Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Risankizumab for the Treatment of the Patients with Moderate to Severe Plaque Psoriasis During a 24-Week Period: Real-Life Experience
Authors Gönülal M , Balcı DD, Öztürkcan S
Received 19 October 2023
Accepted for publication 13 December 2023
Published 20 December 2023 Volume 2023:16 Pages 3653—3659
DOI https://doi.org/10.2147/CCID.S442427
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Anne-Claire Fougerousse
Melis Gönülal,1 Didem Didar Balcı,1 Serap Öztürkcan2
1Department of Dermatology, University of Health Sciences, Izmir Tepecik Training and Research Hospital, İzmir, Turkey; 2Department of Dermatology, Manisa Celal Bayar University Hafsa Sultan Hospital, Manisa, Turkey
Correspondence: Melis Gönülal, Email [email protected]
Introduction: Several authors have reported their experiences in real-world clinical practice, confirming the therapeutic efficacy of risankizumab in plaque psoriasis. We aimed to reflect our experience with risankizumab treatment in patients with psoriasis.
Materials and Methods: Patients who presented to the dermatology outpatient clinics of two tertiary care centers between November 2021 and August 2022, diagnosed with psoriasis and treated with risankizumab, constituted the target population. Data including gender, age, weight, type of psoriasis, affected body sites, disease duration, previous treatments, duration of risankizumab treatment, psoriasis area and severity index scores, comorbidities, the reasons for drug discontinuation, adverse effects, and the patients’ naïve or non-naïve status were obtained from electronic patient folders.
Results: Overall, 120 cases were included. While 73 (60.8%) cases were male, 47 (39.2%) were female. Eighty-six (68.3%) of all cases were biologic non-naive. A total of 49 patients (40.8%) had comorbidities. No significant correlations existed between biologic-naïve or non-naïve status, comorbidity status, and the PASI 75-90-100 responses.
Conclusion: Risankizumab is an effective treatment option for both biologic naive or non-naive patients with or without comorbidities. However, long-term studies, including more extensive patient series, are needed to validate its efficacy and safety in real-life clinical settings.
Keywords: psoriasis, risankizumab, anti-IL 23
Introduction
Psoriasis is an inflammatory skin disease affecting 125 million people worldwide. It has a complex pathogenesis involving several chemokines and cytokines such as IL-22, IL-23, tumor necrosis factor α (TNF-α), interferon α (IFN-α), interleukin (IL)-17A, other members of the IL-17 family.1–3 Risankizumab is a humanized immunoglobulin G1 (IgG1) monoclonal antibody used for treating plaque psoriasis. It selectively inhibits IL-23 by binding to its p19 subunit. Since IL-23 is involved mainly in T cell-mediated peripheral inflammation, its inhibition reduces the skin lesions in patients with psoriasis.4,5 The recommended treatment schedule necessitates subcutaneous injections of 150 mg (75 mg, BID) of risankizumab in the first week, the fourth week, and every 12 weeks afterward. Notably, this medication was confirmed by the US Food and Drug Administration in 2019 for treating adults with moderate-to-severe plaque psoriasis.6,7
Several authors confirmed its short-term and long-term effectiveness in plaque psoriasis in clinical settings. In this study, we report our clinical experience during a 24-week risankizumab treatment with psoriasis patients.
Materials and Methods
This study was conceived as a retrospective two-center study and accomplished under the ethical regulations of the Declaration of Helsinki. It was authorized by the University of Health Sciences Izmir Tepecik Training and Research Hospital Ethical Review Committee (09.12.2022/11-43). Patients who presented to the dermatology outpatient clinics of the University of Health Sciences, Izmir Tepecik Training and Research Hospital, and Manisa Celal Bayar University Hafsa Sultan Hospital between November 2021 and August 2022, diagnosed with psoriasis and treated with risankizumab comprised the target population of this retrospective cohort. The patients who were lost to follow-up were omitted. Both verbal and written informed consents were obtained from study participants. Data including age, gender, weight, psoriasis type, involved body areas, duration of disease, prior treatments, duration of risankizumab treatment, first psoriasis area and severity index (PASI) scores, and comorbid conditions were obtained from electronic patient folders. Data including the 5th, 12th, and 24th week PASI scores, time to reach the PASI75, PASI90, and PASI100 responses, the highest PASI scores, the causes for drug discontinuation, side effects and the patients’ naïve or non-naïve status were also present in these folders. These data were also retrieved.
Statistical analyses were conducted by the Statistical Package for Social Sciences (SPSS v.24.0, IBM) program. Descriptive data were given as means±standard deviations (SDs) and ranges [minimum–maximum]. The chi-square test was conducted to compare the categorical parameters. On the other hand, the independent samples t-test was used for comparing the normally distributed numerical data. The p values were considered significant when lower than 0.05.
Results
While 129 patients met the inclusion criteria, 9 were excluded due to incomplete data. Therefore, 120 cases were included. Among these patients, 73 (60.8%) were male and 47 (39.2%) were female. The mean patient age was 47.6±13.5 [18–79]; there was no significant difference between female and male patients regarding mean patient age (50±14.9 vs 46±12.4, p>0.05). The mean patient weight was 76.5±9.3 [55–115] kg. Male and female patients were also similar concerning mean patient weight (78.5±7.6 vs 73.4±10.8, p>0.05). The mean value for the first PASI was 11.1±5.3; 11.9±6 in females and 10.5±4.8 in males. Among all cases, 117 had plaque psoriasis, 2 had palmoplantar pustular psoriasis, and 1 had guttate and plaque psoriasis together. All patients had psoriasis on other sites (eg, scalp psoriasis, psoriatic arthritis, palmoplantar psoriasis, flexural psoriasis, nail psoriasis). At least 75% PASI score improvement was observed in 97 (80.8%) cases. Among these cases, 32 were female and 65 were male. On the other hand, no improvement was detected in 23 (19.2%) patients in the 12th week. While 15 of these patients were female, 8 were male. There were at least 90% PASI score improvements in 67 (55.9%) cases; among these cases, 16 were female, and 51 were male. Forty-nine (13 females, 36 males) patients showed a PASI score improvement of at least 100% (40.8%) in the 12th week. There were PASI score improvements of at least 75% in 116 (96.7%) cases (45 females and 71 males), while no improvement was noticed in 2 (1.7%) patients (2 females and 2 males) in the 24th week. In total, 111 (92.5%) cases showed at least 90% PASI score improvement in the 24th week. Among these patients, 42 were females and 69 were males. More than 100% PASI score improvement was detected in 100 (83.3%) cases in the 24th week. While 39 of these patients were females, 61 were males.
The review regarding comorbidities revealed that 49 (40.8%) patients had comorbid conditions, including cardiovascular disease, duodenal ulcer, dyslipidemia, diabetes mellitus, colon cancer, thrombocytopenia, multiple sclerosis, hypertension, hepatitis B seropositivity, and metabolic syndrome. Among the patients with comorbidities, 21 were females, and 28 were males. Risankizumab treatment was discontinued in 9 (7.5%) patients. In 5 cases, the discontinuation was due to the inefficiency of the drug, while non-adherence to the study protocol was the main reason in the remaining 4 cases. In 36 cases, risankizumab treatment was given after using one biological agent, while it was prescribed after using two biological agents in 17 patients. In addition, 2 patients used three biologics, 1 case four biologics, and another case five biologics before initiating the risankizumab treatment. No severe adverse effects were observed in any patients. The patient data are depicted in Tables 1–5 and Figures 1–3.
 |
Table 1 Information About the Patients and Medication of Risankizumab |
 |
Table 2 Information About PASI 75-90-100 Responses of All the Patients and Female and Male Patients Separately at Week 24 |
 |
Table 3 Comparison Between Male and Female Cases About Time to Reach PASI 75-90-100 Responses at Week 24 |
 |
Table 4 Comparision Between Naive and Non Naive Cases About PASI 75–90-100 Responses at Week 24 |
 |
Table 5 Comparision Between Comorbid and Non Comorbid Cases About PASI 75–90-100 Responses at Week 24 |
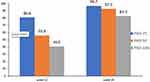 |
Figure 1 PASI responses of all cases at 12th and 24th weeks. |
 |
Figure 2 PASI responses of female patients at 12th and 24th weeks. |
 |
Figure 3 PASI responses of male patients at 12th and 24th weeks. |
Discussion
Our study showed that risankizumab was an effective and reliable therapeutic option for psoriasis patients. In our work, at the end of the 12th week, a PASI75 response was received in 80.8% of all cases (68% of females, 89% of males). We also found that while 55.9% (34% of females, 69.9% of males) of all patients achieved a PASI90 response, a PASI100 response was received in 40.8% of the cases (27.6% of females, 49.3% of males). In addition, at the end of the 24th week, 96.7% of all cases reached a PASI 75 response (95.7% of females, 97.3% of males). Of note, 92.5% of all patients achieved a PASI90 response (89.4% of females, 94.5% of males), and 83.3% of the cases reached a PASI100 response (83% of females and 83.6% of males). In the UltiMMa 1 trial, the authors reported that 75.3% of the patients reached the PASI90 response in the 16th week. On the other hand, the UltiMMa trial revealed that 74.8% of the patients achieved a PASI90 response at the same time interval. Of note, both of these trials were Phase 3 trials, and while 34.2% of the patients were biologic non-naïve in the former trial, 40.1% were biologic non-naïve in the latter. Severe adverse effects were observed in 2% of the cases in UltiMMa 1 and 2.4% of the patients in UltiMMa 2 trials.8,9 The IMMerge trial was conducted with 164 cases using risankizumab, 37.8% of whom were biologic non-naïve. In this study, 66% and 84% of the patients reached a PASI90 response at weeks 12 and 24. At week 12, 32% of the cases achieved a PASI100 response, while 56% reached a PASI100 response in 24 weeks. Severe adverse effects such as a major cardiovascular event (n=2), systemic infections (n=3), and malignancy (n=1) were detected in 6 patients.10,11 On the other hand, Gkalpakiotis et al,12 who reported their clinical experience on 154 patients, noted that 63.8% of their patients reached a PASI90 response at week 16 and 44.7% achieved a PASI 100 response during the same time interval. Notably, 61.7% of these cases were biologic non-naïve. These authors also denoted that 77.3% reached a PASI90 response, and 59.1% achieved a PASI 100 response at week 28. During this study, 1 patient with Morbus Morbihan disease developed colorectal cancer. In the work of Borroni et al,13 the data of 77 patients, of whom 39% were biologic non-naïve, were analyzed. This analysis revealed that 85.7%, 61%, and 28.6% of the patients reached PASI75, PASI90 and PASI100 responses, respectively. None of their cases experienced severe adverse events. Caldorola et al reviewed 112 cases in their study. In this cohort, 58% of the patients were biologic non-naïve. These authors noted that, at week 16, 90.7%, 72.2%, and 55.6% of their patients reached PASI75, PASI90 and PASI100 response, respectively. In our study, at week 28, we detected that 97%, 91%, and 75% of our patients reached a PASI75, PASI90 and PASI100 response, respectively.14 Also, we did not have to discontinue the risankizumab treatment due to any severe side effects of the medication. In the study of Elgaard et al15 PASI 75, PASI 90 and PASI 100 responses were determined as 66.7%, 55.6%, 38.9% at the end of follow up of 30 weeks. For risankizumab, both the PASI90 and PASI100 response rates in our study are higher than the response rates reported in the study of Bauvelt et al.16
In our study, at week 12, male patients’ PASI75, PASI90, and PASI100 responses were better than those of female cases. However, these responses were similar between male and female patients at week 24. In addition, we noted that the time to reach PASI75, PASI90, and PASI100 responses was shorter in female patients than in male patients. Also, there were significant correlations between female and male cases regarding the time to reach PASI90 and PASI100 responses (p= 0.005 and p<0.001).
Our study found no significant correlations between biologic naïve and biologic non-naïve cases concerning PASI 75-90-100 responses. In line with this, UltiMMa 1 and UltiMMa 2 trials concluded that biologic naïve and non-naïve patients achieved similar PASI 75-90-100 responses.10 In the IMMvent trial, which included 301 patients using risankizumab, 39% were biologic non-naïve. This study concluded that the patients re-randomized from adalimumab to risankizumab at week 16 could reach similar response rates reported in other phase 3 studies.17 Megna et al worked on 39 cases, of whom 94.9% were biologic non-naïve, while Hansel et al reviewed the data of 57 patients who completed a 16-week follow-up period.18,19 In the latter study, 41 (71.9%) patients were formerly treated with a biologic, and it was determined that prior biologic treatments did not significantly impact the study outcomes when the data of biologic-naïve and non-naïve patients were compared.19 In line with the abovementioned studies, our results indicated that risankizumab was a valuable treatment alternative for patients with moderate-to-severe psoriasis unresponsive to other biologics. These real-world results are important as patients with psoriasis have often tried multiple systemic biologics and non-biological therapies before initiating risankizumab.
Our study did not determine a significant correlation between patients with and without comorbid conditions regarding PASI 75-90-100 responses. This finding is consistent with the studies reported by Gkalpakiotis et al, Borroni et al, and Caldarola et al10–12 In their study, Gargiulo et al included 131 patients and found that risankizumab’s efficacy was unaffected by the patient’s body mass index and comorbidities.20 In addition, in our study, risankizumab showed no significant safety findings, and up to week 24, no relevant side effects were reported among all patients receiving risankizumab, in accordance with both the clinical trials and other real-life studies.8,18
In conclusion, our retrospective review confirmed the effectiveness and safety of risankizumab in clinical settings. These furthermore, it revealed that risankizumab was effective in both biologic-naïve and non-naïve patients with or without comorbid conditions. Studies with more extensive patient series and extended follow-up times are required to validate our results.
Funding
The authors have indicated they have no funding sources.
Disclosure
The authors have indicated they have no potential conflicts of interest to disclose.
References
1. Papp KA, Blauvelt A, Bukhalo M, et al. Risankizumab versus Ustekinumab for Moderate-to-Severe Plaque Psoriasis. N Engl J Med. 2017;376(16):1551–1560. doi:10.1056/NEJMoa1607017
2. Haugh IM, Preston AK, Kivelevitch DN, Menter AM. Risankizumab: an anti-IL-23 antibody for the treatment of psoriasis. Drug Des Devel Ther. 2018;12:3879–3883. doi:10.2147/DDDT.S167149
3. Cline A, Feldman SR. Risankizumab for psoriasis. Lancet. 2018;392(10148):616–617. doi:10.1016/S0140-6736(18)31781-1
4. Armstrong AW, Read C. Pathophysiology, Clinical Presentation, and Treatment of Psoriasis: a Review. JAMA. 2020;323(19):1945–1960. doi:10.1001/jama.2020.4006
5. Ruggiero A, Picone V, Martora F, Fabbrocini G, Megna M. Guselkumab, Risankizumab, and Tildrakizumab in the Management of Psoriasis: a Review of the Real-World Evidence. Clin Cosmet Invest Dermatol. 2022;15:1649–1658. doi:10.2147/CCID.S364640
6. Tokuyama M, Mabuchi T. New Treatment Addressing the Pathogenesis of Psoriasis. Int J Mol Sci. 2020;21(20):7488. doi:10.3390/ijms21207488
7. Gu C, Yang J. Risankizumab for the treatment of psoriasis. Expert Rev Clin Pharmacol. 2019;12(9):851–857. doi:10.1080/17512433.2019.1657829
8. Gordon KB, Strober B, Lebwohl M, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392(10148):650–661. doi:10.1016/S0140-6736(18)31713-6
9. Augustin M, Lambert J, Zema C, et al. Effect of Risankizumab on Patient-Reported Outcomes in Moderate to Severe Psoriasis: the UltIMMa-1 and UltIMMa-2 Randomized Clinical Trials. JAMA Dermatol. 2020;156(12):1344–1353. doi:10.1001/jamadermatol.2020.3617
10. Warren RB, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab vs. secukinumab in patients with moderate-to-severe plaque psoriasis (IMMerge): results from a Phase III, randomized, open-label, efficacy-assessor-blinded clinical trial. Br J Dermatol. 2021;184(1):50–59. doi:10.1111/bjd.19341
11. Crowley JJ, Langley RG, Gordon KB, et al. Efficacy of Risankizumab versus Secukinumab in Patients with Moderate-to-Severe Psoriasis: subgroup Analysis from the IMMerge Study. Dermatol Ther (Heidelb). 2022;12(2):561–575. doi:10.1007/s13555-021-00679-6
12. Gkalpakiotis S, Cetkovska P, Arenberger P. Risankizumab for the Treatment of Moderate-to-Severe Psoriasis: real-Life Multicenter Experience from the Czech Republic. Dermatol Ther (Heidelb). 2021;11(4):1345–1355. doi:10.1007/s13555-021-00556-2
13. Borroni RG, Malagoli P, Gargiulo L, et al. Real-life Effectiveness and Safety of Risankizumab in Moderate-to-severe Plaque Psoriasis: a 40-week Multicentric Retrospective Study. Acta Derm Venereol. 2021;101(11):adv00605. doi:10.2340/actadv.v101.283
14. Caldarola G, Zangrilli A, Bernardini N, et al. Risankizumab for the treatment of moderate-to-severe psoriasis: a multicenter, retrospective, 1 year real-life study. Dermatol Ther. 2022;35(6):e15489. doi:10.1111/dth.15489
15. Elgaard CDB, Iversen L, Hjuler KF. Guselkumab, tildrakizumab, and risankizumab in a real-world setting: drug survival and effectiveness in the treatment of psoriasis and psoriatic arthritis. J DermatolTreat. 2023;34(1):2133531. doi:10.1080/09546634.2022.2133531
16. Blauvelt A, Leonardi CL, Gooderham M, et al. Efficacy and safety of continuous risankizumab therapy vs treatment withdrawal in patients With moderate to severe plaque psoriasis: a phase 3 randomized clinical trial. JAMA Dermatol. 2020;156(6):649–658. doi:10.1001/jamadermatol.2020.0723
17. Reich K, Gooderham M, Thaçi D, et al. Risankizumab compared with Adalimumab in patients with moderate-to-severe plaque psoriasis (IMMvent): a randomised, double-blind, active-comparator-controlled phase 3 trial. Lancet. 2019;394(10198):576–586. doi:10.1016/S0140-6736(19)30952-3
18. Megna M, Potestio L, Ruggiero A, Camela E, Fabbrocini G. Risankizumab treatment in psoriasis patients who failed anti-IL17: a 52-week real-life study. Dermatol Ther. 2022;35(7):e15524. doi:10.1111/dth.15524
19. Hansel K, Zangrilli A, Bianchi L, et al. A multicenter study on effec- tiveness and safety of risankizumab in psoriasis: an Italian 16-week real-life experience during the COVID-19 pandemic. J Eur Acad Dermatol Venereol. 2021;35(3):e169–e170. doi:10.1111/jdv.17003
20. Gargiulo L, Ibba L, Pavia G, et al. Real-life effectiveness and safety of risankizumab in 131 patients affected by moderate-to-severe plaque psoriasis: a 52-week retrospective study. Dermatol Ther (Heidelb). 2022;12(10):2309–2324. doi:10.1007/s13555-022-00795-x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
