Back to Journals » Vascular Health and Risk Management » Volume 18
Risk Factors for Coronary Heart Disease Among Lebanese Women: A Case–Control Study
Authors Ghaddar F , Zeidan RK, Salameh P, Tatari S, Achkouty G, Maupas-Schwalm F
Received 18 November 2021
Accepted for publication 30 March 2022
Published 16 April 2022 Volume 2022:18 Pages 297—311
DOI https://doi.org/10.2147/VHRM.S350108
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Takashi Kajiya
Fatima Ghaddar,1 Rouba K Zeidan,2– 5 Pascale Salameh,4,6– 8 Souzan Tatari,9 Guy Achkouty,10 Françoise Maupas-Schwalm11
1Doctoral School of Biology Health and Biotechnologies, Toulouse University, Toulouse, France; 2Sharjah Institute of Medical Research, University of Sharjah, Sharjah, United Arab Emirates; 3Faculty of Public Health II, Lebanese University, Mount-Lebanon, Lebanon; 4INSPECT-LB, National Institute of Public Health, Clinical Epidemiology and Toxicology, Beirut, Lebanon; 5CERIPH, Center for Research in Public Health, Faculty of Public Health, Lebanese University, Mount-Lebanon, Lebanon; 6Department of Research, Faculty of Pharmacy, Lebanese University, Beirut, Lebanon; 7Department of Primary Care and Population Health, University of Nicosia Medical School, Nicosia, Cyprus; 8School of Medicine, Lebanese American University, Byblos, Lebanon; 9Cardiology department, Rafik Hariri University Hospital, Beirut, Lebanon; 10Cardiology Department, Mount Lebanon University Hospital, Mount-Lebanon, Lebanon; 11Faculty of Medicine, CHU Toulouse Rangueil, Toulouse, France
Correspondence: Fatima Ghaddar, Doctoral school of Biology Health and Biotechnologies, Toulouse University, Toulouse, France, Tel +32 470 53 71 52, Email [email protected]
Purpose: Women are increasingly concerned by coronary heart disease (CHD), with peculiarities of their own, particularly concerning risk factors. The aim of the study was to assess the risk factors for CHD in Lebanese women over forty.
Patients and Methods: A case–control study was carried out in 6 hospitals in Beirut and Mount-Lebanon, from December 2018 to December 2019 including 1500 patients (1200 controls and 300 cases). Women were stratified into pre- and post-menopausal groups. Personal and medical data were collected from hospital records and during an interview where validated questionnaires were used. Binary logistic regressions were performed to investigate potential predictors of CHD in the 2 groups.
Results: In post-menopausal women, dyslipidemia (adjusted odds ratio [aOR], 3.018; 95% confidence interval, 2.102– 4.332), hypertension (aOR: 2.449, [1.386– 4.327]), a family history of CHD (aOR: 2.724, [1.949– 3.808]), cigarette smoking (aOR: 2.317, [1.574– 3.410]) and common non-rheumatic joint pain (aOR: 1.457, [1.053– 2.016]) were strongly associated with CHD. Conversely, living in Mount Lebanon seemed protective, compared to Beirut (aOR: 0.589, [0.406– 0.854]), as well as having a moderate monthly income (aOR: 0.450, [0.220– 0.923]), adhering to a Mediterranean diet (aOR: 0.965, [0.936– 0.994]), and practicing physical activity [PA] (aOR: 0.396, [0.206– 0.759] and 0.725, [0.529– 0.992], respectively for high and moderate vs low PA). In pre-menopausal women, dyslipidemia (aOR: 6.938, [1.835– 26.224]), hypertension (aOR: 6.195, [1.318– 29.119]), family histories of dyslipidemia (aOR: 6.143, [1.560– 24.191]) and CHD (aOR: 4.739, [1.336– 16.805]) reached statistical significance.
Conclusion: The identification of factors associated with CHD in women, some of which are frequent and trivialized in post-menopause, underlines the need to put in place specific and dedicated CHD prevention strategies in women.
Keywords: coronary disease, risk factors, aging, pre-menopausal women, post-menopausal women
Introduction
According to recent world health organization (WHO) data, coronary heart disease (CHD) remains the leading cause of death worldwide, with increasing prevalence in Africa and Middle East countries,1 and ranked as the main cause of death in Lebanon.2 While premenopausal women have a lower cardiovascular risk than men, it is well recognized that their risk catches up to that of men as they age and change their hormonal status.3 Also, recent epidemiological studies show a more important decrease in CHD mortality rates in men compared to women.4
Although everyone shares most traditional risk factors (RFs), a significantly different gender weighting seems to exist. Some RFs might have a higher impact on women’s cardiovascular disease (CVD) risk. Women are also increasingly adopting smoking and alcohol consumption.5 Moreover, environmental stressors caused by urban living or urbanization (population density, economic activity, transportation, sanitation, long-term exposures to air pollution, noise, lack of surrounding greenery, building morphology, ….) cannot be denied as factors leading to cardiovascular health problems, especially among women.6,7 This relation was also demonstrated by previous work, indicating the effect of living in Beirut, the capital of Lebanon, on heart disease compared with outside of Beirut; where older participants and women were more likely to report cardiovascular risk factors (CVRFs) than younger participants and men.8,9 Furthermore, it has been reported that the medical management of women, due to various factors (failure to consider initial symptoms, delay in medical consultation, sometimes less pathognomonic symptomatology) could differ significantly from that of men, increasing the risk of medical problems.10 Thus, despite women living longer than men, many of those extra years are spent in poor health.11
Some studies have previously been interested in CVRFs in the general Lebanese population12,13 due to the considerable impact of the topic in public health and the need to improve knowledge of a medical problem which appears to be worsening.9 However, women are under-represented in heart disease research (about 20% of enrolled patients in most clinical studies),10 while CVD accounting for one third of all female deaths.14 This lack is not in accordance with the health, social and environmental evolution of society. The aim of our study is to carry out an analysis of the RFs for CHD in Lebanese women over 40, based on a case-control study. This would allow us to develop avenues of reflection to propose an improvement in the medical prevention of these women who are currently less concerned with cardiovascular risk programs.
Materials and Methods
Study Design and Study Population
A case-control study was carried out in Beirut and Mount-Lebanon, approved by the Institutional Review Board ethical committee of each participating hospital, in accordance with Lebanon’s ethical legislation, and the Declaration of Helsinki. Six hospitals were contacted to obtain their authorization to participate in the study (Central Military Hospital, Lebanese Hospital Geitaoui, Sacred Heart Hospital, Makassed General Hospital, Mount-Lebanon University Hospital, and Rafik Hariri University Hospital). Eligible patients were selected from hospital admission lists and their informed consent was obtained prior to enrollment.
Women aged over 40, hospitalized between December 2018 and December 2019, without previous heart disease (myocardial infarction [MI], CHD, valvular heart disease, cardiomyopathy, and myocarditis) could be included. The cases group was composed of women diagnosed with CHD (MI, or stable/unstable angina) for the first time, and control group consisted of women randomly selected from surgery and general medicine departments of the same hospitals with no personal history of CHD.
Cancer, mental disorder, human immunodeficiency virus, end-stage renal disease, chronic steroid treatment and pregnancy were exclusion criteria.
Data Collection
Data were obtained from medical records and questionnaires completed during a face-to-face interview after assessing participants’ capacity to respond using the Abbreviated Mental Test Score.15
The data collected, secondarily anonymized, were: socio-demographics (age, marital status, educational level, working status, monthly income and place of residence (Beirut, Mount-Lebanon, South Lebanon and Nabatieh, North Lebanon and Bekaa Valley)), lifestyle data (smoking, eating habits (using Lebanese Mediterranean Diet Score (LMDS)13), alcohol consumption and self-reported pollution exposure (closeness to generators, traffic, factories, …)16). Joint pain, rheumatic diseases, periodontitis, and post-menopausal status were self-declared. Medical and family histories were evaluated, in relation to the onset of premature CHD, presence of CVRFs and comorbidities. Several health-related scores such as medication adherence (Lebanese Medication Adherence Scale (LMAS),17 Beirut Distress Scale-22 (BDS-22),18 physical activity (PA, International Physical Activity Questionnaire (IPAQ)),19 and sedentary lifestyle were calculated.
Sample Size
Sample size was calculated using Epi info7, assuming a Type I error of 5%, a study power of 80%, and a confidence interval (CI) of 95%. We used the CHD prevalence (9% in over forty Lebanese women13) in our calculation. Thus, the minimum sample size necessary to show a double increase in CHD risk, in a ratio case/control of 1/4, was 1500 participants.
Individual RFs Definitions
Hypertensive women were either self-declared, taking anti-hypertensive drugs or with a hospitalized blood pressure measured over 140/90 mmHg. Women with diabetes were defined as taking hypoglycemic drugs, self-declared or those with biological evidence for diabetes (blood sugar: fasting ≥7 mmol/L or random ≥11.1 mmol/L or glycated hemoglobin ≥6.5%). Dyslipidemia was defined through self-reporting, lipid-lowering treatment, or by biological data when available (non-High-Density Lipoprotein Cholesterol (non-HDLc) ≥3.4 mmol/L; triglycerides ≥1.7 mmol/L; or Low-Density Lipoprotein Cholesterol (LDLc) ≥3 mmol/L).
A family history of premature CHD was defined as a first-degree relative who developed CHD before the age of 55 for men and 65 for women.
Body Mass Index (BMI) was calculated (overweight defined as BMI ≥25 kg/m2 and obese as BMI ≥30 kg/m2). Menopause was considered to be present when there was no history of menstruation for 12 consecutive months.
Environmental and Behavioral RFs Definitions
Income per family member was defined as the monthly household income of the family divided by the number of its members, and categorized into low, middle or high income according to the poverty line and the minimum wage adopted in Lebanon.20
Exposure to outdoor (living area, closeness to a road, traffic jam, an electricity generator, or factories and exposure to gases or toxic substances) and indoor (heating and cooking methods) air pollution16 was also assessed based on patients’ self-reported information.
The women’s residence was further analyzed in terms of CHD RFs, highlighting the impact of living in the Lebanese capital (Beirut) compared to outside Beirut.
Women who had smoked cigarettes and/or waterpipes in the previous 12 months were considered current smokers and those who had quit smoking more than a year earlier were considered former smokers. The cumulative doses of cigarettes and waterpipes were computed as the average number of daily packs or weekly waterpipes respectively, multiplied by the duration of smoking.21 Exposure to secondhand smoking (home or workplace) was defined by the self-declared average exposure period in daily hours from the previous week.22
The IPAQ long form assessed the level of PA in four domains: work, domestic, transport and leisure; PA intensity was evaluated by frequency (days/week) and duration (min/day) over the past 7 days.23 The total volume of PA was computed by weighting each type of activity by its estimated energy needs (metabolic equivalent (MET): 3.3 for walking, 4 for moderate PA and 8 for vigorous PA) generating a combined score in MET.minutes/week (low amount: <600, moderate: 600 to <3000 and high PA levels ≥3000 MET.min/week). We have also estimated sedentary periods, for weekdays and weekends.
Dietary habits were evaluated using LMDS, consisting of twenty major components, distributed into 10 beneficial and 10 harmful foods.13 Scores varied from 0 to 80 (maximal adherence to Mediterranean diet).
Psychological distress was measured using BDS-22,18 composed of 22 questions and reflecting 6 factors (depression, demotivation, psychosomatic, mood deterioration, intellectual inhibition and anxiety), with a Likert scale (0-never to 3-always). Possible scores range from 0 to 66 (maximum psychological distress).
Patient Medication Adherence was assessed by the LMAS composed of occupational, psychological, annoyance and economic factors.17 The sum of all items vary from 0 to 14 (maximum therapeutic adherence).
Statistical Analysis
Data were analyzed using SPSS, version 21. Descriptive statistics including percentages and means (± standard deviations) were used to describe patients’ characteristics. Bivariate analyses were performed using Student’s t-test to verify the association between CHD and continuous variables, or with the adjusted t-test. For categorical variables, Pearson-Chi2 and Fisher exact tests were used to compare percentages. Crude odds ratios (OR) and adjusted OR with their respective 95% CI were reported. The reliability of some scores was estimated by calculating Cronbach’s alpha (>0.7: acceptable). The candidate predictors for the multivariate analyses were identified by taking those which had a p-value <0.20 in the bivariate analysis. Two multivariate logistic regression models (using the “backward” method) were performed to control for confounding variables (particularly age) and determine independent predictors of CHD among pre- and post-menopausal women. A p-value <0.05 was considered significant. The final models were reached after ensuring the adequacy of data using Hosmer-Lemeshow test, and the absence of any multicollinearity between predictors using the correlation matrix.24
Results
Sample Description and Sociodemographic Patients’ Characteristics
From 2146 women initially screened, 646 (30.1%) were not included, leading to a study size of 1500 patients (1200 as controls (80%) and 300 as cases (20%)) (Figure 1).
 |
Figure 1 Flowchart of women included in the study. |
Women were divided into pre- and post-menopausal groups. Table 1 shows the baseline socio-demographic characteristics of the study sample. CHD patients were significantly older in both groups (46.44±4.27 vs 44.48±3.82 in pre-menopausal group, and 66.68±9.38 vs 65.39±10.73 in post-menopausal group, for cases and controls, respectively). Almost half (48.7%) of the non-coronary post-menopausal women lived in Mount-Lebanon, while 28% of cases lived in the capital Beirut.
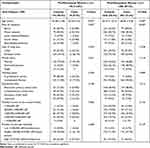 |
Table 1 Baseline Socio-Demographic Characteristics of Study Population |
Lifestyle and Individual RFs for CHD
As expected, usual RFs of CHD emerged in our study (Table 2). Regarding risky behaviors, current cigarette smoking was associated with CHD in pre-menopausal (OR: 4.878 [1.441–16.508]) and post-menopausal (OR: 1.917 [1.431–2.567]) women, where a clear positive dose-response relationship between pack-years and odds of CHD was also demonstrated. Moreover, the majority of individual RFs were significantly and markedly more common in CHD patients of both groups.
 |
Table 2 Differences in Lifestyle and Individual Risk Factors According to Studied Women Status |
We also found that common joint pain, was significantly associated with higher odds of CHD (OR: 2.985 [1.020–8.734] and 1.686 [1.270–2.237] for pre- and post-menopausal groups, respectively).
Environmental and Behavioral RFs for CHD
Our results (Table 3) showed that a toxic respiratory environment is associated with CHD in women with a significant result for passive smoking (OR: 4.541 [1.011–20.393] and 1.401 [1.075–1.828] for pre- and post-menopausal women, respectively), while declared exposure to pollution tended to be higher among cases, but did not reach statistical significance.
 |
Table 3 Difference in Various Environmental and Behavioral Risk Factors According to Studied Women Status |
Conversely, adherence to LMDS appeared to be responsible for a significant reduction of approximately 4% in odds of CHD in post-menopausal women for each one-unit increase in LMDS (OR: 0.962 [0.937–0.987]).
Psychological distress was found to be more frequent for coronary postmenopausal women, with a remarkable internal consistency (alpha’s Cronbach: 0.981) specifically in the depression (OR: 1.037 [1.005–1.069]), mood deterioration (OR: 1.066 [1.009–1.126]), intellectual inhibition (OR: 1.073 [1.010–1.140]) and anxiety domains (OR: 1.102 [1.019–1.192]).
Medication adherence, assessed by LMAS (with excellent internal consistency, alpha’s Cronbach=0.87), was significant only for the post-menopausal group among the 1257 studied women under medical treatment, revealing a reduction of about 6% in odds of CHD.
Concerning PA, more than half of coronary post-menopausal women reported exercising a little or not at all (54.3%), while PA seemed to be associated with a significant decrease in odds of CHD: moderate PA showed a 29.5% reduction in odds of CHD, and high PA a 61.8% decrease, compared to no or low PA (OR: 0.705 [0.535–0.929] or 0.382 [0.220–0.664] respectively). While, for pre-menopausal women, high PA alone was found to be significant in protecting against CHD (OR: 0.099 [0.012–0.843]).
Independent Predictors of CHD
Dyslipidemia (aOR: 6.938 [1.835–26.224], p=0.004), hypertension (aOR: 6.195 [1.318–29.119], p=0.021), family histories of dyslipidemia (aOR: 6.143 [1.560–24.191], p=0.009) and premature CHD (aOR: 4.739 [1.336–16.805], p=0.016) were the only RFs associated with CHD in pre-menopausal women.
Dyslipidemia (aOR: 3.018 [2.102–4.332], p<0.001), hypertension (aOR: 2.449 [1.386–4.327], p=0.002), family history of premature CHD (aOR: 2.724 [1.949–3.808], p<0.001), cumulative cigarette smoking (aOR: 2.317 [1.574–3.410], p<0.001), and joint pain (aOR: 1.457 [1.053–2.016], p=0.023) were the independent RFs for CHD in postmenopausal women, while an inverse association was found between CHD and living in Mount-Lebanon (compared to Beirut, aOR: 0.589 [0.406–0.854], p=0.005), having a moderate individual monthly income (aOR: 0.450 [0.220–0.923], p=0.029), following the Mediterranean diet (aOR: 0.965 [0.936–0.994], p=0.020), and PA (aOR: 0.725 [0.529–0.992] and 0.396 [0.206–0.759], for moderate and high PA, respectively, p=0.007) (Table 4).
 |
Table 4 Factors Believed to Be Associated with Cardiovascular Risk for the Women Studied |
Another protective factor assessed, LMAS, was not significantly associated with CHD at this stage.
Discussion
This is, to our knowledge, the first case-control study conducted to assess RFs of CHD among hospitalized Lebanese women and we hope that the results found will help shed light on a currently not yet sufficiently studied problem concerning the cardiovascular health of aging women. This study was conducted to further clarify the nature of CHD RFs in Lebanese women, not only the elderly but also those of reproductive age. It is not uncommon nowadays to see pre-menopausal women admitted with CHD.
Common coronary RFs were noted, but their relative importance differed in pre- and post-menopausal women. Dyslipidemia was found to be associated with the highest odds ratio in both groups, consistent with previous works, showing that dyslipidemia has the greatest population-adjusted risk in women compared to all other known CVRFs.25 In contrast, other studies in South Asia found a statistically significant relationship in post-menopausal women only,26 which could be explained by their sample size and the younger age of pre-menopausal women included in their study (30 years and older). On another hand, previous data showed that 3.9 million worldwide deaths were attributable to high non-HDLc in 2017, increasing among women since 1980,27 and it is actually well known that lipid levels change in post-menopausal women after reduction of estrogen production (decline in HDLc and increase in LDLc), subsequently contributing to an increased CHD risk.28,29 Moreover, Lebanon has the highest prevalence of hypercholesterolemia30 compared with other countries such as Turkey, Saudi Arabia and India. Also, it has been found that Lebanese women were more likely to suffer from dyslipidemia than men.9
Hypertension was also significantly associated with CHD in both groups which correlates well with the findings of Gierach et al and Maas et al31,32 Our findings underscore the importance of early identification of hypertension in middle-aged women as a first step in the evaluation and treatment of CHD in the premenopausal period, as each 10 mmHg increment of systolic blood pressure was found to be associated with a 25% increased risk of cardiovascular events.4 While hypertension prevalence and severity reach significantly higher rates in women than men over 65, this gap is likely to increase with the aging population.4 A systematic review showed that the hypertension prevalence occurs more frequently among Arab women,33 and is increasing in Lebanon.9 Moreover, women appear to have lower rates of hypertension control than men,34,35 including in Lebanon.36 This could be due to the political instability and various conflicts that have occurred in recent years in Lebanon. Previous studies have demonstrated the importance of stress exposure (war, disaster, explosion and terror) on blood pressure levels and hypertension control, especially among women.37
Similar to previous studies,13 we found that family history of premature CHD increased the CHD risk. It is an independent prognostic indicator, and early detection of silent atherosclerosis may usefully improve the CHD prevention in concerned women. Additionally, a first-degree family history of dyslipidemia predicted CHD in the premenopausal group, which could also help to better identify high-risk women and potentially initiate or intensify CHD prevention strategies.
Smoking, an avoidable factor that appeared to have a multiplicator effect with the other major CHD RFs,4 was well correlated with postmenopausal women’s CHD, with a known cumulative deleterious effect in our study as previously described.38 A meta-analysis reported that women had a 25% increased risk of smoking-induced CHD compared to men.39 However, the harmful impact of smoking in CHD is underestimated, especially in low- and middle-income countries, and real risk on women’s health could be higher.39 Unfortunately, Lebanese women exhibit the highest rates of smoking prevalence of the Middle Eastern countries, due to its liberal character, westernization and the lessening of cultural constraints on women’s behavior.40 WHO reported that about one-third of women in Lebanon use tobacco, compared to 6% in Jordan, a demographic group that could greatly benefit from control initiatives.41,42 However, it seems that implementing such tobacco control programs may be a challenge in Lebanon, given that a recent ban on smoking in public areas has been largely ignored.41
A socio-economic gradient in heart disease, previously reported in wealthy, mainly Western countries, is also discernible in Lebanon.43 In fact, the economic factor was inversely associated with CHD, consistent with population-based studies from Lebanon.8 It suggests that among residents of Lebanon, a middle-income developing country, women with moderate monthly income level have lower odds of CHD than those with a lower monthly income level. However, the higher income level, although achieving an odds ratio<1, did not reach statistical significance, perhaps due to the small (but representative) sample size in this category.
Living in the capital Beirut (crowded urban area) compared to Mount-Lebanon (peri-urban area) was positively associated to CHD. Living in Beirut exposes participants to higher levels of stress, in part due to exposure to various environmental factors, traffic-related air pollutants, noise, higher levels of violence, and lower social support, consistent with previous national8,9 and international44,45 studies. Similarly, the lack of green spaces in an urban area can negatively affect a person’s well-being and PA.46 Previous works revealed that women may be more vulnerable to urbanization in terms of CVRFs (hypertension, psychiatric disorders) than men.7,47,48 Further national analysis will be needed to elucidate the effect of urban environment in Lebanon on cardiovascular health in both genders.
Adherence to LMDS was associated with lower odds of CHD in postmenopausal women, in agreement with previous national studies.49 This relation was also described in recent studies, where adopting a Mediterranean diet pattern was related to improved arterial stiffness and reduced risk of chronic diseases.50,51 Bihuniak et al also demonstrated positive associations between the Mediterranean diet and health of postmenopausal American women, particularly with a reduced risk of CVRFs.52 Furthermore, women adhering to the Mediterranean diet may have better CVRFs protection than men (21% vs 14% respectively).53 Unfortunately, a deviation in dietary habits exists in Lebanon, as in all transitional countries adopting a more Westernized lifestyle.
Moreover, our results showed that moderate or vigorous PA had an inverse association with CHD in women compared to those with no or low PA. This is consistent with data in favor of a substantial reduction in the incidence of cardiovascular events by PA in postmenopausal women.54,55 We also demonstrated an inverse dose-response relationship, with higher activity levels being associated with lower CHD, in agreement with several previous reports.56 However, an overview of systematic reviews and meta-analysis from 20 MENA (Middle East and North Africa) countries revealed that only the adult Lebanese and Jordanian women were more active than men compared to other regions.55 Urbanization, residence in Beirut, car ownership, and obstacles in some areas of Lebanon’s governorates, mainly rural villages, where it is socially unacceptable for women to walk or exercise alone outside the home without the company of a family member, may affect their PA.57,58 In our study, 93% of postmenopausal women were unemployed, factor that may be of importance in physical engagement of women,59 we can deduce that the domestic activity could protect from CHD by fighting against sedentary lifestyle, as has been mentioned by others.60
Finally, an enlightening result of our study was the significant link between CHD and the presence of joint pain. Studied postmenopausal women who suffer from it were almost 1.5 times more likely to have CHD than those without. Thus, this disorder, which increases with age, especially in menopause,61 can not only affect the daily life of aging women, it also limits their PA,62 which increases the CVD risk, therefore has an impact on women’s life expectancy. Additionally, evidence shows that chronic diseases and musculoskeletal disorders frequently coexist; people with musculoskeletal problems are about twice as likely to suffer from chronic diseases such as heart disease, gastric ulcers, neurological and endocrine disorders.63 Other evidence also suggests that this relation is biologically plausible, as daily back pain was associated with reduced quality of life, mobility and longevity and increased risk of coronary events in elderly women.64 Relation between rheumatoid arthritis and heart disease is described,65,66 but very few studies focus on commonplace joint pain.67 A previous study reported that over half (56%) of CHD patients suffered from musculoskeletal conditions, with joint pain accounting for 64.4% of them.61 Joint pain in aging women seems harmless and is thus probably neglected by women, while it could constitute a medical warning sign for them and their attending physicians.
Strengths and Limitations
This study has several strengths in its design: the random selection of controls minimizes associated biases; also, the use of incident cases allows more accurate recall of past exposures, helps with temporality and avoids survival bias. The relatively large number of participants and the choice of a control/case ratio of 4/1 increased its power. However, it is a retrospective observational study that cannot determine causality between factors and disease occurrence. Otherwise, evaluation of some RFs and preventive measures were self-declared, which could lead to misclassification. A differential recall bias could be present, as CHD patients were more likely to remember accurately their exposures’ history compared to non-coronary patients. Finally, although we considered many RFs to decrease potential confounding, residual confounding might still be possible, related to unmeasured factors.
Conclusion
The study of CVRFs in women is a necessity since they are well affected by CHD. Improved screening and therapeutic management of arterial hypertension and dyslipidemia in this population is needed. It is necessary to intensify the fight against smoking and encourage women to adhere to a Mediterranean diet. Screening mechanisms for silent atherosclerosis in women with a family history of premature CHD, increased awareness of dwelling region and reduction of poverty are also important steps. Moreover, the common joint pain, often trivialized and neglected in menopaused women, could be integrated in prevention strategies and dedicated care. Women in pre-menopause could benefit from a dedicated information program aimed at not trivializing this symptom, probably associated with other deleterious elements such as less PA and a more sedentary lifestyle. Taken together, these findings highlight the importance of formulating appropriate policies and implementing interventions to halt the CHD progression in Lebanese women. Thus, the role of policymakers and health providers, in cooperation with the ministry of public health and non-governmental organizations, to provide quality services and to raise awareness in women to lower the burden of the disease.
Abbreviations
aOR, adjusted odds ratio; BDS-22, Beirut Distress Scale; BMI, body mass index; CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; CVRFs, cardiovascular risk factors; HDLc, high-density lipoprotein cholesterol; IPAQ, International Physical Activity Questionnaire; LDLc, low-density lipoprotein cholesterol; LMAS, Lebanese Medication Adherence Scale; LMDS, Lebanese Mediterranean Diet Score; MET, metabolic equivalent; MI, myocardial infarction; OR, odds ratio; PA, physical activity; RFs, risk factors; SPSS, Statistical Package for the Social Sciences; WHO, World Health Organization.
Data Sharing Statement
The data can be made available upon reasonable request to the corresponding author.
Ethics Approval and Informed Consent
The study protocol was reviewed and approved by the Institutional Review Board (IRB) ethical committee of each participating hospital, in accordance with Lebanon’s ethical legislation, and the Declaration of Helsinki. The informed consent process was confirmed by the IRB and obtained from all participants before the interview. Patients were informed that their response will be kept confidential.
Acknowledgments
We would like to thank all our participants who shared with us their personal and intimate information. In addition, to all hospital administrations that agreed to participate in the study. Grateful thanks and recognition to the Military hospital team, especially Colonel Elie Fikani for their cooperation and facilitation of administrative issues.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting the article or reviewing it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to take responsibility and be accountable for all aspects of the work.
Funding
This work was supported by financial grants from Medilab SAL, Beirut, Lebanon [grant number 001/20]. No funding bodies had any role in study design, data collection and analysis, interpretation of data, decision to publish, or preparation of the manuscript.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Almahmeed W, Arnaout MS, Chettaoui R, et al. Coronary artery disease in Africa and the Middle East. Ther Clin Risk Manag. 2012;8:65–72. doi:10.2147/TCRM.S26414
2. Institute for Health Metrics and Evaluation (IHME). Global burden disease profile, Lebanon. Institute for Health Metrics and Evaluation; 2019. Available from: http://www.healthdata.org/lebanon.
3. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–2381. doi:10.1093/eurheartj/ehw106
4. Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141(9). doi:10.1161/CIR.0000000000000757
5. Möller-Leimkühler AM. Gender differences in cardiovascular disease and comorbid depression. Dialogues Clin Neurosci. 2007;9(1):71–83. doi:10.31887/DCNS.2007.9.1/ammoeller
6. Chen Z, Liu M, Zhang S, et al. Urban index and lifestyle risk factors for cardiovascular diseases in China: a cross-sectional study. Sci Prog. 2021;104(1):368504211003762. doi:10.1177/00368504211003762
7. Zhang N. Urban–rural disparities in cardiovascular disease risks among middle-aged and older Chinese: two decades of urbanisation. Ageing Soc. 2020;40(7):1405–1427. doi:10.1017/S0144686X18001794
8. Ramahi T, Khawaja M, Abu-Rmeileh N, Abdulrahim S. Socio-economic disparities in heart disease in the Republic of Lebanon: findings from a population-based study. Heart Asia. 2010;2(1):67–72. doi:10.1136/ha.2009.000851
9. Isma’eel HA, Almedawar MM, Breidy J, et al. Worsening of the cardiovascular profile in a developing country. Glob Heart. 2018;13(4):275–283. doi:10.1016/j.gheart.2018.03.001
10. Mehta LS, Beckie TM, DeVon HA, et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation. 2016;133(9):916–947. doi:10.1161/CIR.0000000000000351
11. Institute for Health Metrics and Evaluation (IHME). Finding from the Global Burden of Disease (GBD) 2017 study. The Lancet; 2018. Available from: http://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017_Booklet.pdf.
12. Ghaddar F, Salameh P, Saleh N, et al. Noncardiac Lebanese hospitalized adult patients’ awareness of their coronary artery disease risk factors. Vasc Health Risk Manag. 2018;14:371–382. doi:10.2147/VHRM.S176167
13. Zeidan RK, Farah R, Chahine MN, et al. Prevalence and correlates of coronary heart disease: first population-based study in Lebanon. Vasc Health Risk Manag. 2016;12:75–84. doi:10.2147/VHRM.S97252
14. Perk J, De Backer G, Gohlke H, et al. European guidelines on cardiovascular disease prevention in clinical practice (version 2012): the Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) * Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2012;33(13):1635–1701. doi:10.1093/eurheartj/ehs092
15. Qureshi KN, Hodkinson HM. Evaluation of a ten-question mental test in the institutionalized elderly. Age Ageing. 1974;3(3):152–157. doi:10.1093/ageing/3.3.152
16. Salameh P, Salame J, Khayat G, et al. Exposure to outdoor air pollution and chronic bronchitis in adults: a case-control study. Int J Occup Environ Med. 2012;3(4):165–177.
17. Bou Serhal R, Salameh P, Wakim N, et al. A new Lebanese medication adherence scale: validation in Lebanese hypertensive adults. Int J Hypertens. 2018;2018:3934296. doi:10.1155/2018/3934296
18. Barbour B, Saadeh N, Salameh PR. Psychological distress in Lebanese young adults: constructing the screening tool ‘BDS-22. Int J Cult Ment Health. 2012;5(2):94–108. doi:10.1080/17542863.2011.563043
19. Hagströmer M, Oja P, Sjöström M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9(6):755–762. doi:10.1079/PHN2005898
20. Lebanon minimum wage - world minimum wage rates; 2020. Available from: https://www.minimum-wage.org/international/lebanon.
21. Sibai AM, Tohme RA, Almedawar MM, et al. Lifetime cumulative exposure to waterpipe smoking is associated with coronary artery disease. Atherosclerosis. 2014;234(2):454–460. doi:10.1016/j.atherosclerosis.2014.03.036
22. McGorrian C, Yusuf S, Islam S, et al. Estimating modifiable coronary heart disease risk in multiple regions of the world: the INTERHEART modifiable risk score. Eur Heart J. 2011;32(5):581–589. doi:10.1093/eurheartj/ehq448
23. The IPAQ group. IPAQ scoring protocol - international physical activity questionnaire; 2005. Available from: https://sites.google.com/site/theipaq/scoring-protocol.
24. Berry W, Feldman S. Multiple Regression in Practice. SAGE Publications, Inc.; 1985. doi:10.4135/9781412985208
25. Garcia M, Mulvagh SL, Merz CNB, Buring JE, Manson JE. Cardiovascular disease in women: clinical perspectives. Circ Res. 2016;118(8):1273–1293. doi:10.1161/CIRCRESAHA.116.307547
26. Nazeer M, Naveed T, Ullah A. A case - control study of risk factors for coronary artery disease in Pakistani females. Ann King Edw Med Univ Print. 2010;16(3):162–168.
27. NCD Risk Factor Collaboration (NCD-RisC). Repositioning of the global epicentre of non-optimal cholesterol. Nature. 2020;582(7810):73–77. doi:10.1038/s41586-020-2338-1
28. Matthews KA, Meilahn E, Kuller LH, Kelsey SF, Caggiula AW, Wing RR. Menopause and risk factors for coronary heart disease. N Engl J Med. 1989;321(10):641–646. doi:10.1056/NEJM198909073211004
29. El Khoudary SR, Aggarwal B, Beckie TM, et al. Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American Heart Association. Circulation. 2020;142(25). doi:10.1161/CIR.0000000000000912
30. Samaha AA, Zouein F, Gebbawi M, et al. Associations of lifestyle and dietary habits with hyperlipidemia in Lebanon. Vessel Plus. 2017. doi:10.20517/2574-1209.2017.18
31. Maas AH, Franke HR. Women’s health in menopause with a focus on hypertension. Neth Heart J. 2009;17(2):68–72. doi:10.1007/BF03086220
32. Gierach GL, Johnson BD, Bairey Merz CN, et al. Hypertension, menopause, and coronary artery disease risk in the Women’s Ischemia Syndrome Evaluation (WISE) Study. J Am Coll Cardiol. 2006;47(3 Suppl):S50–58. doi:10.1016/j.jacc.2005.02.099
33. Tailakh A, Evangelista LS, Mentes JC, Pike NA, Phillips LR, Morisky DE. Hypertension prevalence, awareness, and control in Arab countries: a systematic review. Nurs Health Sci. 2014;16(1):126–130. doi:10.1111/nhs.12060
34. Wilkins K, Gee M, Campbell N. The difference in hypertension control between older men and women. Health Rep. 2012;23(4):33–40.
35. Hage FG, Mansur SJ, Xing D, Oparil S. Hypertension in women. Kidney Int Suppl. 2013;3(4):352–356. doi:10.1038/kisup.2013.76
36. Mouhtadi BB, Kanaan RMN, Iskandarani M, Rahal MK, Halat DH. Prevalence, awareness, treatment, control and risk factors associated with hypertension in Lebanese adults: a cross sectional study. Glob Cardiol Sci Pract. 2018;2018(1):6. doi:10.21542/gcsp.2018.6
37. Pickering TG. Terror strikes the heart–September 11, 2001. J Clin Hypertens Greenwich Conn. 2002;4(1):58–60. doi:10.1111/j.1524-6175.2002.00747.x
38. Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi:10.1016/S0140-6736(04)17018-9
39. Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet Lond Engl. 2011;378(9799):1297–1305. doi:10.1016/S0140-6736(11)60781-2
40. Sibai AM, Iskandarani M, Darzi A, et al. Cigarette smoking in a Middle Eastern country and its association with hospitalisation use: a nationwide cross-sectional study. BMJ Open. 2016;6(4):e009881. doi:10.1136/bmjopen-2015-009881
41. Azar ST, Hantash HA, Jambart S, et al. Factors influencing dyslipidemia in statin-treated patients in Lebanon and Jordan: results of the Dyslipidemia International Study. Vasc Health Risk Manag. 2014;10:225–235. doi:10.2147/VHRM.S57194
42. World Health Organization. World Health Organization NCD country profiles. Lebanon; 2011. Available from: https://www.who.int/nmh/countries/lbn_en.pdf.
43. Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S; Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet Lond Engl. 2008;372(9650):1661–1669. doi:10.1016/S0140-6736(08)61690-6
44. Grazuleviciene R, Andrusaityte S, Dėdelė A, et al. Urban environment and health: a cross-sectional study of the influence of environmental quality and physical activity on blood pressure. Int J Environ Res Public Health. 2021;18(11):6126. doi:10.3390/ijerph18116126
45. Kumar R, Singh MC, Singh MC, et al. Urbanization and coronary heart disease: a study of urban-rural differences in northern India. Indian Heart J. 2006;58(2):126–130.
46. Jia X, Yu Y, Xia W, et al. Cardiovascular diseases in middle aged and older adults in China: the joint effects and mediation of different types of physical exercise and neighborhood greenness and walkability. Environ Res. 2018;167:175–183. doi:10.1016/j.envres.2018.07.003
47. Srivastava K. Urbanization and mental health. Ind Psychiatry J. 2009;18(2):75–76. doi:10.4103/0972-6748.64028
48. Kondo MC, Fluehr JM, McKeon T, Branas CC. Urban green space and its impact on human health. Int J Environ Res Public Health. 2018;15(3):E445. doi:10.3390/ijerph15030445
49. Nasreddine L, Naja F, Sibai AM, Helou K, Adra N, Hwalla N. Trends in nutritional intakes and nutrition-related cardiovascular disease risk factors in Lebanon: the need for immediate action. Leban Med J. 2014;62(2):83–91. doi:10.12816/0004102
50. Mattioli AV, Palmiero P, Manfrini O, et al. Mediterranean diet impact on cardiovascular diseases: a narrative review. J Cardiovasc Med Hagerstown Md. 2017;18(12):925–935. doi:10.2459/JCM.0000000000000573
51. George SM, Ballard-Barbash R, Manson JE, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the women’s health initiative observational study: evidence to inform national dietary guidance. Am J Epidemiol. 2014;180(6):616–625. doi:10.1093/aje/kwu173
52. Bihuniak JD, Ramos A, Huedo-Medina T, Hutchins-Wiese H, Kerstetter JE, Kenny AM. Adherence to a Mediterranean-style diet and its influence on cardiovascular risk factors in postmenopausal women. J Acad Nutr Diet. 2016;116(11):1767–1775. doi:10.1016/j.jand.2016.06.377
53. Dontas AS, Zerefos NS, Panagiotakos DB, Vlachou C, Valis DA. Mediterranean diet and prevention of coronary heart disease in the elderly. Clin Interv Aging. 2007;2(1):109–115. doi:10.2147/ciia.2007.2.1.109
54. Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–725. doi:10.1056/NEJMoa021067
55. Chaabane S, Chaabna K, Abraham A, Mamtani R, Cheema S. Physical activity and sedentary behaviour in the Middle East and North Africa: an overview of systematic reviews and meta-analysis. Sci Rep. 2020;10(1):9363. doi:10.1038/s41598-020-66163-x
56. Sattelmair J, Pertman J, Ding EL, Kohl HW, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–795. doi:10.1161/CIRCULATIONAHA.110.010710
57. Chamieh MC, Moore HJ, Summerbell C, Tamim H, Sibai AM, Hwalla N. Diet, physical activity and socio-economic disparities of obesity in Lebanese adults: findings from a national study. BMC Public Health. 2015;15(1):279. doi:10.1186/s12889-015-1605-9
58. Sibai AM, Costanian C, Tohme R, Assaad S, Hwalla N. Physical activity in adults with and without diabetes: from the ‘high-risk’ approach to the ‘population-based’ approach of prevention. BMC Public Health. 2013;13(1):1002. doi:10.1186/1471-2458-13-1002
59. Sosa M, Sethares KA, Chin E. The impact of demographic and self-management factors on physical activity in women. Appl Nurs Res. 2021;57:151353. doi:10.1016/j.apnr.2020.151353
60. Koolhaas CM, Dhana K, Golubic R, et al. Physical activity types and coronary heart disease risk in middle-aged and elderly persons: the Rotterdam study. Am J Epidemiol. 2016;183(8):729–738. doi:10.1093/aje/kwv244
61. Watt FE. Musculoskeletal pain and menopause. Post Reprod Health. 2018;24(1):34–43. doi:10.1177/2053369118757537
62. Lamb SE, Guralnik JM, Buchner DM, et al. Factors that modify the association between knee pain and mobility limitation in older women: the women’s health and aging study. Ann Rheum Dis. 2000;59(5):331–337. doi:10.1136/ard.59.5.331
63. Williams A, Kamper SJ, Wiggers JH, et al. Musculoskeletal conditions may increase the risk of chronic disease: a systematic review and meta-analysis of cohort studies. BMC Med. 2018;16(1):167. doi:10.1186/s12916-018-1151-2
64. Zhu K, Devine A, Dick IM, Prince RL. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine. 2007;32(18):2012–2018. doi:10.1097/BRS.0b013e318133fb82
65. Goodson N. Coronary artery disease and rheumatoid arthritis. Curr Opin Rheumatol. 2002;14(2):115–120. doi:10.1097/00002281-200203000-00007
66. Lee TH, Song GG, Choi SJ, Seok H, Jung JH. Relationship of rheumatoid arthritis and coronary artery disease in the Korean population: a nationwide cross-sectional study. Adv Rheumatol. 2019;59(1):40. doi:10.1186/s42358-019-0084-6
67. Glehr M, Kaltenbach A, Glehr R, et al. Physician awareness of knee and hip pain in the context of coronary heart disease treatment. ScientificWorldJournal. 2014;2014:494801. doi:10.1155/2014/494801
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
