Back to Journals » Patient Preference and Adherence » Volume 17
Respecting the Patient’s Right to Information in Hospital Wards in Poland – Socio-Economic Determinants of Patients’ Opinions
Authors Borowska M, Augustynowicz A, Olszewski P, Religioni U
Received 26 June 2023
Accepted for publication 18 August 2023
Published 18 September 2023 Volume 2023:17 Pages 2311—2323
DOI https://doi.org/10.2147/PPA.S421336
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Mariola Borowska,1 Anna Augustynowicz,1,2 Paweł Olszewski,3 Urszula Religioni2
1Department of Economics of Health and Medical Law, Medical University of Warsaw, Warsaw, Poland; 2School of Public Health Centre of Postgraduate Medical Education of Warsaw, Warsaw, Poland; 3Lazarski University in Warsaw, Warsaw, Poland
Correspondence: Mariola Borowska, Department of Economics of Health and Medical Law, Medical University of Warsaw, Warsaw, 02-091, Poland, Email [email protected]
Background: Implementation of the patient’s statutory right to information is one of determinants the quality and safety of medical services. The patients’ opinions survey is an element of patient-centric care, which is now one of the most important things in modern healthcare. The main aim of the work is to examine patients’ opinions on the observance of patients’ right to information in the hospital and quality of healthcare in the hospital. A secondary objective was to examine the impact of socioeconomic variables on patients’ opinions.
Materials and Methods: The study was based on the Computer-Assisted Web Interview (CAWI) questionnaire, carried out in March 2022. The sample included 801 persons. Respondents were patients hospitalized within a maximum of 12 months. The questionnaire contained closed questions about the quality of medical care, observance of the patient’s right to information.
Results: Probability of referral was measured using the Net Promoter Score (NPS). Respondents answered the question about the recommendation on a scale from 0 to 10. People who rated the hospital ward at 10 and 9 are promoters, people who rated the hospital ward at 8 and 7 are neutral people. In turn, people who rated the hospital ward at 6, 5, 4, 3, 2, 1 or 0 are critics, ie people who will not recommend the hospital to their relatives. Most patients in hospital wards were the detractors (37%). The percentage of promoters was only 1% lower (36%) than that of the detractors. Patients was rated medical and nursing staff at a similar level with regard to the observance of the patient’s right to information.
Conclusion: Most statistically significant differences in the assessment of medical care in the hospital ward were associated with such sociodemographic variables as age and income. People aged 55– 64 and 65+ rated most of the analyzed aspects better.
Keywords: patients’ rights, right to information, health care quality, patient, patient experience
Background
The availability and quality of medical services are key aspects for the functioning of health care systems with regard to the socio-economic conditions and demographic trends in developed countries.1 In its numerous publications, the World Health Organization indicates that health care systems should, be ready for a change in the directions of clinical care, and put emphasis on the quality-oriented health care.2 The World Health Organization defines quality of health care as care that is effective, efficient, integrated, patient-centered, equitable and safe. The extent to which the quality of health care can be described as acceptable depends on the ability of services to meet the needs of users and adapt to the expectations and needs of patients.1–3 According to the guidelines of the World Health Organization, quality in healthcare is defined on many levels and includes areas such as outcome, use of available resources, including economic resources, the way services are organized and the level of patient satisfaction.4,5 In health care, quality is defined not only according to material criteria, but also according to sociological and psychological criteria and concepts. In the health care system, quality is assessed on the basis of material, psychological and sociological criteria. It involves the use of all the necessary achievements of satisfy people’s needs, and it means care that is available, accepted, comprehensive, continuous and documented, thus being a confirmation between the criteria of care and the care itself, the effective operation of health care to increase the level of health and satisfaction from healthcare in a population.6–9The survey of patients’ opinions is an element of patient-centric care, allowing the patient to participate in the treatment process and adjusting units to accreditation standards.8,10,11
The concept of patients’ rights was developed on the basis of the Universal Declaration of Human Rights adopted in 1948 by the United Nations General Assembly (UN), which unequivocally states that every human being has the inherent right to life, freedom, privacy, free development in society and respect for their dignity. The purpose of the concept of patients’ rights is to protect the patient’s autonomy against the interference of others, as well as the right to demand appropriate conditions for the exercise of these rights.12,13 Patients’ rights are a set of norms guaranteed by the state to every human being. These rights result from the use of health services and define the standards of work of medical staff. They include the right to health protection, immediate medical assistance due to a threat to the patient’s health or life, intimacy and respect for personal dignity during the provision of health services, dying in peace and dignity, pastoral care, obtaining accessible information about health, expressing consent to the medical examination and many others. Patient rights are important not only from the perspective of the patient who receives a high-quality service, but also from the perspective of the professional performance of duties by medical staff.14–16 The basic patient’s right is the right to consent (or object) to the proposed medical procedures. This applies to both treatment and diagnostics, prevention, rehabilitation and other health care services. The situations in which treatment can be performed despite the patient’s objection are very limited.14 The right to consent to the provision of a health service is related to the right to information, because it is impossible to make the right decision without having the right information. Each patient who uses health services or applies for them has the right to obtain information. In addition, the information provided by medical personnel should be clear and understandable. The doctor should provide information about the diagnosis, suggested and possible diagnostic and therapeutic methods and the foreseeable consequences of their use or non-use, as well as about the treatment results and prognosis. If a patient does not want to be informed about all or some of the facts concerning their health, they also have the right not to be provided with this information. The patient has the right to name a person or persons who will be provided information about the patient’s health and treatment by the doctor.14 Implementation of the patient’s statutory right to information determines the quality and safety of the services provided the medical entity.15
Accreditation standards are significant factors that define the way of providing medical care, affect the awareness of medical professionals, and the management of health care facilities affect not only the medical staff, but also the management staff of the medical entity. The accreditation requirements for hospitals include the Quality Improvement and Patient Safety. Improvement of the quality of care involves continuous monitoring, analysis and improvement is based on continuity in the process of control, analysis and improvement of clinical processes and management stewardship. Quality improvement is aimed at reducing risk for both patients and care providers. It is achieved through the monitoring and assessment of the performance of an entity (quality indicators), on the basis of which specific improvement methods are implemented on the basis of which the management of the facility can apply supporting and improving activities. Improvement is conditioned by the knowledge of the current quality monitoring. Therefore, it is necessary to measure the performance of an entity, ie to collect relevant data according to reliable methodologies, evaluate and analyze the data, determine the changes that should be introduced for improvement, implement them, ie obtain data allowing to draw conclusions about quality and organization, evaluate this data, and prepare a project of changes and implement and make new measurements in order to determine whether the introduced change has translated into improvement. Thanks to the research on the quality of medical care and patient satisfaction, the medical entity not only meets the accreditation standards, but above all responds to the changing needs of patients and adapts to the environment in which it operates to the changing environment related to socio-demographic variables and a number of economic factors affecting the environment in which the medical entity operates.11,17–19
In the 21st century, we treat health as a potential and a derivative of the conditions in which people live. The aim of the system is to optimize health and improve it for the entire population. With the change in the rules of operation of the centrally planned system financed from the state budget to a system financed with funds from the from health insurance, the increase in patients’ expectations, the implementation of legal regulations related to patients’ rights and changes in the rules of operation of providers has increased interest in research on the level of expectations and satisfaction of patients. In recent years, there has been an increase in interest in research related to the quality of health services. The obtained results have a cognitive and practical aspect, as they allow for taking effective action to improve the quality of health care. Limitations of current knowledge in this field is that if we want to reach credible and measurable results that can be the basis for introducing changes in the organization we must examine this kind of information periodically. A one-off examination does not provide us with a periodic state of quality and information and compliance with patient rights in the hospital. That is why we have prepared a study that we conducted on a specific sample and we want to carry it out periodically.
The aim of the study is to examine patients’ opinions on the observance of patients’ right to information in the hospital and quality of health care in the hospital. This allows you to identify areas for improvement in quality and safe. Observing the rights of the patient determines the safety and quality of medical care in the medical entity and enables the identification of areas requiring reorganization in the entity. The secondary objective was to observe of socioeconomic variables in connection with patients’ opinions, including gender, age, place of residence, education level, employment status, and salary. These data can provide information on which groups of patients need to increase the scope of information obtained in wards.
Materials and Methods
The study was based on the CAWI conducted on an online consumer panel. It was performed in March 2022. In the panel, users are kept informed about emerging surveys, if they meet the criteria for their completion. The authors of the study carried out the study themselves using the wizard. The sample was purposive. The sampling was supported by a random sampling algorithm for respondents meeting the sample criteria. Respondents were hospitalized patients who met the inclusion criteria was used. This was hospitalization in the past 12 months.
The uniform method of implementing the survey avoids the influence of the survey method on the results. The survey contains 14 closed questions and one open question. Six of the survey questions are derived from accreditation standards. Patient-defined comprehensiveness is high. The first question in the survey is used to determine the value of the Patient Recommendation Index. The open-ended question allows for feedback on the reasons for patient satisfaction/dissatisfaction with the care. The survey was validated, as part of the oopiece.pl project, during which the survey was conducted on the given questionnaire, as part of a nationwide survey of patient satisfaction with hospital care.
The research tool was a standardized questionnaire, divided into two parts. The first part dealt with quality issues in care, including whether medical staff treat patients with respect, how patients’ pain is treated, and whether ancillary services, such as meal delivery, maintain standards of hygiene and freshness. Local conditions were also asked. Another element was the issue of respecting the patients’ right to information, ie whether the medical staff informed patients about the possibilities of diagnosis and treatment, whether they involved patients in the treatment process, whether they spoke clearly and understandably. The second part concerned socio-economic data.
It was examined what affects the quality and safety perceived by patients, the general opinion of the patient about the hospital and his willingness to recommend the hospital/hospital ward to his relatives. Probability of referral was measured using the Net Promoter Score (NPS). Respondents answered the question about the recommendation on a scale from 0 to 10. People who rated the hospital ward at 10 and 9 are promoters, people who rated the hospital ward at 8 and 7 are neutral people. In turn, people who rated the hospital ward at 6, 5, 4, 3, 2, 1 or 0 are critics, ie people who will not recommend the hospital to their relatives, and may even recommend not using a given medical facility due to its low quality. In order to obtain a full picture of the quality of the service, the questions with a response scale of 0–10 were accompanied by an open, qualitative question, which was intended to justify the result on the response scale. The key issue that provided the most valuable information was an open question about the reason for your satisfaction or dissatisfaction. All responses from the open-ended question were analyzed and the data aggregated according to those responses that appeared most frequently. Several such types of answers that appeared most frequently were classified.
The determinants of the implementation of the patient’s right to information (pursuant to Article 9 of the Act on Patient Rights and the Ombudsman for Patients’ Rights) were analyzed. It was verified whether the medical staff (medical and nursing staff separately) actively listened to the patient during each conversation and whether the information about patient’s health, treatment, care activities and medical interventions was passed on in a way that was understandable and clear to the patient. In addition, it was analyzed how often, during the qualification for a medical procedure and/or hospitalization, the medical staff informed the patient about possible methods of treatment and their consequences, and asked the patient for their opinion while deciding on treatment methods.
Answers to individual questions on the observance of the patient’s right to information were classified on the following scale: never, sometimes, usually, always.
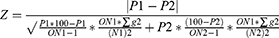
Only statistically significant results were presented in the study. The standard confidence level was 95%. Hypotheses regarding the value of proportions in the population of respondents were verified and the proportions in individual populations were compared, based on the proportions in a random sample (or two or more samples) of a given population. The significance count takes into account the percentage as well as the sample size, in this case significance versus total. We use NIPO Diana program.
ON is the total unweighted sample size; N is the weighted sample size; there is accumulated using the weighted factor g.
Results
The sample consisted of 801 adult persons, including 57% women and 43% men. The largest group of respondents were persons aged 25–34 (28%) and those aged 35–44 (22%). Respondents aged 55–64 accounted for 11% and those over 65 years of age accounted for 10% of the sample. Higher education was declared by 44% of the respondents, including 59% women and 41% men. Secondary education was declared by 43% of respondents, including 55% women and 45% men, and primary education was declared by 13% of respondents, including 53% women and 47% men. The biggest number of respondents were inhabitants of rural areas (21%) and cities with more than 500,000 inhabitants (17%). Regarding the professional status, employed persons accounted for 69%, and the unemployed ones for 31% (the answers unemployed / not working refer to people who are unemployed and people who are retired) of the research sample. The average net income of up to PLN 3000 was declared by 37% of the respondents, and the income of over PLN 5000 was declared by 20% of the respondents. 12% of the respondents refused to provide an answer to the question about their net income. Statistically significant differences were identified to the greatest extent in relation to the age of the patients. People aged 55–64 and 65+ significantly more often positively assessed their stay in a hospital ward.
Patients were asked whether they would recommend a hospital/hospital ward to their family and friends. The respondents were not only asked to give an answer on a scale 0–10, but also to justify the score and indicate in an open-ended question why they would or would not recommend the hospital ward. 36% of the respondents were promoters, 27% were neutral respondents, and 37% were detractors. The detractors mainly criticized long waiting time for hospital admission, poor quality of medical and nursing care, and tasteless meals. Some of the detractors also indicated highly important factors that could have affected the poor quality of care such as the shortage of medical staff, and too heavy workload on medical staff. The study was conducted in the time of the pandemic, which is why some patients indicated no possibility of being visited by family as a considerable drawback. The promoters pointed to the high quality of medical and nursing care and good hospital conditions.
Considering the patient’s right to information, the patients were asked whether the medical staff listened to them with interest during their hospital stay. The results for nursing and medical staff have been presented separately, as staff provide different types of information to the patient. Nurses/midwives inform about the medical interventions and other medical activities and care activities. Doctors make the qualification for a medical procedure and/or hospitalization and about the possible methods of treatment and their consequences. The results are presented in two categories, with regard to medical and nursing staff (Table 1).
 |
Table 1 During Your Hospital Stay, How Often Did the Medical Staff Representatives Listen to You with Interest? |
Detractors (NPS scale) significantly more often indicated that the medical staff never listened to them with interest, both the medical staff (16%) (p=0.0001; SD=0.826) and nursing staff (21%) (p=0.0001; SD=0.826). The answer “sometimes” was declared in this group significantly more often (46% and 45% with regard to medical staff and nursing staff, respectively) (p=0.0001; SD=0.826, p=0.0001; SD=0.826). Promoters (NPS scale) claimed significantly more often that the medical staff always listened to them with interest (53% and 56% with regard to medical staff and nursing staff, respectively) (p=0.0001; SD=0.714, p=0.0001; SD=0.712). The biggest number of statistically significant differences were observed when analyzing the demographic data according to the respondents’ age. The highest values were found in persons aged 18–24 and 55–64. Young persons aged 18–24 increasingly more often declared that both the medical and nursing staff never listened to them with due interest. Persons aged 55–64 significantly more often declared that both the medical and nursing staff always listened to them with due interest (40% and 43%, respectively) (p=0.04957; SD=0.820), p=0.01968; SD=0.931). Respondents’ answers were also analyzed with regard to their monthly net salary. Statistically significant differences were observed in persons with the net income of more than PLN 5000. They indicated the answer “never” and “sometimes” significantly less often. Persons with the net income PLN 3001–5000 significantly less often indicated (26%) (p= 0.0001; SD=0.946) that the nursing staff always listened to them with due interest.
Another important determinant of the observance of the patient’s right to information is providing the patient with the information about medical interventions, their health condition and treatment in a clear and understandable way, using a language accessible to the patient. The question about the medical staff focused on providing the patient with information on their health condition and treatment (Table 2).
 |
Table 2 During Your Hospital Stay, How Often Did Doctors Inform You, in an Understandable Way, About Your Condition and Treatment Management? |
Promoters (NPS scale) declared significantly more often that the medical staff informed them in a clear and understandable way about their health condition and treatment (62%) (p=0.01236; SD=0.723). They also significantly less frequently indicated that the medical personnel had never talked to them in a clear and understandable way about their health condition and treatment (2%) (p=0.00036; SD=0.723). Detractors (NPS scale) declared significantly more often that the medical staff never (18%) (p=0.00001; SD=0.947) and sometimes (36%) (p=0.00001; SD=0.947) informed them in a clear and understandable way about their health condition and treatment. An analysis of the age of the respondents showed statistically significant differences in the younger age groups (18–24 years) and in the older age groups (55–64 years). Persons aged 18–24 indicated significantly more often that during their stay in the hospital, the medical staff never (14%) (p=0.02926; SD=1.025) informed them in a clear and understandable way about their health and treatment, and significantly less often that the medical staff always (29%) (p=0.04862; SD=1.025) informed them in a clear and understandable way about their health and treatment. Persons aged 55–64 significantly more often indicated that the medical staff always (55%) (p=0.00079; SD=0.899) talked to them about their health and treatment in an accessible and understandable way.
With regard to the nursing staff, the patient was asked about being informed about the medical interventions and other care activities (Table 3).
 |
Table 3 During Your Hospital Stay, How Often Did the Nurses, Midwives Inform You, in an Understandable Way, About the Procedures and Other Activities Being Performed? |
Promoters (NPS scale) declared significantly more often that during their hospital stay, the nursing staff informed them in a clear and understandable way about treatments and other care activities (58%) (p=0.00001; SD=0.703). They also significantly less often indicated that the nursing staff had never talked to them about nursing activities and procedures in a clear and understandable way (2%) (p=0.00559; SD=0.703). Detractors (NPS scale) declared significantly more often that the nursing staff never (17%) (p=0.00001; SD=0.930) and sometimes (38%) (p=0.00001; SD=0.930) informed them in a clear and understandable way about procedures and other care activities. An analysis of the age of the respondents showed statistically significant differences in the younger age groups (18–24 years) and in the older age groups (55–64 years). Persons aged 18–24 significantly more often indicated that the nursing staff never (14%) (p=0.00767; SD=0.993) informed them and significantly less frequently indicated that the staff always (25%) (p=0.01730; SD=0.993) informed them about the medical procedures in a clear and understandable way. Respondents aged 55–64 significantly more often indicated that they were always (49%) (p=0.01463; SD=0.906) clearly and comprehensibly informed by the nursing staff about the care activities and interventions.
The right to information also includes access to full information about possible treatments and their consequences. The patients’ opinion was examined on how often the medical staff informed the patient about the possible methods of treatment and their consequences during the qualification for a medical procedure and/or hospitalization (Table 4).
 |
Table 4 During Your Qualification for Surgery and Hospital Stay, How Often Did Your Doctors Inform You About Possible Treatment Options and Their Consequences? |
Promoters (NPS scale) declared significantly more often that the medical staff always (63%) (p=0.00001; SD=0.708) informed them about possible methods of treatment and their consequences during the qualification for a procedure and/or hospitalization. Detractors significantly more often declared that the medical staff never (20%) (p=0.00001; SD=0.996) informed them about possible treatment methods and their consequences during the qualification for a procedure and/or hospitalization. Considering the age of respondents, statistically significant differences were observed in the age group of 18–24 years old. Persons from this age group significantly less frequently indicated that the medical personnel always (28%) (p=0.01942; SD=1.033) informed them about the possible methods of treatment and their consequences during the qualification for a procedure and/or hospitalization. Persons aged 65+ significantly more often indicated that the medical staff always (51%) (p=0.03677; SD=0.886) informed them about possible methods of treatment and their consequences during the qualification for a medical procedure and/or hospitalization.
Participation in the treatment process is another important determinant for the observance of the patient’s right to information. It was analyzed how often the medical staff asked the patient for their opinion while choosing treatment methods during the qualification for a medical procedure and/or hospitalization (Table 5).
 |
Table 5 During Your Qualification for Surgery and Hospital Stay, How Often Did Doctors Ask Your Opinion When Choosing Treatment Methods? |
Promoters (NPS scale) significantly more often declared that the medical staff always (43%) (p=0.00001; SD=1.019) and significantly less often that they never (12%) (p=0.00077; SD=1.019) asked patients for their opinion when choosing treatment methods during the qualification for a procedure and/or hospitalization. Detractors (NPS scale) significantly more often declared that the medical staff never (34%) (p=0.00001; SD=1.036) and sometimes (29%) (p=0.00153; SD=1.036) asked the patients for their opinion when choosing treatment methods during the qualification for a procedure and/or hospitalization. With regard to age, statistically significant differences were observed mainly in the age groups of 25–34- and 55–64-year-olds. Persons aged 25–34 significantly less often indicated that the medical personnel never (16%) (p=0.04982; SD=1.061) asked them for their opinion when choosing treatment methods during the qualification for a procedure and/or hospitalization.
Discussion
Our research shows that the majority of patients staying in hospital wards in Poland are opponents (37%) who would not recommend the facility to others. Importantly, however, the percentage of promoters, ie people who rated the hospital ward highly, was only 1% lower (36%) than the percentage of critics.
Interestingly, the assessment of medical care in the hospital ward was associated with such sociodemographic variables as age and income. People aged 55–64 and 65+ rated most of the analyzed aspects better.
According to the Beryl Institute, patient experience is the sum of all interactions, shaped by an organization’s culture, that influence patient feelings across the healthcare continuum.20 Due to sociodemographic variables the opinion of patients on the observance of the patient’s right to information and the quality of care in the hospital ward was different. People aged 55–64 and 65+ rated most of the analyzed aspects better, including active listening by the medical staff, informing the patient about their health condition, diagnostic and therapeutic procedures and care activities in a clear and understandable way, asking the patient for their opinion when choosing treatment methods. In a study of respect for patient rights in independent public health care institutions, using an entity located in the Silesian province as an example, it was observed that the patient’s right to information about his health is respected. The information provided is understandable and accurate. The part of the questionnaire concerning informing patients about planned medical services medical services and the consequences associated with them showed that 83.3% of respondents agreed that the information was provided in a clear and understandable manner. The reason for the few negative opinions may have been the fact that patients, although clearly informed, in some cases doctors use medical terms that are not understood by the parties involved.21 In today’s health systems based on patient-centrism, the recommendation rate is an important element in assessing the quality and safety of services.22,23 In one of the joint WHO and OECD reports in 2019, it was noted that the hospital recommendation rate is one of the basic indicators of “patient centeredness”.22 In addition to measuring the quality of medical care, the study also developed the so-called Patient Recommendation Index, which was built on the basis of the recommendation index. The most valuable data was provided by the answer to the open question, because it contained many issues raised by patients regarding safety and the level of services in the entity.23,24 The British National Health Service (NHS) has introduced mandatory patient opinion surveys based on a modified version of the NPS - Friends and Family Test (FFT). The question asked to respondents is: “How likely are you to recommend our ward to friends and family if they needed similar care or treatment?”.25,26 In the case of the recommendation rate, is aggravating to interpret only the numerical value of the indicator. The number itself, unfortunately, provides little information about what the actual rating is. Only an indicator combined with an open-ended question in which the patient answers why he or she gave a high or low rating is of added value. The benefits include the fact that it is understandable to patients, it can be the basis for analyzing specific patient behavior, eg in the case of outpatient specialty care it can indicate the reasons for not attending appointments, it identifies critical points, weaknesses, problems and inconveniences that affect patient dissatisfaction, it is used for benchmarking - the result can be compared with the results of other health care providers.27 In this study, the recommendation rate allowed several conclusions to be drawn; respondents who were categorized as detractors on the NPS scale indicated many important issues related to the quality and safety of medical services, including long waiting time for hospital admissions and poor quality of medical and nursing care and the care of medical staff, which was not at the highest level according to the respondents. The waiting time for hospital admission affects the entire subsequent diagnostic and therapeutic process. Patients also emphasized a highly important issue that may be related to the poor quality of care, which is the shortage of medical staff, and thus the excessive workload on medical staff. Patients categorized as promoting the hospital paid attention to the friendly and professional care of the representatives of the medical staff and the high standard of living conditions - cleanliness, intimacy. In study about assessment of the impact of the COVID-19 pandemic on stress for nursing staff showed a change in the perception of stress by nursing staff and an increase in stress symptoms compared to the time before the pandemic. Stress factors include the fear of transmitting the virus from the workplace to relatives, the threat to the life and health of one’s own and the loved ones, quickly introduced organizational changes and continuous work in an increased sanitary regime. All the factors contribute to a heavy workload, high stress levels and a high risk of burnout among nursing staff. Factors that caused stress were the fear of infecting oneself and loved ones, many quick, chaotic changes in the organization of work and work in a very strict sanitary regime, which was associated with many difficulties in performing daily duties. All these factors contribute to a high level of fatigue, organizational chaos and a high probability of professional burnout among nurses.28,29 Another study on the observance of the patients’ rights that focused on organizational factors and was conducted in nurses working in intensive care units showed several factors, such as bad attitude of nurses towards patients, socio-economic problems, working hours, heavy workload in a limited time. The study was conducted in 160 nurses who indicated the factors influencing the quality of nursing care based on the patient’s rights charter.30 A study in a group of Iranian nurses showed that the knowledge of the Patient Rights Act was acceptable; however, the rights of the patients were not respected. It seems that the notification of the Act on patients’ rights increased the nurses’ awareness of patients’ rights, although the improvement of nurses’ work requires broader actions.31
Observation of the patients’ rights guarantees the quality and safety of medical services, and it is a condition for the implementation of patient-centered medical care in which the patient participates in the diagnostic and therapeutic process. Awareness of patient rights among medical staff and patients themselves, along with their opinions on these rights, is a challenge for healthcare professionals. Patients’ rights are very specific legal regulations that have been developed in order to protect the dignity and autonomy of the patient. In the research conducted in 2021 in a group of over 600 patients and over 900 representatives of medical staff, conclusions were drawn about patients’ knowledge of their rights and the knowledge and awareness of medical staff. Education, work experience and profession affect the knowledge of and respect for the patient’s rights.32 The mode of hospital admission is a factor that affects the knowledge of the patients’ rights. The lack of knowledge of the medical staff about the patients’ rights has a significant impact on the compliance with these rights or their violation. Studies have shown that the doctors, nurses and midwives have a good knowledge of patients’ rights.32 Good knowledge of patients’ rights among healthcare professionals translates into a high level of information for patients about their rights, which correlates with a high level of patients’ awareness.32
Another important aspect is to promote patients’ rights through the accreditation of hospitals. Both legal regulations and accreditation standards involve patients’ rights. However, they differ in a significant way, as regulations define minimum standards, while accreditation standards describe optimal performance of a facility. Regulations focus on the provisions of law, while accreditation standards indicate what hospitals can do to implement these rights, which can help to standardize activities across hospitals. A recent study from Israel confirms this approach, and it also emphasizes that international accreditation standards and national laws may differ when it comes to the definition of real rights.33
The observance of patients’ rights is primarily associated with the knowledge of these rights, which largely depends on the level of education. High importance regarding respect for patients’ rights in daily practice has also been examined in the group of nursing students in several European countries: Poland, Slovakia and Spain. The degree of the observance of patients’ rights in health care facilities in Poland, Spain and Slovakia varies significantly in the opinion of the nursing students, which has negative consequences for the patient. In the study, differences were observed with regard to the level of knowledge of nursing students about selected patients’ rights in the personalized health care, which requires systemic educational activities at the university level in individual countries. The level of knowledge of patients’ rights among nursing students is not the same, and it includes the knowledge of the right to information about the patient’s health, confidentiality of information and patient’s medical records, the right to withdraw objections to organ and tissue donation, the right to pastoral care and to deposit valuable items.15 Analyzes of many other authors show an unfavorable situation of patients with regard to their rights in various medical entities. A survey of 500 Iranian patients using inpatient and specialist outpatient care showed that approximately 93% of patients had not received any information on their rights.34
Respondents were asked whether they had been given information on possible treatment methods and their consequences by the medical staff, and whether during the qualification for a procedure and/or hospitalization they were asked for their opinion on a specific method of diagnosis or therapy. This is an extremely important issue in the light of the patient’s participation in the diagnostic and therapeutic process. In a study conducted in a group of 514 patients hospitalized in Minia University Hospital in Egypt, it was found that approximately 76% of patients were not aware of the patient rights charter, and 98.1% of the respondents claimed that the medical staff had not informed them about available treatment options.35 This suggests that healthcare providers should put more stress on making patients aware of their rights and involve patients in the process of making decisions on the treatment. In a meta-analysis on the awareness of patient rights among Iranian patients, 20 articles assessing observance rates of patient rights were analyzed. The study reviewed the main issues related to the Patient Rights Act in different parts of the world. The observance rate of patient rights was considered to be sufficient to a certain extent. However, contradictory findings revealed in this study suggest certain shortcomings that need to be addressed. There seems to be a need for a better description and improvement of the indicators of health service awareness among patients with regard to their knowledge of patients’ rights.36 Another study on the awareness of patient rights among patients of the Tertiary University Hospital (cross-sectional study) showed that women were more aware of their rights than men, and young adults were more aware of their rights than the representatives of other age groups. The conclusions of the study are that effective measures have to be taken to improve the overall awareness not only among patients but also among various beneficiaries of the health care services. Educational materials for patients and their families should be prepared in an understandable language and distributed to patients during hospital admission or hospitalization. In addition, education of medical professionals should focus on patients’ rights, and both students and hospital staff should be taught about the importance of these rights, the need to make patients aware of their rights and the consequences of the observance of patients’ rights.37 A study conducted in Pakistan on a group of 220 patients shows that the majority of patients (64%) are not aware of their rights. The level of awareness was higher in patients of private hospitals as opposed to the public ones. Most patients were dissatisfied with the way in which their rights were observed, especially in public hospitals.36 A study on 200 patients in Tehran shows that it is necessary to organize trainings about patient confidentiality and privacy, and to promote the observance of patients’ rights. In addition, both healthcare providers and patients have to be informed about patients’ rights. Patients can be educated about their rights at admission or at any other appropriate time through conversation and educational materials.38,39
Given the above, repeated assessment of the quality of healthcare and adherence to patient rights can be of great importance. Regular monitoring of these applications can be of great importance in improving the internal processes and quality of service of the facilities. Importantly, further research should focus not only on hospital care, but also on primary care and specialist care. It is important to examine whether there are inequalities in the quality of services depending on specialization.
Limitations of the Study
As with any study, this one also has some limitations. The main limitation is the unrepresentative sample with regard to age, which does not allow to draw conclusions on the entire population. Half of the respondents were persons aged 25–44, and only 10% were persons over 65 years of age who are the patients that use a significant percentage of hospital services. Another limitation of the study is its one-time nature. In order to constantly monitor the quality of health care and observance of patient rights, have consideration for patient experience, improve internal processes and the quality of services, constant and regular research in this area should be performed. Another limitation is lack of comprehensive examination of the quality of medical care in the hospital ward and the observance of all patient rights. Another limitation is the focus on hospital care, omitting the type of hospital ward where the patient was staying, which would certainly affect the interpretation of the study results. It would also be important to examine not only inpatient care, but also outpatient specialist care and primary care, where the patient’s experience may be significantly different.
Conclusions
Most statistically significant differences in the assessment of medical care in the hospital ward were associated with such sociodemographic variables as age and income. People aged 55–64 and 65+ rated most of the analyzed aspects better, including active listening by the medical staff, informing the patient about their health condition, diagnostic and therapeutic procedures and care activities in a clear and understandable way, asking the patient for their opinion when choosing treatment methods. Younger persons, who had probably more knowledge about the patient’s rights, assessed the observance of the patient’s rights more critically. The key issue is the knowledge of the patient’s rights by medical staff and by the patients themselves. Therefore, systemic activities should be taken in order to educate future medical personnel in this area and to put emphasis on the development of the ability of medical personnel to communicate with the patient. This is a key ability that affects the entire therapeutic process. Therefore, medical schools and universities should include the patients’ rights and communication with patients in their curricula. Patients who highly assessed the medical staff with regard to their communication skills, also highly assessed the treatment results.
There were no statistically significant differences in the perception of having their rights to information respected in the groups of patients of different professions. Both medical and nursing staff were assessed at a similar level. This is why, the patients’ rights and communication with patients should be included in the teaching programs for both doctors and nurses.
The percentage of promoters and detractors was similar (36% vs 38%). Dissatisfied patients waited a long time to be admitted to the hospital. They were also not satisfied with the care and meals. Promoters paid attention to the kind and professional care of the representatives of the medical staff and the high standard of living conditions - cleanliness, intimacy.
Regular patient satisfaction surveys allow for the monitoring of the observance of patients’ rights and the quality of services, and for the identification of areas that require changes to adapt to accreditation standards and guarantee safety in a medical entity.
Ethic and Consent Statements
We confirm that the work and conducted research are in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study.
Acknowledgments
Among other things, the Bioethics Committee operates in accordance with the Law on the Medical Profession - The Law of December 5, 1996 on the Profession of Physician and Dentist. Article 29 Opinion of the Bioethics Commission on a medical experiment project. In this article there is information about the necessity of obtaining the opinion of the Bioethics Commission for medical experiments. This study does not meet the definition of a medical experiment and therefore the authors do not have the opportunity to obtain the commission’s approval, because there is no legal basis for this.
Funding
01/Z/MBM/N/21.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lilleheie I, Debesay J, Bye A, et al. A qualitative study of old patients’ experiences of the quality of the health services in hospital and 30 days after hospitalization. BMC Health Serv Res. 2020;20(1):446. doi:10.1186/s12913-020-05303-5
2. Kingston A, Robinson L, Booth H, et al. Projections of multi-morbidity in the older population in England to 2035: estimates from the population ageing and care simulation (PACSim) model. Age Ageing. 2018;47(3):374–380. doi:10.1093/ageing/afx201
3. Batalden P. Getting more health from healthcare: quality improvement must acknowledge patient coproduction—an essay by Paul Batalden. BMJ. 2018:k3617. doi:10.1136/bmj.k3617
4. World Health Organization Working Group. Quality ace in heath care; 1989.
5. Donabedian A. The Definition of Quality. Health Administration PRESS; 1980.
6. Manelin EB. Health care quality improvement and the ambiguous commodity of care. Med Anthropol Q. 2020;34(3):361–377. doi:10.1111/maq.12608
7. Butkus R, Rapp K, Cooney TG, et al. Envisioning a better U.S. health care system for all: reducing barriers to care and addressing social determinants of health. Ann Intern Med. 2020;21:172. doi:10.7326/M19-2410
8. Yang BK, Johantgen ME, Trinkoff AM, et al. State nurse practitioner practice regulations and U.S. health care delivery outcomes: a systematic review. Med Care Res Rev. 2021;78(3):183–196. doi:10.1177/1077558719901216
9. Geyman J. COVID-19 has revealed America’s broken health care system: what can we learn? Int J Health Serv. 2021;51(2):188–194. doi:10.1177/0020731420985640
10. Barć K, Weber C, Maksymowicz-śliwińska A, et al. Healthcare provision in amyotrophic lateral sclerosis: procedures, queries and pitfalls in Germany and Poland. Amyotroph Lateral Scler Frontotemporal Degener. 2020;21(3–4):193–202. doi:10.1080/21678421.2020.1746345
11. Standardy Akredytacyjne; 2022. Available from: https://www.cmj.org.pl/akredytacja/standardy.php.
12. Sigman M. Introduction: personalized medicine: what is it and what are the challenges? Fertil Steril. 2018;109::944–945. doi:10.1016/j.fertnstert.2018.04.027
13. Powszechna Deklaracja Praw Człowieka [UNIVERSAL DECLARATION OF HUMAN RIGHTS] Polish; 2022. Available from: http://libr.sejm.gov.pl/tek01/txt/onz/1948.
14. Dz.U. Ustawa z dnia 6 listopada 2008 r. o prawach pacjenta i Rzeczniku Praw Pacjenta. Polish; 2009.
15. Kupcewicz E, Grochans E, Kadučáková H, et al. Personalized healthcare: the importance of patients’ rights in clinical practice from the perspective of nursing students in Poland, Spain and Slovakia-A cross-sectional study. J Pers Med. 2021;11(3):191. doi:10.3390/jpm11030191
16. WHO patients’ rights; 2022. Available from: https://www.who.int/genomics/public/patientrights/en/.
17. Busby M, Matthews R, Burke FJT, Mullins A, Shumacher K. Is any particular aspect of perceived quality associated with patients tending to promote a dental practice to their friends and colleagues? Br Dent J. 2015;218:E12. doi:10.1038/sj.bdj.2015.229
18. Kroll Maarten W. The net promoter score an asset to patient experience surveys? Health Expect. 2014. doi:10.1111/hex
19. American Association for Public Opinion Research (AAPOR), Standard Definitions. Final dispositions of case codes and outcome rates for surveys. IX revision; 2016.
20. Defining patient and human experience; 2023. Available from: https://theberylinstitute.org/defining-patient-experience/.
21. Owoc A, Bojar I, Owoc J, et al. Functioning of the healthcare system in Poland – interest and self-assessed level of knowledge of the surveyed. Zdr Publ. 2009;119(3): 239–242.
22. Quentin W. Measuring healthcare quality: improving healthcare quality in Europe. Characteristics, effectiveness, and implementation of different strategies; 2019.
23. Reichheld F. The Ultimate Question 2.0. How Net Promoter Companies Thrive in a Customer Driven World, Boston; 2011.
24. Colvin G The simple metric that’s taking over big business. 2022. Available from: https://fortune.com/longform/net-promoter-score-fortune-500-customer-satisfaction-metric/.
25. Department of Health. The NHS friends and family test implementation guidance; 2012. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213047.
26. Wilberforce M, Poll S, Langham H, et al. Measuring the patient experience in community mental health services for older people: a study of the Net Promoter Score using the Friends and Family Test in England. Int J Geriatr Psychiatry. 2019;34(1):31–37. doi:10.1002/gps.4978
27. Denkiewicz L. Metodologia Patient Experience Design jako narzędzie badania opinii pacjentów. Copyright by Next Medica Sp. z o.o. Warszawa. Polish; 2020.
28. Grzelak L, Szwarc P. Wpływ pracy w czasie pandemii COVID-19 na stres personelu pielęgniarskiego. Polish. Innowacje w pielegniarstwie i naukach o zdrowiu. 2021;1(6). doi:10.21784/IwP.2021.001
29. Wasilewski TP. Subiektywna ocena wybranych aspektów satysfakcji z pobytu w szpitalu pacjentów oddziałów zabiegowych. Polish. Pieleg Chir Angiol. 2021;3:81–86.
30. Mousavi S, Mohammadi N, Ashghali Farahani M, Hosseini AF. Observing patients’ rights and the facilitating and deterrent organizational factors from the viewpoint of nurses working in intensive care units. J Client Cent Nurs Care. 2017;3:27–36. doi:10.32598/jccnc.3.1.27
31. Sheikhtaheri A, Jabali M, Dehaghi ZH. Nurses’ knowledge and performance of the patients’ bill of rights. Nurs Ethics. 2016;23:866–876. doi:10.1177/0969733015584967
32. Czajkowska M, Janik A, Zborowska K, et al. Knowledge and opinions of patients and medical staff about patients’ rights. Ginekol Pol. 2021;92(7):491–497. doi:10.5603/GP.a2021.0014
33. Engel C. Promoting patients’ rights through hospital accreditation. ISR J Health Policy Res. 2020;9(1):70. doi:10.1186/s13584-020-00421-1
34. Ansari S, Abeid P, Namvar F, et al. Respect to the bill of patients’ rights in the educational hospitals in Ahvaz, Iran Middle East. J Sci Res. 2013;4::440–444. doi:10.5829/idosi.mejsr.2013.13.4.71229
35. Mohammed E, Seedhom A, Ghazawy E. Awareness and practice of patient rights from a patient perspective: an insight from Upper Egypt. Int J Qual Health Care. 2018;1:145–151. doi:10.1093/intqhc/mzx182
36. Abedi G, Shojaee J, Moosazadeh M. Awareness and observance of patient rights from the perspective of Iranian patients: a systematic review and meta-analysis. Iran J Med Sci. 2017;42:227–234. doi:10.1016/j.puhe.2005.10.014
37. Agrawal U, D’Souza B, Seetharam A. Awareness of patients’ rights among inpatients of a tertiary care teaching hospital- a cross-sectional study. J Clin Diagn Res. 2017;11:IC01–IC06. doi:10.7860/JCDR
38. Tabassum T, Ashraf M, Thaver I. Hospitalized patients’ awareness of their rights-a cross sectional survey in a public and private tertiary care hospitals of Punjab, Pakistan. J Ayub Med Coll Abbottabad. 2016;28:582–586.
39. Borowska M, Religioni U, Augustynowicz A. Patients’ opinions on the quality of services in hospital wards in Poland. Int J Environ Res Public Health. 2023;20(1):412. doi:10.3390/ijerph20010412
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.