Back to Journals » Open Access Surgery » Volume 15
Retrospective Analysis of Inguinal Hernia in Pediatric Patients in a Tertiary Center, Addis Ababa, Ethiopia
Authors Tigabie W , kiflu W, Temesgen F, Getachew H, Nigussie T, Dejenie B , Tadesse A, Derbew M
Received 22 June 2021
Accepted for publication 10 February 2022
Published 24 February 2022 Volume 2022:15 Pages 9—15
DOI https://doi.org/10.2147/OAS.S324618
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Luigi Bonavina
Workye Tigabie,1 Woubedel Kiflu,2 Fisseha Temesgen,2 Hanna Getachew,2 Tihitena Nigussie,2 Belachew Dejenie,2 Amezene Tadesse,2 Miliard Derbew2
1Department of Surgery, St. Peter Specialized Hospital, Addis Ababa, Ethiopia; 2Department of Surgery, Pediatrics Surgery Unit, Tikur Anbessa Hospital, Addis Ababa, Ethiopia
Correspondence: Workye Tigabie, Email [email protected]
Background: Inguinal hernia is one of the most frequent reasons for referral to the pediatric surgery unit. The incidence ranges from 1% to 5% in the pediatric population. Surgery for inguinal hernia is among the most commonly performed procedures, with good overall outcomes and few complications.
Objective: The study aimed to evaluate the pattern and outcome of inguinal hernia surgery in children.
Methodology: This retrospective 5-year cross-sectional study was conducted on all pediatric patients with inguinal hernia (age < 13 years) operated on between September 1, 2014, and August 31, 2019, in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia.
Results: The male to female ratio of inguinal hernia was 19:1. It was slightly more predominant on the right side and bilaterality occurred in about 10.6% of cases. The mean age at presentation was 15 months, and the average waiting time for patients to be operated on was 5 months. The overall incarceration and strangulation rates were 24% and 3.8%, respectively. Infants had a higher risk of incarceration/strangulation than other children. Among patients who underwent elective surgery, 63% (53/84) of operations were carried out as day-case surgery. The overall mortality, complication rate, and recurrence risk following surgery were 0.9%, 11.5%, and 9.6%, respectively. Bilaterality increased the occurrence of late postoperative complications.
Conclusion: All inguinal hernia cases were indirect hernias operated on by standard open surgical techniques. Our study showed increased incarceration rates, recurrences, and complications after surgery. This is because of the delayed presentation of patients and delayed intervention for patients. Therefore, early and timely intervention with proper surgical techniques should always be considered.
Keywords: inguinal hernia, incarceration, outcome, pattern, day-case surgery
Introduction
Inguinal hernia repair is one of the most commonly performed operations and it is among the most frequent reasons for referral to pediatric surgery clinics. The incidence of inguinal hernia is 1–5% in the pediatric population and is even higher in premature babies, as high as 10–30%.1–9 Inguinal hernias were described before 1550 BC. However, modern surgery began in the late nineteenth century with the more accurate understanding of the anatomy.2 Inguinal hernias in children are due to a persistent processus vaginalis in 99% of indirect cases. However, direct inguinal and femoral hernias can rarely exist, in about 0.5–1% of cases.2,7,10
Diagnosis is made according to clinical history and physical examination, with the classic clinical feature of a bulge or lump that transmits a cough impulse, often with crying.2,4 Imaging, especially ultrasonography, is useful for doubtful and less clear-cut clinical presentations.2,4,7 Surgery is indicated for all patients diagnosed with an inguinal hernia to avoid the risk of incarceration and strangulation of the bowel, gonadal infarction, and atrophy.1–4,7,11–13 The risk of incarceration in most patients generally ranges from 3% to 16%, and infants are at relatively high risk.1–4,7,11–13 Complications of hernia are associated with significant morbidity, higher mortality, and increased overall hospital stay.1,2,6,7
It is commonly advised to operate on inguinal hernia within 10 days of diagnosis, and 48 hours after successful reduction of incarceration, to achieve good results.4,11,14
Either standard open or laparoscopic techniques can be used to repair inguinal hernias. Both techniques have shown comparable outcomes in most studies.4,7,9,11,14 Contralateral inguinal exploration in children is an area of active debate and, as yet, there is no consensus.4,7,9,11,14
No similar study was found in Ethiopia and only limited literature of its kind is reported in most other African countries. Therefore, this study, conducted in the biggest tertiary specialized hospital of the country, will serve as a baseline work for other researchers, especially for those in developing nations who are interested in working on further studies on this topic.
Methods and Materials
A 5-year retrospective cross-sectional study in all children diagnosed with inguinal hernia (age <13 years) was conducted from September 1, 2014, to August 31, 2019, in Tikur Anbessa Specialized Hospital (TASH), Addis Ababa, Ethiopia. The data needed for this research were collected by reviewing the patients’ charts using a checklist developed for this study. The collected data were coded and entered into EpiData version 3.1. The cleaned data were exported to SPSS version 23.0 software and analyzed. Chi-squared and Fisher’s exact tests were used to report outcomes stratified by patient characteristics. Logistic regression was also used to identify patient variables associated with outcomes.
Inclusion Criteria
All children diagnosed with inguinal hernia (aged <13 years) were eligible for inclusion, regardless of the condition of the child.
Ethical Considerations
As patient charts contain vital information regarding patients’ demographic factors and general health status, proper chart handling was given priority. All charts taken from the chart store for the study were returned in a timely and proper manner. The proposal of this study was reviewed and approved by the relevant ethical committee of the college on May 20, 2019.
Results
A total of 129 inguinal hernia surgeries were carried out in the study period, of which 104 were included in the study, giving the study a retrieval rate of 80.6%.
Socio-Demographic Characteristics
A total of 104 study cases that fulfilled the inclusion criteria were selected based on a retrospective medical card review (from September 1, 2015 to September 1, 2019). Among all patients, 99 (95.2%) of the study participants were males and five (4.8%) were females. Most of our patients, 42 (40.4%), were infants less than 3 months of age. The age range at presentation was 1 day to 12 years, with a mean of 15 months (SD 27). Most of the infants, 66 (63.5%), were delivered at term (Table 1).
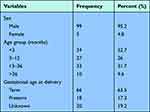 |
Table 1 Socio-Demographic Factors in Patients Operated on for Inguinal Hernia, TASH, Addis Ababa, Ethiopia |
Clinical Profile of Inguinal Hernia
All patients were symptomatic at the time of diagnosis. Altogether, 46% of (n=48) of the hernia cases occurred on the right side, 43.2% (n=45) occurred on the left side, and there were 11 (10.6%) cases of bilaterality. All of our study patients were found to have an indirect inguinal hernia. The average age at diagnosis was 15 months (range 1 days to 12 years). About 16.3% (n=17) of patients had associated hydrocele detected clinically or by ultrasonography. Most 103 (99%) patients had a radiologic diagnosis. Only one patient was not subjected to radiologic diagnosis. Only 18 patients (17.3%) had associated anomalies, the most common of which were hydrocephalus, bladder exstrophy, VACTERL (vertebral, anorectal, cardiac, tracheoesophageal, renal, and limb anomalies), and isolated cardiac anomalies. Only one (1%) of the study patients had a family history that affected his sibling. The mean waiting time for surgery was 5.25 months (range 0–72 months).
Surgical Profile of Inguinal Hernia
All patients were operated on by a standard open technique. Only 19.2% of patients (n=20) underwent the operation on an emergency basis. In most of the elective cases, 63% (n=53) were operated on as daycare surgery, while the remaining 36.9% (n=31) needed admission because of the associated comorbid conditions or premature gestational age, or because they had immediate complications related to the anesthesia.
Most of the patients underwent hernia repair during the age of infancy (Table 2). The average time interval between diagnosis and surgery was 5 months and the waiting time ranged from 0 to 72 months. About 29% of patients (n=30) developed preoperative complications. The overall rates of incarceration and strangulation were 24% and 3.8%, respectively. The rate of complication before surgery was higher in the infant age group compared with those above infantile age (p<0.007). There was no record of more than one attack of incarceration.
 |
Table 2 Factors Associated with Preoperative Hernia Complications Among Patients Operated on for Inguinal Hernia in TASH |
The mean time interval between diagnosis and preoperative complications (incarceration/strangulation) was 73 days (SD 273). The types of treatment for incarceration were emergency surgery with/without an attempt at manual reduction, which accounted for 60% (15/25), manual reduction and operation at the same admission, 32% (8/25), and manual reduction and then discharge for delayed surgery, 8% (2/25). All patients were operated on under general anesthesia. The contents of the hernia found during surgery were small bowel in 95 cases (91.3%), appendix in six (5.8%), ovary and tube in one (1%), sigmoid colon in one (1%), and omentum in one patient (1%). External inguinal canal opening was required in 21 cases (21.6%). The techniques of hernia repair were simple high ligation of the sac for 98 patients (94.2%) and tightening of the deep inguinal ring for six patients (5.8%). The type of stitch used was all absorbable Vicryl and the wound closure technique was subcuticular in all cases. No contralateral exploration was carried out. Imaging ultrasonography was not performed for two patients (1.9%). The mean duration of surgery in patients with unilateral hernias was 56.0 minutes (range 15–170 minutes), while the mean duration of surgery in those with bilateral hernias was 89.0 minutes (range 50–160 minutes). The median duration of anesthesia was 77 minutes (range 25–300 minutes).
Only 15 patients (14.4%) received caudal anesthesia; in most of the remaining patients, pain management was achieved by acetaminophen/and NSAIDs.
Outcome and Associated Factors
Immediate complications occurred in four patients (3.8%). These complications were apnea in one patient (1%), spasm in one (1%), bradycardia in one (1%), and immediate recurrences in one patient (1%). These complications were associated with anesthesia, except for the immediate recurrence, which was related to technical error.
There were eight cases of late postoperative complications and two patients required admission. Bilaterality increased the occurrence of late complications (Table 3). The wound infection rate was 1.9% (2/104 procedures). The wound infections were generally minor and required no admission. Testicular atrophy occurred in one patient (1%) following strangulation, which required resection of the gangrenous ileum, and there was decreased flow at the testis at the time of presentation, which later required orchiectomy after 2 years of follow-up.
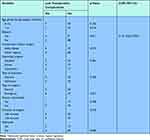 |
Table 3 Factors Associated with Patient Outcome Among Patients Operated on for Inguinal Hernia in TASH |
There was one case of contralateral hernia, detected 10 months after the initial right-sided hernia repair. A 9.6% (n=10) rate of recurrence of inguinal hernia was found in this study throughout follow-up. The mean duration of recurrence was 4 months (range 1 month to −12 months). The overall mortality rate was 0.9% (n=1), in a patient who had severe pulmonary hypertension, who underwent operation on an elective basis and died in the early postoperative period.
Discussion
Inguinal hernia is one of the commonest surgical problem in children. The incidence of inguinal hernia is 1–5% in the pediatric population and is even higher in premature babies, being as high as 10–30%.1–9 Timely repair of these hernias is recommended to reduce the risk of incarceration, strangulation, and overall morbidity and mortality.1,2,4–7,11,14,15 In this study, inguinal hernia affected many more males than females, in a ratio of 19:1. This is a known fact and consistent with other similar studies.5,7,8,13,16,17 Among all patients, infants less than one year of age accounted for about 58.7% (n=61) of the cases, which is a higher proportion than reported in other countries.5,6,18
The age range at presentation varied from 1 day to 12 years, with a mean age of 15 months, which is lower than the mean ages reported in other studies.5,16 This is because some patients will present late, assuming spontaneous closure of the hernia.
Associated hydrocele was detected in 17% of patients, which is higher than in a report by Himanshu Acharya et al in India.7 This is reasonable because we had a higher ratio of patients younger than one year of age, in whom the incidence of hydrocele is likely to be higher. Our study, unlike most others in the literature, found no significant difference in the occurrence of hernia in terms of location, with a right- to left-side ratio of 1.07:1.5–8,16,18 There was 10.6% bilaterality of hernia, which is similar to reports in studies by Himanshu Acharya et al and Ezomike et al,7,13 and lower than that reported in a study by Alrzoq et al.16 Among all patients, 28.8% (30/104) of cases presented with a hernia complication which required emergency surgery. Therefore, the overall incarcerations and strangulation rates in our study were 24% and 3.8%, respectively. This agrees with a report from west Ghana by Ohene-Yeboah and Abantanga,12 and is higher than in studies by Nick Zavras et al, Himanshu Acharya et al, and Gupta and Rohatgi.7,9,18 The rate of complications before surgery was higher in the infant age groups compared with above-infant age groups (p<0.007). This corresponds to a study by Wenk et al in Switzerland.11 Regarding intraoperative details in our study, opening of the inguinal canal was required in 21.6% (21/104) of cases and tightening of the ring was carried out in six patients (5.6%). The mean duration of surgery in patients with unilateral hernias was 56.0 minutes (range 15–170 minutes) while the mean duration of surgery in those with bilateral hernias was 89.0 minutes (range 50–160 minutes). This is slightly higher than reports from other studies by Ciro Esposito et al and Usang et al.4,5
The results on the contents of the hernia sac were no different from those previously reported by Ciro Esposito et al and Nick Zavras et al.4,9
There was no contralateral exploration done in our study. However, some literature recommends contralateral exploration, especially for female infants less than 6 months old and for left-sided hernias.4,7,9,11,14 In our study, among all patients operated on for inguinal hernia, only 3.8% (n=4) and 7.7% (n=8) of patients developed early and late postoperative complications, respectively. This is lower than reported by Gahukamble and Khamage and by Mabula and Chalya.6,17 Bilaterality was the only factor statistically significant associated with the occurrence of late complications (p=0.01). The wound infection rate was 1.9% (2/104), which is slightly higher than in the studies by Ciro Esposito et al and Himanshu Acharya et al.4,7 Our study also revealed that there were 9.6% (n=10) cases of recurrence of inguinal hernia that were found during the follow-up. This is higher than in reports from western countries.4,7,8,16 This high rate may be because of the lack of sufficiently high ligation of the sac or early interference following incarcerated bowel reduction. There was one case of contralateral hernia detected 10 months after the initial right-sided hernia repair during the study period, giving an incidence rate for metachronous contralateral inguinal hernia (MCIH) of 0.9%. This is lower than in other studies.9,11,14 Among all patients operated on for inguinal hernia, only one patient, who had underlying cardiac disease, died in the early postoperative period, giving an overall mortality rate of 0.9% (n=1), which is consistent with most studies in the literature and in a textbook on pediatric surgery.2,19
Strength of the Study
Our study is the first comprehensive study on this specific topic in children in Ethiopia. It provides an important baseline for future work within resource-limited settings like those of sub-Saharan Africa.
Limitations of the Study
This was a single-center, retrospective study, with a limited number of patients. Therefore, prospective studies are encouraged.
Conclusion
All inguinal hernia cases were operated on using a standard open surgical technique.
Surgical treatment should be offered in a timely manner to prevent possible complications and minimize associated morbidities and mortality. Infants in particular are at increased risk of incarceration and it would be wise to consider operating on them soon, subject to available waiting lists. Our study showed a relatively high incidence of patients presenting with complications, recurrences, and postoperative complications. This is because of the delayed presentation of patients and delayed intervention for patients. Therefore, early and timely intervention with proper surgical techniques should always be considered.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The ethics committee that approved the study is Addis Ababa University, College of Health Sciences Institutional Review Board. The board also waived the requirement for consent to participate. This study was conducted in accordance with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Suad Gholoum RB, Laberge J-M, Puligandla PS. Incarceration rates in pediatric inguinal hernia: do not trust the coding. J Pediatr Surg. 2010;45:1007–1011. doi:10.1016/j.jpedsurg.2010.02.033
2. Holcomb GW
3. Steven L, Lee JMG, Sydorak RM. A critical review of premature infants with inguinal hernias: optimal timing of repair, incarceration risk, and postoperative apn. J Pediatr Surg. 2010;9:46.
4. Ciro Esposito M, Escolino M, Turrà F, et al. Current concepts in the management of inguinal hernia and hydrocele in pediatric patients in laparoscopic era. Semin Pediatr Surg. 2016;25(4):232–240. doi:10.1053/j.sempedsurg.2016.05.006
5. Usang UE, Sowande OA, Adejuyigbe O, et al. Day case inguinal hernia surgery in Nigerian children: prospective study. Afr J Paediatric Surg. 2008;5(2):76. doi:10.4103/0189-6725.44181
6. Gahukamble D, Khamage A. Early versus delayed repair of reduced incarcerated inguinal hernias in the pediatric population. J Pediatr Surg. 1996;31(9):1218–1220. doi:10.1016/S0022-3468(96)90235-3
7. Himanshu Acharya RA, Agrawal V, Abhishek T, Chanchlani R. Management of inguinal hernia in children: a single center experience of 490 patients. Int Surg J. 2016;3(1):346.
8. Olatoregun DG, Olatoregun Frank BO. Review of inguinal hernia surgeries performed in Nigerian Children. IOSR J Dental Med Sci. 2014;13:6.
9. Nick Zavras AC, Misiakos E, Salakos C, et al. Current trends in the management of inguinal hernia in children. Int J Clin Med. 2014;5:770.
10. Ameh EA, Bickler SW, Lakhoo K, Nwomeh BC, Poenaru D. Pediatric Surgery - a Comprehensive Text Book for Africa; 2010:
11. Wenk K, Sick B, Sasse T, Moehrlen U, Meuli M, Vuille-dit-Bille RN. Incidence of metachronous contralateral inguinal hernias in children following unilateral repair — a meta-analysis of prospective studies. J Pediatr Surg. 2015;50:
12. Ohene-Yeboah M, Abantanga F. Inguinal hernia disease in Africa: a common but neglected surgical condition. West Afr J Med. 2011;30(2):77–83.
13. Ezomike U, Ekenze S, Amah C. Irreducible inguinal hernias in the paediatric age group. Nigerian J Med. 2013;22(3):230–233.
14. Ron O, Eaton S, Pierro A. Systematic review of the risk of developing a metachronous contralateral inguinal hernia in children. Br J Surg Soc. 2007;94:804–811.
15. Ohene-Yeboah M, Abantanga FA. Inguinal hernia disease in Africa: a common but neglected surgical condition. West Afr J Med. 2011;30:77–83.
16. Alrzoq RA, Alhaji AMA, Alolayt IYI, et al. The incidence of inguinal hernia among children. Egypt J Hosp Med. 2018;70(3):483–486. doi:10.12816/0043492
17. Mabula JB, Chalya PL. Surgical management of inguinal hernias at Bugando Medical Centre in northwestern Tanzania: our experiences in a resource-limited setting. BMC Res Notes. 2012;5(1):585. doi:10.1186/1756-0500-5-585
18. Gupta D, Rohatgi M. Inguinal hernia in children: and Indian experience. Pediatr Surg Int. 1993;8(6):466–468. doi:10.1007/BF00180345
19. Ameh EA. Morbidity and mortality of inguinal hernia in the newborn. Niger Postgrad Med J. 2002;9(4):233–234.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
