Back to Journals » Cancer Management and Research » Volume 12
Risk Factors That Influence Surgical Decision-Making for Patients with Low-Risk Differentiated Thyroid Cancer with Tumor Diameters of 1–4 cm
Authors Wang X, Zhang C, Srivastava A, Yu W, Liu C, Wei D , Li Y, Yang J
Received 25 June 2020
Accepted for publication 3 November 2020
Published 2 December 2020 Volume 2020:12 Pages 12423—12428
DOI https://doi.org/10.2147/CMAR.S268716
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Sanjeev K. Srivastava
Xiangming Wang,1,* Chao Zhang,1,* Akanksha Srivastava,2 Wenbin Yu,3,* Chuan Liu,4 Dongmin Wei,5 Yuncheng Li,6 Jianming Yang1
1Department of Otolaryngology Head and Neck Surgery, The Second Hospital of Anhui Medical University, Hefei, People’s Republic of China; 2Department of Head and Neck Surgery, University of Texas MD Anderson Cancer Center, Houston, TX, USA; 3Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Head and Neck Surgery, Peking University Cancer Hospital and Institute, Beijing, People’s Republic of China; 4Department of Otorhinolaryngology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, People’s Republic of China; 5Department of Otorhinolaryngology, Qilu Hospital of Shandong University, Shandong, People’s Republic of China; 6Department of Otorhinolaryngology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianming Yang
Department of Otolaryngology Head and Neck Surgery, The Second Hospital of Anhui Medical University, Hefei 230601, People’s Republic of China
Tel +86 551 63869515
Email [email protected]
Yuncheng Li
Department of Otorhinolaryngology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, People’s Republic of China
Email [email protected]
Background: There are several controversies between thyroid lobectomy and total thyroidectomy for surgical management of low-risk differentiated thyroid cancer (DTC) with a tumor diameter of 1– 4 cm.
Patients and Methods: In this study, we explore the factors related to selection of type of surgical procedure for 103 low-risk DTC patients with a tumor diameter of 1– 4 cm.
Results: Among 103 low-risk DTC patients with tumor diameters of 1– 4 cm, 43 patients underwent total thyroidectomy and 60 patients underwent thyroid lobectomy based on postoperative pathology. A ROC curve showed that the optimal diagnostic threshold for selecting surgical modality was a tumor diameter of 2.15 cm. For these low-risk DTC patients, the sensitivity and specificity for predicting thyroid lobectomy when tumor diameter < 2.15 cm while total thyroidectomy when tumor diameter ≥ 2.15 cm are 46.5% and 78.3%, respectively. There were significant differences between the selection of type of surgical procedure in patient groups with 1) tumors with multiple foci group vs a single focus (P< 0.05), and 2) tumor diameter of ≥ 2.15 cm vs < 2.15 cm (P< 0.05). There was no significant difference between gender and age groups (P> 0.05). Multivariate analysis confirmed that tumors with multiple foci and diameter ≥ 2.15 cm were the primary risk factors for implementation of total thyroidectomy (P< 0.05).
Conclusion: The diameter and multifocal nature of low-risk DTC tumors are the primary factors related to preferred surgical modality. This study revealed that thyroid lobectomy is more applicable to patients with tumor diameter < 2.15 cm and a single focus, whereas, total thyroidectomy was preferred in patients with tumor diameter ≥ 2.15 cm and/or multiple foci.
Keywords: differentiated thyroid cancer, cancer metastasis, operation type, factor analysis
Introduction
In recent years, the incidence of differentiated thyroid cancer (DTC) has increased rapidly and has become one of the most common malignant tumors.1 DTC mostly grows inert and has a good prognosis.2 Nevertheless, a small proportion of DTC patients have recurrence and cancer-related mortality, as shown in long-term follow-up studies.3 Surgery is the first choice for treatment of DTC. Current surgical guidelines by the American Thyroid Association recommend the optimal surgical modality for DTC tumors with a diameter ≤1 cm and tumor diameter >4 cm.4 However, there are no clear recommendations regarding the surgical management of low-risk DTC with tumor diameters of 1–4 cm, with many controversies reported in the literature between thyroid lobectomy and total thyroidectomy.5 Low-risk DTC refers to those tumors with no high-risk characteristics of thyroid cancer such as extrathyroid invasion, clinically visible local or distant metastasis, head and neck radiation history, and positive family history. It is recommended that the above two surgical modalities should be selected according to disease features and the patient’s choice for low-risk DTC.4 Total thyroidectomy is conducive to further radioactive iodine treatment and postoperative follow-up monitoring, which can reduce the risk of recurrence of cancer and secondary surgical procedures,6 whereas thyroid lobectomy can preserve the contralateral normal thyroid tissue function and reduce the risk of injury of recurrent laryngeal nerve and parathyroid gland.
The most common local metastasis of DTC is to cervical lymph nodes, and is reported to be between 20% and 50%,7,8 while the micrometastasis rate approaches 90%.9 A large number of studies have found that lymph node metastasis is an independent risk factor for recurrence and prognosis of DTC patients after primary surgical management,10,11 indicating tumor metastasis could be an important factor for selection of type of surgical procedure for low-risk DTC with tumor diameter of 1–4 cm. However, some lymph node metastasis cannot be found during preoperative examination. For instance, Zhao et al12 found that 61.9% thyroid cancer lymph node metastasis were undiagnosed in ultrasound examination. Subsequently, the diagnosis of lymph node metastasis prior to primary surgical management is not a criterion of choosing between thyroid lobectomy and total thyroidectomy. Some studies have shown that tumor diameter, gender, age, and the multifocal nature of the tumor are relevant factors for DTC lymph node metastasis.13,14 Therefore, we retrospectively analyzed clinical data and postoperative pathology of low-risk DTC with tumor diameter of 1–4 cm for patients treated at the Department of Otolaryngology Head and Neck Surgery of the Second Hospital of Anhui Medical University and to ascertain the selection criteria between the two surgical modalities, namely thyroid lobectomy and total thyroidectomy.
Patients and Methods
Study Patients
The clinical data and postoperative pathological data of 378 patients with malignant thyroid tumors who underwent surgical treatment from January 2014 to May 2020 in the department of Otolaryngology Head and Neck Surgery of the Second Hospital of Anhui Medical University were collected. Inclusion criteria for data analysis: 1) the primary surgical treatment of thyroid nodule was performed at the Second Hospital of Anhui Medical University, Hefei, China with availability of complete clinical and pathological data; and 2) a diagnosis of DTC was confirmed by postoperative pathology with the tumor diameter of 1–4 cm. Exclusion criteria: 1) the post-operative pathological diagnosis of patients with thyroid nodules after operation was not DTC or was unclear; 2) the patient was found to have any high-risk characteristics of thyroid cancer before surgery; and 3) tumor diameter was ≤1 cm or >4 cm.
According to current surgical guidelines by the American Thyroid Association, when cancer metastasis is found in DTC patients’ postoperative pathology, the total thyroidectomy is needed; while no cancer metastasis is found in DTC patients’ postoperative pathology, the thyroid lobectomy is recommended. Therefore, the review and analysis of postoperative pathology of DTC patients may provide the surgeons with new information to help select the appropriate surgical modality for these patients. All DTC patients included in the study were divided into six groups according to the tumor diameter confirmed by postoperative pathology, namely group A (1.0–1.5 cm), B (1.6–2.0 cm), C (2.1–2.5 cm), D (2.6–3.0 cm), E (3.1–3.5 cm), and F (3.6–4.0 cm). All DTC patients included in the study were divided into two groups according to age ≤45 years old and age >45 years old. Furthermore, DTC with ≥2 cancer foci within the thyroid gland were included in the multiple foci group, while DTC with one cancer focus were included in the single focus group. Informed consent was obtained from the study participants prior to study commencement. The study protocol was approved by the Second Hospital of Anhui Medical University Ethics Committee.
Statistical Analysis
For ROC curve analysis, the type of surgery according to the postoperative pathology was selected. The sensitivity, specificity, and optimal diagnostic threshold of surgery type according to tumor diameter were calculated. Univariate analyses using χ2 test were conducted to evaluate relationships between the type of surgical modality and tumor diameter, gender, age, single focus and multiple foci. All the factors used for univariate analysis were incorporated into binary logistic regression equations to determine the relevant factors for selection of the surgical modality in low-risk DTC with tumor diameter of 1–4 cm. SPSS 22.0 software was used for data management and analysis. Alpha level of 0.05 was chosen for statistical significance.
Results
Clinical and Pathological Data of Patients
A total of 103 low-risk DTC patients with tumor diameter of 1–4 cm were included in this study (Table 1) with a mean age of 43.79±14.18 years (range=19–77 years). Based on postoperative pathology, 40 patients (38.83%) had lymph node metastasis, four patients (3.88%) had extraglandular invasion of thyroid gland, one patient (0.97%) had lymphatic vessel invasion, and two patients (1.94%) had evidence of two or more types of thyroid cancer metastasis. Based on this postoperative pathology information, the total thyroidectomy should have been recommended for 43 patients with metastasis (41.75%), while thyroid lobectomy should have been recommended for 60 patients (58.25%) without metastasis.
 |
Table 1 Distribution of Clinical and Pathological Factors in 103 Low-Risk DTC Patients with Tumor Diameter of 1–4 cm |
As shown in Figure 1, with the increase of tumor diameter, the percentage of total thyroidectomy recommended in each group showed an overall upward trend, while the percentage of thyroid lobectomy recommended in each group showed an overall downward trend. The ROC curve analysis was applied to calculate the optimal diagnostic threshold (Figure 2). The area under ROC curve was 0.655 (95% CI=0.548–0.761). The tumor diameter value corresponding to the largest Youden index is the optimal diagnostic threshold for judging the operation type selection. As shown in Figure 2, the optimal diagnostic threshold for tumor diameter was 2.15 cm. For low-risk DTC with a tumor diameter of 1–4 cm, the sensitivity and specificity for predicting completion thyroid lobectomy when the tumor diameter was <2.15 cm while completion total thyroidectomy when the tumor diameter was ≥2.15 cm were 46.5% and 78.3%, respectively.
 |
Figure 1 Percentage of cases recommended for total thyroidectomy and thyroid lobectomy in each group by tumor diameter. |
 |
Figure 2 The ROC curve for selection of type of surgery in 103 low-risk DTC patients by tumor diameter. |
As shown in Table 2, the univariate analyses revealed that there was a significant difference between the types of surgical modality opted for based on the number of tumor foci, and tumor diameters of ≥2.15 cm vs <2.15 cm (P<0.05). There were no significant differences between the surgery type based on gender and age groups (P>0.05). Four factors, including tumor diameter, tumor multifocal nature, age, and gender were incorporated into the logistic regression equation. As shown in Table 3, the multivariable analysis showed that the tumor diameter and multifocal nature were important clinical factors, which affected the selection of surgical procedure for low-risk DTC patients with a tumor diameter of 1–4 cm (OR=3.251, 95% CI=1.293–8.174 for tumor multifocal feature and OR=3.443, 95% CI=1.386–8.554 for tumor diameter). Thus, thyroid lobectomy might be more applicable to patients with a tumor diameter <2.15 cm and a single focus, while total thyroidectomy might be preferred in patients with a tumor diameter ≥2.15 cm and/or multiple foci.
 |
Table 2 Univariate Analysis on Association Between Risk Factors and Selection of Operation Type in 103 Cases with Low-Risk DTC |
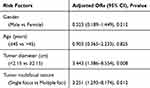 |
Table 3 Multivariate Analysis on Associations Between Risk Factors with Selection of Operation Type in 103 Cases with Low-Risk DTC |
Discussion
Differentiated thyroid cancer has an overall good treatment prognosis and long-term outcomes. However, guidelines on optimal surgical management are sparse, due to difficulties in carrying out prospective clinical research. Consequently, there are many disputes in the treatment scheme of DTC, especially between selection of a thyroid lobectomy vs total thyroidectomy in low-risk DTC tumors ranging in diameter between 1 and 4 cm. Patient and tumor characteristics that may predict the optimal surgical modality are largely unexplored in the literature. Our study results revealed that the metastatic rate of low-risk DTC with a tumor diameter of 1–4 cm was 41.75% (43/103), which is similar to the 44–49% reported in other literatures.15,16
Injury of recurrent laryngeal nerve (RLN) is one of serious complications of thyroid surgery, which may significantly affect the quality-of-life of the patients. Unilateral RLN injury may cause hoarseness or irritating cough in the patients. Bilateral RLN injury is a rare and more serious complication and may cause dyspnea and even endanger life.17,18 A previous study reported that unilateral RLN injury was observed in 55 (2.3%) patients and bilateral RLN injury in four (0.2%) patients among 2,365 patients after thyroid surgery.19 Moreover, with the significant increase in incidence of DTC in the past two decades, the number of thyroidectomy operations and the number of cases of RLN injury has increased significantly. Meanwhile, the injury of RLN was also the most common complication caused by surgical malpractice after thyroid surgery.20,21 However, the selection of appropriate and reasonable surgical modality for DTC patients may reduce the risk of secondary surgery, and injury of recurrent laryngeal nerve.
With the increase of tumor diameter, the probability of lymph node metastasis, extraglandular invasion, and other cancer metastasis of low-risk DTC with tumor diameter of 1–4 cm increased significantly (Figure 1). When the tumor diameter ≥2.15 cm, the metastatic rate of low-risk DTC can reach 60.61% (20/33). Univariate analysis and multivariate analysis results of relevant factors for the selection of surgical modality also showed that low-risk DTC with tumor diameter ≥2.15 cm has higher cancer metastasis risk than low-risk DTC with tumor diameter <2.15 cm, and total thyroidectomy is recommended (OR=3.443, P<0.05). Ito et al22 also found that DTC with a tumor diameter >2 cm has stronger invasive biological characteristics and is more likely to have local recurrence and distant metastasis than DTC with a tumor diameter ≤2 cm. Therefore, tumor diameter is an important related factor for the selection of optimal surgical treatment modality for low risk DTC ranging between 1–4 cm.
Clinically, the age of 45 years old is a remarkable cut-off point for risk stratification of the DTC patients.23 However, our results in this study showed that there was no statistical difference in metastasis of low-risk DTC between the two age groups ≤45 and >45 years (P=0.580). The possible reasons for non-significance in this study could be because: 1) the research objects are different. In this study, the DTC with a tumor diameter ≤1 cm, DTC with a tumor diameter >4 cm, and high-risk DTC with a tumor diameter of 1–4 cm were excluded, and such a criteria for patient recruitment could lead to a selection bias for metastasis between the two groups in this study; and 2) the small sample size could lead to low statistical power for statistical analysis. Thus, future larger studies are needed to validate our findings.
DTC is more common in females (the proportion of females in this study is 75.73%). However, some studies have found that the correlation between lymph node metastasis of thyroid cancer and gender is not significant.24 Univariate and multivariate analysis results in this study show that there is no statistical difference in cancer metastasis rate and type of surgical management between male and female groups (P>0.05).
The results of this study show that multiple foci are the relevant factors for cancer metastasis in low-risk DTC with a tumor diameter of 1–4 cm, and total thyroidectomy was the recommended surgical modality in such cases (OR=3.251, P<0.05). This is similar to previous research results.25 Presumably, the reason is that multiple cancer foci in the thyroid gland may indicate that the thyroid cancer has more active biological characteristics, stronger invasiveness, and may be more prone to cancer metastasis.
In conclusion, within the limitations of this study, the results revealed that the diameter and multifocal nature of the tumor are the primary factors related to the selection of surgery type between thyroid lobectomy and total thyroidectomy for low-risk DTC, ranging in diameter between 1 and 4 cm. For tumor diameter <2.15 cm or single focus, thyroid lobectomy was more applicable, whereas tumor diameter ≥2.15 cm or multiple foci were more likely subjected to total thyroidectomy.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of the Second Hospital of Anhui Medical University and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Acknowledgement
We thank Dr. Guojun Li for critical guidance, reading and revision of the manuscript.
Author Contributions
All authors contributed to data analysis, drafting, or revising of the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. WHO/IARC. World Cancer Report 2014. Lyon: IARC Press; 2014:738–750.
2. Gorshtein A, Benbassat C, Robenshtok E, Shimon I, Hirsch D. Response to treatment is highly predictable in cn0 patients with papillary thyroid carcinoma. World J Surg. 2016;40(9):2123–2130. doi:10.1007/s00268-016-3507-0
3. Grogan RH, Kaplan SP, Cao H, et al. A study of recurrence and death from papillary thyroid cancer with 27 years of median follow-up. Surgery. 2013;154(6):1436–1446. doi:10.1016/j.surg.2013.07.008
4. Haugen BR, Alexander EK, Bible KC, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the american thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. doi:10.1089/thy.2015.0020
5. McLeod DS, Sawka AM, Cooper DS. Controversies in primary treatment of low-risk papillary thyroid cancer. Lancet. 2013;381(9871):1046–1057. doi:10.1016/s0140-6736(12)62205-3
6. Macedo FIB, Mittal VK. Total thyroidectomy versus lobectomy as initial operation for small unilateral papillary thyroid carcinoma: a meta-analysis. Surg Oncol. 2015;24(2):117–122. doi:10.1016/j.suronc.2015.04.005
7. Shaha AR. Central lymph node metastasis in papillary thyroid carcinoma. World J Surg. 2018;42(3):630–631. doi:10.1007/s00268-017-4459-8
8. Feng JW, Yang XH, Wu BQ, Sun DL, Jiang Y, Qu Z. Predictive factors for central lymph node and lateral cervical lymph node metastases in papillary thyroid carcinoma. Clin Transl Oncol. 2019;21(11):1482–1491. doi:10.1007/s12094-019-02076-0
9. Qubain SW, Nakano S, Baba M, Takao S, Aikou T. Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery. 2002;131(3):249–256. doi:10.1067/msy.2002.120657
10. Mansour J, Sagiv D, Alon E, Talmi Y. Prognostic value of lymph node ratio in metastatic papillary thyroid carcinoma. J Laryngol Otol. 2018;132(1):8–13. doi:10.1017/S0022215117002250
11. Lee CW, Roh JL, Gong G, et al. Risk factors for recurrence of papillary thyroid carcinoma with clinically node-positive lateral neck. Ann Surg Oncol. 2015;22(1):117–124. doi:10.1245/s10434-014-3900-6
12. Zhao Z, Zhao Z, Ma J, Jing S. Clinical significance of ultrasonography in the diagnosis of central clearing of papillary thyroid carcinoma. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2015;29(6):538–541.
13. Suman P, Wang CH, Abadin SS, Moo-Young TA, Prinz RA, Winchester DJ. Risk factors for central lymph node metastasis in papillary thyroid carcinoma: a national cancer data base (NCDB) study. Surgery. 2016;159(1):31–39. doi:10.1016/j.surg.2015.08.032
14. Ji YB, Yoo HS, Song CM, Park CW, Lee CB, Tae K. Predictive factors and pattern of central lymph node metastasis in unilateral papillary thyroid carcinoma. Auris Nasus Larynx. 2016;43(1):79–83. doi:10.1016/j.anl.2015.09.005
15. Cheng SP, Chien MN, Wang TY, Lee JJ, Lee CC, Liu CL. Reconsideration of tumor size threshold for total thyroidectomy in differentiated thyroid cancer. Surgery. 2018;164(3):504–510. doi:10.1016/j.surg.2018.04.019
16. Ying DT, Zhang YY, Han Y. Analysis of the benefits and risks of 1 to 4 centimetre well-differentiated thyroid carcinoma with lobectomy. Int J Surg. 2017;44(2):115–117.
17. Caragacianu D, Kamani D, Randolph GW. Intraoperative monitoring: normative range associated with normal postoperative glottic function. Laryngoscope. 2013;123(12):3026–3031. doi:10.1002/lary.24195
18. Deniwar A, Kandil E, Randolph G. Electrophysiological neural monitoring of the laryngeal nerves in thyroid surgery: review of the current literature. Gland Surg. 2015;4(5):368–375. doi:10.3978/j.issn.2227-684X.2015.04.04
19. Calò PG, Medas F, Conzo G, et al. Intraoperative neuromonitoring in thyroid surgery: is the two-staged thyroidectomy justified? Int J Surg. 2017;41(Suppl 1):S13–S20. doi:10.1016/j.ijsu.2017.02.001
20. Dralle H, Lorenz K, Machens A. Verdicts on malpractice claims after thyroid surgery: emerging trends and future directions. Head Neck. 2012;34(11):1591–1596. doi:10.1002/hed.21970
21. Gambardella C, Polistena A, Sanguinetti A, et al. Unintentional recurrent laryngeal nerve injuries following thyroidectomy: is it the surgeon who pays the bill? Int J Surg. 2017;41(Suppl 1):S55–S59. doi:10.1016/j.ijsu.2017.01.112
22. Ito Y, Kudo T, Kihara M, et al. Prognosis of low-risk papillary thyroid carcinoma patients: its relationship with the size of primary tumors. Endocr J. 2012;59(2):119–125. doi:10.1507/endocrj.ej11-0288
23. Qu H, Sun GR, Liu Y, He QS. Clinical risk factors for central lymph node metastasis in papillary thyroid carcinoma: a systematic review and meta-analysis. Clin Endocrinol (Oxf). 2015;83(1):124–132. doi:10.1111/cen.12583
24. Liu N, Nie CL, Zhang JW. Risk factors of the central lymph node metastasis in papillary thyroid carcinoma. Chin J Endemiol. 2015;34(5):340–343.
25. Feng J, Gan X, Shen F, Cai W, Xu B. The role of two tumor foci for predicting central lymph node metastasis in papillary thyroid carcinoma: a meta-analysis. Int J Surg. 2018;52:166–170. doi:10.1016/j.ijsu.2018.02.029
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
