical Centre to conduct the study. Then, objectives of the study were explained to the staff of the record office. The patients’ names were not recorded in the data collection checklist. Confidentiality of all the reviewed charts was maintained. The patient-informed consent was renounced due to the anonymized data. This study was conducted according to Declaration of Helsinki.
Results
Socio-Demographic Characteristics of Study Participants
A total of 261 study participants (87 cases and 174 controls) were included in the study, of which 41.4% were aged between 25–54 years, and the mean±standard deviation age of the patients was 47.6±14.6 and 42.5±12.3 for controls and cases, respectively. Concerning the sex of the study participants, about two-thirds (65.2%) of them were males, with male to female ratio of 1.8:1. With regard to residence area, 66.7% of patients came from rural areas, of those 28.2% died in the first 72 hours after admission of ED (Table 1).
 |
Table 1 Socio-Demographic Characteristics Between Early and Late Mortality Among Patients Visiting the Adult Emergency Department of Jimma Medical Centre, Ethiopia, 2022 (n=261) |
Clinical Characteristics of the Study Participants
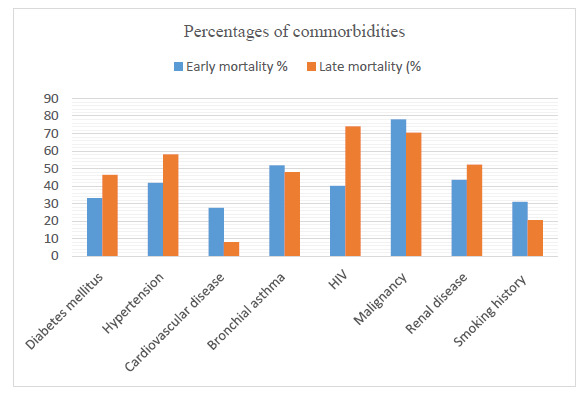
Concerning preexisting medical illnesses, 76 (29.1%) of the cases and 107 (40.1%) of the controls had comorbidities. The majority, 66 (44%) and 84 (56%), of the cases and controls, respectively, had at least two comorbidities. The most common comorbidity both in cases and in the control group was malignancy, which accounts for 68 (78.2%) and 123 (70.8%), respectively. The percentage of early mortality was higher among patients with comorbidity than among those without comorbidities. Most of the patients categorized red zone (resuscitation area) had higher late mortality, 42 (24.2%) versus 72 (82.8%) (Table 2).
 |
Table 2 Clinical Characteristics Between Early Mortality and Late Mortality Among Patients Who Died at Jimma Medical Centre, 2022 (n=261) |
Immediate Causes of Mortality Among Cases and Controls
Regarding the immediate cause of early mortality, most cases, 78 (89.6%), and 77 (44.3%) controls had respiratory failure. Fifty-four (31%) controls and 32 (36.8%) cases had cardiac failure, and 40 (56.2%) controls and 32 (44.4%) cases had cardiac and respiratory failure. More than half of the cases 55 (29.1%) and 134 (70.9%) controls had multi-organ failure (Table 3).
 |
Table 3 Causes of Early and Late Mortality Among ED Patients of Jimma Medical Center, Ethiopia 2022 |
This study shows that road traffic accident (RTA) was a frequent traumatic cause of early mortality in adult emergency departments. Of the total participants, 54 (31%) cases and 31 (43.5%) controls experienced RTA, followed by assault injuries, fall injuries, and gunshot wounds in proportions of 22 (25.8%), 21 (75%), and 13 (7.4%), respectively. Regarding the site of the injury, head injuries accounted for 134 (77%) of controls and 55 (63.2%) of cases, chest injuries for 34 (19.5%) of controls and 23 (26.4%) of cases, and spinal cord injuries for 13 (7.3%) of controls and 14 (16.1%) of cases (Table 3).
Factors Associated with Adult Emergency Early Mortality
First, the bivariate logistic regression was performed for dependent variables (early mortality and late mortality) to identify the association between predictor variables. In the bivariate logistic regression, predictor variables having a P-value less than 0.25 at 95% confidence level were transferred into multivariate logistic regression to compute adjusted odds ratio. The model fitness was checked by Hosmer–Lemeshow goodness of model fitness test. In the multivariate analysis, triage score, age, head injury, respiratory failure, cardiovascular disease, and residence revealed significant association.
Those patients triaged into the red zone were 2.3 times more likely to die early than those who were assigned to another triage category [(AOR=2.3; 95% CI: 1.10, 5.55) P=0.001)]. Aged patients (≥65 years of age) were 3.2 times more likely to die early than their younger counterparts [(AOR=3.2; 95% CI: 1.74, 7.23) P=0.003)] (Table 4).
 |
Table 4 Bivariate and Multivariate Regression Between Early Mortality and Late Mortality Among ED Patients of Jimma Medical Center, Ethiopia 2022 |
Additionally, patients having CVD were 4.79 times more likely to die within the first three days of adult emergency admission compared to those who had no cardiovascular disease (AOR=4.79; 95% CI: 1.73, 13.27). Likewise, patients who came from rural areas had a 6.57 times augmented probability of early mortality compared to those from urban areas (AOR=6.57; 95% CI: 1.39, 31.13), and the odds of early mortality among patients who had respiratory failure were 3.2 times higher compared to their counterparts [(AOR=3.2; 95% CI: 1.04, 7.69) P=0.013)]. Moreover, the other variable that showed a significant association with early mortality was those who had mild or moderate brain injury; they were 78% less likely to die within the first three days than those who had severe brain injury (Table 4).
Discussion
During emergency department care, patients can die early (within the first 72 hours of ED presentation) or late. Even though there are limited studies in the literature carried out in low-income countries, the causes of such death can be multifactorial which includes presence of comorbidity, quality of healthcare services, injury, and medical illness.2,20 Thus, this study aimed to identify causes of early mortality and related factors among case and control groups.
According to the study results, regarding preexisting medical illnesses, 76 (29.1%) of the cases and 107 (40.1%) of controls had comorbidities. The majority of them had at least two comorbidities, 66 (44%) of cases and 84 (56%) controls. Out of these comorbidities, diabetes mellitus, hypertension, and CVD were the most common among both cases and controls. This finding was consistent with a case control study conducted in Tehran that revealed that a majority of patients had more than one comorbidity, and among these comorbidities cardiovascular diseases, DM, and cerebrovascular accidents were the most common causes of early mortality.20 It was also consistent with a study conducted at Tikur Anbessa Specialized Hospital which elucidated that more than half of the primary causes of death involved more than two co-morbidities as a secondary cause of mortality, mainly including hypertension, diabetes, and cardiovascular disease.9 However, our study finding was in contrast to a study conducted in Nigeria which showed that cardiovascular disease was a major cause of early mortality.21 This discrepancy might have occurred due to cardiovascular disease being a broad concept which had subdivisions with different severity and fatality (arrhythmia can cause early death while heart failure may not).
Regarding the traumatic cause of early mortality, this study reported that RTA is a frequent traumatic cause of early mortality in adult emergency departments, which accounts for 54 (31%) cases and 31 (43.5%) controls who experienced RTA. This study is consistent with the findings from India that indicated that most of the traumatic causes of adult ED admissions were RTA (36.9).22 Furthermore, this study finding was consistent with a study conducted at Buganda Medical Centre in Northwestern Tanzania which showed that road traffic accident contributes 58.8% of early mortality among patients who visited the emergency department.23
Those patients triaged into red zone were 2.3 times more likely to die early than those who were assigned to another triage category [(AOR=2.3; 95% CI: 1.10, 5.55) P=0.001)]. Older age and those treated in clinical specialties had higher rates of hospitalization and death. This finding was in line with a study done on triage at the emergency department which showed that patients in the high-priority group or red categories of triage level were 10.6 times more likely to have early mortality than other triage categories in the emergency department (P<0.0001).17 But a surprising study done on adult emergency department mortality at Tikur Anbessa Specialized Hospital revealed that triage category red zone was significantly associated with decreased early emergency department mortality, AOR 0.23; 95% CI: 0.1–0.55.2 The possible cause of this difference could be due to differences in the early intervention on patients who have life-threatening conditions. Thus, this leads us to conclude that some cases under the red triage category were easily reversible and treatable conditions, and/or this group of clients admitted to ED Tikur Anbessa Specialized Hospital had got immediate intervention as required. Furthermore, in the case of our study, it indicated that even though those patients triaged under the red triage category most probably have poor outcome, the quality of services provided for the patient and the resource availability affect the patient to benefit from resuscitation room.
Aged patients (≥65 years of age) were 3.2 times more likely to die early compared to their younger counterparts [(AOR=3.2; 95% CI: 1.74, 7.23) P=0.003)]. It is in line with a study finding on the analysis of early mortality in the emergency department, which stated that early mortality at the emergency department is far higher among aged patients than among their counterparts.1 It is consistent with a study done in Tehran on the cause of emergency department mortality; this showed that patients aged over 60 years were 3.8 more likely to die early in the emergency department compared to those in other age categories (AOR=3.8; 95% CI: 1.8–7.8; P=0.01).20 Furthermore, it is a natural fact that aged people have compromised immune systems, thus a person with a compromised immune system cannot handle additional diseases and/or trauma. Thus, they are highly likely to die early as compared to patients in other age categories.
Patients having CVD were 4.79 times more likely to die within the first 72 hours of adult emergency admission compared to those who had no CVD (AOR=4.79; 95% CI: 1.73, 13.27). This finding was consistent with a study done at a university hospital in Pleven which elucidated that patients having CVD were 2.3 times (AOR=2.3; 95% CI: 1.73, 13.27) more likely to die within the first 72 hours of emergency department admission compared to those who had no CVD.6 Besides, It is also consistent with a study done in Tehran on the cause of emergency department mortality that reported that presentation with CVD complaints increase the ED early mortality by 7.3 times compared with those who had no CVD (OR=7.3; 95% CI: 3.5–16.1; P<0.001).20
Additionally, those patients who had mild or moderate brain injury were 78% less likely to die within the first three days than those who had a severe brain injury. This study finding is directly in line with studies done in Ethiopia and Kenya on the pattern and predictors of early mortality at adult emergency departments that showed or reported that emergency department early mortality is less likely among those who have no severe brain injury by 73% and 83%, respectively.2,18 It is also consistent with a study conducted in Addis Ababa, which revealed that severe head injury is the most common cause of early death among ED patients.9 Additionally, this study's finding was consistent with a study conducted in Tehran which showed that patients with severe brain injury were 4.6 times (AOR=4.6; 95% CI: 2.0–13.2; P<0.001) more likely to die early in the emergency department compared to their counterparts.20
Strengths and Limitations of the Study
This study attempted to generalize causes of early mortality compared with late mortality by a case control study design that identified which patients had benefited from emergency department care even though quality of care matters to the survival of the patients. As the study site was the largest referral hospital in the south west part of the country, this study was a single-center study.
Conclusions
Early mortality at the emergency department was significantly revealed among patients having CVD, comorbidity, and road traffic accident. Respiratory and cardiac failures were the most common cause of early death among patients that visited the emergency department. Being aged, having a severe head injury, having CVD, having respiratory failure, and rural residence were associated with increased early mortality at an emergency department. In addition, the quality of service in the resuscitation room should be improved, since most deaths occurred among those triaged under the red triage category.
Data Sharing Statement
Data will be available upon request from the corresponding author.
Acknowledgments
We are impressively thankful to Jimma University for providing us with financial support to conduct this work.
Author Contributions
All authors equally contributed to this work beginning from the conception, study design, execution, acquisition of data, analysis, and interpretation. Authors of this work took part in the drafting, revising, and/or critically reviewing of the article and finally agreed on the journal to which the article was submitted. All authors also reviewed and agreed on all versions of the article before submission, during revision, and agreed to be accountable for all aspects of the work.
Funding
This study was funded by Jimma University, Ethiopia and the funder has no interference with the conduction, analysis, and publication process of this manuscript.
Disclosure
The authors declare no competing interest in this research work.
References
1. Stefanovski PH, Vladimir Radkov R, Lyubomir Ilkov T, et al. Analysis of mortality in the emergency department at a university hospital in Pleven. J Int Med Res. 2017;45(5):1553–1561. doi:10.1177/0300060517707901
2. Yosha HD, Tadele A, Teklu S, Melese KG. A two-year review of adult emergency department mortality at Tikur Anbesa specialized tertiary hospital, Addis Ababa, Ethiopia. BMC Emerg Med. 2021;21(1):1–9. doi:10.1186/s12873-021-00429-z
3. Reynolds TA, Mfinanga JA, Sawe HR, Runyon MS, Mwafongo V. Emergency care capacity in Africa: a clinical and educational initiative in Tanzania. J Public Health Policy. 2012;33(S1):S126–S137. doi:10.1057/jphp.2012.41
4. Razzak JA, Kellermann AL. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–905.
5. Søvsø MB, Hermansen SB, Færk E, et al. Diagnosis and mortality of emergency department patients in the North Denmark region. BMC Health Serv Res. 2018;18(1):1–9. doi:10.1186/s12913-018-3361-x
6. Hsia R, Razzak J, Tsai AC, Hirshon JM. Placing emergency care on the global agenda. Ann Emerg Med. 2010;56(2):142–149. doi:10.1016/j.annemergmed.2010.01.013
7. Zhao Z, Guo F. Introduction [to Transition and Challenge: China’s Population at the Beginning of the 21st Century]. In: Transition and Challenge: China’s Population at the Beginning of the 21st Century. Oxford University Press; 2007.
8. Alghnam S, Alkelya M, Alfraidy M, Al-bedah K, Albabtain IT, Alshenqeety O. Outcomes of road traffic injuries before and after the implementation of a camera ticketing system: a retrospective study from a large trauma center in Saudi Arabia. Ann Saudi Med. 2017;37(1):1–9. doi:10.5144/0256-4947.2017.1
9. Hunchak C, Teklu S, Meshkat N, Meaney C, Puchalski Ritchie L. Patterns and predictors of early mortality among emergency department patients in Addis Ababa, Ethiopia. BMC Res Notes. 2015;8(1):1–9. doi:10.1186/s13104-015-1592-z
10. Obermeyer Z, Abujaber S, Makar M, et al. Emergency care in 59 low-and middle-income countries: a systematic review. Bull World Health Organ. 2015;93(8):577–586. doi:10.2471/BLT.14.148338
11. United Nations DoE, Social Affairs PD. Changing levels and trends in mortality: the role of patterns of death by cause (United Nations publication, ST/ESA/SER. A/318); 2012.
12. Hirshon JM, Risko N, Calvello EJ, et al. Health systems and services: the role of acute care. Bull World Health Organ. 2013;91(5):386–388. doi:10.2471/BLT.12.112664
13. Mowery NT, Dougherty SD, Hildreth AN, et al. Emergency department length of stay is an independent predictor of hospital mortality in trauma activation patients. J Trauma Acute Care Surg. 2011;70(6):1317–1325. doi:10.1097/TA.0b013e3182175199
14. Workina A, Habtamu A, Zewdie W. Reasons for emergency department visit, outcomes, and associated factors of oncologic patients at emergency department of Jimma University Medical Centre. Open Access Emerg Medi. 2022;14:581–590. doi:10.2147/OAEM.S381816
15. Deresse E, Komicha MA, Lema T, Abdulkadir S, Roba KT. Road traffic accident and management outcome among in Adama Hospital Medical College, Central Ethiopia. Pan Afr Med J. 2021;38:190. doi:10.11604/pamj.2021.38.190.11650
16. Opiro K, Wallis L, Ogwang M. Assessment of hospital-based adult triage at emergency receiving areas in hospitals in Northern Uganda. Afr Health Sci. 2017;17(2):481–490. doi:10.4314/ahs.v17i2.23
17. Becker JB, Lopes MCBT, Pinto MF, Campanharo CRV, Barbosa DA, Batista REA. Triage at the Emergency Department: association between triage levels and patient outcome. Revista da Escola de Enfermagem da USP. 2015;49(5):0783–0789. doi:10.1590/S0080-623420150000500011
18. Chalya PL, Mabula JB, Dass RM. 25. Injury characteristics and outcome of road traffic crash victims at Bugando Medical Centre in Northwestern Tanzania. J Trauma Manag Outcomes. 2012;6(1). doi:10.1186/1752-2897-6-1
19. Lugo LH, García HI, Cano BC, Arango JC, Alcaraz OL. Multicentric study of epidemiological and clinical characteristics of persons injured in motor vehicle accidents in Medellín, Colombia, 2009–2010. Colomb Med. 2013;44(2):100–107. doi:10.25100/cm.v44i2.1106
20. Alimohammadi H, Bidarizerehpoosh F, Mirmohammadi F, et al. Cause of emergency department mortality; a case-control study. Emergency. 2014;2(1):30.
21. Mould-Millman N-K, Dixon JM, Burkholder T, et al. Validity and reliability of the South African Triage Scale in prehospital providers. BMC Emerg Med. 2021;21(1):1–9. doi:10.1186/s12873-021-00406-6
22. Negussie A, Getie A, Manaye E, Tekle T. Prevalence and outcome of injury in patients visiting the emergency Department of Yirgalem General Hospital, Southern Ethiopia. BMC Emerg Med. 2018;18(1):14. doi:10.1186/s12873-018-0165-6
23. Caldwell JC, Jain S. Health Transition Review. Natl Centre Epidemiol Populat Health. 1997;7:1–1997.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
