Back to Journals » Clinical Ophthalmology » Volume 14
Retinal Artery Contraction After Phenylephrine as a Cardiovascular Risk Biomarker
Authors Casado A , López-de-Eguileta A, Fonseca S, Cerveró A, Gaitán J
Received 29 January 2020
Accepted for publication 1 April 2020
Published 11 May 2020 Volume 2020:14 Pages 1269—1275
DOI https://doi.org/10.2147/OPTH.S247680
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Alfonso Casado, Alicia López-de-Eguileta, Soraya Fonseca, Andrea Cerveró, Jorge Gaitán
Department of Ophthalmology, Hospital Universitario Marqués de Valdecilla, Santander, Spain
Correspondence: Jorge Gaitán
Ophthalmology Department, Hospital Marqués de Valdecilla, Av. Valdecilla, 25, Santander 39008, Cantabria, Spain
Tel +34 605762803
Email [email protected]
Background and Aim: We investigated the in vivo changes of artery diameter (AD) and vein diameter (VD) after topical phenylephrine 2.5% instillation, and its relationship with the Systematic Coronary Risk Evaluation (SCORE).
Methods: This is a cross-sectional study. Healthy control patients were included. All of the participants underwent enhanced depth imaging by spectral-domain optical coherence tomography before and 30 minutes after phenylephrine instillation, using eye-tracking and follow-up software. Changes in AD and VD were assessed.
Results: The study included 45 eyes of 45 patients (14 males and 31 females). The mean age was 58.6 ± 15.1 years (26– 88 years). Mean SCORE risk estimation value was 2.0 (0– 14). No significant correlation was found between pre-phenylephrine AD or VD with age (p=0.237 and p=0.821, respectively), SCORE (p=0.545 and p=0.723, respectively). AD significant thinned after phenylephrine (p< 0.001), whereas no significant changes could be depicted in VD (p=0.474). Changes in AD after phenylephrine were significantly related with SCORE risk estimation (p=0.035). Discordantly, changes in VD after phenylephrine were not significantly related with SCORE (p=0.505).
Conclusion: As a significant thinning of AD occurred following phenylephrine instillation, and as the magnitude of this thinning is related with SCORE, it is useful to test the retinal artery contraction to infer the cardiovascular health status.
Keywords: choroidal thickness, peripapillary choroidal thickness, retinal nerve fiber layer, phenylephrine
Introduction
Changes in retinal vascular pattern have been proved to be related to systemic cardiovascular diseases.1 In fact, a dilated fundoscopic exam is necessary for staging of hypertensive retinopathy.2 It is possible to detect changes in the microvasculature of the retina which are connected with the development of cardiovascular diseases. It has also been suggested endothelial dysfunction is a pathogenic factor in these findings.3
Histopathological studies in monkeys have shown that changes in retinal vessels reveal vascular damage from hypertension, aging, and other diseases.4,5 However, retina offers a feasibility place to observe microcirculation directly, and to study in vivo the structure and pathology of the human circulation. The study of vascular pattern using photography examination of the retina have allowed to relate retinal arteriolar narrowing with reduced myocardial perfusion measures on cardiac magnetic resonance imaging6 or lacunar stroke.7 Other retinopathy changes could be associated with coronary artery calcification,8 as well as larger retinal venular diameter has been connected to an increase in inflammatory markers.9
Nevertheless, the advances in technology allow us to analyze retinal vessels using optical coherence tomography (OCT). With this device, diameter of vessels could be measured more accurately, as the arteries and veins are scanned and showed in a tangential or axial view, where they could be highly reproducible and repeatable measured.10–12
Otherwise, in vitro studies in rats have shown that different aortic ring responses to phenylephrine were associated with cardiovascular status. Aloysius et al published that normoglycaemic tissues contract significantly more than the diabetic tissues, disclosing an endothelial vascular dysfunction in damaged arteries.13 Besides, Jiménez-Altayó et al have analyzed the contraction of mesenteric arteries in a mouse model of accelerated senescence.14 This study revealed that arteries of mice with a western-type high-fat diet showed a reduced contraction comparing with those without this diet, revealing an aberrant production of nitric oxide (NO) by inducible NO synthase (iNOS). This aberrant iNOS-derived NO production has been implicated in the pathogenesis of endothelial dysfunction and vascular disease, and has been published to be involved in pathological conditions as chronic inflammatory diseases, including atherosclerosis.15,16
The purpose of our study was to analyze the vascular retinal pattern using OCT, comparing both the artery and vein contraction after topical instillation of phenylephrine in the eye, and if their contraction is related to their cardiovascular risk, investigating the Systematic Coronary Risk Evaluation (SCORE) of the patients.17
Patients and Methods
Patients
All participants were recruited from the Ophthalmology department of Valdecilla Hospital, from May 2017 to June 2018. The study protocol was approved by the Ethics Committee of Valdecilla Hospital, and it was performed in accordance with the principles of the Declaration of Helsinki. Written consent forms were distributed to all the participants before the examinations.
All subjects were required to have a refractive error less than −6.0 diopters of sphere or 3 diopters of cylinder, no history of ocular diseases. To reduce statistical bias, only the left eye of the patients was included in the study.
Exclusion criteria included clinically relevant opacities of the optic media and low-quality images due to unstable fixation, or severe cataract (patients with mild to moderate cataract might be enrolled in the study, but only high-quality images were included).
Clinical Assessment
All subjects underwent a thorough ophthalmic examination on the day of OCT imaging, including best-corrected visual acuity, refraction, intraocular pressure (IOP) measurement with GAT, slit lamp examination and fundus examination. The refractive error was recorded using an auto refractometer Canon RK-F1 (Canon USA Inc., Lake Success, NY, USA). Axial length (AL) was measured by Lenstar LS 900 (Haag Streit AG, Koeniz, Switzerland). Thirty minutes after instillation, ophthalmic evaluation has ruled out an angle closure using slit lamp.
SCORE was calculated as previously described, according to their underlying risks for coronary heart disease, including age, cholesterol, smoking and systolic blood pressure.17
Optical Coherence Tomography Procedure
Prior to the administration of the phenylephrine eye drops (pre-treatment) and 30 min after instillation, 2 vertical optic nerve scans were obtained of each patient’s left eye using an enhanced deep image (EDI) with spectral-domain OCT (Spectralis HRA+OCT, Heidelberg Engineering, Heidelberg, Germany; wavelength for scan: 870 nm).
A single, well-trained ophthalmologist (ALE) performed all OCT examinations. The EDI image was averaged over 100 scans using the automatic averaging mode. The follow-up acquisition mode, unique to this SD-OCT device, was used to perform the second measurement, as it automatically placed follow-up scans in precisely the same anatomic location as previous scan.
Vein diameter (VD) and artery diameter (AD) were measured with a vertical caliper as previously described12 by two masked and experienced investigators (JG, SF), who were blinded to phenylephrine and SCORE status. To assess the cardiovascular risk we used the HeartScore online tool by the European Society of Cardiology, specifically for a low-risk population (Spain) and modified by HDL.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics V.20.0 (International Business Machine Corporation, Armonk, NY, USA).
A 1-sample Kolmogorov–Smirnov test was used to verify the normality of the data distribution. The AD and VD before and after phenylephrine 2.5% instillation were compared using paired Student’s T-test. Pearson correlation analysis was performed to assess the relationship between SCORE, age and AL, and AD and VD. The intraclass correlation coefficient (ICC) was used to determine the reliability of the measurements. An ICC value <0.40 represents poor agreement, 0.40–0.75 represents fair to poor agreement and >0.75 represents excellent agreement. The level of statistical significance was set at P < 0.05.
Results
Overall, 45 eyes of 45 patients (14 males and 31 females) were included in the study. Table 1 describes the demographic and clinical participant´s characteristics. The mean age was 58.6 ± 15.1 years (age range: 26–88 years). Mean SCORE risk estimation value was 2.0 (range 0–14). The mean spherical equivalent was measured as −0.84 ± 0.63 diopters. Mean AL was 23.3 ± 1.1 mm (range, 21.3–27.2 mm). Mean IOP was 14.6 ± 3.0 mmHg (IOP range 9–21 mmHg). Mean best-corrected visual acuity was 20/25. All eyes included in the study were phakic eyes. Table 2 represents the treatments of the patients.
 |
Table 1 Demographic and Clinical Participant´s Characteristics (45 Eyes of 45 Individuals). Data for Quantitative Variables are Shown as Mean (Standard Deviation). |
 |
Table 2 Participant´s Treatments (45 Eyes of 45 Individuals). Data for Treatments for the Patients Admitted to the Study in Percentage |
The ICCs were 0.990, 0.996, 0.993 and 0.987 for pre-phenylephrine AD, pre-phenylephrine VD, post-phenylephrine AD and post-phenylephrine VD, respectively.
No significant correlation was found between age and pre-phenylephrine AD nor VD (R=0.032; p=0.237 and R=0.001; p=0.821, respectively), SCORE (R=0.018; p=0.545 and R=0.001; p=0.723, respectively), IOP (R=0.0005; p=0.237 and R=0.001; p=0.821, respectively); nor for AL (R=0.018; p=0.378 and R=0.162; p=0.107, respectively).
Figure 1 shows the pre and post-phenylephrine diameter of artery and vein. After 30 minutes of phenylephrine instillation, we found a significant thinning of the diameter of arteries (116.7 ± 19.3 µm pre-phenylephrine and 113.4 ± 17.9 post-phenylephrine; p<0.001), whereas no significant changes could be depicted in VD (143.9 ± 26.2 µm pre-phenylephrine and 145.9 ± 17.5 post-phenylephrine; p=0.474).
Interestingly, changes in AD were related with SCORE risk estimation (R=0.106; p=0.029), as it is pointed out in Figure 2 where the highest the SCORE result was, the smaller change in artery diameter we got. However, no significant correlation was found between changes in AD with age (R=0.076; p=0.066). Differently, we found no significant correlation between VD and SCORE risk estimation (R=0.015; p=0.477) or age (R=0.002; p=0.775).
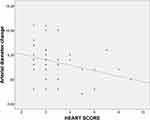 |
Figure 2 Correlation between arteries’ diameter changes before and after phenylephrine and SCORE risk estimation (R=0.106; p=0.029). |
Discussion
Phenylephrine is a mydriatic agent used commonly by ophthalmologists to induce pupil dilation. Besides, OCT is available in every Ophthalmology department. For these reasons, this phenylephrine-artery contraction test could be easily performed in 30 minutes and allow both the ophthalmologist and cardiologist to establish the coronary risk of the patient. To our knowledge, this is the first study to analyze the retinal vascular contraction to phenylephrine and its relation with the coronary risk.
Analysis of peripheral vessels as found in subcutaneous fat (eg, from gluteal biopsies) could predict risk of cardiovascular disease events.18–21 These studies suggest that peripheral vascular remodeling is one of the first manifestations of target organ damage, taking place before cardiac hypertrophy or proteinuria. However, analysis of retinal vessels has the advantage that the study could be performed in vivo and that it’s possible to observe in vivo vascular reaction to different stimuli.
Previous studies analyzing the retina using photography have suggested the retinal arteriolar diameter as a biomarker of coronary microvascular disease. Retinal arteriolar narrowing has been associated with cardiovascular events.6,7 Wang et al found that the smaller retinal arteriolar caliber was associated with lower hyperemic myocardial blood flow and perfusion reserve, in asymptomatic adults with no coronary calcification.6 Similarly, Lindley et al demonstrated that the patients with lacunar stroke were more likely than those with other stroke subtypes to have microvessel signs that could be depicted as retinal arteriolar narrowing.7 Otherwise, retinal venular morphology could be also related with cardiovascular diseases. Thus, Ong et al have associated not only retinal arteriolar narrowing, but also increased arteriolar and venular tortuosity with ischemic stroke,22 as well as Klein et al published that a larger retinal venular diameter could be related with systemic inflammation, measuring interleukin 6, C-reactive protein, and amyloid A levels.9 So retina vessel analysis could bring heaps of information of cardiovascular systemic damage. However, technology has brought today the possibility to in vivo analyze the vessel retinal caliber with the OCT. Using this device, it is possible to measure retinal structures in a more reproductive way than using retinal pictures.10–12 In fact, OCT could become an important ancillary test to diagnose patients with cerebral small vessel diseases such as cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, in which a larger retinal AD and VD have depicted.12 Furthermore, our study showed that the changes in AD could be used to ascertain cardiovascular risk of the patient. Performing an OCT examination takes only one minute per eye. This phenylephrine test requires a 2-times exploration disjointed 30 minutes, but it allows the examiner to perform different patient’s analysis in a short period of time. This study is based on in vitro analysis with rats and mice that have revealed that aortic and mesenteric artery, respectively, respond better to phenylephrine if the cardiovascular state is desirable.13,14 First, Aloysius et al analyzed the contraction of the aortic ring of rats with phenylephrine.13 They found that diabetes induced desensitization of the smooth muscle cells to phenylephrine stimulation, so normoglycaemic tissues contract significantly more than the diabetic tissues. They proved that NO modulates phenylephrine contraction via cyclic guanosine monophosphate (cGMP), as blockade of NO with Nomega-Nitro-L-arginine methyl ester (L-NAME) enhanced contraction, as well as blockade of cGMP with methylene blue enhanced contraction, as suggested previously by Dora et al.23 NO is also proposed by Jiménez-Altayó et al to be the principal agent to cause artery contraction after phenylephrine.14 They analyzed the contraction of mesenteric arteries in a mouse model of accelerated senescence. Mice with a western-type high-fat diet reflected a reduced contraction compared with those without this diet, revealing an aberrant production of NO by the endothelial cells. Before this diet, contraction after phenylephrine was equally potentiated by L-NAME, however, after high-fat diet feeding, it could be depicted a suppression of the NO-mediated modulation of phenylephrine contraction by L-NAME, that could produce a lower contraction of the arteries. We believe that all this evidence support our idea that a worse vascular reactivity to phenylephrine is driven by endothelial dysfunction and it is therefore a marker of risk, as proved by the correlationship with the SCORE.
Other tests investigating the contraction to potassium chloride and relaxation to acetylcholine reflected no differences between cardiovascular status response in rats or mice13,14. Thus, we have chosen phenylephrine to examine its effect in retinal vessels. Also as it is a common eye drop easily available and used by ophthalmologists.
Several limitations are present in this study. First, one single vertical scan has been used. However, these scans might represent the AD and VD as previously published.10–12 As the examiner was masked, no influence in the results could be associated. Future studies should compare OCT results with fundus photography measurements such as The Beaver Dam Eye Study.9 Our group considered that OCT measurement could appreciate better slight changes in retinal vessel’s diameter.
Secondly, we analyzed the changes only 30 minutes after phenylephrine drops instillation. Li et al24 analyzed changes in choroidal thickness 0, 30 and 60 minutes after drop instillation. Nevertheless, similar changes were depicted in 30 and 60 minutes measurements. We analyzed differences in a single 30 minutes post-instillation examination as it may be convenient for clinical practice due to its simplicity. In addition, IOP after phenylephrine instillation have not been assessed and an increase of this measurement might change vessel’s diameter. However, ophthalmic evaluation after phenylephrine instillation have ruled out an angle closure.
Thirdly, we have chosen patients with no eye diseases. So this test could not be performed if glaucoma, pseudoexfoliation or retinal diseases are found, as these pathologies might change vascular diameters.25–27 Besides, transparency is required to perform this analysis, so cataract or corneal diseases could preclude this test. However, as two eyes are available in human being, if one of them is affected with these diseases, the other is usable to perform this test.
In addition, 2.5% phenylephrine instillation might rise systemic blood pressure and this effect might change retinal vessel’s diameter. Some studies proved no significant systemic blood pressure change after both 2.5% or the 10% concentration28,29 whereas other studies showed a significant rise.30,31 Future studies might assess systemic blood pressure 30 min after 2.5% phenylephrine instillation. However, we believe that if a rise of systemic blood pressure is produced, it is slight and might not change retinal vessel’s diameter or, even though, retinal artery contraction might be still a useful cardiovascular risk biomarker.
Moreover, we did not find a suitable explanation in literature explaining why AD significant thinned after phenylephrine (p<0.001), whereas no significant changes could be depicted in VD (p=0.474). It might be related with the different response of them to nitric oxide, as well as it might depend on their different stiffness,2,3 but more studies should be assessed to find out this question.
Finally, our sample size is small. However the results show that there might be a tendency of correlation between contraction of retinal arteries and cardiovascular status that should be studied in subsequent works.
In summary, we present a test to find out the cardiovascular status of a patient with a simple OCT analysis before and after a phenylephrine drop instillation.
Author Contributions
A. Casado and J. Gaitán conceived of the presented idea. A. Casado developed the theory and performed the computations. J. Gaitán, A. López de Eguileta and A. Cerveró performed the analytical methods and encouraged S. Fonseca to investigate and verify the measurements made in the OCT and supervised the findings of this work. All authors discussed the results and contributed to the final manuscript. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Klein R. Retinopathy in a population-based study. Trans Am Ophthalmol Soc. 1992;90:561–594.
2. Katakam R, Brukamp K, Townsend RR. What is the proper workup of a patient with hypertension? Cleve Clin J Med. 2008;75:663–672. doi:10.3949/ccjm.75.9.663
3. Wong TY, McIntosh R. Systemic associations of retinal microvascular signs: a review of recent population-based studies. Ophthalmic Physiol Opt. 2005;25:195–204. doi:10.1111/j.1475-1313.2005.00288.x
4. Garner A, Ashton N, Tripathi R, Kohner EM, Bulpitt CJ, Dollery CT. Pathogenesis of hypertensive retinopathy. An experimental study in the monkey. Br J Ophthalmol. 1975;59:3–44. doi:10.1136/bjo.59.1.3
5. Ashton N, Peltier S, Garner A. Experimental hypertensive retinopathy in the monkey. Trans Ophthalmol Soc UK. 1969;88:167–186.
6. Wang L, Wong TY, Sharrett AR, Klein R, Folsom AR, Jerosch-Herold M. Relationship between retinal arteriolar narrowing and myocardial perfusion: multi-ethnic study of atherosclerosis. Hypertension. 2008;51:119–126. doi:10.1161/HYPERTENSIONAHA.107.098343
7. Lindley RI, Wang JJ, Wong MC, et al. Retinal microvasculature in acute lacunar stroke: a cross-sectional study. Lancet Neurol. 2009;8:628–634. doi:10.1016/S1474-4422(09)70131-0
8. Wong TY, Cheung N, Islam FM, et al. Relation of retinopathy to coronary artery calcification: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2008;167:51–58. doi:10.1093/aje/kwm256
9. Klein R, Klein BE, Knudtson MD, Wong TY, Tsai MY. Are inflammatory factors related to retinal vessel caliber? The Beaver Dam Eye Study. Arch Ophthalmol. 2006;124:87–94. doi:10.1001/archopht.124.1.87
10. Muraoka Y, Tsujikawa A, Kumagai K, et al. Age and hypertension-dependent changes in retinal vessel diameter and wall thickness: an optical coherence tomography study. Am J Ophthalmol. 2013;156:706–714. doi:10.1016/j.ajo.2013.05.021
11. Goldenberg D, Shahar J, Loewenstein A, Goldstein M. Diameters of retinal blood vessels in a healthy cohort as measured by spectral domain optical coherence tomography. Retina. 2013;33:1888–1894. doi:10.1097/IAE.0b013e31829477f2
12. Alten F, Motte J, Ewering C, et al. Multimodal retinal vessel analysis in CADASIL patients. PLoS One. 2014;9(11):e112311. doi:10.1371/journal.pone.0112311
13. Aloysius UI, Achike FI, Mustafa MR. Mechanisms underlining gender differences in Phenylephrine contraction of normoglycaemic and short-term Streptozotocin-induced diabetic WKY rat aorta. Vascul Pharmacol. 2012;57(2–4):81–90. doi:10.1016/j.vph.2011.11.009
14. Jiménez-Altayó F, Onetti Y, Heras M, Dantas AP, Vila E. Western-style diet modulates contractile responses to phenylephrine differently in mesenteric arteries from senescence-accelerated prone (SAMP8) and resistant (SAMR1) mice. Age (Dordr). 2013;35(4):1219–1234. doi:10.1007/s11357-012-9450-6
15. Hill BG, Dranka BP, Bailey SM, Lancaster JR
16. Villanueva C, Giulivi C. Subcellular and cellular locations of nitric oxide synthase isoforms as determinants of health and disease. Free Radic Biol Med. 2010;49(3):307–316. doi:10.1016/j.freeradbiomed.2010.04.004
17. Conroy RM, Pyörälä K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24(11):987–1003. doi:10.1016/S0195-668X(03)00114-3
18. De Ciuceis C, Porteri E, Rizzoni D, et al. Structural alterations of subcutaneous small-resistance arteries may predict major cardiovascular events in patients with hypertension. Am J Hypertens. 2007;20:846–852. doi:10.1016/j.amjhyper.2007.03.016
19. Rizzoni D, Porteri E, Boari GE, et al. Prognostic significance of small-artery structure in hypertension. Circulation. 2003;108:2230–2235. doi:10.1161/01.CIR.0000095031.51492.C5
20. Schiffrin EL, Park JB, Intengan HD, Touyz RM. Correction of arterial structure and endothelial dysfunction in human essential hypertension by the angiotensin receptor antagonist losartan. Circulation. 2000;101:1653–1659. doi:10.1161/01.CIR.101.14.1653
21. Park JB, Schiffrin EL. Small artery remodeling is the most prevalent (earliest?) form of target organ damage in mild essential hypertension. J Hypertens. 2001;19:921–930. doi:10.1097/00004872-200105000-00013
22. Ong YT, De Silva DA, Cheung CY, et al. Microvascular structure and network in the retina of patients with ischemic stroke. Stroke. 2013;44(8):2121–2127. doi:10.1161/STROKEAHA.113.001741
23. Dora KA, Hinton JM, Walker SD, Garland CJ. An indirect influence of phenylephrine on the release of endothelium-derived vasodilators in rat small mesenteric artery. Br J Pharmacol. 2000;129(2):381–387. doi:10.1038/sj.bjp.0703052
24. Li Z, Zeng J, Jin W, Long W, Lan W, Yang X. Time-course of changes in choroidal thickness after complete mydriasis induced by compound tropicamide in children. PLoS One. 2016;11(9):e0162468. doi:10.1371/journal.pone.0162468
25. Takai Y, Tanito M, Omura T, Kawasaki R, Kawasaki Y, Ohira A. Comparisons of retinal vessel diameter and glaucomatous parameters between both eyes of subjects with clinically unilateral pseudoexfoliation syndrome. PLoS One. 2017;12(6):e0179663. doi:10.1371/journal.pone.0179663
26. Adiarti R, Ekantini R, Agni AN, Wong TY, Sasongko MB. Retinal arteriolar narrowing in young adults with glaucomatous optic disc. J Glaucoma. 2018;27(8):699–702. doi:10.1097/IJG.0000000000000997
27. Newman A, Andrew N, Casson R. Review of the association between retinal microvascular characteristics and eye disease. Clin Exp Ophthalmol. 2018;46(5):531–552. doi:10.1111/ceo.13119
28. Symons RCA, Walland MJ, Kaufman DV. Letter to the editor. Eye. 1997;11:946–947. doi:10.1038/eye.1997.239
29. Malhotra R, Banerjee G, Brampton W, et al. Comparison of the cardiovascular effects of 2.5% phenylephrine and 10% phenylephrine during ophthalmic surgery. Eye. 1998;12:973–975. doi:10.1038/eye.1998.252
30. Chin KW, Law NM, Chin MK. Phenylephrine drops in ophthalmic surgery: a clinical study on cardiovascular effects. Med J Malaysia. 1994;49:158–163.
31. Kenawy NB, Jabir M. Phenylephrine 2.5% and 10% in phacoemulsification under topical anaesthesia: is there an effect on systemic blood pressure? Br J Ophthalmol. 2003;87(4):505–506. doi:10.1136/bjo.87.4.505
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

