Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
Risk Factors and Neurologic Outcomes in Patients with Traumatic Brain Injury and Coagulopathy Within 72 h After Surgery
Authors Chang T, Yan X, Zhao C, Zhang Y, Wang B, Gao L
Received 8 June 2021
Accepted for publication 6 August 2021
Published 10 September 2021 Volume 2021:17 Pages 2905—2913
DOI https://doi.org/10.2147/NDT.S323897
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Taro Kishi
Tao Chang,1,* Xigang Yan,2,* Chao Zhao,3,* Yufu Zhang,4 Bao Wang,4 Li Gao4
1Department of Emergency, The Second Affiliated Hospital of Air Force Medical University, Xi’an, 710038, Shaanxi Province, People’s Republic of China; 2Department of Anesthesiology, The Second Affiliated Hospital of Air Force Medical University, Xi’an, 710038, Shaanxi Province, People’s Republic of China; 3Department of Neurology, The Second Affiliated Hospital of Air Force Medical University, Xi’an, 710038, Shaanxi Province, People’s Republic of China; 4Department of Neurosurgery, The Second Affiliated Hospital of Air Force Medical University, Xi’an, 710038, Shaanxi Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Li Gao
Department of Neurosurgery, The Second Affiliated Hospital of Air Force Medical University, No. 1, Xinsi Road, Xi’an, 710038, Shaanxi Province, People’s Republic of China
Tel +86 29-84777765
Email [email protected]
Objective: The purpose of this study was to explore the effect of coagulopathy in patients with traumatic brain injury (TBI) during the early postoperative period.
Methods: The baseline characteristics, intraoperative management, and follow-up data of 462 patients with TBI between January 2015 and June 2019 were collected and retrospectively analyzed by multivariate logistic regression. Coagulopathy was defined as activated partial thromboplastin time > 40 s, international normalized ratio > 1.4, or platelet counts < 100× 109/L.
Results: Multivariate logistic regression analysis revealed that the Glasgow Coma Scale (GCS) on admission, Injury Severity Score (ISS) on admission, pupil mydriasis, duration of surgery, intraoperative blood loss, and intraoperative crystalloid resuscitation were independent risk factors for patients who developed coagulopathy after surgery. There were statistical differences in mortality (p = 0.049), the Glasgow Outcome Scale-Extended (GCS-E; p = 0.024), and the modified Rankin Scale (p = 0.043) between the patients with and without coagulopathy 1 week after surgery. Coagulopathy within 72 h after surgery revealed the higher mortality at 1 week (66.7%), 3 months (71.4%), and 6 months (76.2%). Coagulopathy within 72 h after surgery in patients with a TBI predicted worse disease progression and unfavorable neurologic outcomes.
Conclusion: Taking practical and reasonable measures to manage these risk factors may protect patients with TBI from postoperative coagulopathy.
Keywords: traumatic brain injury, postoperative coagulopathy, surgery, risk factor, mortality
Introduction
The prevalence of coagulopathy is 7–63% in patients with traumatic brain injury (TBI) and >60% in patients with severe TBI on admission.1,2 The overall mortality of TBI-associated coagulopathy is 17%–86%, and approximately 34% occur within 24 h after the injury.3–5 The risks of hypocoagulopathy is associated with prolonged bleeding or progression of hemorrhagic lesions, and this pathologic phenomenon may persist at least 48 h after injury.6
In the early stage of trauma, multiple system functions, such as coagulation, anticoagulation and fibrinolysis are unbalanced due to tissue injury, hypoperfusion, systemic inflammatory reaction and other factors, which makes it difficult for the body to maintain normal hemostatic function, resulting in coagulopathy.3,7 Coagulopathy is an important reason for the high incidence and progression of secondary injury caused by trauma, such as secondary intracranial hemorrhage, secondary cerebral infarction, deep vein thrombosis and discrete intravascular coagulation.8,9
It has been reported that the injury can induce a massive release of tissue factor into the systemic circulation, which leads to the activation of the extrinsic coagulation pathway. Moreover, platelet dysfunction, endogenous anticoagulation, endothelial activation, fibrinogen modification, inflammation, and hyperfibrinolysis can elicit increased and potentially severe bleeding,10,11 which plays a critical role in coagulopathy after TBI.8,12–14 There are few studies that have focused on the effect of coagulopathy on patients with TBI during the early postoperative period. Therefore, the purpose of the present study was to explore the risk factors and neurologic outcomes of coagulopathy in patients with TBI within 72 h after surgery.
Subjects and Methods
Patient Population
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Air Force Medical University (20194651). All patients or their legal guardians signed the informed consent. A total of 462 patients with TBIs who were treated in the Trauma Center of the Second Affiliated Hospital of Air Force Medical University between January 2015 and June 2019 were enrolled in this retrospective study. The clinical data and follow-up data of the patients were collected and retrospectively analyzed. Among the 462 patients, 143 developed coagulopathy within 72 h after surgery. Inclusion criteria: 18–70 years of age; Glasgow Coma Scale (GCS) ≤ 8; Abbreviated Injury Scale (AIS) head ≥ 3; extracranial AIS < 3; and craniectomy without preoperative coagulopathy. Exclusion criteria: isolated penetrating head injury; multiple-organ failure; time from injury to surgery >12 h; pregnancy; intravenous fluids or blood > 2000 mL before enrollment; preoperative coagulopathy; and craniotomy before admission.
Definitions
The indication for decompressive craniectomy was based on the 4th edition of TBI guidelines.15 All surgeries were performed by an associate chief surgeon with 12 years of experience. A head computed tomography (CT) scan was obtained at 0 h, 24 h, 72 h, and 5 days after surgery. An expanding contusion was diagnosed by comparison with the first head CT examination after surgery. Specifically, a follow-up CT scan that showed new lesions or increase in the original size of abnormalities > 33% or 12.5 mL was considered to signify an expanding contusion.16,17
The patients underwent coagulation testing at 2 h, 24 h, and 72 h after surgery. Coagulopathy was defined as an activated partial thromboplastin time (APTT) > 40 s, an international normalized ratio (INR) > 1.4, or platelet counts < 100×109/L. Standard treatment of coagulopathy was generally based on the administration of the following: tranexamic acid [10–20 mg/kg] within 3 h after the injury; red blood cells, plasma, and platelets in a 1:1:1 ratio; fresh frozen plasma [10–20 mL/kg]; platelets [5 mL/kg]; fibrinogen concentrate [30–50 mg/kg]; or cryoprecipitate [5–10 mL/kg].3
Neurologic Outcome Assessment
The neurologic outcomes were evaluated at 1 week, 3 months, and 6 months after surgery using mortality, the Glasgow Outcome Scale-Extended (GOS-E), and modified Rankin scale (mRS).
Statistical Analysis
SPSS 20.0 (SPSS, Inc., Chicago, IL, USA) and MedCalc (version 19.0.4; MedCalc, Inc., Mariakerke, Belgium) were used for statistical analysis. Continuous data with normal distribution are represented as the means ± standard deviation (SD) and analyzed by Student’s t-test for normal distributions. Continuous data with non-normal distribution are described as median (IQR) and analyzed using the non-parametric rank-sum test (Wilcoxon-W test). Categorical data are presented as frequencies and analyzed by a Chi-square test or Fisher's exact test. Variables with p < 0.05 were entered into multivariate regression analysis (F-to-enter set at zero) to identify the risk factors for coagulopathy and mortality in patients with postoperative TBI. To determine the area under the curve (AUC) for predicting coagulopathy in patients with TBI in the early postoperative period, we performed receiver operating characteristic curve analysis. The difference between the AUC values was compared using parametric Z test. A p-value <0.05 was considered statistically significant, and p values for multiple comparisons were adjusted using the Holm–Bonferroni correction.
Results
In the cohort of 462 patients with TBI, the incidence of coagulopathy within 72 h after surgery was 30.9%. Patients with coagulopathy had significantly lower GCS on admission (p < 0.001), higher ISS on admission (p = 0.006), unilateral mydriasis (p < 0.001), bilateral mydriasis (p = 0.005), duration of surgery (p = 0.046), contusion expansion within 24 h after surgery (p = 0.014), length of hospital stay (p < 0.001), intraoperative blood loss (p < 0.001), and an increased requirement for intraoperative crystalloid resuscitation (p < 0.001) than patients without coagulopathy after surgery (Tables 1 and 2).
 |
Table 1 Baseline Characteristics |
 |
Table 2 Intraoperative Fluid Management and Transfusion of Blood Components |
Multivariate logistic regression analysis revealed the association between patients with coagulopathy after surgery and GCS on admission (OR = 0.748; 95% CI = 0.647–0.866; p < 0.001), ISS on admission (OR = 1.058; 95% CI = 1.016–1.102; p = 0.007), unilateral pupil mydriasis (OR = 3.405; 95% CI = 2.032–5.703; p < 0.001), bilateral pupil mydriasis (OR = 4.947; 95% CI = 1.751–13.978; p = 0.003), duration of surgery (OR = 2.199; 95% CI = 1.853–2.610; p < 0.001), intraoperative blood loss (OR = 1.002; 95% CI = 1.001–1.002; p < 0.001), and intraoperative crystalloid resuscitation (OR = 1.004; 95% CI = 1.003–1.005; p < 0.001; Table 3).
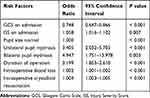 |
Table 3 Multivariate Logistic Regression for Risk Factors of Coagulopathy in Patients with TBI After Surgery |
There were statistical differences in mortality (p = 0.049), GOS-E (p = 0.024), and mRS (p = 0.043) between patients with coagulopathy and patients without coagulopathy 1 week after surgery (Table 4). Development of a coagulopathy within 72 h after surgery revealed a trend for higher mortality at 1 week (66.7%), 3 months (71.4%), and 6 months (76.2%), respectively (Table 5). Furthermore, univariate and multivariate analyses showed that coagulopathy within 72 h after surgery (OR = 2.438; 95% CI = 1.190–4.994; p = 0.015), contusion expansion within 24 h after surgery (OR = 16.643; 95% CI = 7.528–36.795; p < 0.001), contusion expansion between 24 and 72 h after surgery (OR = 8.365; 95% CI = 1.976–35.404; p = 0.004), and contusion expansion > 72 h after surgery (OR = 5.813; 95% CI = 2.025–16.684; p = 0.001) were the independent risk factors for mortality in patients with postoperative TBI (Tables 6 and 7).
 |
Table 4 The Neurologic Outcomes in Different Follow-Up Periods |
 |
Table 5 The Neurological Outcomes in Different Follow-Up Periods for Coagulopathy |
 |
Table 6 Univariate Analysis of Non-Survived Patients with Postoperative TBI |
 |
Table 7 Multivariate Analysis of Non-Survived Patients with Postoperative TBI |
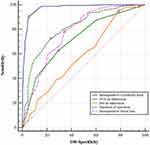
The AUC value for predicting the incidence of postoperative coagulopathy was 0.719 (95% CI = 0.676–0.760; p < 0.001) with a cut-off of 6.5 for GCS on admission, 0.589 (95% CI = 0.535–0.644; p = 0.002) with a cut-off of 11.5 for ISS on admission, 0.815 (95% CI = 0.773–0.856; p < 0.001) with a cut-off of 3.79 for the duration of surgery, 0.972 (95% CI = 0.957–0.986; p < 0.001) with a cut-off of 1650 mL for intraoperative crystalloid resuscitation, and 0.774 (95% CI = 0.732–0.817; p < 0.001) with a cut-off of 835 mL for intraoperative blood loss (Figure 1). There were statistical differences in the AUC values between intraoperative crystalloid resuscitation and GCS on admission (Z = 9.634, p < 0.001), ISS on admission (Z = 13.511, p < 0.001), duration of surgery (Z = 6.913, p < 0.001), and intraoperative blood loss (Z = 8.633, p < 0.001).
Discussion
Mounting evidence have identified the following independent risk factors for the development of acute coagulopathy after TBI: a GCS ≤ 8; pre-hospital intravenous fluid infusion ≥ 2000 mL; subarachnoid hemorrhage; and midline shift on CT imaging.1,2 In addition, patients with penetrating TBI have higher incidence of coagulopathy and higher mortality rate than patients with closed craniocerebral injury.18 Intravenous mannitol and hypertonic saline are routinely used to control intracranial hypertension in patients with severe TBI. However, a single bolus infusion of hypertonic fluids worsens hypocoagulability and hyperfibrinolysis in patients with hemorrhagic shock trauma.4 The present study demonstrated that some risk factors, such as GCS on admission, ISS on admission, and abnormal pupil size, can be used to assess the severity of brain injury after trauma and predict the occurrence of coagulopathy for patients with TBI within 72 h after surgery. Notably, preoperative bilateral mydriasis was a strong predictor of coagulopathy. Nevertheless, for severe TBI patients with or without coagulopathy, despite undergoing decompressive craniectomy, there are high mortality and disability rates.
In the setting of trauma or emergency surgery, intraoperative bleeding can be minimized with optimal preoperative preparation, but cannot be prevented completely. In this study, the duration of surgery (OR = 2.199) and intraoperative blood loss (OR = 1.002) were the independent risk factors for postoperative coagulopathy. It has been confirmed that shortening the duration of surgery, avoiding unnecessary blood loss, and reducing blood transfusion may help save the medical resources, reduce the medical costs, and decrease the mortality rate.19,20
The main goals of fluid therapy for patients with TBI are to optimize cerebral perfusion and maintain adequate cerebral oxygenation. The anesthesiologist may prefer rapid intraoperative fluid infusion to maintain blood pressure and cerebral blood flow stability when blood pressure decreases markedly after the induction of general anesthesia or relief of intracranial hypertension. Although we have confirmed that a large volume of intraoperative crystalloid resuscitation is an independent risk factor for patients with coagulopathy in the early postoperative period (OR = 1.004), there is still considerable controversy about fluid resuscitation for trauma patients. Shin et al21 have reported that the volume of intraoperative fluid administration (900–1100 mL) is consistently associated with optimal 30-day mortality, respiratory complications, acute kidney injury, and postoperative length of stay in adults undergoing non-cardiac surgery. Hahn et al22 have recommended the intraoperative administration of 3–5 mL/kg/h of crystalloids. However, additional fluid should be administered to patients who have more bleeding during surgery. Crystalloid resuscitation (>2000 mL) for patients with TBI is associated with increased mortality. Therefore, limited resuscitation before and after surgery may be indicated.23,24
A coagulopathy in TBI patients is strongly associated with progressive hemorrhagic injury. Approximately one-half of TBI patients with coagulopathy subsequently exhibit hemorrhagic progression of the initial brain contusions within 48 h.1 There were statistical differences in contusion expansion within 24 h between patients who did and did not develop coagulopathy 1 week after surgery in our research. Furthermore, coagulopathy within 72 h after surgery and contusion expansion during the early postoperative period were the independent risk factors for non-survival of patients with TBI. The research results conclusively prove that coagulopathy alone and contusion expansion secondary to a coagulopathy may be associated with increased mortality.
At different onset times, coagulopathy could lead to different mortality rates, and coagulopathy with early onset after injury and long duration is a marker for increased morbidity and poor outcomes.25 Carrick et al have reported that the incidence of coagulopathy is increased from 21% to 41% from the 1st to 3rd days in patients with TBI.6 Finally, the mortality rate is 62%, and the length of stay is increased by 1 day in such patients. In agreement with Solla et al26 and Yuan et al,27 we reported that coagulopathy within 72 h after surgery portended a higher mortality rate. Therefore, it is essential to prevent coagulopathy and shorten the duration of the coagulopathy to improve clinical neurologic outcomes.
There are also some limitations in our study. First, retrospective clinical study has a significant selection bias that might influence the results. Second, these data, including osmotic/diuretic drugs, fluid resuscitation, severe hypoxia or asphyxia, and blood loss in the pre-hospital emergency care, are not uniformly available for us to incorporate into the subgroup analysis. Third, traditional blood coagulation tests, as the most commonly used method to detect coagulation abnormalities, do not provide the status of platelets, fibrinogen function, and fibrinolysis in coagulation cascades. Indeed, thromboelastography could play an essential role in accurately diagnosing platelet dysfunction, fibrinogen deficiency, and hyperfibrinolysis.
Conclusion
Among TBI patients who develop coagulopathy within 72 h after surgery, there may be worse disease progression and unfavorable neurologic outcomes in the early postoperative period. Moreover, coagulopathy in long duration after surgery is associated with high mortality rate at different postoperative periods. Hence, we should implement practical and reasonable measures to prevent and manage those risk factors, which may protect TBI patients from developing coagulopathy after surgery.
Abbreviations
TBI, traumatic brain injury; GCS, Glasgow Coma Scale; AIS, Abbreviated Injury Scale; APTT, activated partial thromboplastin time; INR, International Normalized Ratio; GOS-E, Glasgow Outcome Scale-Extended; mRS, modified Rankin Scale; IQR, interquartile range; ISS, Injury Severity Score.
Ethics Approval and Informed Consent
All procedures performed in the study were in accordance with the ethical standards and approved by the Medical Ethics Committee of the Second Affiliated Hospital of Air Force Medical University (Grant number: 20194651). This study was conducted in accordance with the Declaration of Helsinki.
Consent for Publication
We have obtained the informed consent from all patients or their legal guardians.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the General Program of National Natural Science Foundation of China [Grant number: 81971186].
Disclosure
Tao Chang, Xigang Yan, Chao Zhao are co-first authors for this study. The authors declare that they have no competing interests.
References
1. Hoyt DB. A clinical review of bleeding dilemmas in trauma. Semin Hematol. 2004;41:40–43. doi:10.1053/j.seminhematol.2003.11.009
2. Maegele M. Coagulopathy after traumatic brain injury: incidence, pathogenesis, and treatment options. Transfusion. 2013;53(Suppl 1):28S–37S. doi:10.1111/trf.12033
3. Maegele M, Schochl H, Menovsky T, et al. Coagulopathy and haemorrhagic progression in traumatic brain injury: advances in mechanisms, diagnosis, and management. Lancet Neurol. 2017;16:630–647. doi:10.1016/S1474-4422(17)30197-7
4. Delano MJ, Rizoli SB, Rhind SG, et al. Prehospital resuscitation of traumatic hemorrhagic shock with hypertonic solutions worsens hypocoagulation and hyperfibrinolysis. Shock. 2015;44:25–31. doi:10.1097/SHK.0000000000000368
5. Greuters S, van den Berg A, Franschman G, et al. Acute and delayed mild coagulopathy are related to outcome in patients with isolated traumatic brain injury. Crit Care. 2011;15:R2. doi:10.1186/cc9399
6. Carrick MM, Tyroch AH, Youens CA, Handley T. Subsequent development of thrombocytopenia and coagulopathy in moderate and severe head injury: support for serial laboratory examination. J Trauma. 2005;58:725–729. doi:10.1097/01.TA.0000159249.68363.78
7. Harhangi BS, Kompanje EJ, Leebeek FW, et al. Coagulation disorders after traumatic brain injury. Acta Neurochir. 2008;150(2):165–175. doi:10.1007/s00701-007-1475-8
8. Frith D, Brohi K. The acute coagulopathy of trauma shock: clinical relevance. Surgeon. 2010;8(3):159–163. doi:10.1016/j.surge.2009.10.022
9. Davenport RA, Guerreiro M, Frith D, et al. Activated protein C drives the hyperfibrinolysis of acute traumatic coagulopathy. Anesthesiology. 2017;126(1):115–127. doi:10.1097/ALN.0000000000001428
10. Gando S, Hayakawa M. Pathophysiology of trauma-induced coagulopathy and management of critical bleeding requiring massive transfusion. Semin Thromb Hemost. 2016;42:155–165.
11. Yuan Q, Sun YR, Wu X, et al. Coagulopathy in traumatic brain injury and its correlation with progressive hemorrhagic injury: a systematic review and meta-analysis. J Neurotrauma. 2016;33:1279–1291. doi:10.1089/neu.2015.4205
12. Zia E, Engström G, Svensson PJ, et al. Three-year survival and stroke recurrence rates in patients with primary intracerebral hemorrhage. Stroke. 2009;40(11):3567–3573. doi:10.1161/STROKEAHA.109.556324
13. Rizoli SB, Scarpelini S, Callum J, et al. Clotting factor deficiency in early trauma-associated coagulopathy. J Trauma. 2011;71(5 Suppl 1):S427–S434.
14. Schmidt LB, Goertz S, Wohlfahrt J, et al. Recurrent intracerebral hemorrhage: associations with comorbidities and medicine with antithrombotic effects. PLoS One. 2016;11(11):e0166223. doi:10.1371/journal.pone.0166223
15. Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15. doi:10.1227/NEU.0000000000001432
16. Nasi D, Di Somma L, Gladi M, et al. New or blossoming hemorrhagic contusions after decompressive craniectomy in traumatic brain injury: analysis of risk factors. Front Neurol. 2018;9:1186. doi:10.3389/fneur.2018.01186
17. Anderson CS, Heeley E, Huang Y, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368:2355–2365. doi:10.1056/NEJMoa1214609
18. Folkerson LE, Sloan D, Davis E, et al. Coagulopathy as a predictor of mortality after penetrating traumatic brain injury. Am J Emerg Med. 2018;36:38–42. doi:10.1016/j.ajem.2017.06.057
19. Fullenbach C, Zacharowski K, Meybohm P. Improving outcome of trauma patients by implementing patient blood management. Curr Opin Anaesthesiol. 2017;30:243–249. doi:10.1097/ACO.0000000000000427
20. Goobie SM, Gallagher T, Gross I, Shander A. Society for the advancement of blood management administrative and clinical standards for patient blood management programs. (pediatric version). Paediatr Anaesth. 2019;29:231–236. doi:10.1111/pan.13574
21. Shin CH, Long DR, McLean D, et al. Effects of intraoperative fluid management on postoperative outcomes: a hospital registry study. Ann Surg. 2018;267:1084–1092. doi:10.1097/SLA.0000000000002220
22. Hahn RG. Adverse effects of crystalloid and colloid fluids. Anaesthesiol Intensive Ther. 2017;49:303–308.
23. Spahn DR, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:98.
24. Ko A, Harada MY, Barmparas G, et al. Limit crystalloid resuscitation after traumatic brain injury. Am Surg. 2017;83:1447–1452. doi:10.1177/000313481708301234
25. Lustenberger T, Talving P, Kobayashi L, et al. Time course of coagulopathy in isolated severe traumatic brain injury. Injury. 2010;41:924–928. doi:10.1016/j.injury.2010.04.019
26. Solla DJF, de Amorim RLO, Kolias AG, et al. Incremental prognostic value of coagulopathy in addition to the crash score in traumatic brain injury patients. Neurocrit Care. 2021;34(1):130–138. doi:10.1007/s12028-020-00991-7
27. Yuan Q, Yu J, Wu X, et al. Prognostic value of coagulation tests for in-hospital mortality in patients with traumatic brain injury. Scand J Trauma Resusc Emerg Med. 2018;26:3. doi:10.1186/s13049-017-0471-0
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.