Back to Journals » Vascular Health and Risk Management » Volume 18
Risk Factors for Calcific Aortic Valve Disease in Afghan Population
Authors Sherzad AG , Shinwari M, Azimee MA, Nemat A , Zeng Q
Received 6 June 2022
Accepted for publication 6 August 2022
Published 18 August 2022 Volume 2022:18 Pages 643—652
DOI https://doi.org/10.2147/VHRM.S376955
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Abdul Ghafar Sherzad,1,2 Muhibullah Shinwari,3 M Azim Azimee,2 Arash Nemat,1,4 Qingchun Zeng1,5
1Department of Cardiology, State Key Laboratory of Organ Failure Research, Nanfang Hospital, Southern Medical University, Guangzhou, Guangdong, People’s Republic of China; 2Department of Biochemistry, Faculty of Medicine, Nangarhar University, Nangarhar, Afghanistan; 3Department of Physiology, Faculty of Medicine, Nangarhar University, Nangarhar, Afghanistan; 4Department of Microbiology, Kabul University of Medical Sciences, Kabul, Afghanistan; 5Guangzhou Regenerative Medicine and Health Guangdong Laboratory, Guangzhou, 5100050, People’s Republic of China
Correspondence: Abdul Ghafar Sherzad, Department of Biochemistry, Faculty of Medicine, Nangarhar University, Nangarhar, Afghanistan, Tel +937 83545284, Email [email protected] Qingchun Zeng, Department of Cardiology, Nanfang Hospital, Southern Medical University, 1838 Northern, Guangzhou Ave, Guangzhou, 510515, People’s Republic of China, Tel/Fax +86 20-61360416, Email [email protected]
Objective: Evidence from previous studies suggests that calcific aortic valve disease (CAVD) is not an unavoidable consequence of aging, and may be linked to explicit risk factors. However, little is known regarding the Afghan population in this context. The current study aimed to identify the clinical features of CAVD and determine independent risk factors for CAVD in the Afghan population.
Patients and Methods: A case-control study was conducted among 1072 Afghan participants (age > 18 years) from January 2018 to December 2020. The study participants were divided into two groups based on echocardiographic findings: 536 individuals with CAVD and 536 age- and sex-matched controls. Data were collected using questionnaires from the medical records of all cases and controls. The independent predictors of CAVD were evaluated using multivariate logistic regression analysis.
Results: The mean age of study participants was 65.3 ± 13.5 years (range, 20– 100 years). Of the 536 patients with CAVD, 77 (14.4%) had aortic valve stenosis, 415 (77.4%) had aortic valve calcification, and 44 (8.2%) had bicuspid aortic valve. Multivariate logistic regression analysis revealed that sedentary lifestyle (odds ratio [OR] = 2.517, p = 003), diabetes mellitus (DM) (OR = 1.902, p = 006), high body mass index (BMI ≥ 30 kg/m2) (OR = 1.776, p = 005), good socioeconomic status (OR = 1.724, p = 021), and hypertension (OR = 1.664, p ˂0.001) were independent risk factors for CAVD in the Afghan population.
Conclusion: It was observed that sedentary lifestyle, diabetes mellitus, high BMI (≥ 30 kg/m2), good socioeconomic status, and hypertension are independent risk factors for the development of CAVD compared to those with a normal aortic valve in the Afghan population.
Keywords: aortic valve sclerosis, aortic valve calcification, aortic valve stenosis, risk factors for atherosclerosis, independent risk factors
Introduction
Calcific aortic valve disease (CAVD) begins with early aortic valve sclerosis (AVSc), which is characterized by leaflet thickening without restriction of left ventricular outflow and evolves later to acquired aortic valve stenosis (AVS), which is characterized by leaflet stiffening, flow obstruction, and compromised cardiac function.1 According to a study by Otto et al, individuals with sclerosis have a 50% greater risk of cardiovascular events such as myocardial infarction and death from heart disease as a result of CAVD.2 CAVD is a major public health concern worldwide; in 2019, there were an estimated 9,404,078 cases (male 5,027,261, female 4,376,817) of CAVD. Globally, even with age standardization, CAVD incidence, prevalence, and mortality increased 3.51, 4.43, and 1.38-fold from 1990 to 2019, respectively. In 2019, an estimated 126,827 patients (54,175 men and 72,652 women) died from CAVD globally. The highest mortality from CAVD was recorded in the USA, followed by that in Germany and Japan (248,256, 13,154, and 12,868, respectively).3 CAVD is the third most common cardiovascular disease in the western world, after coronary heart disease and hypertension, and accounts for half of all valvular heart disease.4 It is the most common indication for aortic valve replacement surgery or transcatheter treatment.5,6 CAVD has been linked to risk factors of atherosclerosis and shows several similarities to atherosclerotic heart disease in terms of etiological, clinical, and histopathologic characteristics.7 It is currently recognized that an active inflammatory process such as atherosclerosis causes CAVD, rather than the previously held belief that age was the only risk factor.8 Previous research on CAVD has shown links with risk factors for atherosclerosis, although the important variables have differed across investigations. Aronow et al studied a very senior population using 2D echocardiography and revealed that hypertension, diabetes mellitus (DM), and high total cholesterol and low HDL cholesterol levels were linked to a higher incidence of CAVD.9 CAVD risk factors are comparable to those of atherosclerosis, including advanced age, male sex, smoking, high cholesterol, high blood pressure, DM, and renal failure.10 Other researchers have attributed aortic valve calcification (AVC) to age, male sex, high blood pressure, high LDL cholesterol, and metabolic diseases such as Paget’s disease, hyperparathyroidism, and anatomical abnormalities that impede sufficient flow (such as a bicuspid valve) are also important risk factors for AVC.11 According to current data, clinically significant atherosclerosis is not present in 50% of patients with CAVD.12 Evborn et al; Thanassoulis et al; Dumesnil et al; Lindroos et al; and Messika et al, as cited in Kaltoft et al, identified obesity as another factor that can raise the risk of aortic valve stenosis, but inconsistent evidence has been provided in earlier research studies.13 Furthermore, a recent study revealed a significant association between a high body mass index and the risk of developing aortic valve stenosis, Larsson et al cited in Kaltoft et al.13 In addition, Kaltoft et al tested the hypothesis that genetically based obesity measured using body mass index is causally associated with the risk of aortic valve stenosis and replacement.13 Consequently, the genesis of CAVD has been linked to atherosclerotic pathways. CAVD cannot be prevented or stopped using currently available pharmacologic therapy. A detailed investigation of the independent risk factors needs to be undertaken to establish preventive measures and modes of medical therapy for CAVD. The prevalence and impact of CAVD impose a great burden on the healthcare system and social services, especially with the advancement of the economy, which warrants a comprehensive understanding of the relevant risk factors. However, studies investigating the prevalence and risk factors for CAVD in Afghanistan are lacking. Therefore, the present study was designed to reveal the potential clinical pointers that may be associated with the development of CAVD, which can deepen our understanding of the disease and enable the development of treatment strategies in the Afghan population.
Materials and Methods
Study Design and Sampling
A retrospective case-control study design was used with 1072 participants, who were admitted or treated as outpatients at the cardiology unit of Amiri Medical Complex, Sahak Cardiac Care Center, Cure Hospital, and Daudzai Medical Complex during the time frame from January 2018 to December 2020. The study population were classified into two groups based on echocardiography findings: 536 CAVD cases and 536 age- and sex-matched controls were included in the study. The inclusion criteria were: 1) patients first diagnosed as having significant CAVD during echocardiography; hyper echogenic valves, focal areas of leaflet thickening, leaflet activity not restricted, valve area ≥ 3 cm2, and a transvalvular blood flow rate of ≤ 2.5 m/s was defined as AVC; thickened leaflets with reduced systolic opening on 2D imaging and an increased anterograde velocity (≥ 2.5 m/s) across the valve, and valve area < 3 cm2 was defined as aortic stenosis.10 2) residents of Afghanistan. 3) Age ≥18 years. Patients with rheumatic heart disease, congenital heart disease (except bicuspid aortic valve), and those who had repeated echocardiography were excluded from the study. The control group consisted of a similar number of age- and sex-matched visitors to the hospital undergoing elective diagnostic echocardiography for suspected cardiovascular disease at the same hospitals who were free from any evidence of CAVD. The Kelesy method was used to calculate the sample size. The Open Epi (http://www.openepi.com/SampleSize/SSMean.htm) Sample Size calculator was used to identify a representative sample with consideration of 95% two-sided confidence level, 80% power, ratio of case to control 1, 45% hypothetical proportion of controls with exposure, and 1.5% least extreme odds ratio to be detected. The calculated sample size for this study was 1072 participants (536 CAVD cases and 536 age- and sex-matched controls).14
Data Collection and Patient Characteristics
Data were collected from the medical records of all the cases and controls. The data contained demographic characteristics (age, sex, body mass index [BMI], marital status, occupation, education, physical activity, and socioeconomic status), as well as important risk factors such as smoking, history of hypertension, DM, hyperlipidemia, coronary heart disease, family history of coronary heart disease, presence of chronic renal failure, laboratory parameters (total cholesterol [TC], triglyceride [TG], low-density lipoprotein [LDL] cholesterol, high-density lipoprotein [HDL] cholesterol, fasting blood glucose, blood urea nitrogen, and creatinine levels), and echocardiography findings. Patients with systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, self-reported hypertension, or those on anti-hypertensive medication were defined as having hypertension.15 Patients with fasting blood glucose ≥ 126 mg/dl, self-reported DM, or use of insulin or other oral hypoglycemic drugs were classified as having DM.15 Hyperlipidemia was defined as serum cholesterol > 200 mg/dl, low-density lipoprotein cholesterol level > 130 mg/dl, or use of lipid lowering agents.16 Considerable coronary angiographic evidence of coronary artery disease [CAD] with 50% or greater occlusion of at least one main coronary artery or a major branch (> 2.5-mm diameter) was deemed significant. Angina pectoris or a proven myocardial infarction were categorized as CAD.17 Family history of CAD was defined as disease in a first-degree male relative aged ˂ 55 years and first-degree female relative aged ˂ 55 years of age; smoking was defined as > 10 pack-years of smoking.8 BMI was calculated for all participants, and obesity was defined as BMI ≥ 30 kg/m2.18 Physical activity was classified as sedentary (nearly completely inactive); regular moderate activity (eg trying to run, heavy gardening, calisthenics) for a minimum 3 hours per week; and intense (regular hard physical preparation for competing (eg running events and racing)).19
Echocardiography
Echocardiography was performed for all participants, and two-dimensional echocardiographic examinations were performed (parasternal long-axis, short-axis, and apical long-axis views) using a cardiac ultrasound machine (model SSH-160A, Toshiba, Tustin, California). Aortic valve abnormalities were classified as AVC, aortic stenosis, and bicuspid aortic valve. Calcification was defined as an antegrade valve velocity of ≤ 2.5 m/s, valve area ≥ 3 cm2 and increasing echogenicity and thickness of the leaflets without limitation of mobility. Stenosis was defined as thickened leaflets with reduced systolic opening on 2D imaging, increased antegrade valve velocity (≥ 2.5 m/s) across the valve and valve area < 3 cm2.10
Ethical Approval and Consent
This manuscript is the result of a series of retrospective studies conducted in partial fulfillment of the Master of Cardiovascular diseases at the Southern Medical University, China. Dr. Abdul Ghafar Sherzad, Assistant Professor at Nangarhar University, is the corresponding author, who has conducted his research under the academic supervision of Professor Qingchun Zeng. This study was conducted in Afghanistan after receiving ethical approval (referencing IBR no.4/10-08-2020) from the Department of Research, Faculty of Medicine, Nangarhar University. Consent was waived for obtaining data from medical records of deceased patients. However, consent was obtained from remaining patients via phone. The study complies with the Declaration of Helsinki.
Statistical Analysis
Initial data were entered into an Excel spreadsheet then exported to Statistical Package for the Social Sciences (SPSS) software version 26.0 for analysis. The distribution of quantitative data was tested for normality using the Shapiro–Wilk test, and summarized as the mean ± SD with approximately normal distributions and compared using Student’s t-test, or as median and interquartile ranges for continuous variables with skewed distributions and analyzed by nonparametric Mann–Whitney U-test, respectively. All qualitative data were recorded as numbers (n) or rates (%). Comparisons between the two groups for categorical data were performed using the chi-squared test and post hoc chi-square test to reduce the chances of obtaining false – positive results (type 1 errors). Univariate logistic regression was used to analyze risk factors for CAVD. A multivariable logistic regression model was used to assess the independent predictors of CAVD. Significant univariate variables with a p value < 0.05 were included in the multiple logistic regression analysis for OR and 95% confidence intervals. All p values were two-sided, and a p value < 0.05 was considered statistically significant.
Results
In this study, a total of 1072 individuals were enrolled, of whom 64.7% were male and 35.3% were female. The mean age of study participants was 65.3 ± 13.2 years (range, 20–100 years). Of the total number of patients with CAVD, 77/536 (14.4%) had aortic valve stenosis, 415/536 (77.4%) had AVC, and 44/536 (8.2%) had bicuspid aortic valve. Sedentary activity, DM, high BMI (≥ 30 kg/m2), good socioeconomic status, and hypertension were significantly more prevalent in patients with CAVD than in the control group. There was no significant association between CAVD cases and the presence of hyperlipidemia, CAD, smoking, and chronic renal failure. The statistical data of the baseline information of the study participants and cardiovascular risk factors of CAVD cases and the control group are shown in Tables 1 and 2.
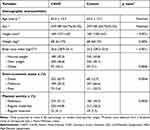 |
Table 1 Demographic Characteristics Among CAVD Cases and Control Participants |
 |
Table 2 Cardiovascular Risk Factors Among CAVD Cases and Control Participants |
The participants were divided into 3 groups: group 1, normal weight; group 2, overweight; and group 3, obese. Using chi-square analysis, we found a significant association between BMI groups and CAVD occurrence. On the other hand, using the post hoc chi-square test, it was also revealed that participants who were at a higher risk of obesity were case patients (P = 0.004) (Table 1).
Categorical and continuous variables found to have a statistically significant association with CAVD in the chi-squared test; Student’s t-test and Mann–Whitney U-test analysis were first entered into a univariate logistic regression model (one DV and one IV) with CAVD as the dependent variable. The findings revealed that DM, high BMI ≥30 kg/m2), good socioeconomic status, sedentary lifestyle, hyperlipidemia, hypertension, CAD, family history of CAD, smoking, elevated levels of TC, TG, LDL, decreased HDL, and high FBS were statistically significant risk factors for CAVD (Table 3).
 |
Table 3 Risk Factors Associated with CAVD: Univariate Logistic Regression Analysis |
A multivariate logistic regression analysis was used to further confirm the independent risk factors for CAVD. Independent risk factors found to have a statistically significant association with CAVD in the univariate analysis were entered into a multivariate logistic regression model (one DV and more IV) with CAVD as the dependent variable. The findings revealed that sedentary lifestyle, DM, high BMI (≥30 kg/m2), good socioeconomic status, and hypertension were independent risk factors for CAVD in the Afghan population (Table 4).
 |
Table 4 Risk Factors Associated with CAVD: Multivariate Logistic Regression Analysis |
The analysis was repeated using a multiple variable logistic regression model. Age was used as a continuous variable. Sex, sedentary physical activity, good socioeconomic status, BMI, hypertension, and diabetes were included as categorical variables. After adjusting for age and sex, sedentary physical activity was associated with a 5.9-fold higher risk, hypertension was associated with a 1.9-fold higher risk, obesity was associated with a 1.8-fold higher risk, good socioeconomic status was associated with a 1.7-fold higher risk, and DM was associated with a 1.6-fold higher risk of CAVD (Table 5).
 |
Table 5 Multivariate Logistic Regression Analysis Adjusted for Age and Sex |
In addition, coronary artery disease (CAD), hyperlipidemia, and smoking were not statistically significantly associated with CAVD.
Discussion
Multiple independent risk factors have been implicated in the development of CAVD.20 The current case-control study findings reveal a significant link between independent risk factors for atherosclerosis and the existence of CAVD in the Afghan population. To the best of our knowledge, this was the first study to investigate this type of association, which was not identified by other studies conducted in a specific Afghan context. As a result, our study was conducted to determine whether there were any independent risk factors for CAVD development in the Afghan population.
In this study, a total of 1072 individuals were enrolled, of which 64.7% were male and 35.3% were female. The mean age of study participants was 65.3 ± 13.2 years (range, 20 −100 years). Of the total number of patients with CAVD, 77/536 (14.4%) had aortic valve stenosis, 415/536 (77.4%) had AVC, and 44/536 (8.2%) had bicuspid aortic valve. The study found that sedentary lifestyle, DM, high BMI (≥ 30 kg/m2), good socioeconomic status, and hypertension were independent risk factors for CAVD in the Afghan population. CAD, hyperlipidemia, and smoking were not significantly associated with CAVD.
A sedentary lifestyle is a risk factor for cardiovascular disease, according to observational, epidemiologic, postmortem, and physiologic studies.21,22 One study found that atherosclerosis could be reversed/prevented with exercise in experimental animals.23 Investigation, i.e. that there was a significant association between a sedentary lifestyle and CAVD occurrence (p = 0.003). This finding is in contrast to that reported by Kontogeorgos et al, who found an insignificant association between aortic valve sclerosis and sedentary lifestyle.24 The significant results in our study can be attributed to the fact that people from higher social classes in our country do not exercise routinely; and some are even ashamed of exercising in public as people make fun of them. Moreover, most of the study participants belonged to the sedentary lifestyle group (51.1% among the test cases and 34.5% among controls) as compared to the regular moderate activity and regular intense activity groups.
Our study reported that DM was an independent risk factor for CAVD (p value = 0.006). These findings are consistent with those of studies conducted by Aronow et al, Adler et al, Mohler et al, Messika-Zeitoun et al, Ferreira González et al, Hacioglu et al, Thaden et al, Yan et al, Ye et al, and Kontogeorgos et al,9,24–32 all of which revealed that DM was an independent risk factor for CAVD, whereas other studies did not.10,14,24
CAVD caused by obesity may result from metabolic changes in the obese body or structural alterations to the heart. Structurally, obesity raises blood pressure, which puts more workload on the heart and may affect the morphology of the left ventricle33 and aortic valve, and promote atherosclerosis by injuring endothelial cells.34 Obesity, through its metabolic effects, raises the concentrations of atherogenic lipoproteins35 that are deposited on the aortic valve leaflets.34 Continuous damage and lipid accumulation trigger an inflammatory response and the invasion of mast cells, macrophages, and T-lymphocytes36 inflammatory mediators induce the differentiation of valve interstitial cells into osteoblasts, which results in the calcification of the valve leaflets.34 Evborn et al; Thanassoulis et al; Dumesnil et al; Lindroos et al; and Messika et al, as cited in Kaltoft et al, identified the association between BMI and aortic valve stenosis, which has shown inconsistent evidence.13 Furthermore, a recent study revealed a significant relationship between a high body mass index and with the risk of developing aortic valve stenosis Larsson et al cited in Kaltoft et al.13 Besides this, Kaltoft et al, tested the hypothesis that genetically based obesity measured by body mass index is causally associated with risk of aortic valve stenosis and replacement.13 In support of our findings, previous studies have demonstrated that high BMI (≥ 30 kg/m2) was an independent risk factor for CAVD.7,24,30,37,38
In the present study, a significant association was found between the good socioeconomic group and CAVD (p = 0.004). This finding is in contrast with the findings of a study conducted by Picardo et al who reported no significant association between aortic valve sclerosis and socioeconomic status.39 This result may be because most our study participants belonged to a higher socioeconomic group (65.7% among cases and 12.7% among controls). Moreover, in our country, affluent people consume more sugar and fatty food, do not exercise regularly, and commute by car.
Furthermore, the present study revealed that hypertension was an independent risk factor for CAVD (p < 0.001). These findings are consistent with the findings of several studies,7,9,10,28,29,31,32,37,38,40,41 which reported a significant association between hypertension and CAVD risk. These findings are in contrast to those of the studies conducted by Ye et al, Chadha et al, Sathyamurthy, and Picardo et al, who reported no significant association between aortic valve sclerosis and hypertension.8,27,39,42
Potential explanations for the association between hypertension and aortic valve disease include the possibility that hypertension results in abnormally high tensile stress on the aortic leaflets. Alternatively, turbulent flow patterns associated with high volume flow rates may lead to low shear stress, resulting in endothelial injury and disruption, as is seen in atherosclerotic lesions.10
This study did not identify a statistically significant association between high blood lipid levels, smoking, coronary artery disease, and risk of CAVD, potentially because of the better contemporary treatment of hyperlipidemia. This was especially true for statins. To identify AVC in patients with dyslipidemia, the increased level of lipoprotein (a) (Lp (a)) in the blood is considered an important risk factor for CAVD. Unfortunately, in our study, there was no information about Lp (a) in the medical records of the patients concerned. In addition, these laboratory tests are not available in our country. Hence, the association between hyperlipidemia and CAVD was found to be not statistically significant. Additional research is needed to better understand the relationship between Lp (a) levels and the risk of CAVD.
Smoking is generally considered a bad habit in our community, and smokers usually conceal it from other people and physicians. Therefore, the smoking graph was probably falsely low. Compared to other studies, we found that any independent association of smoking with CAVD was not statistically significant.
According to current data, clinically significant atherosclerosis is not present in 50% of patients with CAVD.12 The majority of patients with CAD do not develop aortic valve disease, despite the fact that atherosclerosis and CAVD have the same risk factors.8,16,43
In the present study, this may be explained as follows: owing to economic problems and the unavailability of advanced diagnostic tools such as angiography and standardized, quantifiable imaging tools for the assessment of aortic valve sclerosis and stenosis in Afghanistan, where patients cannot afford to undergo advanced investigations and treatment. Instead, electrocardiography is the only routine diagnostic tool for patients with CAD in Afghanistan’s hospitals and is not specific for diagnosing CAD. Therefore, patients might not have been correctly diagnosed, and sometimes were misdiagnosed. In addition, long-term antiplatelet and lipid-lowering drugs are prescribed for most patients, which may decrease the incidence of AVC. Therefore, our study showed no significant independent association between CAD and CAVD.
Furthermore, age and sex were independent risk factors for CAVD in other studies, but we could not prove it as risk factors because we conducted pairs matched case-control study. Once we have matched controls to cases according to a given characteristic (age, sex), we cannot study that characteristic.
This study had several limitations. First and most importantly, it was a case-control study, and we failed to determine the incidence of CAVD in the Afghan population. This further limited the deduction of any causal association between the risk factors and CVAD. Another major limitation in all case-control studies is the influence of confounding factors that may bias the observed association. Another shortcoming is a conceptual problem with matching of the control; once we have matched controls to cases according to a given characteristic; study of that characteristic becomes superfluous. It is also worth mentioning that the sample size of the current study was comparable to that of other published international studies; however, there are no studies available on the subject in the context of Afghanistan.
Conclusion
The study found a statistically significant independent association between risk factors for atherosclerosis and CAVD in the Afghan population, regardless of age or sex. It has been shown by the present study that a sedentary lifestyle, high BMI (≥ 30 kg/m2), DM, good socioeconomic status, and hypertension are independent risk factors for the development of CAVD in the Afghan population.
Data Sharing Statement
In order to ensure confidentiality of the participants in this study and to perceive ethical consideration, data cannot be publicly released. Hence, data can be accessed upon request from Dr. Abdul Ghafar Sherzad, Assistant Professor, Department of Biochemistry, Faculty of Medicine, Nangarhar University, Nangarhar, Afghanistan, via email: [email protected]
Acknowledgments
The authors would like to express their gratitude to the research departments, specifically the cardiology units of Amiri Medical Complex, Sahak Cardiac Care Center, Cure Hospital, and Daudzai Medical Complex, for all their contributions and research inputs.
Author Contributions
All authors made substantial contributions to the conception, design, acquisition of data, or analysis and interpretation of data, and took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work. All the authors have read and approved the final manuscript.
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Rajamannan NM, Evans FJ, Aikawa E, et al. Calcific aortic valve disease: not simply a degenerative process a review and agenda for research from the national heart and lung and blood institute aortic stenosis working group. Circulation. 2011;124(16):1783. doi:10.1161/CIRCULATIONAHA.110.006767
2. Otto CM, Lind BK, Kitzman DW, Gersh BJ, Siscovick DS. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly. N Engl J Med. 1999;341(3):142–147. doi:10.1056/NEJM199907153410302
3. Yi B, Zeng W, Lv L, Hua P. Changing epidemiology of calcific aortic valve disease: 30-year trends of incidence, prevalence, and deaths across 204 countries and territories. Aging. 2021;13(9):12710–12732. doi:10.18632/aging.202942
4. Scatena M, Jackson MF, Speer MY, Leaf EM, Wallingford MC, Giachelli CM. Increased calcific aortic valve disease in response to a diabetogenic, procalcific diet in the LDLr-/-ApoB100/100 mouse model. Cardiovasc Pathol. 2018;34:28–37. doi:10.1016/j.carpath.2018.02.002
5. Iung B, Vahanian A. Degenerative calcific aortic stenosis: a natural history. Heart. 2012;98(Suppl4):iv7–iv13. doi:10.1136/heartjnl-2012-302395
6. Hisamatsu T, Miura K, Fujiyoshi A, et al. Serum magnesium, phosphorus, and calcium levels and subclinical calcific aortic valve disease: a population-based study. Atherosclerosis. 2018;273:145–152. doi:10.1016/j.atherosclerosis.2018.03.035
7. Agmon Y, Khandheria BK, Meissner I, et al. Aortic valve sclerosis and aortic atherosclerosis: different manifestations of the same disease?: insights from a population-based study. J Am Coll Cardiol. 2001;38(3):827–834. doi:10.1016/S0735-1097(01)01422-X
8. Chadha D, Malani S, Bharadwaj P, Karthikeyan G, Hasija P. Risk factors for degenerative aortic valve disease in India: a case control study. Med J Armed Forces India. 2018;74(1):33–37. doi:10.1016/j.mjafi.2017.03.004
9. Aronow WS, Schwartz KS, Koenigsberg M. Correlation of serum lipids, calcium, and phosphorus, diabetes, mellitus and history of systemic hypertension with presence or absence of calcified or thickened aortic cusps or root in elderly patients. Am J Cardiol. 1987;59(9):998–999. doi:10.1016/0002-9149(87)91144-1
10. Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. J Am Coll Cardiol. 1997;29(3):630–634. doi:10.1016/S0735-1097(96)00563-3
11. Faggiano P, Antonini-Canterin F, Baldessin F, Lorusso R, D’Aloia A, Dei Cas L. Epidemiology and cardiovascular risk factors of aortic stenosis. Cardiovasc Ultrasound. 2006;4(1):1–5. doi:10.1186/1476-7120-4-27
12. Honda S, Miyamoto T, Watanabe T, et al. A novel mouse model of aortic valve stenosis induced by direct wire injury. Arterioscler Thromb Vasc Biol. 2014;34(2):270–278. doi:10.1161/ATVBAHA.113.302610
13. Kaltoft M, Langsted A, Nordestgaard BG. Obesity as a Causal risk factor for aortic valve stenosis. J Am Coll Cardiol. 2020;75(2):163–176. doi:10.1016/j.jacc.2019.10.050
14. Pohle K, Otte M, Mäffert R, et al. Association of cardiovascular risk factors to aortic valve calcification as quantified by electron beam computed tomography. Elsevier. 2004;79:1242–1246.
15. Iwata S, Walker MD, Di Tullio MR, et al. Aortic valve calcification in mild primary hyperparathyroidism. J Clin Endocrinol Metab. 2012;97(1):132–137. doi:10.1210/jc.2011-2107
16. Ortlepp J, Schmitz F, Bozoglu T, Hanrath P, Hoffmann R. Cardiovascular risk factors in patients with aortic stenosis predict prevalence of coronary artery disease but not of aortic stenosis: an angiographic pair matched case–control study. Heart. 2003;89(9):1019–1022. doi:10.1136/heart.89.9.1019
17. Hoagland PM, Cook EF, Flatley M, Walker C, Goldman L. Case-control analysis of risk factors for presence of aortic stenosis in adults (age 50 years or older). Am J Cardiol. 1985;55(6):744–747. doi:10.1016/0002-9149(85)90149-3
18. Fakhrzadeh H, Bandarian F, Adibi H, et al. Coronary heart disease and associated risk factors in Qazvin: a population-based study. East Mediterr Health J. 2008;14(1):33–41.
19. Saltin B, Grimby G. Physiological analysis of middle-aged and old former athletes: comparison with still active athletes of the same ages. Circulation. 1968;38(6):1104–1115. doi:10.1161/01.CIR.38.6.1104
20. Sathyamurthy I, Alex S. Calcific aortic valve disease: is it another face of atherosclerosis? Indian Heart J. 2015;67(5):503–506. doi:10.1016/j.ihj.2015.07.033
21. Blackburn H, Jacobs JDR. Physical activity and the risk of coronary heart disease. Mass Medical Soc. 1988;319:1217–1219.
22. Ijaz B, Siddique S, Khan AA, Najib MA. Risk factors for coronary artery disease. Proceeding SZPGMI. 1990;5:37-45. Available from: https://proceedings-szmc.org.pk/public/old-doc/1991/Risk-Factors-for-Coronary-Artery-Disease-An-Epidemiological-Study.pdf/. Accessed August 16, 2022.
23. Blankenhorn DH, Kramsch DM. Reversal of atherosis and sclerosis. The two components of atherosclerosis. Circulation. 1989;79(1):1–7. doi:10.1161/01.CIR.79.1.1
24. Kontogeorgos S, Thunström E, Basic C, et al. Prevalence and risk factors of aortic stenosis and aortic sclerosis: a 21-year follow-up of middle-aged men. Scand Cardiovasc J. 2020;54(2):115–123. doi:10.1080/14017431.2019.1685126
25. Adler Y, Fink N, Spector D, Wiser I, Sagie A. Mitral annulus calcification—a window to diffuse atherosclerosis of the vascular system. Atherosclerosis. 2001;155(1):1–8. doi:10.1016/S0021-9150(00)00737-1
26. Mohler ER. Mechanisms of aortic valve calcification. Am J Cardiol. 2004;94(11):1396–1402. doi:10.1016/j.amjcard.2004.08.013
27. Ye T, Ma T, Wang Q, et al. 江苏省无锡市老年人主动脉瓣膜钙化患病率及危险因素分析 [Prevalence and risk factors of aortic valve calcification among the elderly residents of Wuxi city, Jiangsu province]. Zhonghua Xin Xue Guan Bing Za Zhi. 2019;47(7):544–548. Chinese. doi:10.3760/cma.j.issn.0253-3758.2019.07.007
28. Ferreira-González I, Pinar-Sopena J, Ribera A, et al. Prevalence of calcific aortic valve disease in the elderly and associated risk factors: a population-based study in a Mediterranean area. Eur J Prev Cardiol. 2013;20(6):1022–1030. doi:10.1177/2047487312451238
29. Thaden JJ, Nkomo VT, Suri RM, et al. Sex-related differences in calcific aortic stenosis: correlating clinical and echocardiographic characteristics and computed tomography aortic valve calcium score to excised aortic valve weight. Eur Heart J. 2016;37(8):693–699. doi:10.1093/eurheartj/ehv560
30. Messika-Zeitoun D, Bielak LF, Peyser PA, et al. Aortic valve calcification: determinants and progression in the population. Arterioscler Thromb Vasc Biol. 2007;27(3):642–648. doi:10.1161/01.ATV.0000255952.47980.c2
31. Yan AT, Koh M, Chan KK, et al. Association between cardiovascular risk factors and aortic stenosis: the CANHEART aortic stenosis study. J Am Coll Cardiol. 2017;69(12):1523–1532. doi:10.1016/j.jacc.2017.01.025
32. Hacioglu B, Ozturk S, Gursu M, et al. Lipid profile and inflammation in degenerative valvular disease. Med Bull Haseki. 2015;53:1.
33. Otto CM, Prendergast B. Aortic-valve stenosis—from patients at risk to severe valve obstruction. N Engl J Med. 2014;371(8):744–756. doi:10.1056/NEJMra1313875
34. Pawade TA, Newby DE, Dweck MR. Calcification in aortic stenosis: the skeleton key. Am J Cardiol. 2015;66(5):561–577. doi:10.1016/j.jacc.2015.05.066
35. Varbo A, Benn M, Smith GD, Timpson NJ, Tybjærg-Hansen A, Nordestgaard BG. Remnant cholesterol, low-density lipoprotein cholesterol, and blood pressure as mediators from obesity to ischemic heart disease. Circ Res. 2015;116(4):665–673. doi:10.1161/CIRCRESAHA.116.304846
36. Otto CM, Kuusisto J, Reichenbach DD, Gown AM, O’Brien KD. Characterization of the early lesion of’degenerative’valvular aortic stenosis. Histological and immunohistochemical studies. Circulation. 1994;90(2):844–853. doi:10.1161/01.CIR.90.2.844
37. Peltier M, Trojette F, Sarano ME, Grigioni F, Slama MA, Tribouilloy CM. Relation between cardiovascular risk factors and nonrheumatic severe calcific aortic stenosis among patients with a three-cuspid aortic valve. Am J Cardiol. 2003;91(1):97–99. doi:10.1016/S0002-9149(02)03010-2
38. Owens DS, Katz R, Takasu J, Kronmal R, Budoff MJ, O’Brien KD. Incidence and progression of aortic valve calcium in the multi-ethnic study of atherosclerosis (Mesa). Am J Cardiol. 2010;105(5):701–708. doi:10.1016/j.amjcard.2009.10.071
39. Picardo PJ, Khariong PDS, Hajong R, et al. Study of aortic valve sclerosis as a marker of Atherosclerosis in acute coronary syndromes. J Clin Diagn Res. 2016;10(12):OC05.
40. LlNDROOS M, Kupari M, Valvanne J, Strandberg T, Heikkilä J, TlLVIS R. Factors associated with calcific aortic valve degeneration in the elderly. Eur Heart J. 1994;15(7):865–870. doi:10.1093/oxfordjournals.eurheartj.a060602
41. Linefsky J, Katz R, Budoff M, et al. Stages of systemic hypertension and blood pressure as correlates of computed tomography-assessed aortic valve calcium (from the multi-ethnic study of atherosclerosis). Am J Cardiol. 2011;107(1):47–51. doi:10.1016/j.amjcard.2010.08.042
42. Sathyamurthy I, Alex S, Kirubakaran K, Sengottuvelu G, Srinivasan K. Risk factor profile of calcific aortic stenosis. Indian Heart J. 2016;68(6):828–831. doi:10.1016/j.ihj.2016.04.007
43. Rossi A, Gaibazzi N, Dandale R, et al. Aortic valve sclerosis as a marker of coronary artery atherosclerosis; a multicenter study of a large population with a low prevalence of coronary artery disease. I J Cardiol. 2014;172(2):364–367.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
