Back to Journals » ClinicoEconomics and Outcomes Research » Volume 13
Results of a Time and Motion Survey Regarding Subcutaneous versus Intravenous Administration of Daratumumab in Patients with Relapsed or Refractory Multiple Myeloma
Authors Slavcev M, Spinelli A, Absalon E, Masterson T , Heuck C, Lam A, De Cock E
Received 19 January 2021
Accepted for publication 19 April 2021
Published 8 June 2021 Volume 2021:13 Pages 465—473
DOI https://doi.org/10.2147/CEOR.S302682
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
Mary Slavcev,1 Allison Spinelli,2 Elisabeth Absalon,3 Tara Masterson,4 Christoph Heuck,4 Annette Lam,1 Erwin De Cock5
1Global Market Access, Janssen Global Services, Raritan, NJ, USA; 2Global Medical Affairs, Janssen Global Services, Raritan, NJ, USA; 3Real World and Late Phase, Syneos Health Clinical SARL, Paris, France; 4Medical Group Oncology, Janssen Research & Development, LLC, Spring House, PA, USA; 5Real World and Late Phase, Syneos Health Clinical Spain SL, Madrid, Spain
Correspondence: Mary Slavcev
Janssen Global Services, 19 Green Belt Drive, Toronto, ON, M3C 1L9, Canada
Tel +1 519 572 3989
Email [email protected]
Purpose: Daratumumab (DARA) is a humanized anti-CD38 monoclonal antibody and approved as monotherapy or in combination with standard of care regimens for the treatment of multiple myeloma (MM). DARA intravenous (IV) administration is time-consuming; availability of DARA subcutaneous (SC) is expected to reduce this burden. A time and motion survey was undertaken to elicit healthcare providers’ (HCPs’) understanding of the workflow and time estimates for administration of DARA IV and SC (beyond treatment time) in patients with relapsed/refractory MM.
Patients and Methods: This web-based, prospective survey collected data from HCPs at sites that actively enrolled patients in the phase 3 COLUMBA trial, a multicenter, noninferiority study of DARA IV versus DARA SC. Data collection included time actively spent on pre-specified drug preparation and drug administration/patient care activities; active HCP and chair time were extrapolated for first and subsequent treatments.
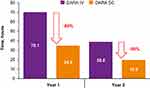
Results: Compared with DARA IV, DARA SC reduced median total active HCP time by 63.8% (from 265.9 to 96.3 minutes) and 49.5% (from 179.2 to 90.4 minutes) for first and subsequent treatments, respectively. When extrapolated to the anticipated number of treatments per year (23 in Year 1 and 13 in Year 2, per label), estimated active HCP time per patient was reduced by 50% in Years 1 (from 70.1 to 34.8 hours) and 2 (from 38.8 to 19.6 hours) for DARA SC versus DARA IV. Estimated chair time for DARA SC was decreased by 97% versus DARA IV for first (from 456.9 to 13.3 minutes) and subsequent treatments (from 238.0 to 8.1 minutes).
Conclusion: These results suggest that DARA SC is associated with less active HCP involvement during drug preparation and drug administration/patient care compared with DARA IV, potentially reducing burdens on patients and caregivers and creating efficiencies for HCPs and healthcare facilities, allowing more patients access to care.
Keywords: daratumumab, subcutaneous, treatment burden, survey
Introduction
Multiple myeloma (MM) is the second most common hematological cancer and is characterized by high levels of mortality and significant disease burden.1–4 Improving treatment for MM thus remains a top healthcare priority, and in recent years, targeted treatments have substantially improved response and survival in patients diagnosed with MM.5,6 Despite these advances in efficacy, treatment regimens have become increasingly complex and time-consuming,5 and healthcare providers (HCPs) are often overburdened and may struggle to keep up with patient demand.7 Complex treatment schedules requiring multiple hospital visits, lengthy infusion procedures, and potential side effects from infusions present a major burden to patients’ health-related quality of life (HRQoL) and healthcare systems.1–4
Daratumumab (DARA) is a humanized monoclonal antibody targeting CD38 with a well-characterized mechanism of action.8 DARA is approved for intravenous (IV) infusion as monotherapy or in combination with standard of care (SOC) regimens for patients with relapsed/refractory MM (RRMM), and as combination therapy with SOC for patients with newly diagnosed MM.9,10 Administration of DARA IV takes approximately 7 hours for the first infusion and 3–4 hours for subsequent infusions.9 Such long infusion times can negatively impact both HCP efficiency and patients’ satisfaction with treatment. Studies have found higher satisfaction rates with subcutaneous (SC) treatments compared with IV treatments among HCPs11 and patients with cancer.7,12,13 Furthermore, IV therapy is associated with an increased risk of infusion-related reactions (IRRs) in patients.14
To reduce the burden of DARA treatment administration, reduce IRRs, and improve patient satisfaction, an SC formulation of DARA was developed (DARA 1800 mg co-formulated with recombinant human hyaluronidase PH20 [rHuPH20; 2000 U/mL; ENHANZE® drug delivery technology, Halozyme, Inc., San Diego, CA, USA]). In the phase 1b PAVO study (NCT02519452), DARA SC was shown to have durable responses and an acceptable safety profile.15–17 In the phase 3 COLUMBA trial (NCT03277105), at a median follow-up of 7.5 months, overall response rate and maximum trough concentration with DARA SC were noninferior to DARA IV in patients with RRMM.18 DARA SC demonstrated a similar safety profile and a higher level of patient satisfaction compared with DARA IV while reducing the median time of treatment administration and the rate of injection site reactions (ISRs).18 Based on these results, DARA SC was approved by the US Food and Drug Administration and the European Medicines Agency.10,19 It is estimated that administration time for DARA SC during the first year of treatment will take <2 hours (115 minutes), assuming an SC injection duration of approximately 5 minutes and 23 injections.18,19
Time and motion (T&M) methodology consists of decomposing a process into essential activities and involves the repeated measurement of each pre-specified activity by trained observers. Prior to its approval in May 2020, data on the administration of DARA SC could only be collected prospectively as part of ongoing clinical trials. Given the logistic complexity associated with implementing a T&M study alongside a clinical trial, a survey of HCPs was selected as the preferred data-collection approach. Here, we report the results of a T&M survey conducted to elicit HCPs’ understanding of the workflow and time estimates for the administration of DARA IV and DARA SC beyond treatment time alone.
Materials and Methods
Survey Design
This prospective, cross-sectional, global survey collected primary data from HCPs regarding the preparation and administration processes for DARA SC and DARA IV for the treatment of patients with RRMM. Surveys were completed on a web-based platform complying with the Health Insurance Portability and Accountability Act. Data collection occurred from December 2019 until April 2020. The survey completion time was up to 1 hour, and remuneration was provided to respondents for their time.
Patient data, including efficacy and safety information, were not collected, and as such this research does not add any risk to patients. HCPs did not modify their standard of care practices for their patients as part of this survey completion. For these reasons, no regulatory or ethics committee submissions were required.
Participants
Practicing HCPs from centers that enrolled patients in the phase 3 COLUMBA clinical trial were invited to participate. Key eligibility criteria were an excellent understanding of DARA IV preparation and administration processes, and experience with DARA SC as part of the COLUMBA trial. Initial contact was made by the marketing authorization holder of DARA (Janssen Biotech, Inc.; Horsham, PA, USA); investigators who responded positively were sent a formal email invitation that included a website link to complete the survey. Investigators were asked to provide up to two completed surveys of HCPs at their site and were permitted to delegate the completion of the survey to a staff member, as long as the staff member had the required experience with DARA IV and DARA SC.
Survey Methodology
The survey was designed to elicit qualitative information regarding the typical DARA IV and SC workflow and management pathways (focusing on the who, what, where, when, and how), as well as quantitative opinion-based estimates of active HCP time. Active HCP time was defined as time fully dedicated to a single patient (as opposed to performing activities not related to this patient). The survey chronologically worked through all key steps and included four major sections: 1) DARA IV preparation in the pharmacy/drug preparation area, 2) DARA IV infusion administration in the patient care area, 3) DARA SC preparation in the pharmacy/drug preparation area, and 4) DARA SC injection administration in the patient care area. Drug preparation activities included collection of materials, preparation of the DARA IV infusion bag, filtration of DARA vials, and transport of the DARA IV infusion bag or syringe to the patient care area; as the stability of the SC product is only 4 hours, pharmacists cannot prepare the drug ahead of the patient’s visit.19 Drug administration/patient care activities included patient arrival/registration, blood sampling, physician consultation visits, line flushing or installing of a peripheral cannula (IV only), administration of pre-medication, record keeping, DARA IV infusion connection/dose escalation/monitoring/disconnection, DARA SC injection, and post-DARA management. For each pre-specified activity, the average active time and the likelihood (0–100%) that each HCP performed the task were captured. When estimating HCP time, participants were asked to think of how the task is typically performed per their local practice for DARA IV and as part of the COLUMBA trial for DARA SC. The primary language of the survey was English. For Japan, a Japanese version was developed.
To avoid missing data, the survey was designed with drop-down lists for categorical responses, and questions related to activity time required a mandatory response before being able to move forward. The use of free-text fields was limited. Data were exported from the web-based platform to Microsoft® Office Excel® 2007 (Redmond, Washington, USA) on a weekly basis and subjected to ongoing data quality control. Any inconsistent or missing data were clarified with the respondent by email and/or over the phone.
Statistical Analysis
The primary endpoints were mean and median active HCP time for each pre-specified activity, and mean and median total active times per single infusion and injection process. The latter were derived as the sum of the mean and median active HCP time, respectively, for each pre-specified activity making up the infusion and injection process (drug preparation area/pharmacy and patient care area/infusion suite combined). For some activities, mean and median time required an adjustment as follows: 1) the task constituted different scenarios and a weighted time was calculated based on the proportion distribution of those scenarios to occur (eg, blood sampling by means of venous access device, peripheral cannula, or venipuncture), 2) the task had a given likelihood of occurrence (eg, the management of IRR after DARA IV or ISR after DARA SC), and 3) the task had a given likelihood of occurrence and the HCP was actively involved with the patient during a given proportion of that time (eg, infusion dose escalation and monitoring during infusion).
Across all participants, mean and median total active HCP time were extrapolated to the first year of therapy by multiplying with the expected number of infusions or injections per year. Assuming DARA monotherapy or in combination with lenalidomide/dexamethasone or pomalidomide/dexamethasone, according to product label, DARA IV and DARA SC treatments should be administered 23 times in Year 1 and 13 times in Year 2.9,19 In addition, a post hoc analysis estimated patient chair time based on HCP inputs for pre-treatment activities (for DARA IV: Line flushing or installation of a peripheral cannula, and DARA infusion connection), infusion/injection duration, and post-treatment activities (disconnecting the DARA infusion, line flushing, post-DARA medication administration, and monitoring). Calculations were performed for Year 1 and Year 2 (ie, a proxy for subsequent years).
This was a descriptive, non-comparator study without a formal sample size calculation and no formal statistical comparisons were planned. The study applied a convenience sampling approach with a target sample size of up to 100 completed surveys; analyses were conducted on available surveys completed. Descriptive statistics for continuous variables included number of observations, mean, median, minimum, and maximum. Median results are reported here, as these are considered a better measure of central tendency than the mean. Descriptive statistics for categorical variables included counts and percentages. A sensitivity analysis was conducted comparing a subgroup of respondents with fully validated data with the overall population; fully validated data were available for 18 of the 26 respondents who provided all follow-up data. Participants were anonymized and no comparison in time between participants was made. All statistical analyses were performed using Microsoft® Office Excel® 2007.
Results
The survey was stopped prematurely in April 2020 due to reasons related to COVID-19; results presented thus represent completed surveys by that time. A total of 26 respondents from 16 unique centers and 8 countries (Brazil, Greece, Israel, Japan, Poland, Sweden, Taiwan, and Ukraine) completed the survey. Respondents included various study personnel, including principal investigators (n = 7), subinvestigators (n = 2), study coordinators (n = 7), study nurses (n = 8), and pharmacists (n = 2). Respondents classified their place of work as a general hospital (n = 7), specialized oncology hospital (n = 3), teaching/research hospital (n = 1), or a combination of those categories (n = 5).
Median total active HCP time for first and subsequent treatments was substantially reduced for DARA SC compared with DARA IV (Figure 1A). For DARA IV, the median total active HCP time was 265.9 minutes for the first infusion and 179.2 minutes for subsequent infusions. For DARA SC, the median total active HCP time was 96.3 minutes for the first injection and 90.4 minutes for subsequent injections. The resulting time savings for DARA SC compared with DARA IV amounted to 63.8% for the first administration and 49.5% for subsequent administrations. Drug preparation time stayed consistent between first and subsequent administrations, and was also relatively consistent between the SC and IV formulations. In contrast, drug administration duration was reduced by 91–99% with DARA SC versus DARA IV (Figure 2A). A comparison of the breakdown of pre-specified activities in the patient care area showed a substantial decrease in infusion-related activities with DARA SC compared with DARA IV, such as dose escalation and monitoring, disconnection and flushing of the infusion line, and record keeping, and a simplification in the drug administration workflow (Figure 3).
When extrapolated to the anticipated number of treatments per year, estimated active HCP time per patient was reduced for DARA SC compared with DARA IV in Year 1 and Year 2 (Figure 4). Estimated active time per patient for Year 1 and Year 2 was 70.1 and 38.8 hours, respectively, for DARA IV and 34.8 and 19.6 hours, respectively, for DARA SC, resulting in a 50% reduction in active HCP time in each year.
Finally, a post hoc analysis showed that estimated patient chair time for DARA SC was decreased by 97% compared with DARA IV. Estimated chair time for DARA IV was 456.9 minutes for the first infusion and 238.0 minutes for subsequent infusions. For DARA SC, estimated chair time for first and subsequent injections was 13.3 and 8.1 minutes, respectively (Figure 5A).
These results were confirmed by a sensitivity analysis, which used fully validated data for 18 of the 26 respondents (Figures 1B, 2B, and 5B).
Discussion
The results of this T&M survey revealed that DARA SC is associated with substantial reductions in active HCP time, duration of drug administration, and patient chair usage compared with DARA IV. The time reduction in active HCP time was largely attributable to tasks related to IV drug administration, as the SC formulation does not require time for activities such as installation of a peripheral cannula, infusion line connection and disconnection (including line flushing), or monitoring during infusion. Significant differences in administration durations between DARA IV and DARA SC were the key drivers in total reduction of patient chair usage with DARA SC.
This time savings has a number of benefits for patients, caregivers, HCPs, and health systems involved in the treatment of patients with MM. Patients with MM are more susceptible to infections during the course of their treatment, which can result in cancer treatment delays or dose reductions and possibly compromise treatment efficacy; in severe cases, infections can also be life-threatening.20,21 Treatment of infections in patients with cancer may require hospitalization, placing an additional burden on patients, caregivers, HCPs, and health systems.22 It is reasonable to assume that a treatment that takes less time would result in less time spent in a hospital or clinic setting and could thereby reduce patients’ risk of acquiring infections at the treatment facility. This potential benefit may be of particular relevance at the present time, during the COVID-19 pandemic, which poses additional health risks to patients, especially those who are already prone to infection.
Other potential patient benefits of reduced treatment time include increased satisfaction and improved HRQoL. Patient-reported satisfaction in the COLUMBA trial was significantly higher with DARA SC compared with DARA IV.18 Similarly, other studies in the oncology setting have found increased levels of patient satisfaction with SC formulations of rituximab,12,13 trastuzumab,11,23 and bortezomib7 compared with IV administration of these drugs. According to patients, one reason for this increased satisfaction with SC formulations was the faster and more convenient administration time.7,23 In a survey in the community oncology setting, most patients reported that reduced chair time would have a moderate or major positive impact on their lives.24 Studies in various disease states also suggest that when patients are satisfied with their treatment regimen, their treatment compliance is increased.25–27 Conversely, complex and lengthy treatment regimens are cited as a possible reason for reduced compliance and persistence with treatment.25 It is possible that the reduced treatment time for DARA SC may lead to greater patient compliance, which may then be associated with improved overall treatment outcomes.26,28
As current treatment of MM occurs in the outpatient setting, caregivers play a central role in managing patient treatment.29 The duties of caregivers of patients with cancer can include financing and scheduling treatments, and transporting patients to and from the hospital or clinic for treatments. Many caregivers have reported emotional, physical, financial, and employment problems due to these responsibilities.29–32 Caregivers may need to miss work on days when patients with MM are scheduled for treatment,24 and some have reported problems getting time off from their employer or inability to keep employment due to caring for a patient with MM.29,31 Reducing the time required for treatment administrations could therefore relieve some of the burden currently faced by caregivers of patients with MM.
Reduced treatment time also has potential benefits for both HCPs and treatment facilities. The demand for oncology services has increased due to an aging population, and patients are living longer due to the introduction of novel treatments.7,33 This has led to an increased demand for HCPs who treat cancer patients, which has outpaced the current influx of new providers entering the workforce.34 This imbalance highlights the need for more efficient cancer treatments that can free up valuable patient chair capacity, consequently increasing the number of available appointments, reducing waiting lists, and leading to increased overall efficiencies of oncology treatment units. SC treatments may also free up chair time for patients with other cancers who need IV treatments, thereby benefiting other patients as well. It would appear that HCPs are cognizant of this need, as in a study comparing SC vs IV trastuzumab for the treatment of breast cancer, more HCPs reported greater satisfaction with the SC formulation,11,23 citing preparation speed and simplicity as the reasons for this preference.23
This study has several important limitations. Unlike a traditional T&M study in which a trained observer repeatedly measures activities using a stopwatch or other time-measuring instruments, data for our survey were self-reported and are subject to response bias.35 This study utilized a small sample size and convenience sampling from sites that enrolled patients in the COLUMBA study, so results may not be generalizable to other HCPs or clinics. Our study also included “non-observable” activities that were expected to be similar between the IV and SC formulations (such as patient arrival, blood sampling, and physician consultation). Past studies have shown that exclusion of these activities reduces active HCP time, especially for IV formulations,36 so time estimates from this survey may be high, and real “observed” time for IV activities may be lower. Our analyses did not account for the accelerated (90-minute) IV infusion protocol that was recently developed by Barr et al37 as it is unknown how widely this infusion protocol is used. Lastly, other T&M studies in oncology settings have shown a high level of heterogeneity in terms of task decomposition among sites and countries, impacting total HCP time.38 Because a standardized survey was used, differences in workflow and detailed task scope between sites and countries could not be elicited.
Despite these limitations, the results of the current study complement the existing literature on the benefits of SC compared with IV treatment administration in oncology, and provide new insight into the quantity of expected time-saving benefits with DARA SC compared with DARA IV formulations.
Conclusions
Results of this T&M survey suggest the potential for substantial time savings with DARA SC compared with DARA IV. DARA SC was associated with less reported active HCP involvement in drug preparation and drug administration and patient care, and less patient chair usage. Results were confirmed by a sensitivity analysis, which used fully validated data for 18 of the 26 respondents. The reduced active HCP time with DARA SC appears to be maintained over first and subsequent visits, and over Year 1 and Year 2 of treatment. The shorter administration time of DARA SC could lead to reduced burden on patients with MM and their caregivers, as well as create efficiencies for HCPs and oncology treatment facilities, therefore allowing more cancer patients to be treated.
Abbreviations
DARA, daratumumab; HCP, healthcare provider; HRQoL, health-related quality of life; ISR, injection site reaction; IRR, infusion-related reaction; IV, intravenous; MM, multiple myeloma; RRMM, relapsed/refractory MM; SC, subcutaneous; SOC, standard of care; T&M, time and motion.
Acknowledgments
This study was supported by Janssen Global Services, LLC. The authors would like to thank the HCPs who participated in the survey and the staff members involved in data collection. Editorial and medical writing support were provided by Corey Eagan, MPH, of Eloquent Scientific Solutions and were funded by Janssen Global Services, LLC.
Author Contributions
All authors meet the International Committee of Medical Journal Editors criteria for authorship of this manuscript and take responsibility for the integrity of the work as a whole. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
MS, AS, TM, CH, and AL are employees of Janssen. EA and EDC are employees of Syneos Health and were compensated by Janssen for conducting the study. CH has a patent US appl# 62/825,244 pending, a patent US appl# 62/825,252, a patent US appl# 62/825,268, a patent US appl# 62/825,278. Interim results from this survey were presented at the 62nd American Society of Hematology Annual Meeting & Exposition as a poster presentation. The abstract was published in Blood 2020; 136 (supplement 1); DOI: https://doi.org/10.1182/blood-2020-139995.
References
1. Ramsenthaler C, Kane P, Gao W, et al. Prevalence of symptoms in patients with multiple myeloma: a systematic review and meta-analysis. Eur J Haematol. 2016;97(5):416–429. doi:10.1111/ejh.12790
2. Baz R, Lin HM, Hui AM, et al. Development of a conceptual model to illustrate the impact of multiple myeloma and its treatment on health-related quality of life. Support Care Cancer. 2015;23(9):2789–2797. doi:10.1007/s00520-015-2644-6
3. Parsons JA, Greenspan NR, Baker NA, McKillop C, Hicks LK, Chan O. Treatment preferences of patients with relapsed and refractory multiple myeloma: a qualitative study. BMC Cancer. 2019;19(1):264. doi:10.1186/s12885-019-5467-x
4. Seitzler S, Finley-Oliver E, Simonelli C, Baz R. Quality of life in multiple myeloma: considerations and recommendations. Expert Rev Hematol. 2019;12(6):419–424. doi:10.1080/17474086.2019.1613886
5. Szabo K, Bodoki L, Nagy-Vincze M, et al. Effect of genetic and laboratory findings on clinical course of antisynthetase syndrome in a Hungarian Cohort. Biomed Res Int. 2018;2018:6416378. doi:10.1155/2018/6416378
6. Kumar SK, Rajkumar SV, Dispenzieri A, et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood. 2008;111(5):2516–2520. doi:10.1182/blood-2007-10-116129
7. Barbee MS, Harvey RD, Lonial S, et al. Subcutaneous versus intravenous bortezomib: efficiency practice variables and patient preferences. Ann Pharmacother. 2013;47(9):1136–1142. doi:10.1177/1060028013503122
8. Krejcik J, Casneuf T, Nijhof IS, et al. Daratumumab depletes CD38+ immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood. 2016;128(3):384–394. doi:10.1182/blood-2015-12-687749
9. DARZALEX® (daratumumab) injection, for intravenous use [prescribing information]. Horsham, PA: Janssen Biotech, Inc; 2020.
10. Darzalex (daratumumab) [summary of product characteristics]. Leiden, The Netherlands: Janssen Biologics BV; 2020.
11. Pivot X, Gligorov J, Muller V, et al. Preference for subcutaneous or intravenous administration of trastuzumab in patients with HER2-positive early breast cancer (PrefHer): an open-label randomised study. Lancet Oncol. 2013;14(10):962–970. doi:10.1016/S1470-2045(13)70383-8
12. Lugtenburg P, Avivi I, Berenschot H, et al. Efficacy and safety of subcutaneous and intravenous rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone in first-line diffuse large B-cell lymphoma: the randomized MabEase study. Haematologica. 2017;102(11):1913–1922. doi:10.3324/haematol.2017.173583
13. Rummel M, Kaiser U, Balser C, et al. Bendamustine plus rituximab versus fludarabine plus rituximab for patients with relapsed indolent and mantle-cell lymphomas: a multicentre, randomised, open-label, non-inferiority phase 3 trial. Lancet Oncol. 2016;17(1):57–66. doi:10.1016/S1470-2045(15)00447-7
14. Nooka AK, Gleason C, Sargeant MO, et al. Managing infusion reactions to new monoclonal antibodies in multiple myeloma: daratumumab and elotuzumab. J Oncol Pract. 2018;14(7):414–422. doi:10.1200/JOP.18.00143
15. San-Miguel J, Usmani SZ, Mateos MV, et al. Subcutaneous daratumumab in patients with relapsed or refractory multiple myeloma: part 2 of the open-label, multicenter, dose-escalation phase 1b study (PAVO). Haematologica; 2020. doi:10.3324/haematol.2019.243790
16. Clemens PL, Yan X, Lokhorst HM, et al. Pharmacokinetics of daratumumab following intravenous infusion in relapsed or refractory multiple myeloma after prior proteasome inhibitor and immunomodulatory drug treatment. Clin Pharmacokinet. 2017;56(8):915–924. doi:10.1007/s40262-016-0477-1
17. Usmani SZ, Nahi H, Mateos MV, et al. Subcutaneous delivery of daratumumab in relapsed or refractory multiple myeloma. Blood. 2019;134(8):668–677. doi:10.1182/blood.2019000667
18. Mateos MV, Nahi H, Legiec W, et al. Subcutaneous versus intravenous daratumumab in patients with relapsed or refractory multiple myeloma (COLUMBA): a multicentre, open-label, non-inferiority, randomised, phase 3 trial. Lancet Haematol. 2020;7(5):e370–e380. doi:10.1016/S2352-3026(20)30070-3
19. DARZALEX FASPROTM (daratumumab and hyaluronidase-fihj) injection, for subcutaneous use [prescribing information]. Horsham, PA: Janssen Biotech, Inc; 2020.
20. Blimark C, Holmberg E, Mellqvist UH, et al. Multiple myeloma and infections: a population-based study on 9253 multiple myeloma patients. Haematologica. 2015;100(1):107–113. doi:10.3324/haematol.2014.107714
21. Valkovic T, Gacic V, Ivandic J, et al. Infections in hospitalised patients with multiple myeloma: main characteristics and risk factors. Turk J Haematol. 2015;32(3):234–242. doi:10.4274/tjh.2013.0173
22. Tai E, Guy GP, Dunbar A, Richardson LC. Cost of cancer-related neutropenia or fever hospitalizations, United States, 2012. J Oncol Pract. 2017;13(6):e552–e561. doi:10.1200/JOP.2016.019588
23. Lazaro Cebas A, Cortijo Cascajares S, Pablos Bravo S, et al. Subcutaneous versus intravenous administration of trastuzumab: preference of HER2+ breast cancer patients and financial impact of its use. J BUON. 2017;22(2):334–339.
24. Fisher MD, Wallick CJ, Miller PJ, et al. Impacts of time spent on rituximab infusion on patient satisfaction, stress, employment, and caregiver burden. Value Health. 2018;21:S36. doi:10.1016/j.jval.2018.04.303
25. Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48. doi:10.2147/PPA.S24752
26. Price D, Harrow B, Small M, Pike J, Higgins V. Establishing the relationship of inhaler satisfaction, treatment adherence, and patient outcomes: a prospective, real-world, cross-sectional survey of US adult asthma patients and physicians. World Allergy Organ J. 2015;8(1):26. doi:10.1186/s40413-015-0075-y
27. Sweileh WM, Ihbesheh MS, Jarar IS, et al. Self-reported medication adherence and treatment satisfaction in patients with epilepsy. Epilepsy Behav. 2011;21(3):301–305. doi:10.1016/j.yebeh.2011.04.011
28. Small M, Anderson P, Vickers A, Kay S, Fermer S. Importance of inhaler-device satisfaction in asthma treatment: real-world observations of physician-observed compliance and clinical/patient-reported outcomes. Adv Ther. 2011;28(3):202–212. doi:10.1007/s12325-010-0108-4
29. Kurtin S, Lilleby K, Spong J. Caregivers of multiple myeloma survivors. Clin J Oncol Nurs. 2013;17(s6):
30. Armoogum J, Richardson A, Armes J. A survey of the supportive care needs of informal caregivers of adult bone marrow transplant patients. Support Care Cancer. 2013;21(4):977–986. doi:10.1007/s00520-012-1615-4
31. Molassiotis A, Wilson B, Blair S, Howe T, Cavet J. Living with multiple myeloma: experiences of patients and their informal caregivers. Support Care Cancer. 2011;19(1):101–111. doi:10.1007/s00520-009-0793-1
32. Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psychooncology. 2010;19(10):1013–1025. doi:10.1002/pon.1670
33. Erikson C, Salsberg E, Forte G, Bruinooge S, Goldstein M. Future supply and demand for oncologists: challenges to assuring access to oncology services. J Oncol Pract. 2007;3(2):79–86. doi:10.1200/JOP.0723601
34. Sharma D, Wallace N, Levinsohn EA, et al. Trends and factors affecting the US adult hematology workforce: a mixed methods study. Blood Adv. 2019;3(22):3550–3561. doi:10.1182/bloodadvances.2019000307
35. Rosenman R, Tennekoon V, Hill LG. Measuring bias in self-reported data. Int J Behav Healthc Res. 2011;2(4):320–332. doi:10.1504/IJBHR.2011.043414
36. De Cock E, Kritikou P, Sandoval M, et al. Time savings with rituximab subcutaneous injection versus rituximab intravenous infusion: a time and motion study in eight countries. PLoS One. 2016;11(6):e0157957. doi:10.1371/journal.pone.0157957
37. Barr H, Dempsey J, Waller A, et al. Ninety-minute daratumumab infusion is safe in multiple myeloma. Leukemia. 2018;32(11):2495–2518. doi:10.1038/s41375-018-0120-2
38. De Cock E, Pivot X, Hauser N, et al. A time and motion study of subcutaneous versus intravenous trastuzumab in patients with HER2-positive early breast cancer. Cancer Med. 2016;5(3):389–397. doi:10.1002/cam4.573
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.