Back to Journals » Clinical Interventions in Aging » Volume 18
Retrograde Approach via Ipsilateral Septal Collateral Channel in Percutaneous Coronary Intervention for Coronary Chronic Total Occlusion: A Single-Center Experience
Authors Deng X, Zhong X, Nie B, Wang R, Lu H, Ge L, Qian J, Ma J, Ge J
Received 3 February 2023
Accepted for publication 2 May 2023
Published 11 June 2023 Volume 2023:18 Pages 933—940
DOI https://doi.org/10.2147/CIA.S404818
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Maddalena Illario
Xin Deng,1,* Xin Zhong,1,* Bin Nie,2 Ruochen Wang,1 Hao Lu,1 Lei Ge,1 Juying Qian,1 Jianying Ma,1 Junbo Ge1
1Department of Cardiology, Zhongshan Hospital, Fudan University, Shanghai Institute of Cardiovascular Diseases, National Clinical Research Center for Interventional Medicine, Shanghai, People’s Republic of China; 2The Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Junbo Ge; Jianying Ma, Email [email protected]; [email protected]
Background: The septal collateral channel (CC) is the preferred channel in retrograde percutaneous coronary intervention (PCI) for chronic total occlusion (CTO). However, reports on the utilization of the ipsilateral septal CC are limited.
Objective: To evaluate the feasibility and safety of the ipsilateral septal CC in retrograde CTO PCI.
Methods: Twenty-five patients with successful wire CC tracking via the ipsilateral septal CC in retrograde CTO PCI were retrospectively analyzed. All procedures were performed by experienced CTO operators. Procedures were divided into the left descending coronary artery (LAD)-septal-LAD group and the LAD-septal-left circumflex coronary artery (LCX) group. Procedural complications and in-hospital outcomes were ascertained.
Results: Both groups were similar with respect to risk factors and angiographic characteristics of the CTO, except for the collateral tortuosity (86.7% vs 20%, p=0.002). The success rate of microcatheter CC tracking was 96%. Both technical success and procedural success rates were 92%. Procedural complications were found in one case (septal perforation, 4%), which happened in the LAD-septal-LAD group (p=0.250). One postoperative adverse event (Q-wave myocardial infarction, 4%) was observed before discharge.
Conclusion: The retrograde approach via the ipsilateral septal CC was feasible, with high success rates and acceptable complications, in the hands of experienced operators.
Keywords: percutaneous coronary interventions, chronic total occlusions, ipsilateral septal collateral, left coronary artery
Introduction
A retrograde approach in percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) is widely used around the world, especially in experienced centers.1 With regard to retrograde collateral channel (CC) selection, the septal collateral is the preferred channel in most scenarios. However, the retrograde approach via ipsilateral septal CCs is rarely performed owing to the severe tortuosity of the channels and the need for a complex guiding catheter technique (such as the “ping-pong” technique).2 A few cases have reported the use of an ipsilateral retrograde approach for the left descending coronary artery (LAD) CTO.3,4 A systematic description of the percutaneous treatment of left coronary artery CTOs using ipsilateral septal CCs in the retrograde revascularization approach has never been carried out.
Our study is the first to focus on the feasibility and safety of an ipsilateral septal CC approach in retrograde CTO PCI.
Methods
Study Population
Between October 2015 and January 2022, all patients with successful wire tracking via ipsilateral septal CCs in retrograde CTO PCI were retrospectively screened from the database of the Chronic Total Occlusion Club, China. Those with missing procedural aspect data (records and angiograms) were excluded. Finally, 25 cases were included and analyzed. Each CTO PCI was performed according to the guidelines and algorithms of the time. The indications for CTO PCI were recorded and evaluated, and the final decision on the initiation of the PCI procedure was made by the operator. Procedures were divided into the LAD-septal-LAD group (n=15) and the LAD-septal-left circumflex coronary artery (LCX) group (n=10).
The study protocol was approved by the medical ethics committee of Zhongshan Hospital. The study complied with the Declaration of Helsinki. All patients provided written informed consent before participating in the procedure.
Study Definitions
The two key characteristics of a CTO are an occlusion with the absence of antegrade flow (Thrombolysis In Myocardial Infarction [TIMI] flow grade 0) through the lesion with a presumed or documented duration of ≥3 months.1 The angiographic characteristics of CTOs included the locations of the CTO, morphology of the stump, calcification at the site of the occlusion (radiopacity present before contrast medium injection), vessel tortuosity (the presence of at least one bend >45° proximal to the occlusion), and grade of collaterals.5,6 The J-CTO score was calculated.5 The collateral tortuosity was defined by McEntegart et al.7 Perioperative myocardial infarction (PMI) was defined by the fourth universal definition of myocardial infarction.8 All analyzed CTOs were performed by experienced CTO operators, who were defined as operators with >100 CTO PCI cases per year.9
CC tracking was defined as achievement of the placement of microcatheters into the distal true lumen using the ipsilateral retrograde approach. Technical success was defined as achievement of TIMI grade 2 or greater antegrade flow in all ≥2.5 mm distal branches with <30% residual stenosis of the target CTO lesion at the end of the procedure.1 Procedural success was defined as the achievement of technical success without in-hospital major adverse cardiac and cerebrovascular events, which included death from all causes, Q-wave myocardial infarction (MI additionally with new pathological Q-wave in the postoperative electrocardiogram), stent thrombosis, revascularization, and stroke.1 Procedural complications were defined as target vessel/septal perforation, donor vessel dissection, and pericardial tamponade requiring pericardiocentesis.10
Data Collection
All patients received dual antiplatelet therapy with aspirin (300 mg) and clopidogrel (300 mg) or ticagrelor (180 mg) before PCI. Statins and beta-blocker agents were prescribed to all individuals if there were no contraindications. Clinical characteristics and in-hospital events were recorded by a physician who was blind to the study design and subsequent data analysis. Angiograms and procedural records were reviewed by two qualified interventional physicians (one physician with >100 total CTO PCI cases per year). If there were any ambiguities in the reports or films, the reports and films were reviewed independently by a third, well-qualified interventional physician. All CTO PCIs were performed according to the current guidelines. All interventional materials, including guidewires and catheters for the retrograde treatment approach, were selected by the operator.
Statistical Analysis
Continuous variables were presented as mean ± standard deviation (SD). Categorical variables were expressed as number (%). Continuous variables were compared by the independent Student’s t-test and categorical variables were compared by the chi-squared test or Fisher’s exact test. A p value <0.05 was considered statistically significant. All data analyses were conducted by SPSS 25.0 and GraphPad Prism 5 software.
Results
Clinical Characteristics
Between October 2015 and January 2022, 25 retrograde CTO PCI procedures through ipsilateral septal CCs were performed by five experienced CTO operators. These cases were divided into the LAD-septal-LAD group (n=15) and LAD-septal-LCX group (n=10). The baseline characteristics of all patients (aged 57.6±12.4 years; 88% men), and of the patients divided into groups are given in Table 1. Overall, 88% suffered from symptoms of ischemia, which was the most common indication for PCI. The left ventricular ejection fraction (LVEF) among all cases was mostly normal (58.4±12.4%). The LVEF in the LAD-septal-LAD group was lower than that in the LAD-septal-LCX group (p=0.060). There were no statistically significant differences in terms of cardiovascular risk factors and comorbidities, including age, body mass index, diabetes, atrial fibrillation, and hypertension.
 |
Table 1 Baseline Clinical Characteristics |
Angiographic Characteristics
As shown in Table 2, the most frequent CTO vessel targeted via ipsilateral septal CCs was the LAD (84%). Occlusion complexity was very pronounced, according to the J-CTO score (1.8±1, 24% J-CTO score ≥3). In particular, blunt stump (52%) and lesion length >20 mm (72%) dictated the use of a retrograde approach in our cohort. Up to 32% had undergone previous unsuccessful CTO-PCIs. In addition, the majority of CCs were classified as CC2 (80%). The CTO complexity was comparable between groups, as was the collateral degree. However, moderate to severe collateral tortuosity was found in the majority of cases in the LAD-septal-LAD group, where it was much more common than in the LAD-septal-LCX group (86.7% vs 20%, p=0.002).
 |
Table 2 Angiographic Characteristics |
Procedural Data
The utilization rates of radial access alone, the ping-pong technique, and 7 F guiding catheters were 76%, 12%, and 76%, respectively. A primary retrograde approach was employed in 28% of cases (Table 3). The Corsair (ASAHI INTECC Co.) and Finecross (Terumo Corporation) microcatheters were most frequently adopted to navigate septal CCs (88%), as demonstrated in Figures 1 and 2. The timing and feasibility of tip injection are also shown in Figures 1 and 2. As illustrated in Figure 3, Sion guidewires (ASAHI INTECC Co.) were most frequently used to cross septal CCs (17 cases, 68%), followed by Sion blue (two cases, 8%), Sion black (two cases, 8%), Fielder XT-R (ASAHI INTECC Co., two cases, 8%), and Such 03 guidewires (ASAHI INTECC Co, two cases, 8%). Among these cases, 28% received multiple guidewires for crossing septal CCs. As shown in Table 3, there were 47.8%, 34.8%, and 17.4% cases where we used the retrograde wire crossing technique, kissing wire technique, and reverse controlled antegrade and retrograde tracking (CART) technique, respectively. The average procedural duration of all cases was 127 minutes. Both technical success and procedural success were achieved in 92% of cases. In addition, the success rate of the microcatheter tracking the septal CC was 96%. There were no differences between groups with regard to the rates of CC tracking success, technical success, or procedural success.
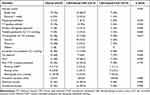 |
Table 3 Procedural Data |
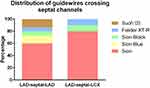 |
Figure 3 Distribution of guidewires crossing septal channels. Abbreviations: LAD, left descending coronary artery; LCX, left circumflex coronary artery. |
In-Hospital Events
As shown in Table 4, postoperative adverse events occurred in one patient (4%), with instances of Q-wave myocardial infarction (MI). This Q-wave MI was associated with the occlusion of the diagonal branch during the procedure. The incidence of procedural complications was 4% (one septal channel perforation, Ellis type 3). There were no other procedural complications, including pericardial tamponade and vessel dissection. The incidence of PMI was 28%. The peak cardiac troponin T value after PCI was 0.15±0.26 ng/mL and the postoperative hospital stay was 1.8±0.9 days. All mentioned variables were evenly distributed between the groups (p>0.050).
 |
Table 4 Procedural Complications and In-Hospital Events |
Discussion
Our study is the first to focus on the feasibility and safety of ipsilateral septal CC in retrograde CTO PCI. Based on the described procedural aspects and outcomes of the ipsilateral retrograde approach, we have two major findings. 1) The retrograde approach via ipsilateral septal CC was feasible, with high success rates and acceptable complications, in the hands of experienced operators. 2) The LAD-septal-LAD pathway was usually accompanied by moderate or severe collateral tortuosity, which may result in a greater likelihood of procedural complications in retrograde CTO PCI.
The septal CC as the contralateral CC is still the preferred pathway for the retrograde approach for CTO PCI. However, contralateral CCs may be uncrossable, even for experts, in 10–20% of cases.11 Currently developed wire technologies and dedicated microcatheters can facilitate the crossing of CCs. Nevertheless, because of the tortuous course and acute angle of channels, ipsilateral septal CCs are seldom considered as a retrograde approach for CTO PCI, even by experienced CTO operators, which is line with our study (a primary ipsilateral retrograde approach accounted for only 28%). Besides, retrograde CTO PCI through ipsilateral septal CCs requires years of dedicated training for operators with complex interventions.
In the present research, LAD-CTOs accounted for the majority of cases, which is opposite to the vessel distribution in ipsilateral retrograde approaches for CTO PCI.12,13 This is because we exclusively focused on ipsilateral septal CCs via septal pathways rather than epicardial channels and LCX self-channels. Regarding the backup support of guiding catheters, radial access and 7 F guiding catheters were basically adequate for the ipsilateral retrograde approach. Radial access in CTO PCI is prevalent not only because of the satisfactory backup support, but also owing to the better ergonomics and lower radiation.14 Besides, 7 F guiding catheters were enough to avoid congestion and excessive friction of antegrade and retrograde material. Although the ping-pong technique can overcome excessive friction, the actual usage rate was only 12%. In our clinical practice, Sion guidewires were first considered (68%) because of their atraumatic tip, flexible shaft, high lubricity, and improved torque response. Once Sion family guidewires had failed to cross the septal channels, Fielder XT-R and Suoh 03 wires were attempted. About one-third of cases accepted at least two guidewires to cross septal channels. The use of tip injection through the microcatheter when the collateral course was not completely understood helped in the guidewire crossing.
Of the 25 cases, there was only one case with failed microcatheter CC tracking, because of the extremely steep angles of the LAD-septal-LCX pathway, which was eventually achieved through an antegrade approach. In addition, there were two technical failures, in which one patient had acute heart failure during the procedure and another had uncrossable occlusion despite the use of stiff guidewires, including Conquest Pro 8-20. Compared with previous research,12,13 our technical success and procedural success rates are slightly higher. We attribute this to the relatively low procedural difficulty, which is reflected by the J-CTO scores (1.8±1) and collateral degree (80% CC2). Another reason for this is that previous research included the full spectrum of CCs and our study excluded epicardial channel analysis. In our clinical practice, the LAD-septal-LAD pathway was technically more challenging because of the sharp angles to overcome. However, there were no differences between groups with regard to the rates of CC tracking success, technical success, or procedural success.
As shown in Table 4, one procedural complication was found in the LAD-septal-LAD pathway. In this case, septal Ellis 3 perforation occurred during the operation (coronary artery fistula to left ventricular) and the patient eventually received conservative treatment because of the low flow. The postoperative electrocardiogram was the same as the previous one and the patient had no ischemia symptoms. The only postoperative adverse event (Q-wave myocardial infarction) was associated with occlusion of the diagonal branch during the procedure. Considering that the diagonal branch was relatively small, no further interventional treatment was carried out. No pericardial tamponade or adverse cardiac events occurred during the hospital stay.
Limitations
First, this was a retrospective study, with inherent bias. The procedural aspects of the analyzed cases may not reflect the situation in the real world (eg, our technical success and procedural success rates were up to 92%). Second, it was a single-center study, which was inevitably accompanied by bias (cases were scarce in other centers). Therefore, further multicenter confirmation of the results is warranted. Third, owing to the complexity of the retrograde approach via the ipsilateral septal CC, these CTO PCIs were relatively scarce and all cases were performed by five experienced CTO operators. For this reason, our findings may not be generalizable to other clinical practices. Larger-scale, multicenter, prospective clinical trials are required to confirm our findings. Fourth, our follow-up was limited to the duration of hospitalization, and long-term follow-up was unavailable.
Conclusion
Despite difficulties in crossing the ipsilateral septal channels, a retrograde approach via the ipsilateral septal CC was feasible, with high success rates and acceptable complications, in the hands of experienced operators.
Funding
The study received funding from the State Key Clinical Specialty Construction Project (YW2021-002) and Shanghai Municipal Key Clinical Specialty (shslczdzk01701).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ybarra LF, Rinfret S, Brilakis ES, et al. Definitions and clinical trial design principles for coronary artery chronic total occlusion therapies: CTO-ARC consensus recommendations. Circulation. 2021;143:479–500. doi:10.1161/CIRCULATIONAHA.120.046754
2. Brilakis ES, Grantham JA, Banerjee S. ”Ping-pong” guide catheter technique for retrograde intervention of a chronic total occlusion through an ipsilateral collateral. Catheter Cardiovasc Interv. 2011;78:395–399. doi:10.1002/ccd.22870
3. Chandra S, Vijay SK, Dwivedi SK. Successful recanalization of a left anterior descending chronic total occlusion via an ipsilateral intraseptal collateral using reverse CART technique. J Invasive Cardiol. 2013;25:E72–E74.
4. Suzuki M, Takagi Y, Tsuchikane E. Percutaneous coronary intervention of chronic total occlusion in a left anterior descending coronary artery using an ipsilateral intraseptal bridging collateral tracking technique. Catheter Cardiovasc Interv. 2010;76:536–540. doi:10.1002/ccd.22561
5. Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213–221. doi:10.1016/j.jcin.2010.09.024
6. Werner GS, Ferrari M, Heinke S, et al. Angiographic assessment of collateral connections in comparison with invasively determined collateral function in chronic coronary occlusions. Circulation. 2003;107:1972–1977. doi:10.1161/01.CIR.0000061953.72662.3A
7. McEntegart MB, Badar AA, Ahmad FA, et al. The collateral circulation of coronary chronic total occlusions. Eurointervention. 2016;11:e1596–e1603. doi:10.4244/EIJV11I14A310
8. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40:237–269.
9. Zhong X, Gao W, Hu T, et al. Impact of subintimal plaque modification on reattempted chronic total occlusions percutaneous coronary intervention. JACC Cardiovasc Interv. 2022;15:1427–1437. doi:10.1016/j.jcin.2022.06.015
10. Ge L, Zhong X, Ma J, et al. Safety and feasibility of a low frame rate protocol for percutaneous coronary intervention to chronic total occlusions: preliminary experience. Eurointervention. 2018;14:e538–e545. doi:10.4244/EIJ-D-17-00515
11. Rathore S, Katoh O, Matsuo H, et al. Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv. 2009;2:124–132. doi:10.1161/CIRCINTERVENTIONS.108.838862
12. Mashayekhi K, Behnes M, Valuckiene Z, et al. Comparison of the ipsi-lateral versus contra-lateral retrograde approach of percutaneous coronary interventions in chronic total occlusions. Catheter Cardiovasc Interv. 2017;89:649–655. doi:10.1002/ccd.26611
13. Azzalini L, Agostoni P, Benincasa S, et al. Retrograde chronic total occlusion percutaneous coronary intervention through ipsilateral collateral channels: a multicenter registry. JACC Cardiovasc Interv. 2017;10:1489–1497. doi:10.1016/j.jcin.2017.06.002
14. Achim A, Szigethy T, Olajos D, et al. Switching from proximal to distal radial artery access for coronary chronic total occlusion recanalization. Front Cardiovasc Med. 2022;9:895457. doi:10.3389/fcvm.2022.895457
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


