Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 17
Results and Follow-Up of a Sequential Q-Switched Laser Therapy for Nevus of Ota in Infants
Authors Zheng H, Xu AE, Qiao G, Sun XY, Deng J, Zhang Y
Received 12 October 2023
Accepted for publication 19 January 2024
Published 3 February 2024 Volume 2024:17 Pages 339—347
DOI https://doi.org/10.2147/CCID.S444410
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Rungsima Wanitphakdeedecha
Han Zheng, Ai-E Xu, Gang Qiao, Xiao-Yu Sun, Jia Deng, Yong Zhang
Laser Center, Hangzhou Third People’s Hospital, Zhejiang, 310009, People’s Republic of China
Correspondence: Han Zheng, Laser Center, Hangzhou Third People’s Hospital, No. 38 West Lake Avenue, Hangzhou, 310009, People’s Republic of China, Tel +86-13958159341, Email [email protected]
Background and Aim: There is a dearth of scholarly investigation pertaining to the effectiveness and safety of laser therapy for nevus of Ota manifestation in infants. The objective of this study is to examine the efficacy and safety of administering laser therapy at an early stage to treat nevus of Ota in infants.
Methods: A total of 102 infants below the age of one who had nevus of Ota were treated at the Laser Center at Hangzhou Third People’s Hospital. The treatment approach involved a combination of the Q-switched laser (with a wavelength of 755 nm) and the Q-switched laser (with a wavelength of 1064 nm). The treatment sessions were conducted at six-month intervals. Prior to and after each session, photographs and relevant parameters were documented, including any skin reactions. Subsequent follow-up was conducted through phone calls, WeChat, and text messages, and the parents/guardians of the infants completed a general questionnaire as well as Conner’s Abbreviated Symptom Questionnaire.
Results: Laser therapy exhibited significant efficacy in the treatment of nevus of Ota in infants. Success rates reached 88.7% after four sessions and 99.3% after seven sessions. No instances of serious adverse reactions, except for pain, were reported. Among the 47 infants subject to follow-up, 14 experienced a recurrence, resulting in a recurrence rate of 29.8%. Factors contributing to these recurrences included lesion size, subtypes, exposure to the sun, and location. Subsequent laser treatments, typically involving two to three additional sessions, proved effective in mitigating recurrences. Notably, none of the infants exhibited any signs of fear, anxiety, or other psychological abnormalities following laser therapy, and the overall satisfaction rate was markedly high.
Conclusion: Commencing laser therapy promptly for nevus of Ota in infants is recommended. This early intervention significantly contributes to the overall well-being of infants, addressing both physical and psychological aspects.
Keywords: infants, laser, nevus of Ota, psychology, Q755, Q1064
Introduction
Nevus of Ota, also referred to as oculodermal melanosis, is an intrinsic pigmentation disorder primarily affecting areas innervated by the trigeminal nerve, with a higher prevalence observed among individuals with darker skin tones, particularly within the Asian population.1 Manifesting typically in early childhood, this condition can lead to facial disfigurement, thereby presenting substantial psychological challenges for affected children. The best options continue to be q-switched lasers with wavelengths of 755 nm and 1064 nm.2 Nevertheless, an ongoing discourse persists regarding the optimal initiation timing of treatment in infants, the efficacy of therapeutic interventions, and the potential for adverse reactions.
In light of this context, a retrospective analysis was undertaken, involving 102 infants below 1 year of age who underwent their initial laser treatment. Subsequently, a follow-up was conducted with 47 of these infants, ranging from 2 to 10 years post-treatment. The primary objective of this research was to explore the timing, efficacy, safety, and psychological ramifications of laser therapy in infants afflicted with nevus of Ota.
Study Participants and Methods
Study Participants
From January 2005 to December 2018, 102 infants who had been diagnosed with nevus of Ota and were treated at the Laser Center at Hangzhou Third People’s Hospital were enrolled in this study. Among these infants, 38 were boys, and 64 were girls. Their ages ranged from 1 to 12 months, with an average age of 5.7 months. All infants displayed symptoms of the condition either at birth or within the first month after birth. The temporal manifestation of the condition demonstrated a duration ranging from 2 to 11 months, spanning the interval from birth to the commencement of the initial therapeutic intervention.
The infants were classified using the Tanino classification criteria,3 as follows:
- Type I (17 cases): Skin lesions covered an area of 1 to 10 cm2, involving regions such as the periorbital area, malar region, temporal region, forehead, nasolabial fold, or ala of the nose.
- Type II (59 cases): Skin lesions covered an area of 10 to 60 cm2, involving regions like the periorbital area, zygomatic bone, temporal region, ala of the nose, and cheek regions.
- Type III (24 cases): Skin lesions covered an area of 60 to 110 cm2, spanning across the scalp, forehead, eyebrow arch, temporal region, and nose.
- Type IV (2 cases): Skin lesions exceeded 110 to 220 cm2 or were even larger.
Out of all the cases, 32 had brown lesions, while 70 had blue lesions. Among these cases, 55 had periorbital skin lesions on the affected side, and 46 cases showed involvement of the sclera of the eyeball on the affected side.
Methods
Preoperative Preparation
During the initial appointment, crucial clinical information was meticulously documented, encompassing the child’s name, gender, age at the time of consultation, consultation date, age of onset of the skin lesion, its location, any involvement of the sclera, and the size of the lesion. Parents/guardians provided their consent by signing an informed consent form. Photographs of the skin lesions were systematically taken before and after each treatment session, with concurrent documentation of post-treatment parameters. Prior to each treatment, a meticulous examination of the color of the skin lesion was conducted to identify any pigmentary irregularities or scars. In cases involving infants aged over 3 months, local anesthesia was administered using a topical compound lidocaine cream in 13 instances. The infant was positioned in a supine (lying face up) posture, and the treatment area was thoroughly cleaned. The practitioner prioritized eye protection through the use of goggles, and the infant’s eyes were shielded with moist gauze or an eye mask. The determination of the suitable energy density for treatment was based on the infant’s age, the color and location of the skin lesion, as well as any prior treatment experiences.
Treatment Equipment
A Q-switched alexandrite laser with a 755 nm wavelength and a Q-switched Nd: YAG laser with a 1064 nm wavelength (Cynosure) were used in combination for the treatment. The first two sessions involved the utilization of the Q755 laser with a 3–4 mm spot size and an energy level ranging from 3.0 to 4.0 J/cm2. Subsequently, commencing from the third session onward, the Q1064 laser was employed, featuring a 4 mm spot size and an energy level ranging from 4.0 to 5.2 J/cm2. Treatments were administered at intervals of 6 months, with photographs taken both before and after each session to evaluate the therapeutic impact. The treatment course ranged from one to seven sessions and concluded upon the improvement of the child’s nevus of Ota. Immediate post-laser therapy reactions included skin redness and swelling. Specifically, the Q755 laser induced a surface-level grayish-white response on the skin, while the Q1064 laser predominantly elicited a purpuric reaction. After the procedure, the treated area was cooled with ice for 30 min, followed by the application of gentamicin ointment.
Criteria for Determining Therapeutic Effect and Recurrence
The criteria for assessing the therapeutic outcome4 and identifying recurrence5 are as follows: In the context of pediatric nevus of Ota cases, notable results were observed in terms of pigmentation improvement and reduction in color intensity. The success rate for lesion color fading ranged from 90% to 100%, with a discernible impact ranging from 61% to 89% for color reduction. Additionally, efficacy was noted in the range of 21% to 60%, while ineffectiveness was documented for color reduction below 20%. The cure rate is expressed as follows: Cure rate = number of cured cases/number of treated cases×100%. Whereas the effective rate is determined as follows: effective rate = (number of cured cases + number of cases with apparent effect)/number of treated cases×l00%. Recurrence was defined as the reappearance of nevus of Ota lesions at the original site beyond a period of 6 months following the resolution of the lesions. The criteria used to evaluate new occurrences included the manifestation of nevus of Ota lesions at different anatomical sites during the later stages of the condition after the absence of lesions was noted during the initial visit.
Recurrence is considered when the nevus of Ota skin lesion returns to a previously treated location more than 6 months after the area was deemed to be fully recovered. A nevus of Ota cutaneous lesion, initially overlooked during primary consultation, must additionally manifest in a different anatomical site to satisfy the criterion pertaining to its newfound emergence.
Follow-Up
Between January and March of 2021, we conducted a follow-up study on infants who had undergone successful laser therapy for nevus of Ota. This follow-up was conducted through phone calls, WeChat, and SMS, utilizing a questionnaire to scrutinize various aspects. These encompassed the identification of any recurrence or new emergency of nevus of Ota after the laser therapy, assessing potential side effects, evaluating the child’s psychological well-being, and gauging their satisfaction with the laser therapy. Since the children involved in the study were quite young and could not fully comprehend the questionnaire and psychological assessment scales, their parents provided the answers on their behalf.
To assess the psychological health of the children, Conner’s Abbreviated Symptom Questionnaire (C-ASQ) was utilized, which encompasses areas such as conduct, learning, psychosomatic disorders, and anxiety. The followed-up study participants included 47 children, consisting of 12 boys and 35 girls, with an average age of 5.3 years. Concurrently, a control group was established, which included 31 children of hospital employees. The control group comprised 14 boys and 17 girls, with an average age of 4.8 years. All members of the control group had healthy skin and did not have any significant medical conditions.
Adverse Reactions
Undesirable responses comprise manifestations including heightened skin pigmentation, diminished skin pigmentation, and the formation of discernible scars within a time frame of two to three months subsequent to the therapeutic intervention.
Statistical Methods
Statistical analysis was conducted using SPSS version 17.0 software. Descriptive statistics, such as percentages, were employed for count data, and the chi-squared test was utilized. A P-value < 0.05 denoted statistical significance。
Results
Comparison of Different Subtypes with Treatment Outcomes
Among the 102 children who underwent laser therapy, the effectiveness of the treatment varied based on the number of sessions. Specifically, the efficacy rate increased to 88.7% after 4 sessions and reached 99.3% after 7 sessions. Notably, the effectiveness differed for various subtypes for the same number of treatments (as shown in Table 1). For subtypes I and II, a single treatment yielded a 49.9% efficacy rate, whereas for subtypes III and IV, it was only 25.3%. This difference was statistically significant (P < 0.05), denoting treatment elicited a swifter response in instances characterized by diminutive and focal lesions. After four treatments, subtypes I and II achieved a remarkable 97.3% efficacy rate (refer to Figure 1), while subtypes III and IV required greater than 4 treatments to attain similar results (Figures 2 and 3).
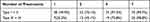 |
Table 1 Comparison of Efficacy Rates Among Different Subtypes After the Same Number of Treatments |
 |
Figure 3 Follow-up process involved in the care of a typical patient. (A) Before treatment; (B) 6 months after the fourth treatment; (C) 3 years after the 5th treatment. |
Comparison of Efficacy Rate After Four Treatments for Nevus of Ota
The laser treatment showed a 30.9% efficacy rate for brown lesions and a 59.1% efficacy rate for blue lesions. This difference in therapeutic effectiveness held statistical significance (P < 0.05), indicating laser intervention demonstrates greater efficacy in addressing blue-black skin lesions compared to brown pigmentation. The cohort of 13 children administered with local anesthesia predominantly comprised type III and type IV cases, constituting 7.6% for 1 case of type I and type II and 92.3% for 12 cases of type III and type IV. Within this group, there were 2 males and 11 females, with an average age at the first treatment of 7.2 months and an average age of onset of 4.6 months. Notably, there was no statistically significant difference in the duration of the disease and the average age of disease onset compared to type III and type IV cases that did not receive external anesthesia. Among those who received topical anesthesia, the efficacy rate was 52.1%, whereas it was 76.7% for individuals who did not receive any anesthesia. This difference in therapeutic outcome also demonstrated statistical significance (P < 0.05). Moreover, it is noteworthy that the efficacy rate for treating the eyelid was comparatively lower than that for the cheek, and, correspondingly, the cheek exhibited a lower efficacy than the forehead, emphasizing once again statistically significant differences (P < 0.05). Further details are available in Table 2.
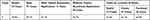 |
Table 2 Comparison of Efficacy Rates for Nevus of Ota Based on Color, Location, and Whether Topical Anesthesia Was Used, After an Average of Four Laser Therapy Sessions |
Among the study cohort, 18 children diagnosed with nevus of Ota experienced the development of fresh lesions around the outer edges of the initial lesion, occurring within a time frame of 6 months to 2 years following their initial laser treatment. These new lesions were predominantly categorized as subtype I and II. Interestingly, the coloration of the lesion in the treated region did not become more intense. Through subsequent rounds of treatment, both the original and newly emerged lesions eventually disappeared. A notable and unfortunate case involved a 4-month-old male infant who underwent laser therapy twice, only to be subsequently diagnosed with intracranial melanoma, and tragically, passed away 3 months later.
Adverse Reactions
Other than discomfort related to the treatment, no additional adverse reactions were observed. There were no cases of scar formation, deepening of pigmentation, or hypopigmentation (Figures 1–3).
Follow-Up
A total of 47 infants and young children diagnosed with nevus of Ota were followed-up. Among them, 12 were males, while 35 were females. On average, the follow-up occurred 3 years after the completion of their laser therapy, with the shortest period being 6 months and the longest period being 15 years. Out of the 47 children, 14 experienced a recurrence, which accounted for approximately 29.8% of the group. There were 14 instances of relapse observed in children, consisting of 5 males and 9 females. The cohort exhibited an average age at the initiation of initial treatment of 6.5 months, with an average age of onset recorded at 2.2 months. Treatment was administered to 21% of cases presenting with type I and II, while the remaining 78.5% involved instances of type III and IV.
One particularly noteworthy case involved a child who had a recurrence 13 years later, possibly linked to changes in hormone levels during puberty. Furthermore, nine children experienced a recurrence within a range of 0.5 to 2 years after treatment. Furthermore, there were five cases where the condition worsened, attributed to factors such as exposure to the sun, trauma, or external injuries. Importantly, all 47 children who were followed up still maintained intact skin. The post-treatment satisfaction rate was high, reaching 95.5%. For more detailed information and visual representations of the results, please refer to Figure 3. Nevus of Ota Type III exhibited the highest post-laser treatment recurrence rate, at 40.9%, with the eyelid area experiencing the most frequent recurrences.
By employing the C-ASQ, no statistically significant differences (P > 0.05) were discerned in the psychological well-being of children who underwent nevus of Ota laser therapy as opposed to those in the control group. For a detailed statistical overview, please refer to Table 3.
 |
Table 3 Comparison of Conner’s Scale Factor Scores Between the Laser Therapy Group and the Control Group (Shown as Mean ± Standard Deviation in Points) |
Discussion
The optimal timing for addressing nevus of Ota in infants has been a subject of contention within the medical community. Divergent viewpoints are present within the medical community, wherein certain practitioners advocate for early intervention, while others assert commencing treatment prematurely may amplify the likelihood of recurrence. The latter proponents endorse a deferred approach, suggesting intervention be postponed until adulthood. During the course of our study, encompassing a retrospective analysis of 102 cases and a subsequent examination of 47 cases, we ascertained laser therapy for nevus of Ota in infants exhibited an overall efficacy rate of 88.7% following 4 sessions. This efficacy rate surpasses figures documented in certain literature pertaining to adult cases.6
Lin et al5 observed a significant improvement in the therapeutic efficacy of laser intervention for nevus of Ota in pediatric patients, illustrating a noteworthy increase of 96.15% with each successive treatment session. Moreover, their findings revealed an inverse relationship between the age at which the child underwent initial treatment and the requisite number of treatments for achieving a cure, with a lower age correlating with a reduced treatment frequency. In a related study, Wang et al7 recorded a cure rate of 97.26% following 10 laser sessions. The efficacy of laser treatment, as demonstrated in the current study, reached 99.3% after 7 treatments. Significantly, the results of our study revealed an average age at the time of the initial treatment selection of 5.33 months, highlighting a proclivity for initiating interventions at an early stage.
The enhanced efficacy of laser therapy in infants can be attributed to the presence of fewer and shallower pigments in early-stage nevus of Ota, as well as the thin and metabolically active skin in infants, which allows for faster pigment absorption.6 As a result, treatments administered to infants yield expeditious outcomes. Throughout our investigation, it was observed that nevus of Ota types I and II exhibited a remarkable efficacy rate of 97.3% after only 4 treatment sessions, indicating substantial improvement in a considerable number of patients. However, for types III and IV, more than 4 sessions were necessary, with the efficacy rate reaching 99.3% after 7 sessions, aligning with the efficacy rate reported for adults in literature.6
Furthermore, it is crucial to emphasize the adoption of a retrospective design in the present study, and the absence of antecedent experiences with picosecond treatment. Ohshiro et al8 documented the safety and efficacy of the picosecond emerald-green laser in addressing nevus of Ota. Chesnut et al9 observed discernible enhancements in three individuals who, having undergone multiple Q-switched laser treatments without significant responses for nevus of Ota, exhibited marked improvement following 2 to 3 sessions of picosecond emerald-green laser treatment. The results suggest that the application of picosecond laser technology holds promise for augmenting therapeutic effectiveness and reducing the necessary frequency of interventions in the management of nevus of Ota among pediatric patients in prospective clinical contexts.
In our retrospective analysis, the order of efficacy after four laser treatments was as follows: eyelid < cheek < forehead, indicating a statistically significant difference in therapeutic effect (P < 0.05). The diminished pace of chromatic attenuation within the orbital region under laser therapy, relative to adjacent anatomical regions, can be ascribed to the distinctive tissue architecture inherent to the particular anatomical locale.10 In some cases, to ensure safety, treatment of sensitive areas like the eyelid may need to be temporarily paused and resumed once the child can cooperate better. Moreover, our investigation findings indicate that laser therapy exhibited a pronounced level of safety, with the sole noteworthy adverse effect being discomfort. Consequently, patients conveyed a heightened satisfaction level regarding the administered treatment.
Lin et al5 reported a recurrence rate of 15.4% for nevus of Ota in children. They correlated the recurrence with the age of onset, suggesting a higher likelihood of recurrence in younger children. Similarly, Wang et al7 demonstrated a recurrence rate of 16.67%, with a focus on early age of onset as a contributing factor. In our study, the observed recurrence rate of 29.8% is deemed to be associated with the early age of onset (average age of onset being 2.2 months) in the followed-up cases. The higher recurrence rate in 14 cases can be attributed to the predominance of type III and type IV cases, accounting for 78.5% of the cases.
There were 14 cases (29.8%) of recurrences among the 47 follow-up cases, which is higher than what has been noted in studies on adults.6 The susceptibility of a child’s immature skin, combined with the heightened vulnerability of younger individuals to nevus of Ota, represents one potential causative factor. Studies by Wang et al11 and Hidano et al,12 investigating 131 and 240 cases, respectively, identified early childhood and adolescence as the two primary peak periods for the onset of nevus of Ota. We hypothesize that variations in hormone levels during puberty may contribute to the recurrence observed in one case in our study, occurring 13 years after therapy.11 Additionally, four cases exhibited worsening following exposure to sunlight or trauma. Hori suggests that interactions between existing dermal melanocytes and epidermal melanocytes result in a depletion of epidermal melanin due to their migration to hair follicles.13 External variables, including topical hormones, exposure to the sun, cosmetics, trauma, and dermal inflammation, have the potential to amplify melanin in specific facial regions,14 leading to the new emergence or recurrence of nevus of Ota. Consequently, it is crucial to emphasize the importance of protection from the sun and the avoidance of skin damage following nevus of Ota treatment.
In addition, nine cases—with an average of less than 2 treatments—experienced recurrences between 6 months and 2 years after therapy. This suggests a direct link between recurrence and the insufficient number of treatments. The subtype and location have an impact on the recurrence rate as well. For instance, type III nevus of Ota has the highest risk of recurrence,15 perhaps due to the larger coverage of skin lesions, which can lead to potential mistakes during laser scans. As the most frequent site of recurrence and a sensitive location, the eyelid demands extreme caution during treatment to protect the eyes. Treatment for this area may sometimes need to be terminated, which leads to fewer treatments and eventual recurrence. Therefore, the recommendations from the follow-up are as follows: before the procedure, it is essential to inform parents about the possibility of new emergence and recurrences. During laser therapy, meticulous attention should be given to cover all areas, and a slight overlap is recommended in selecting appropriate parameters for comprehensive treatment. Ideally, the number of treatment sessions should exceed four. Following the treatment, it is crucial to avoid sun exposure, trauma, and other external injuries to prevent recurrence.
The mental health of children is more important than ever in this modern era, which is marked by an advanced materialistic society. Children afflicted with nevus of Ota, a condition associated with a heightened propensity for facial disfigurement, may encounter sentiments of inadequacy, particularly during critical developmental milestones such as the initiation of daycare or formal schooling. These emotions could have adverse effects on both their mental and physical health, manifesting as social challenges.16 Given the young age of the children, they often cannot understand or respond to psychological assessment questionnaires. Therefore, these questionnaires were filled out on their behalf by their parents or legal guardians. The C-ASQ was used as the reference scale in this study. The outcomes revealed a lack of statistically significant differences among the pediatric patients who underwent laser therapy for nevus of Ota in comparison to the participants in the control group across all measured factors (P > 0.05). These findings indicate that laser intervention does not induce psychological apprehension in pediatric patients. Furthermore, the timely application of laser therapy serves as a preventive measure against the psychological ramifications associated with nevus of Ota among school-age children. These children exhibited no indication of diminished self-esteem and demonstrated a capacity to engage in normal social interactions within educational environments. Such outcomes contribute to the overall well-being of affected children, fostering both physical and mental health throughout their developmental stages.
In our retrospective study, we observed a greater demand for treatment sessions to achieve resolution among infants with nevus of Ota (13 cases) who underwent laser therapy with topical anesthetic compared to those without the administration of anesthetic. The application of a topical anesthetic may induce epidermal swelling, potentially impeding the laser’s ability to penetrate deeply and diminishing the rate of pigment eliminationInfants are frequently assumed to be incapable of experiencing or recalling pain due to the incomplete maturation of their neural systems. However, despite the absence of behavioral or psychiatric issues in the observed children, studies suggest that early-life encounters with pain can have both immediate and lasting effects on an individual.17 Therefore, it is essential to consider pain management during laser therapy for nevus of Ota in infants.
Infants can experience pain relief through intravenous anesthetics, but there are also additional risks associated with the procedure. Conversely, empirical evidence indicates a significant decrease in the efficacy of laser treatment when using topical anesthetics, necessitating additional sessions to achieve the desired outcomes. Consequently, it is advisable to consult with parents early in the decision-making process regarding the use of anesthetics. Additionally, infants younger than 3 months of age and anyone receiving treatment with high ferritin hemoglobin inducers should not be administered topical anesthetics. Based on our findings, we recommend contemplating the use of topical anesthesia for infants aged 3 months and older. It appears more suitable to initiate an initial laser therapy session for nevus of Ota after this age and subsequently apply topical anesthetic as needed.
Based on the results of our retrospective study, blue-black skin lesions appear to respond more favorably to laser treatment than brown ones. Notably, Q755 lasers exhibit a great affinity for blue-black pigments. Owing to its pronounced affinity for pigments and expeditious efficacy, commencing the treatment regimen with the Q755 laser during the initial two to three sessions emerges as the optimal course of action. The Q1064 laser can then be used in subsequent treatments to focus on deeper-seated pigments and possibly help avoid recurrence. However, further investigation is required to fully validate this approach.
The unfortunate death of an infant patient with cerebral melanoma during therapy raises significant concerns, underscoring the crucial need for regular follow-up after nevus of Ota laser therapy. Timely care is essential if any unusual pigment skin abnormalities emerge following treatment. To rule out the presence of malignant tumors, a pathology biopsy should be conducted whenever practical.
The nevus of Ota laser therapy method has substantially improved. The best options continue to be Q-switched lasers with wavelengths of 755 nm and 1064 nm.18 While instances of relapse and the development of new lesions following therapeutic interventions have been observed, highlighting the distinctive features of recurrent lesions becomes crucial. Specifically, these features may include a lighter hue and a reduced area of coverage compared to the original lesion. As a result, the patient often has less pain during successive laser sessions. Satisfactory results can be obtained even if additional two or three laser sessions are required. More importantly, early intervention shields the child from possible psychological effects. Early nevus of Ota treatment can help a child feel less inadequate or insecure, ultimately boosting their self-confidence.
Conclusion
When treating nevus of Ota in pediatric patients, deeming the potential for recurrence as a significant impediment to laser therapy is considered unwarranted. We advocate for the prompt initiation of laser therapy when an infant reaches the age of 3 months. To elaborate, the timely initiation of therapeutic interventions, coupled with preventive measures and sustained, comprehensive long-term monitoring, not only enhances the physical and emotional well-being of a child with nevus of Ota, but also contributes to a healthier home environment.
Data Sharing Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Hangzhou Third People’s Hospital (2021KA039). A written informed consent was obtained from legal guardians of all participants.
Consent for Publication
Consent for publication was obtained from every legal guardians whose data and images are included in this manuscript.
Acknowledgments
We are particularly grateful to all the people who have given us help for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang JB, Wang HW. Skin Laser Cosmetic Treatment. Beijing: Tsinghua University Press; 2004:37–38.
2. Zhao XZ, Ji YL, Ma BB, et al. Clinical analysis of Q-switched emerald laser treatment for nevus of Ota Chinese. J Med Aesthet Beauty. 2002;8(5):26l–262.
3. Tanino H. Nevus fuscoceruleus ophthalmomaxillaris Ota. Jpn J Dermatol. 1939;46:435–451.
4. Lin XH, Shao XH, Yang Y, Cai JF. Analysis of recurrent cases of nevus of Ota after Q-switched 755nm laser treatment. Chin J Aesthet Med. 2005;14(5):617–618.
5. Lin T, Zhou ZC, Gong XD, et al. Retrospective analysis of laser treatment for nevus of Ota in children. Chin Cosmet Med. 2010;6:865–867.
6. Yang YC, Guo ZH. Analysis of the therapeutic effect of Q-switch emerald laser on 220 cases of nevus of Ota with different colors. Chin J Aesthet Med. 2010;19(10):1519–1520.
7. Wang Y. Retrospective analysis of laser treatment of nevus of Ota in children. J Clin Med Lit. 2018;5(48):56.
8. Ohshiro T, Ohshiro T, Sasaki K, et al. Picosecond pulse du ration laser treatment for dermal melanocytosis in Asians: a retrospective review. Laser Ther. 2016;25(2):99–104. doi:10.5978/islsm.16-OR-07
9. Chesnut C, Diehl J, Lask G. Treatment of nevus of Ota with a picosecond 755-nm alexandrite laser. Dermatol Surg. 2015;41(4):508–510. doi:10.1097/DSS.0000000000000326
10. Hague JS, Lanigan SW. Laser treatment of pigmented lesions in clinical practice: a retrospective case series and patient satisfaction survey. Clin Exp Dermatol. 2008;33(2):139–141. doi:10.1111/j.1365-2230.2007.02574.x
11. Chan HH, Lam LK, Wong DS, et al. Nevus of Ota: a new classification based on the response to laser treatment. Lasers Surg Med. 2001;28(3):267–272. doi:10.1002/lsm.1049
12. Wang ZZ, Wei LK, Mou XL. Analysis of the onset time of nevus of Ota. Chin J Med Aesthet. 1998;1998;153–154.
13. Hidano A, Kajima H, Ikeda S, et al. Natural history of nevus of Ota. Arch Dermatol. 1967;95(2):187–195. PMID: 6018994. doi:10.1001/archderm.1967.01600320043006
14. Hori Y, Kawashima M, Oohara K, et al. Acquired, bilateral nevus of Ota-like macules. J Am Acad Dermatol. 1984;10(6):961–964. doi:10.1016/S0190-9622(84)80313-8
15. Long TF, Liu L, He L, et al. Androgen, estrogen and progesterone receptors in acquired bilateral nevus of Ota-like macules. Pigm Cell Melanoma Res. 2010;23(1):144–146. doi:10.1111/j.1755-148X.2009.00644.x
16. Weng WL, Li Q, Yu WL. Number of recurrent cases of nevus of Ota treated with Q-switched laser. J Clin Dermatol. 2012;41(1):53–55.
17. Qian G, Yu BQ, Li LN, et al. Clinical analysis of nevus of Ota and investigation of social psychology among adolescent patients The Chinese. J Dermatovenereol. 2009;23(10):667–668.
18. McPherson C, Miller SP, El-Dib M, et al. The influence of pain, agitation, and their management on the immature brain. Pediatr Res. 2020;88(2):168–175. doi:10.1038/s41390-019-0744-6
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


