Back to Journals » Infection and Drug Resistance » Volume 13
Rifampicin-resistant Mycobacterium tuberculosis by GeneXpert MTB/RIF and Associated Factors Among Presumptive Pulmonary Tuberculosis Patients in Nepal
Authors Sah SK , Bhattarai PR, Shrestha A, Dhami D, guruwacharya D, Shrestha R
Received 20 May 2020
Accepted for publication 17 July 2020
Published 20 August 2020 Volume 2020:13 Pages 2911—2919
DOI https://doi.org/10.2147/IDR.S263795
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Shiv Kumar Sah,1 Pramod Raj Bhattarai,2 Anjana Shrestha,3 Deepak Dhami,3 Deepa guruwacharya,3 Renu Shrestha3
1Little Buddha College of Health Science, Purbanchal University, Minbhawan, Kathmandu, Nepal; 2National Tuberculosis Control Center, Bhaktapur, Nepal; 3Asian College for Advance Studies, Purbanchal University, Satdobato, Lalitpur, Nepal
Correspondence: Shiv Kumar Sah
Purbanchal University, Little Buddha College of Health Science, Minbhawan, Kathmandu, Nepal
Email [email protected]
Background: Mycobacterium tuberculosis(MTB) remains a major public health problem worldwide, and emergence of drug-resistant TB has become a significant obstacle to effective TB control. However, the rate of MTB and rifampicin resistant-MTB (RR-MTB) in the Nepalese setting has not been studied extensively. Therefore, the present study aims to assess the rate of MTB and RR-MTB and further determine the factors associated with it.
Methods: A retrospective cross-sectional study, among national representative data of 990 consecutive presumptive TB resister of patients subjected to the GeneXpert test that presented to the tuberculosis referral hospital, was conducted over a one year period from February 2018 to January 2019. Significance for the difference for categorical data was performed by Chi-square test and factors associated with MTB and RR-MTB were assessed using binary logistic regression yielding OR with 95%CI.
Results: Of total 990 presumptive tuberculosis analyzed cases, median ages of the patients were 39± 19.09 years and two-thirds of the patients were male 653 (66.0%). The estimated prevalence of MTB in presumptive TB patients was 13.8% (95%CI: 11.88%– 16.16%), and risk for MTB was significantly associated with previously treated patients: OR: 10.4 (P< 0.001). The estimated prevalence of RR-MTB in MTB confirmed patients was 10.2% (4.97%– 15.1%). Our study confirmed no association of RR-TB with age, sex, ethnicity, geographical diversity and previous history of treatment failure (P> 0.05).
Conclusion: The overall prevalence of MTB and RR-MTB was high in Nepalese study population, and that being previously treated with anti-TB drug remained significant predictors for MTB; proactive measures are urgently needed to address the challenge of prompt diagnosis, early management and improved monitoring of treatment to limit the emergence drug-resistant MTB strains in the community.
Keywords: MTB prevalence, RR-MTB prevalence, risk factors, Nepal
Introduction
Tuberculosis (TB) remains a major public health problem globally, accounting 10 millioncases (range: 9.0–11.1 million); surprisingly two-thirds represents the developing country.1 Moreover, in 2017, TB remained one of the top 10 causes of death and the leading cause from a single infectious agent, with an estimated 1.3 million deaths (range: 1.2–1.4 million), worldwide.1 Emergence of drug-resistant TB continues to be a significant public health crisis, and has further worsened the situation and become a significant obstacle to effective TB control.2 According to global tuberculosis reports, worldwide in 2017, 558,000 people (range: 483,000–639,000) developed TB that was resistant to rifampicin (RR-TB), the most effective first line drug, and of these, 82% had multidrug-resistant TB (MDR-TB). Globally, 3.5% of new TB cases and 18% of previously treated cases had MDR/RR-TB1
TB remains one of the leading public health problems in Nepal. According to the 2016/17 national tuberculosis programme, a total of 31,764 cases of TB were identified. The estimated annual incidence rate of all forms of TB is 111/100,000, whereas the incidence rate of new and relapse is 108/100,000 population.3
One of the greatest risk factors for drug-resistant TB is problems in treatment and diagnosis, especially in developing countries. If TB is identified and treated early, drug resistance can be avoided. The rapid detection of Mycobacterium tuberculosis (MTB) is crucial for early diagnosis and management of disease to minimize the high risk of disease transmission from person to person and emergence of MDR-TB. Xpert MTB/Rif assay, endorsed by WHO, is able to assess simultaneously detection of M. tuberculosis and rifampicin resistance mutation in the rpoB gene within two hours.4,5 The Xpert assay is highly rapid, sensitive and specific in diagnosis of both pulmonary and extra pulmonary tuberculosis.6–8 Additionally, it was shown to be cost-effective for TB diagnosis compared to microscopy in resource limited countries.9
Moreover, the prevalence of MTB and RR/MTB and its contributing factors described in literature vary largely across countries, which may also differ from Nepal. However, to date, the prevalence of MTB and RR-MTB has not been addressed extensively in the Nepalese setting. Therefore, the present study was aimed at assessing the rate of RR-MTB using the Xpert MTB/Rif assay, and further to identify the influencing factors associated with it.
Methods
Study Design
This was a retrospective cross-sectional study where data were evaluated retrospectively from the patients over a one year period from February 2018 to January 2019.
Study Setting
This study was conducted at National Tuberculosis Center (NTC), Bhaktpur Nepal. This is a referral governmental hospital where the referral patients from different health services across the country visit the hospital for diagnosis and treatment of the disease.
Outcome Variables
The core variable used for the study was MTB and RR-MTB. The covariates included in this study were: age, sex, ethnic group, geographic diversity, TB treatment history.
Study Population and Selection
Presumptive TB patients who visited NTCTuberculosis Center for the diagnosis and treatment of the disease, who met the inclusion criteria were enrolled in the study. To be eligible, all age groups with signs and symptoms suggestive of TB underwent the GeneXpert Rif/MTB assay test and smear test. Patients with insufficient demographic and clinical information were excluded from the study. A total 197 records of study participants who had no records of smear test were excluded from 1187 subjects, resulting in 990.
Data Collection
A structured questionnaire and checklist was used for the data collection. Patient’s demographic including age, sex, ethnicity, TB treatment history, geographic diversity and results of smear test for bacteriological presentation or not, rifampicin resistance using the GeneXpert/MTB assay was assessed retrospectively from the patient’s medical chart as well as from laboratory chart.
Laboratory investigation
From the respiratory specimen collected, acid fast bacilli microscopy and Xpert MTB/RIF assay was performed. If the presence of MTB was detected, GeneXpert was also used to look for evidence of rifampicin resistance.
From the sample, MTB bacilli was purified and concentrated by the Xpert MTB/RIF. Genomic material was isolated from the captured bacteria by sonication and the genomic DNA subsequently amplified by PCR. Furthermore, all the clinically relevant rifampicin resistance, inducing mutations in the rpoB gene in the MTB genome in a real-time format using fluorescent probes called molecular beacons were identified. Internal quality controls (sample processing control and probe check control) were used during the assay.
GeneXpert MTB/RIF Assay
GeneXpert analysis was performed in accordance to the protocol provided by its manufacturer (Cepheid, Sunnyvale, CA, USA), module GX-IV-4. Sputum specimens were used directly for the test. Briefly, the sample-reagent (SR) (Cepheid) was added at a 2:1 ratio to the sputum sample and incubated for 15 min at room temperature. The treated sample was shaken gently during incubation and then transferred into the cartridge.
Data Processing and Analysis
The data collected from TB registration book were entered into an excel spreadsheet and then exported to SPSS version 20 (IBM Corporation, Armonk, NY, USA) for analysis. Continuous data were presented as mean ±SD. Descriptive data were presented as frequency and percentage. Rifampicin resistance was the outcome variable. The association between the outcome variable test status and independent variables were computed using Chi-square test and where applicable Fisher’s exact test. Crude OR of associated factors (age, sex, ethnicity, geographic diversity) of the outcome variables was determined. Confidence interval was set at 95% and P value less than 0.05% considered to be statistically significant for all tests.
Ethical Aspects
Study protocol was approved by the NTC for commencement of the study. To ensure the confidentiality of the participants' information, data were anonymously used; and any other confidential information was highly secured. Since we used secondary data, informed consent was not sought from the study participants.
Results
The estimated prevalence of MTB among presumptive TB patients was 13.8%, with lower limit 11.88% and upper limit 16.16% (Table 1)
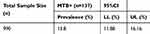 |
Table 1 Prevalence of Mycobacterium tuberculosis (MTB) |
Demographics and associations of MTB with sociodemographic parameters are presented in Table 2. This retrospective cross-sectional study was conducted among 990 presumptive tuberculosis cases. Median ages of the patients were 39±19.09 years (1–93), and two-thirds of the patients were male 653 (66.0%).
 |
Table 2 Demographics and Association of Sociodemographic Characteristics with Mycobacterium tuberculosis (MTB), and Bivariate Analysis of Risk Factors for Positive MTB |
Mean ages of MTB+ patients had lower positive finding compared to those of MTB– patients, without there being a significant difference (P>0.05). The highest positive finding for MTB 30 (14.78%) was observed in the age group above 60 years, whereas four (12.9%) MTB prevalent were reported in pediatric patients. Proportion of positive MTB was slightly higher in male 92 (14.08%) than female 45 (13.35%) patients. With respect to ethnicity, Dalit caste repreported to have the highest 10 (16.66%) rate of MTB. Patients residing in hilly regions appeared to have higher 104 (14.37%) positive findings of MTB. Categorical analysis for significance of association of MTB towards age, sex, ethnicity and geographical diversity was null (P>0.05). Proportion of MTB+ was significantly higher in previously treated patients 57 (50.00) compared to treatment-naïve patients 80 (9.13) (P<0.001), and the odds of developing MTB were significantly higher in previously treated patients: OR: 10.44 (95%CI: 6.77–16.12, P<0.001)
As shown in Table 3, the estimated prevalence of RR-MTB in TB-confirmed patients was 10.2%, with 4.97% lower level and 15.1% upper level.
 |
Table 3 Prevalence of Rifampicin-resistant Mycobacterium tuberculosis (RR-MTB) Among Presumptive Patients |
Association between RR-MTB and patient’s sociodemographic characteristics are illustrated in Table 4. Rate of rifampicin-resistant TB in the pediatric population was predominantly higher 1 (25%), compared to other ages groups, 15–39 years and 40–60 years, with 7 (10.60%) and 4 (10.81%) respectively. Female subjects had nearly twice 7 (15.55%) as many RR-TB as male 7 (7.60%) patients. With respect to ethnical group, proportion of RR-MTB was higher in Madhesi, Janjati and Dalit with 1 (16.66%), 12 (12.76%) and 1 (10.00%), respectively. Patients belonging to the Terai region had higher rate RR-MTB 3 (20.0%), compared to Himalayan 2 (11.11%) and hilly region 9 (8.65%). Proportion of RR-MTB was predominantly higher in previously treated patients 8 (13.79%), compared to treatment-naive patients 6 (7.50%). No significant association between RR-MTB and age, sex, ethnicity, geographical diversity and previous history of treatment failure was observed (P>0.05).
 |
Table 4 Association Between Sociodemographic Characteristics and Rifampicin Resistant MTB Among TB Confirmed Patients, and Bivariate Analysis of Risk Factors for RR-MTB |
Discussion
Rifampicin remains the most effective drug to treat TB, and the advent of resistance to it has had enormous impact on the TB-control program. Several epidemiological studies have attempted to unveil the impact and management of multidrug resistant-TB, however, little is known about the rifampicin-resistant TB, especially in Nepal. In this study several important findings were noted.
Studies around the world have reported a diverse magnitude of M. tuberculosis infection. In the present study the prevalence of M. tuberculosis was found to be 13.8% which is lower than the estimates of earlier studies, ranges from 15.4–25%, in different study settings.10–13 However, this estimate is lower compared to the previous reports in Mali (10%)14 and Mexico (7.5%).15 This variation could be explained by the difference in geographical variation, methods of diagnosis, study setting, or TB control practice.
The prevalence of M. tuberculosis among pediatric TB patients (12.9%) in the present study is comparable to the reports from South Africa (13%)16 and Uganda (14%).17 However, it is lower than a study conducted in Southwest Ethiopia (31.7%).18 Owing to different cut-off points for age groups applied in previous literature, it is difficult to make it comparable with ours regarding the association between MTB and age groups. Based on our study results, there was no significant association between age groups and MTB (P>0.05). The results of our study refute the association of an earlier study,12 where the age group stratified by <10 years 10–16 years, 17–23 years, 24–30 years, 31 to 37 years, 38–44 years, 45–51, 52–58 and >58 was significantly associated with MTB. Likewise, in a study conducted by Mulu et al, in Debre Markos referral hospital, Ethiopia,13 age group ≤10, 11–17, 18–30, 31–40, 41–50,51-60, and 61–92 was significantly associated with the patients with and without evidence of MTB (P<0.05). These variations across the studies could be attributed to the difference in sample size and difference in cut-off points for age groups.
Moreover, in agreement with the earlier studies,13,19,20 our study demonstrated a high rate of MTB, 66 (14.16) in age group 15–39 years. This might be due to more exposure in outer environment, high workload and wide range of mobility of this age group people to acquire the TB bacilli.
In this study, the detection rate of M. tuberculosis among male subjects (14.08%) was slightly higher than female subjects (13.35%). This is comparable with a study from Eastern Uttar Pradesh, India,21 a population-based prevalence survey of TB in the Tigray region of Ethiopia22 and a report from WHO.23 Although, the proportion of male MTB subjects were higher than female MTB, the difference was not significant (P>0.05), which also confirms the earlier study.12 However, in a study conducted by Mulu et al, in Debre Markos refferal hospital, Ethiopia,13 the proportion of MTB male subjects were significantly higher than MTB female subjects (P<0.05). This difference in sex incidence could be related to the social and health-seeking behavior difference, environmental factors, and tendency of higher exposure of males to the outer environment; smoking and alcoholism are different factors that pose a risk of acquiring the TB bacilli.23
There was a lack of association between MTB and age, sex, ethnicity, and geographic distribution and history of anti-TB drug (P>0.05). However, history of previous treatment failure was significantly correlated with MTB (P<0.001).
A study conducted in northwest Ethiopia revealed no significant association of MTB with sex and history of previous treatment failure. However, age, defined as stratified by <10, 10–16, 17–23, 24–30, 31–37, 38–44, 45–51, 52–58, and >58 years was significantly associated with MTB.12
Regarding treatment history, comparable results were reported by Gautam et al,21 in Eastern Uttar Pradesh India, in Debre Markos referral hospital, Ethiopia,13 and in Zimbabwe,24 where prevalence of MTB were significantly predominated in patients with previously treated cases compared to treatment-naive patients (P<0.05).
The existence of RR-MTB is a serious global health burden. RR-MTB is substantially high in low-income middle countries which may be attributed to its demographic and socioeconomic profile like poverty, lack of knowledge, poor practice, overcrowding, malnutrition, and care during illness and lack of social security. The overall prevalence of RR-MTB among TB confirmed cases was 10.2%. The prevalence of RR-MTB in this study is in line with previous studies reported in Ethiopia (10.3%),13 Nigeria (13.9%),25 and North India (10.5%).26 However, this figure is higher than that demonstrated in various parts of the world, with a prevalence of 2.5%,27 3.4%,10 5.7%,28 7.5%29 and is lower indicated in some region of Ethiopia 15.8–33.3%.12,27,30
The variation of RR-TB across the nation could be related to differences in patient selection, sample size (small sampling could generate high resistance rate), disparities in awareness of studied populations about drug resistance, access to health-care facilities, treatment and poor patient adherence.
With respect to the relationship between RR-MTB and age group, earlier study, conducted in referral hospital in Lagos, Nigeria, showed that being aged ≥45 years was independently associated with RR-TB.31 In the previous study conducted in India, age strata (01–20, 20–40, 40–60, 60–80) was significantly associated with RR-MTB.21 Report from Ethiopia indicated similar finding,10 where age 1–15, 16–30, 31–45, 46–60, >60 was significantly correlated with RR-TB. In comparison, Our study revealed no significant association between RR-MTB and age, which is also supported by one earlier study.32 The insignificant association between RR-MTB and age in this study in our study could be due to the difference in sample size and difference in cut-off points for age groups.
Regarding the association between sex and MTB, there are no conclusive reports. For instance; studies from Ethiopia,27,32 Georgia,33 and Russia34 have demonstrated that RR-MTB is associated with sex. However, in consonant with our study, study conducted by Jaleta et al in Northwest Ethiopia and Mulu et al in Debre Markos referral hospital Ethiopia revealed no significant association between RR-TB and sex.12,13 In the present study, proportion of RR-MTB in female was insignificantly higher than male counterpart (15.55% vs 7.60%). The high rate of RR-MTB among female subjects in our study could be explained by the socioeconomic factors (probably due to lack of control of financial resources at household levels) and delay in seeking health care in females. However, further study in a large population in the Nepalese setting should justify this possible association.
Studies across the countries have shown a substantial variation in the prevalence of RR-MTB in patients with previous anti-TB drug history and new cases. In the present study, the proportion of RR-MTB in previously treated cases (13.79%), which is higher than that reported in an earlier study (2.4%),35 and is lower compared to different study settings, 16.5%,12 (17.1%)13 27.4%.32 The proportion of RR-MTB in new cases in this study (7.59%) is in accordance with previous studies (6.7%),13 (7.6%),13 yet lower than that reported in earlier studies (13.0%),12 27.6%.36
Earlier studies have indicated a significant association between RR-MTB and history of anti-TB drugs, and have shown that RR-MTB is significantly higher in previously treated cases compared to new cases.13,32 In our study, although there was a lack of association between these variables, prevalence of RR-MTB in previously treated cases (13.79%) were higher compared to treatment-naïve patients (5.75%). The high prevalence of RR-MTB in previously treated cases patients suggest that previously treated patients were more likely to harbor drug-resistant strains, and is suggestive of weakness in TB prevention and control measures, as it is conveyed by resistance to rifampicin in new cases as well. This indicates that transmission of RR-MTB has a considerable role in this epidemic, and high frequency of treatment abandonment in earlier days may contribute toward high levels of resistance. Moreover, poor quality of anti-TB drugs used, inappropriate intake of medications and poor management of drug-sensitive TB could contribute to the higher rate of RR-MTB. A population-based survey which analyzed data from 11 countries demonstrated that the chance of developing resistant TB increased with the longer length of treatment as a result of treatment failure.37
In the present study, occurrence of MTB and RR-MTB were not significantly different among ethnic groups (Brahmin/Chhetri, Janjati, Madhesi, and Dalit) as well among the patients residing in different geographically diverse regions of the country (Himalayan, hilly, and Terai). Thus, the findings indicate that the ethnical groups and geographical diversity of the patients are not the contributing factors for the occurrence of MTB and RR-MTB. However, further supporting studies in a large representative population is needed to draw the conclusion.
Limitations
We acknowledge that this study was accomplished with some limitations. First, a lower rate RR-MTB in this study might have affected the results of logistic regression analysis for significance of association.
Second, although the study was conducted in a large sample size, this study was limited to the TB referral hospital in Bhaktpur, Nepal. Therefore, a larger nationwide study using the Xpert assay will provide a better estimate of RR-MTB in Nepal. Despite this limitation, this study became the first to demonstrate the rifampicin resistance in MTB using Xpert in Nepal which can be a further asset for planning of TB management and tackling further increase in the resistance.
Conclusion
Our study unveiled a high rate MTB in Nepalese presumptive TB patients. Occurrence of MTB was significantly associated with the history of anti-TB drugs, and previous treatment with anti-TB drug appeared to be independent predictors for MTB. Our study also demonstrated a high rate of RR-MTB among MTB confirmed patients, and high rate was observed in both previously treated patients and treatment-naïve patients. Thus, MTB and RR-MTB in our Nepalese setting remained an unresolved issue that needs to be addressed soon, and there is a need for improved monitoring of treatment to limit the spread of drug-resistant TB.
Abbreviations
MTB, Mycobacterium tuberculosis; NTC, Nepal Tuberculosis Center; RR-MTB, rifampicin-resistant Mycobacterium tuberculosis; TB, tuberculosis.
Data Sharing Statement
The datasets of the current study will be made available from the corresponding author on reasonable request.
Ethics Approval and Consent
Study protocol was approved by the Research Review Committee of Nepal Tuberculosis Center, Bhaktapur, Nepal.
Consent to Publish
Not applicable.
Acknowledgment
We express our sincere thanks to the Nepal Tuberculosis Center (NTC), Sanothimi, Bhaktapur, for granting us permission for this research, and also thank to the staff of the Department of Microbiology, NTC for their support in obtaining the patient lab reports and coordinating with us.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Global Tuberculosis Report-World Health Organization. Available from: https://apps.who.int/iris/bitstream/handle/10665//9789241565646-eng.pdf. Accessed September 26, 2018
2. Baqui AH, Black RE, El Arifeen S, et al. Effect of zinc supplementation started during diarrhoea on morbidity and mortality in Bangladeshi children: community randomised trial. BMJ. 2002;325(7372):1059. doi:10.1136/bmj.325.7372.1059
3. Saha K, Rao K. Undernutrition in lepromatous leprosy. V. Severe nutritional deficit in lepromatous patients co-infected with pulmonary tuberculosis. Eur J Clin Nutr. 1989;43(2):117–128.
4. Chang K, Lu W, Wang J, et al. Rapid and effective diagnosis of tuberculosis and rifampicin resistance with Xpert MTB/RIF assay: a meta-analysis. J Infect. 2012;64(6):580–588. doi:10.1016/j.jinf.2012.02.012
5. Lawn SD, Nicol MP. Xpert® MTB/RIF assay: development, evaluation and implementation of a new rapid molecular diagnostic for tuberculosis and rifampicin resistance. Future Microbiol. 2011;6(9):1067–1082. doi:10.2217/fmb.11.84
6. Tessema B, Beer J, Emmrich F, Sack U, Rodloff A. First-and second-line anti-tuberculosis drug resistance in Northwest Ethiopia. Int J Tuberculosis Lung Dis. 2012;16(6):805–811. doi:10.5588/ijtld.11.0522
7. Getahun M, Ameni G, Kebede A, et al. Molecular typing and drug sensitivity testing of Mycobacterium tuberculosis isolated by a community-based survey in Ethiopia. BMC Public Health. 2015;15(1):751. doi:10.1186/s12889-015-2105-7
8. Blakemore R, Story E, Helb D, et al. Evaluation of the analytical performance of the Xpert MTB/RIF assay. J Clin Microbiol. 2010;48(7):2495–2501. doi:10.1128/JCM.00128-10
9. Boehme CC, Nabeta P, Hillemann D, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010;363(11):1005–1015. doi:10.1056/NEJMoa0907847
10. Hordofa MW, Adela TB. Prevalence of Refampcin mono resistant Mycobacterium tuberculosis among suspected cases attending at Yirgalem hospital. Clin Med Res. 2015;4(3):75–78. doi:10.11648/j.cmr.20150403.13
11. Geleta DA, Megerssa YC, Gudeta AN, Akalu GT, Debele MT, Tulu KD. Xpert MTB/RIF assay for diagnosis of pulmonary tuberculosis in sputum specimens in remote health care facility. BMC Microbiol. 2015;15(1):220. doi:10.1186/s12866-015-0566-6
12. Jaleta KN, Gizachew M, Gelaw B, Tesfa H, Getaneh A, Biadgo B. Rifampicin-resistant Mycobacterium tuberculosis among tuberculosis-presumptive cases at University of Gondar Hospital, northwest Ethiopia. Infect Drug Resist. 2017;10:185. doi:10.2147/IDR.S135935
13. Mulu W, Abera B, Yimer M, Hailu T, Ayele H, Abate D. Rifampicin-resistance pattern of Mycobacterium tuberculosis and associated factors among presumptive tuberculosis patients referred to Debre Markos Referral Hospital, Ethiopia: a cross-sectional study. BMC Res Notes. 2017;10(1):8. doi:10.1186/s13104-016-2328-4
14. Banda H, Harries A, Welby S, et al. Prevalence of tuberculosis in TB suspects with short duration of cough. Trans R Soc Trop Med Hyg. 1998;92(2):161–163. doi:10.1016/S0035-9203(98)90727-1
15. Sánchez-Pérez H, Flores-Hernández J, Jansá J, Caylá J, Martín-Mateo M. Pulmonary tuberculosis and associated factors in areas of high levels of poverty in Chiapas, Mexico. Int J Epidemiol. 2001;30(2):386–393. doi:10.1093/ije/30.2.386
16. Nicol MP, Workman L, Isaacs W, et al. Accuracy of the Xpert MTB/RIF test for the diagnosis of pulmonary tuberculosis in children admitted to hospital in Cape Town, South Africa: a descriptive study. Lancet Infect Dis. 2011;11(11):819–824. doi:10.1016/S1473-3099(11)70167-0
17. Sekadde MP, Wobudeya E, Joloba ML, et al. Evaluation of the Xpert MTB/RIF test for the diagnosis of childhood pulmonary tuberculosis in Uganda: a cross-sectional diagnostic study. BMC Infect Dis. 2013;13(1):133. doi:10.1186/1471-2334-13-133
18. Workalemahu B, Berg S, Tsegaye W, et al. Genotype diversity of Mycobacterium isolates from children in Jimma, Ethiopia. BMC Res Notes. 2013;6(1):352. doi:10.1186/1756-0500-6-352
19. Deribew A, Negussu N, Melaku Z, Deribe K. Investigation outcomes of tuberculosis suspects in the health centers of Addis Ababa, Ethiopia. PLoS One. 2011;6(4):e18614. doi:10.1371/journal.pone.0018614
20. Yohanes A, Abera S, Ali S. Smear positive pulmonary tuberculosis among suspected patients attending Metehara sugar factory hospital; eastern Ethiopia. Afr Health Sci. 2012;12(3):325–330. doi:10.4314/ahs.v12i3.12
21. Gautam PB, Mishra A, Kumar S. Prevalence of rifampicin resistant mycobacterium tuberculosis and associated factors among presumptive tuberculosis patients in eastern Uttar Pradesh: a cross sectional study. Int J Community Med Public Health. 2018;5(6):2271–2276. doi:10.18203/2394-6040.ijcmph20182039
22. Berhe G, Enqueselassie F, Hailu E, et al. Population-based prevalence survey of tuberculosis in the Tigray region of Ethiopia. BMC Infect Dis. 2013;13(1):448. doi:10.1186/1471-2334-13-448
23. Zhou P, Yang X-L, Wang X-G, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi:10.1038/s41586-020-2012-7
24. Makamure B, Mhaka J, Makumbirofa S, et al. Microscopic-observation drug-susceptibility assay for the diagnosis of drug-resistant tuberculosis in Harare, Zimbabwe. PLoS One. 2013;8(2):e55872. doi:10.1371/journal.pone.0055872
25. Nwadioha S, Nwokedi E, Ezema G, et al. Drug resistant Mycobacterium tuberculosis in Benue, Nigeria. Br Microbiol Res J. 2014;4(9):988–995. doi:10.9734/BMRJ/2014/9084
26. Gupta A, Mathuria JP, Singh SK, Gulati AK, Anupurba S. Antitubercular drug resistance in four healthcare facilities in North India. J Health Popul Nutr. 2011;29(6):583.
27. Nigus D, Lingerew W, Beyene B, Tamiru A, Lemma M, Melaku M. Prevalence of multi drug resistant tuberculosis among presumptive multi drug resistant tuberculosis cases in Amhara National Regional State, Ethiopia. J Mycobac Dis. 2014;4(152):2161–1068.1000152. doi:10.4172/2161-1068.1000152
28. Hamusse SD, Teshome D, Hussen MS, Demissie M, Lindtjørn B. Primary and secondary anti-tuberculosis drug resistance in Hitossa District of Arsi zone, Oromia regional state, Central Ethiopia. BMC Public Health. 2016;16(1):593. doi:10.1186/s12889-016-3210-y
29. Tessema B, Beer J, Merker M, et al. Molecular epidemiology and transmission dynamics of Mycobacterium tuberculosis in Northwest Ethiopia: new phylogenetic lineages found in Northwest Ethiopia. BMC Infect Dis. 2013;13(1):131. doi:10.1186/1471-2334-13-131
30. Mulisa G, Workneh T, Hordofa N, Suaudi M, Abebe G, Jarso G. Multidrug-resistant Mycobacterium tuberculosis and associated risk factors in Oromia Region of Ethiopia. Int J Infect Dis. 2015;39:57–61. doi:10.1016/j.ijid.2015.08.013
31. Adejumo OA, Olusola-Faleye B, Adepoju V, et al. Prevalence of rifampicin resistant tuberculosis and associated factors among presumptive tuberculosis patients in a secondary referral hospital in Lagos Nigeria. Afr Health Sci. 2018;18(3):472–478. doi:10.4314/ahs.v18i3.2
32. Arega B, Menbere F, Getachew Y. Prevalence of rifampicin resistant Mycobacterium tuberculosis among presumptive tuberculosis patients in selected governmental hospitals in Addis Ababa, Ethiopia. BMC Infect Dis. 2019;19(1):307. doi:10.1186/s12879-019-3943-1
33. Toungoussova O, Caugant D, Sandven P, Mariandyshev A, Bjune G. Drug resistance of Mycobacterium tuberculosis strains isolated from patients with pulmonary tuberculosis in Archangels, Russia. Int J Tuberculosis Lung Dis. 2002;6(5):406–414.
34. Lockman S, Kruuner A, Binkin NJ, et al. Clinical outcomes of Estonian patients with primary multidrug-resistant versus drug-susceptible tuberculosis. Clin Infect Dis. 2001;32(3):373–380. doi:10.1086/318489
35. Yang Y, Zhou C, Shi L, Meng H, Yan H. Prevalence and characterization of drug-resistant tuberculosis in a local hospital of Northeast China. Int J Infect Dis. 2014;22:83–86. doi:10.1016/j.ijid.2013.12.015
36. Sethi S, Mewara A, Dhatwalia SK, et al. Prevalence of multidrug resistance in Mycobacterium tuberculosis isolates from HIV seropositive and seronegative patients with pulmonary tuberculosis in north India. BMC Infect Dis. 2013;13(1):137. doi:10.1186/1471-2334-13-137
37. Espinal MA, Laserson K, Camacho M, et al. Determinants of drug-resistant tuberculosis: analysis of 11 countries. Int J Tuberculosis Lung Dis. 2001;5(10):887–893.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
