Back to Journals » Infection and Drug Resistance » Volume 15
Resistance Phenotype and Molecular Epidemiology of Carbapenem-Resistant Klebsiella pneumoniae Isolated from Nanjing Children’s Hospital in Jiangsu Province, China
Authors Tao G , Tan H, Ma J, Chen Q
Received 2 June 2022
Accepted for publication 29 August 2022
Published 14 September 2022 Volume 2022:15 Pages 5435—5447
DOI https://doi.org/10.2147/IDR.S377068
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Guixiang Tao,1 Hua Tan,2 Jingjing Ma,1 Qian Chen1
1Institute of Pediatrics, Children’s Hospital of Nanjing Medical University, Nanjing, People’s Republic of China; 2Department of Laboratory Medicine, Children’s Hospital of Nanjing Medical University, Nanjing, People’s Republic of China
Correspondence: Qian Chen, Institute of Pediatrics, Children’s Hospital of Nanjing Medical University, Nanjing, People’s Republic of China, Tel +8618951768213, Email [email protected]
Objective: The drug resistance phenotype and molecular epidemiological characteristics of carbapenem-resistant Klebsiella pneumoniae (CRKP) were identified among children in Jiangsu Province, China.
Methods: CRKP strains were collected from the Children’s Hospital of Nanjing Medical University from December 2020 to March 2022. CRKP strains were characterized for further study: antimicrobial susceptibility testing, carbapenem resistance genes and homology analysis.
Results: Among 86 strains of CRKP, 85 carried carbapenemase genes; the dominant gene was blaKPC-2 (88.2%, 75/85), followed by blaNDM-1 (4.7%, 4/85), blaNDM-5 (4.7%, 4/85), blaIMP-8 (2.3%, 2/85), and blaOXA-181 (1.2%, 1/85). Among the 86 strains of CRKP, one isolate contained both the blaNDM-5 and blaOXA-181 genes, which is the first time that Klebsiella pneumoniae has been shown to jointly carry these genes in China. Another CRKP strain did not carry any carbapenemase gene. MLST analysis identified a total of 10 different sequence types, among which sequence type (ST) 11 was the most common. PFGE analysis identified 75 blaKPC-2-producing CRKP ST11 strains, of which 68 were dominant clusters distributed among 11 different wards, mainly the neonatal medical centre (18 strains), neonatal surgery (17 strains) and cardiac care unit (CCU) (8 strains) wards.
Conclusion: Clonal dissemination of KPC-2-producing CRKP ST11 was observed in multiple departments. Additionally, non-ST11 strains showed high polymorphism based on molecular typing, indicating increasing diversity in CRKP strains. To our knowledge, this is the first report of NDM-5 and OXA-181-coproducing Klebsiella pneumoniae causing infection in children in China, which poses a significant health risk for paediatric patients. Active surveillance and effective control measures are urgently needed to prevent further transmission of these strains among children.
Keywords: Klebsiella pneumoniae, carbapenemase, KPC-2, ST11, clonal, dissemination, children
Introduction
Klebsiella pneumoniae is an important pathogen causing nosocomial infection, pneumonia, urinary tract infection, bloodstream infection and a series of additional infectious diseases.1,2 Carbapenems (imipenem, meropenem, ertapenem, etc.) are the most effective drugs for the treatment of Klebsiella pneumoniae, but in recent years, the frequent use of carbapenem antibiotics has led to a continuous increase in bacterial resistance. The detection rate of carbapenemase-resistant Klebsiella pneumoniae (CRKP) strains is increasing yearly, and the isolation rate of CRKP in China is also increasing yearly, with CRKP becoming one of the most threatening nosocomial infectious pathogens. According to the latest data from CHINET in 2021, the rate of Klebsiella pneumoniae antimicrobial resistance against imipenem increased from 3.0% to 25.5%, and the rate of antimicrobial resistance against meropenem increased from 2.9% to 27.1%, showing a continuous upwards trend. At present, the drug resistance of Klebsiella pneumoniae is becoming increasingly serious, and the epidemiological study of Klebsiella pneumoniae has become a global hot issue. Understanding the drug resistance of Klebsiella pneumoniae in clinical transmission can provide effective guidance for clinical prevention and treatment.
A large number of studies have shown that CRKP inactivates carbapenems mainly through the following three mechanisms: the production of various carbapenemases, loss of outer membrane proteins and overexpression of efflux pumps. Carbapenemase production is the most common mechanism of drug resistance in Enterobacteriaceae. Isolates from adults mainly produce KPC enzymes,3 while isolates from children produce KPC, NDM and OXA-48-like enzymes.4,5 According to Ambler classification, carbapenemases are mainly distributed in β-lactamase classes A, B and D. Class A KPC enzymes are the most common carbapenemases. Since the first strain of KPC-2-producing CRKP was detected in Zhejiang Province in 2007,6 this type of strain has been reported in various regions of China. In recent years, outbreaks of infection caused by KPC-2-producing CRKP in neonatal wards have been reported in China,7 which is consistent with the prevalence of adult carbapenemase in China. Class B is also known as the metal β-lactamases and includes NDM, IMP, VIM and other types. NDM is the most important subtype of metalloenzymes. In 2014, Acinetobacter baumannii carrying the blaNDM gene was first identified in China.8 Then, an outbreak of Klebsiella pneumoniae carrying the blaNDM gene was reported in adults and children from all over the country. In recent years, outbreaks of NDM-1-producing CRKP in neonatal wards have occurred in Yunnan,9 Beijing,10 Chongqing,11 eastern China12 and other regions. It is worth noting that outbreaks of NDM-5-producing CRKP in children have also occurred in China.13,14 In addition to blaNDM-1 and blaNDM-5, which have been widely reported, sporadic cases of NDM-4-,14 NDM-6-,15 NDM-9-16 and NDM-16-producing17 Klebsiella pneumoniae have also been reported in China. The production of IMP and VIM enzymes by Klebsiella pneumoniae isolates is rare in China. At present, IMP-4-producing Klebsiella pneumoniae has caused outbreaks in a few hospitals in China in recent years,18 while IMP-8-producing Klebsiella pneumoniae has only been reported in Taiwan,19 which has not been reported in pediatric patients. Only one case of IMP-26-20 and IMP-38-21 producing Klebsiella pneumoniae has been reported in China. Vim-producing Klebsiella pneumoniae has been reported in Shenzhen,22 Beijing23 and other regions. OXA-48-like enzyme is a class D β-lactamase that is widely prevalent in European countries and occurs as an epidemic in China. The OXA-48 enzyme has been reported in Beijing,24 Shanghai25 and Taiwan.26 In recent years, OXA-232-producing (a variant of OXA-48 family, and the third most common OXA-48-like carbapenemase worldwide) Enterobacteriaceae began to appear in China, while OXA-232-producing Klebsiella pneumoniae is the most common in Shanghai,27 Zhejiang28 and other regions. According to the above reports, the OXA-48-like enzyme has begun to spread in China. To date, limited studies have isolated CRKP from paediatric patients. On this basis, our study aimed to perform preliminary research on the recent drug resistance characteristics and molecular epidemiology of CRKP isolated from the Children’s Hospital affiliated with Nanjing Medical University.
Methods
Bacterial Strains
This study was conducted in the Children’s Hospital affiliated with Nanjing Medical University, one of the largest tier-one comprehensive children’s hospitals in Jiangsu Province, with 1742 beds, 255.11 million outpatient and emergency visits, 73,600 discharges, 33,600 operations, and an average length of stay of 7.0 days. In this study, nonduplicate CRKP strains were collected from inpatients of the Children’s Hospital affiliated with Nanjing Medical University from December 2020 to March 2022, and electronic medical records of the children were retrospectively collected, including information such as sex, age, ward, main diagnosis and specimen source. This study was approved by the ethics committee of the Children’s Hospital affiliated with Nanjing Medical University.
Strain Identification and Antimicrobial Susceptibility Testing
Klebsiella pneumoniae was identified by a VITEK-2 Compact system (bioMerieux, Marcy-L ‘Etoile, France) and a supporting Vitek 2 identification card. The drug sensitivity test of isolated Klebsiella pneumoniae was carried out by a Vitek 2 Compact system and accompanying GN09 drug sensitivity card according to the manufacturer’s instructions, with the Kirby–Bauer method serving as a supplement. MICs to polymyxin E were tested by broth microdilution. Quality control (QC) strain Escherichia coli ATCC 25922 was used in all testing. Susceptibility breakpoints were interpreted according to the Institute of Clinical and Laboratory Standards (CLSI), except for polymyxin E, which was interpreted based on the European Committee for Antimicrobial Susceptibility Testing (EUCAST) criteria 10.0.29,30
Detection of Resistance Genes
Bacterial genomic DNA was extracted using a DNA extraction kit according to the manufacturer’s instructions, and as previously reported,31–34 the common carbapenemase genes (blaKPC, blaNDM, blaIMP, blaVIM, blaOXA-48) of CRKP isolates were studied by PCR. The PCR products were subjected to 1.0% agarose electrophoresis, and the positive products were sequenced by Sanger sequencing. The complete sequences were compared with those reported in GenBank using the BLAST algorithm (http://www.ncbi.nlm.nih.gov/blast/).
The primer sequences are shown in Table 1. The amplification system consisted of 50 μL: ddH2O (20 μL), Multiplex Buffer (25 μL), Primer1 (10 μM) (2μL), Primer2 (10 μM) (2 μL), and template (1 μL). The PCR amplification conditions were 95 ℃ for 3 min; 95 ℃ for 15s, 55–62 ℃ for 15s, and 72℃ for 15s (35 cycles); and 72 ℃ for 5 min.
 |
Table 1 Primer Sequences for Common Carbapenemase Genes of CRKP |
Molecular Typing
Multilocus Sequence Typing (MLST)
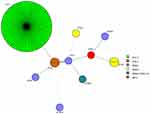
Multilocus sequence typing (MLST) was performed according to the scheme previously described on the Pasteur Institute MLST website (http://bigsdb.pasteur.fr/klebsiella/). The sequence results of 7 housekeeping genes (infB, pgi, mdh, phoE, gapA, tonB and rpoB) were uploaded to the MLST database of Klebsiella pneumoniae to obtain the serial numbers and sequence types of housekeeping genes. The minimum spanning tree of 86 strains of Klebsiella pneumoniae was constructed with BioNumerics 7.6. Each node represents a ST. The node size is proportional to the number of strains in the representative ST. The colour distribution represents the distribution of carbapenemase genes between different STs.
Pulsed-Field Gel Electrophoresis (PFGE)
The genetic relationship of CRKP isolates was determined by pulsed-field gel electrophoresis (PFGE). PFGE was performed according to the protocol established by the Centers for Disease Control and Prevention (Atlanta, GA). Cluster analysis was conducted by BioNumerics software version 7.6 to draw a tree diagram, with more than 80% similarity used to define a group, to compare the genetic relationship between different strains. The UPGMA (Unweighted Pair-Group Method with Arithmetic means) algorithm was used to construct the tree graph. When the similarity index of strains was ≥80%,35 they were classified into the same clone group.
Next-Generation Sequencing
To further study the CRKP strains, KP26 and KP55 in this study were selected for next-generation sequencing. Next-generation sequencing was completed by Guangzhou Weiyuan Gene Technology Co., Ltd., and the sequencing platform was a NovaSeq PE150 system from Illumina. FastQC was used for quality control of the original data, MEGAHIT software was used for genome assembly, and QUAST software was used to evaluate the quality of the genome assembly. Resistance Gene Identifier (RGI) software provided by the Comprehensive Antibiotic Research Database (CARD) was used for comparison with the CARD Database. According to the comparison results of RGI, the resistance gene information was annotated to the database. KP26 and KP55 genome circle maps were drawn by GCview software.
Results
Clinical Characteristics of CRKP Isolates
Among the 86 CRKP strains isolated from December 2020 to March 2022, the median age of children was 1.5 months, and the male-to-female ratio was 1.6.
Among the 86 CRKP isolates, the sources of clinical specimens were sputum (69.8%, 60/86); blood (11.6%, 10/86); urine (8.1%, 7/86); secretions, ascites and pus (2.3%, 2/86); and venous catheters, alveolar lavage fluid and tissue (1.2%, 1/86).
CRKP strains were collected from 12 different wards, mainly distributed in neonatal medicine (24.4%, 21/86) and neonatal surgery (22.1%, 19/86), followed by the surgery intensive care unit (SICU) (15.1%, 13/86), the cardiac care unit (CCU) (9.3%, 8/86), the paediatric intensive care unit (PICU) (8.1%, 7/86), cardiovascular medicine (5.8%, 5/86), the respiratory department (4.7%, 4/86), urinary surgery (3.5%, 3/86), and cardiothoracic surgery (3.5%, 3/86). The emergency ward (n=1), nephrology department (n=1), and neonatal surgery (n=1) accounted for 1.2% (1/86), respectively.
Antimicrobial Susceptibility Testing
CRKP strains from paediatric patients are highly resistant to the most commonly used antibiotics. The antibacterial susceptibility of 86 CRKP strains is shown in Table 2. The 86 clinical isolates in this study were resistant to ampicillin, ampicillin sulbactam, piperacillin, piperacillin tazobactam, cefuroxime, cefuroxime, cefotetan, ceftazidime, ceftriaxone, cefepime, imipenem and cefazolin (100%). The rates of antibacterial resistance to aztreonam and meropenem were 96.5% and 98.8%, respectively. The rates of antibacterial resistance to ciprofloxacin, levofloxacin and sulfamethoxazole were 88.4%, 89.5% and 88.4%, respectively. The rates of antibacterial resistance to amikacin, gentamicin and tobramycin were 3.5%, 4.7% and 3.5%, respectively. Additionally, CRKP strain showed 100.0% sensitivity to polymyxin E.
 |
Table 2 Antimicrobial Susceptibility Patterns of CRKP Strains, % (n) |
Detection of Resistance Genes
Through PCR and sequence comparison with GenBank, 85 strains of 86 CRKP strains were found to carry carbapenemase genes, among which blaKPC-2 was the dominant gene (87.2%, 75/86), followed by blaNDM-1 (4.7%, 4/86), blaNDM-5 (4.7%, 4/86), blaIMP-8 (2.3%, 2/86), and blaOXA-181 (1.2%, 1/86). Notably, 1 strain cocarried blaNDM-5 and blaOXA-181, which was isolated from a child undergoing surgery and on mechanical ventilation, and clinical assessment led to the assumption that this isolate was one of the pathogens causing sepsis.
Among the 86 strains of CRKP, 1 strain was found to not carry any carbapenemase gene. See Section 2.5 for specific gene analysis.
Molecular Typing
MLST results showed that a total of 10 different sequence types (STs) were identified for the 86 strains of CRKP. ST11 (75/86) was the most common. The distribution of carbapenemase in the different STs is shown in (Figure 1). All strains carrying blaKPC-2 (87.2%, 75/86) belonged to ST11, while the strains carrying blaNDM-1 belonged to different STs, including ST17 (n=1), ST29 (n=1), ST252 (n=1) and ST3915 (n=1). The strains carrying the blaNDM-5 gene were ST76 (n=2), ST2601 (n=1) and ST2217 (n=1). The strain carrying blaIMP-8 belonged to ST20, and the strain carrying blaOXA-1 belonged to ST831. The strain carrying the blaNDM-5 and blaOXA-181 genes was classified as ST2601.
The genomic DNA of 86 strains of CRKP was digested by the XbaI enzyme, and a PFGE map of the 86 strains of CRKP could be divided into 15 different clusters. Seventy-five strains of ST11 CRKP producing the KPC-2 enzyme were divided into four clusters, of which 68 strains were in the same cluster. These strains were isolated in multiple departments and were mainly spread in neonatal medicine (n=18), neonatal surgery (n=17) and the CCU (n=8), accounting for 29.0%, 27.4% and 12.9%, respectively. Among them, 85.7% (18/21), 89.5% (17/19) and 100% (8/8) of ST11 clusters producing the KPC-2 enzyme were found in the neonatal medical centre, neonatal surgery, and the CCU, respectively (Figure 2). In addition, the PFGE profiles of 11 other non-ST11 CRKP isolates were divided into 11 different PFGE clusters (Figure 3).
Analysis of Drug Resistance Genes Based on Next-Generation Sequencing
In this study, two strains were found to carry the IMP-8 gene, and one strain was selected for further drug resistance gene analysis (KP26), while the other strain did not carry any carbapenemase gene (KP55), so these two strains were selected for next-generation sequencing.
Ardb Anno1.0 software was used for comparison with the Antibiotic Resistance Genes Database (ARDB) database, and the Klebsiella pneumoniae gene and its corresponding drug resistance function annotation information were combined for analysis.
The acquired resistance genes predicted in the KP26 genome were the β-lactam resistance genes blaCTX-M, blaSHV-2, and blaIMP-8; 2) aminoglycoside resistance genes: APH(3)-IB, APH(6)-ID; 3) fosfomycin resistance gene: FosA5; 4) tetracycline efflux pump: tetC; 5) drug resistance gene efflux pumps: acra, acrb, macb, mdtg, mdth, mdtk, and tolc; and 6) pore protein: OmpA (Figure 4).
 |
Figure 4 Genome circle diagram of the KP26 strain (marked genes are annotated drug resistance genes). |
The acquired resistance genes of KP55 were 1) β-lactam resistance genes: blaCTX-M, blaSHV-2, and blaOXA-1; 2) quinolone resistance gene: qnrB1; 3) tetracycline resistance genes: tetA and tetC. 4) tetracycline efflux pump: tetC; 5) drug resistance gene efflux pumps: acra, acrb, macb, mdtg, mdth, mdtk, and tolc; and 6) pore protein: OmpA (Figure 5)
 |
Figure 5 Genome circle diagram of the KP55 strain (marked genes are annotated drug resistance genes). |
Figures 4 and 5 Genome circle diagram of the KP55 strain (marked genes are annotated drug resistance genes)
Discussion
Carbapenems have long been considered the last line of defence against multidrug-resistant gram-negative bacterial infections. The emergence of CRKP poses a tremendous threat to global public health and a severe challenge to clinical anti-infection treatment, especially for children. The purpose of this study was to research the drug resistance phenotype and epidemiological characteristics of CRKP in the Children’s Hospital affiliated with Nanjing Medical University to help prevent the epidemic of CRKP infection in children. To our knowledge, this is the first time that Klebsiella pneumoniae ST2601, which produces both NDM-5 and OXA-181, has been identified in paediatric patients.
The drug sensitivity results of this study showed that the 86 CRKP strains were all multidrug-resistant bacteria and that their rates of drug resistance to imipenem and meropenem were 100% and 98.8%, respectively. The rate of resistance to cephalosporin and an enzyme inhibitor compound was 100%. The rates of drug resistance to aztreonam, ciprofloxacin, levofloxacin and sulfamethoxazole ranged from 88.4% to 96.5%. The rates of drug resistance to amikacin, gentamicin and tobramycin were 3.5%, 4.7% and 3.5%, respectively. All 86 CRKPs were sensitive to colistin, which may be due to their less use in children.This study showed that infections in children are generally resistant to commonly used antibiotics under the limited selection of antibiotics, and anti-infection treatment is more difficult than in adults. Therefore, hospitals need to strengthen the prevention and control of CRKP strains and strengthen the monitoring of bacterial resistance.
Currently, NDM-1 is the most common carbapenemase in India, Pakistan, and Sri Lanka,36 while ST11 is mostly associated with KPC-2 enzyme in China.3 Among 86 strains of CRKP detected in this study, 75 produced the KPC-2 enzyme among 85 producing carbapenemase, accounting for 88.2% of the isolates, which is consistent with the results of most studies of CRKP in adults in China.37 PFGE showed the cloning and transmission of KPC-2-producing Klebsiella pneumoniae ST11 in many departments in the hospital, mainly in the neonatal medical centre and neonatal surgery department, suggesting that the hospital should take targeted measures, especially to control the outbreak of CRKP clusters in neonatal-related wards.
In this study, 8 strains of Klebsiella pneumoniae carrying the blaNDM gene were identified, among which 4 strains carried blaNDM-1 and 4 strains carried blaNDM-5. The strains carrying the blaNDM-1 gene belonged to different STs, ST17 (1.2%, 1/86), ST29 (1.2%, 1/86), ST252 (1.2%, 1/86) and ST3915 (1.2%, 1/86). Among them, NDM-1-producing Klebsiella pneumoniae ST29 was transmitted in a neonatal ward in India,38 which is alarming. NDM-1-producing Klebsiella pneumoniae ST3925 has never been reported worldwide. Although the two strains carrying the blaNDM-5 gene were all of the same ST (ST76), the PFGE map showed different clusters, reflecting the diversity of the ST76-type pedigree. It was reported that Klebsiella pneumoniae ST76 caused an infection outbreak in neonatal wards in Mexico,39 suggesting that ST76 is a potential high-risk clone that needs more attention. NDM-5-producing Klebsiella pneumoniae has been reported in some countries, such as China: ST4,40 ST65,41 ST290,42 ST337,13 and ST485;43 Italy: ST383;44 Nigeria: ST476;45 Singapore: ST231;46 and USA: ST147.47 However, NDM-5-producing Klebsiella pneumoniae ST2217 and ST2601 found in this study have never been reported globally, indicating that NDM genes have complex diversity and need continuous monitoring.
Two strains carrying blaIMP-8 were also detected in this study. Yan et al reported that IMP-8 was first discovered in an adult Klebsiella pneumoniae infection patient in Taiwan in 2001, and almost all IMP-8-producing strains of Klebsiella pneumoniae were isolated from hospitalized patients in ICUs.48 In addition, blaIMP-8 was found in Klebsiella michiganensis, Enterobacter cloacae and Streptomyces thiobacillus.33 Since then, blaIMP-8 has not been reported in Klebsiella pneumoniae among Chidren. In this study, for the first time, Klebsiella pneumoniae carrying the blaIMP-8 gene was isolated from children in the respiratory ward of our hospital after a gap of more than 20 years. Kong et al reported that 4 strains carrying the blaIMP-4 gene were isolated from Nanjing Children’s Hospital in 2018–2019.49 In this study, 2 strains carrying the blaIMP-8 gene were isolated in 2021, but no strains carrying the blaIMP-4 gene were isolated. This finding indicates that the blaIMP-4 gene is constantly mutating.
This study also revealed that one strain did not carry any carbapenemase genes, instead carrying the β-lactam resistance genes blaCTX-M-15, blaSHV-11, and blaOXA-1, quinolone resistance gene qnrB1, fosfomycin resistance gene FosA6, tetracycline efflux pumps tetA and tetC, drug resistance gene efflux pumps acra, acrb, macb, mdtg, mdth, mdtk, and tolc, and porin OmpA, indicating that the bacterium acquired exogenous drug resistance genes and produced efflux pumps, resulting in multidrug resistance. In 2021, Wajima et al reported a CRKP strain without any carbapenemase gene that carried blaCTX-M-14, tet(A), tet(D), opxAB and qnrS1. In addition, a missense mutation of porin OmpK36 was found.50 The drug resistance genes were different from those in this study. This may be related to regional differences. At the same time, the AcrAB-TolC efflux pump was also found in the strain in this study, which is consistent with the results of most studies, and it is the internal mechanism of multidrug resistance in gram-negative bacteria.
Notably, one strain of CRKP was found to carry both the blaNDM-5 and blaOXA-181 genes in this study. In recent years, OXA-48-like Enterobacteriaceae have begun to appear in China, with Klebsiella pneumoniae being the most common. OXA-48-like carbapenemase has been reported to include OXA-48, OXA-162, OXA-181, OXA-204, OXA-232, OXA-244, and OXA-245.4 Among them, OXA-2325 is the most common in China, whereas the strain carrying the blaOXA-181 gene was isolated in this study, which has not been reported in children. Currently, there are few epidemiological and genomic studies on the cocarriers of OXA-48-like and other carbapenem resistance gene in paediatric patients. In 2021, Klebsiella pneumoniae from a neonatology ward in India were first reported to coproduce OXA-181/OXA-232 and NDM-5 enzymes. The isolates belong to different sequence types (ST14, ST15, ST23, ST48 and ST231),51 while the strain in this study that coproduced NDM-5 and OXA-181 belongs to ST2601, which has not been previously reported anywhere in the world. This strain was isolated from a child hospitalized in the neonatal surgery department for a long time. In future studies, we will focus on the drug-resistant phenotype of the CRKP strain in children in the neonatal surgery ward for continuous vigilant monitoring. The genetic relationship and genetic environment of Klebsiella pneumoniae coproducing MBL and OXA-48-like carbapenemase isolated from the ward were further studied.
In 2022, Zhang et al reported for the first time that a patient returning from Vietnam was infected with a strain that carried both carbapenemases, which was the first report in China on the coexistence of blaNDM-4 and blaOXA-181 genes in Klebsiella pneumoniae ST16.52 What was different from this study was the difference in NDM enzymes. This distinction may be related to the geographical environment where the patient lived at that time. Most previous studies have shown that OXA-48-like transmission occurred by cloning, but a few reports confirmed that the helper plasmid NDM could promote OXA-48-like transmission,4 which highlighted the threat posed by the presence of these carbapenemases together with NDM. Infection with different strains of carbapenemase usually corresponds to different antibiotic treatment schemes. For example, ceftazidime-avibactam, a novel enzyme inhibitor compound approved by the US FDA in February 2015, can effectively inhibit class A (such as KPC and ESBL) and class C (such as AmpC) β-lactamases. It also inhibits type D β-lactamases (such as OXA-48-like) but has no effect on type B metalloenzymes (such as NDM and IMP).53 Studies have shown that the combination of ceftazidime-avibactam and aztreonam, a novel enzyme inhibitor compound, can be used as a treatment plan for metalloenzyme-producing CRKP, but there are still uncertainties in the optimal administration strategy and pharmacokinetics-pharmacodynamics (PK-PD) target of combination therapy.53 Therefore, the emergence of cogenerating bacteria not only increases the difficulty of treatment but also promotes the transmission of drug resistance, which should be given further attention.
Conclusion
In conclusion, the generation of KPC-2 is the main mechanism of carbapenem resistance in children in Nanjing, Jiangsu Province. The KPC-2-producing Klebsiella pneumoniae ST11 strain was clinically transmitted in many departments, most commonly in neonatal medical centres and neonatal surgery departments, suggesting that the CRKP strain was cross-transmitted in neonatal wards. This study is the first report of Klebsiella pneumoniae ST2601 in paediatric patients, revealing simultaneous production of two carbapenemases by Klebsiella pneumoniae, which poses a significant threat to disease recovery in young children. The clinical laboratory should be modified based on its own conditions and clinical needs to carry out carbapenemase type detection. In conclusion, active surveillance and strict infection control measures, particularly for neonatal wards, are urgently needed to prevent further transmission in hospital settings.
Ethical Approval
The guardian of the pediatric patients signed informed consent to participate in the study before the study began and this study was conducted in accordance with the Declaration of Helsinki. The Clinical Research Ethics Committee of the Children’s Hospital of Nanjing Medical University approved the study (202205054-1), as all samples collected in this work were initially used to diagnose patient care without increasing the patient’s medical costs and suffering.
Acknowledgments
This research was supported by the Second Level of the Nanjing Health Youth Talents Training Project (QRX17078).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Stojowska-Swędrzyńska K, Łupkowska A, Kuczyńska-Wiśnik D, Laskowska E. Antibiotic heteroresistance in Klebsiella pneumoniae. Int J Mol Sci. 2021;23(1):449. doi:10.3390/ijms23010449
2. Martin RM, Bachman MA. Colonization, infection, and the accessory genome of Klebsiella pneumoniae. Front Cell Infect Microbiol. 2018;8:4. doi:10.3389/fcimb.2018.00004
3. Han R, Shi Q, Wu S, et al.; China Antimicrobial Surveillance Network (CHINET) Study Group. Dissemination of carbapenemases (KPC, NDM, OXA-48, IMP, and VIM) among carbapenem-resistant enterobacteriaceae isolated from adult and children patients in China. Front Cell Infect Microbiol. 2020;10:314. doi:10.3389/fcimb.2020.00314
4. Pitout JDD, Peirano G, Kock MM, Strydom KA, Matsumura Y. The global ascendency of OXA-48-type carbapenemases. Clin Microbiol Rev. 2019;33(1):e00102–19. doi:10.1128/CMR.00102-19
5. Yin D, Dong D, Li K, et al. Clonal dissemination of OXA-232 carbapenemase-producing Klebsiella pneumoniae in neonates. Antimicrob Agents Chemother. 2017;61(8):e00385–17. doi:10.1128/AAC.00385-17
6. Wei ZQ, Du XX, Yu YS, Shen P, Chen YG, Li LJ. Plasmid-mediated KPC-2 in a Klebsiella pneumoniae isolate from China. Antimicrob Agents Chemother. 2007;51(2):763–765. doi:10.1128/AAC.01053-06
7. Naha S, Sands K, Mukherjee S, et al. KPC-2-producing Klebsiella pneumoniae ST147 in a neonatal unit: clonal isolates with differences in colistin susceptibility attributed to AcrAB-TolC pump. Int J Antimicrob Agents. 2020;55(3):105903. doi:10.1016/j.ijantimicag.2020.105903
8. Chen Y, Zhou Z, Jiang Y, Yu Y. Emergence of NDM-1-producing Acinetobacter baumannii in China. J Antimicrob Chemother. 2011;66(6):1255–1259. doi:10.1093/jac/dkr082
9. Zheng R, Zhang Q, Guo Y, et al. Outbreak of plasmid-mediated NDM-1-producing Klebsiella pneumoniae ST105 among neonatal patients in Yunnan, China. Ann Clin Microbiol Antimicrob. 2016;15:10. doi:10.1186/s12941-016-0124-6
10. Dong F, Zhang Y, Yao K, et al. Epidemiology of carbapenem-resistant Klebsiella pneumoniae bloodstream infections in a Chinese Children’s Hospital: predominance of New Delhi Metallo-β-Lactamase-1. Microb Drug Resist. 2018;24(2):154–160. doi:10.1089/mdr.2017.0031
11. Zou H, Jia X, He X, et al. Emerging threat of multidrug resistant pathogens from neonatal sepsis. Front Cell Infect Microbiol. 2021;12(11):694093. doi:10.3389/fcimb.2021.694093
12. Liu Z, Gu Y, Li X, et al. Identificationand characterization of NDM-1-producing hypervirulent (hypermucoviscous) Klebsiella pneumoniae in China. Ann Lab Med. 2019;39(2):167–175. doi:10.3343/alm.2019.39.2.167
13. Kong Z, Cai R, Cheng C, et al. First reported nosocomial outbreak Of NDM-5-producing Klebsiella pneumoniae in A neonatal unit in China. Infect Drug Resist. 2019;12:3557–3566. doi:10.2147/IDR.S218945
14. Fu B, Yin D, Sun C, et al. Clonal and horizontal transmission of blaNDM among Klebsiella pneumoniae in children’s intensive care units. Microbiol Spectr. 2022;27:e0157421. doi:10.1128/spectrum.01574-21
15. Gong Y, Lu Y, Xue D, et al. Emergence of a carbapenem-resistant Klebsiella pneumoniae isolate co-harbouring dual blaNDM- 6 -carrying plasmids in China. Front Microbiol. 2022;13:900831. doi:10.3389/fmicb.2022.900831
16. Wang X, Li H, Zhao C, et al. Novel NDM-9 metallo-β-lactamase identified from a ST107 Klebsiella pneumoniae strain isolated in China. Int J Antimicrob Agents. 2014;44(1):90–91. doi:10.1016/j.ijantimicag.2014.04.010
17. Xie S, Fu S, Li M, et al. Microbiological characteristics of carbapenem-resistant Enterobacteriaceae clinical isolates collected from county hospitals. Infect Drug Resist. 2020;13:1163–1169. doi:10.2147/IDR.S248147
18. Bai Y, Shao C, Hao Y, Wang Y, Jin Y. Using whole genome sequencing to trace, control and characterize a hospital infection of IMP-4-producing Klebsiella pneumoniae ST2253 in a neonatal unit in a tertiary hospital, China. Front Public Health. 2021;9:755252. doi:10.3389/fpubh.2021.755252
19. Huang YT, Kuo YW, Lee NY, et al.; SMART study group. Evaluating NG-test CARBA 5 multiplex immunochromatographic and cepheid xpert CARBA-R assays among carbapenem-resistant Enterobacterales isolates associated with bloodstream infection. Microbiol Spectr. 2022;10(1):e0172821. doi:10.1128/spectrum.01728-21
20. Yao H, Cheng J, Li A, et al. Molecular characterization of an IncFIIk plasmid co-harboring blaIMP-26 and tet(A) variant in a clinical Klebsiella pneumoniae isolate. Front Microbiol. 2020;11:1610. doi:10.3389/fmicb.2020.01610
21. Wang S, Zhao J, Liu N, et al. IMP-38-producing high-risk sequence type 307 Klebsiella pneumoniae strains from a neonatal unit in China. mSphere. 2020;5(4):e00407–20. doi:10.1128/mSphere.00407-20
22. Patil S, Chen H, Guo C, et al. Emergence of Klebsiella pneumoniae ST307 co-producing CTX-M with SHV and KPC from paediatric patients at Shenzhen Children’s Hospital, China. Infect Drug Resist. 2021;14:3581–3588. doi:10.2147/IDR.S324018
23. Liu E, Jia P, Li X, et al. In vitro and in vivo effect of antimicrobial agent combinations against carbapenem-resistant Klebsiella pneumoniae with different resistance mechanisms in China. Infect Drug Resist. 2021;14:917–928. doi:10.2147/IDR.S292431
24. Guo L, An J, Ma Y, et al. Nosocomial outbreak of OXA-48-producing Klebsiella pneumoniae in a Chinese Hospital: clonal transmission of ST147 and ST383. PLoS One. 2016;11(8):e0160754. doi:10.1371/journal.pone.0160754
25. Xie L, Dou Y, Zhou K, et al. Coexistence of blaOXA-48 and truncated blaNDM-1 on different plasmids in a Klebsiella pneumoniae isolate in China. Front Microbiol. 2017;8:133. doi:10.3389/fmicb.2017.00133
26. Lu MC, Chen YT, Tang HL, et al. Transmission and evolution of OXA-48-producing Klebsiella pneumoniae ST11 in a single hospital in Taiwan. J Antimicrob Chemother. 2020;75(2):318–326. doi:10.1093/jac/dkz431
27. Li X, Ma W, Qin Q, et al. Nosocomial spread of OXA-232-producing Klebsiella pneumoniae ST15 in a teaching hospital, Shanghai, China. BMC Microbiol. 2019;19(1):235. doi:10.1186/s12866-019-1609-1
28. Jia H, Zhang Y, Ye J, et al. Outbreak of multidrug-resistant OXA-232-producing ST15 Klebsiella pneumoniae in a teaching hospital in Wenzhou, China. Infect Drug Resist. 2021;14:4395–4407. doi:10.2147/IDR.S329563
29. European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 10.0; 2020.
30. Clinical and Laboratory Standards Institute. M100‐S29. Performance Standards for Antimicrobial Susceptibility Testing.
31. Zhang P, Shi Q, Hu H, et al. Emergence of ceftazidime/avibactam resistance in carbapenem-resistant Klebsiella pneumoniae in China. Clin Microbiol Infect. 2020;26(1):
32. Rogers BA, Sidjabat HE, Silvey A, et al. Treatment options for New Delhi metallo-beta-lactamase-harboring enterobacteriaceae. Microb Drug Resist. 2013;19(2):100–103. doi:10.1089/mdr.2012.0063
33. Guo X, Wang Q, Xu H, et al. Emergence of IMP-8-producing Comamonas thiooxydans causing urinary tract infection in China. Front Microbiol. 2021;12:585716. doi:10.3389/fmicb.2021.585716
34. Wang X, Wang Y, Zhou Y, et al. Emergence of a novel mobile colistin resistance gene, mcr-8, in NDM-producing Klebsiella pneumoniae. Emerg Microbes Infect. 2018;7(1):122. doi:10.1038/s41426-018-0124-z
35. Tenover FC, Arbeit RD, Goering RV, et al. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol. 1995;33(9):2233–2239. doi:10.1128/jcm.33.9.2233-2239.1995
36. Tilahun M, Kassa Y, Gedefie A, Ashagire M. Emerging carbapenem-resistant enterobacteriaceae infection, its epidemiology and novel treatment options: a review. Infect Drug Resist. 2021;14:4363–4374. doi:10.2147/IDR.S337611
37. Sun K, Chen X, Li C, Yu Z, Zhou Q, Yan Y. Clonal dissemination of multilocus sequence type 11 Klebsiella pneumoniae carbapenemase - producing K. pneumoniae in a Chinese teaching hospital. APMIS. 2015;123(2):123–127. doi:10.1111/apm.12313
38. Mukherjee S, Bhattacharjee A, Naha S, et al. Molecular characterization of NDM-1-producing Klebsiella pneumoniae ST29, ST347, ST1224, and ST2558 causing sepsis in neonates in a tertiary care hospital of North-East India. Infect Genet Evol. 2019;69:166–175. doi:10.1016/j.meegid.2019.01.024
39. Flores-Valdez M, Ares MA, Rosales-Reyes R, et al. Whole genome sequencing of pediatric Klebsiella pneumoniae strains reveals important insights into their virulence-associated traits. Front Microbiol. 2021;12:711577. doi:10.3389/fmicb.2021.711577
40. Pan F, Xu Q, Zhang H. Emergence of NDM-5 producing carbapenem-resistant Klebsiella aerogenes in a pediatric hospital in Shanghai, China. Front Public Health. 2021;9:621527. doi:10.3389/fpubh.2021.621527
41. Zhao J, Zhang Y, Fan Y, et al. Characterization of an NDM-5-producing hypervirulent Klebsiella pneumoniae sequence type 65 clone from a lung transplant recipient. Emerg Microbes Infect. 2021;10(1):396–399. doi:10.1080/22221751.2021.1889932
42. Wang Z, Li M, Shen X, et al. Outbreak of blaNDM-5-harboring Klebsiella pneumoniae ST290 in a tertiary hospital in China. Microb Drug Resist. 2019;25(10):1443–1448. doi:10.1089/mdr.2019.0046
43. Cao X, Zhong Q, Guo Y, et al. Emergence of the coexistence of mcr-1, blaNDM-5, and blaCTX-M-55 in Klebsiella pneumoniae ST485 clinical isolates in China. Infect Drug Resist. 2021;28(14):3449–3458. doi:10.2147/IDR.S311808
44. Lorenzin G, Gona F, Battaglia S, et al. Detection of NDM-1/5 and OXA-48 co-producing extensively drug-resistant hypervirulent Klebsiella pneumoniae in Northern Italy. J Glob Antimicrob Resist. 2022;28:146–150. doi:10.1016/j.jgar.2022.01.001
45. Brinkac LM, White R, D’Souza R, Nguyen K, Obaro SK, Fouts DE. Emergence of New Delhi metallo-β-lactamase (NDM-5) in Klebsiella quasipneumoniae from neonates in a Nigerian hospital. mSphere. 2019;4(2):e00685–18. doi:10.1128/mSphere.00685-18
46. Balm MN, La MV, Krishnan P, Jureen R, Lin RT, Teo JW. Emergence of Klebsiella pneumoniae co-producing NDM-type and OXA-181 carbapenemases. Clin Microbiol Infect. 2013;19(9):E421–3. doi:10.1111/1469-0691.12247
47. Rojas LJ, Hujer AM, Rudin SD, et al. NDM-5 and OXA-181 beta-lactamases, a significant threat continues to spread in the americas. Antimicrob Agents Chemother. 2017;61(7):e00454–17. doi:10.1128/AAC.00454-17
48. Yan JJ, Ko WC, Tsai SH, Wu HM, Wu JJ. Outbreak of infection with multidrug-resistant Klebsiella pneumoniae carrying bla(IMP-8) in a university medical center in Taiwan. J Clin Microbiol. 2001 Dec;39(12):4433-9. doi: 10.1128/JCM.39.12.4433-4439.2001
49. Kong Z, Liu X, Li C, Cheng S, Xu F, Gu B. Clinical molecular epidemiology of carbapenem-resistant Klebsiella pneumoniae among pediatric patients in Jiangsu Province, China. Infect Drug Resist. 2020;13:4627–4635. doi:10.2147/IDR.S293206
50. Wajima T, Sugawara T, Umeda Y, Hagimoto A, Tanaka E, Nakaminami H. Molecular characterisation of carbapenem- and tigecycline-resistant Klebsiella pneumoniae strains isolated from blood and bile samples. J Infect Chemother. 2022;28(2):187–191. doi:10.1016/j.jiac.2021.10.005
51. Naha S, Sands K, Mukherjee S, Saha B, Dutta S, Basu S. OXA-181-like carbapenemases in Klebsiella pneumoniae ST14, ST15, ST23, ST48, and ST231 from septicemic neonates: coexistence with NDM-5, resistome, transmissibility, and genome diversity. mSphere. 2021;6(1):e01156–20. doi:10.1128/mSphere.01156-20
52. Zhang B, Hu R, Liang Q, et al. Comparison of two distinct subpopulations of Klebsiella pneumoniae ST16 co-occurring in a single patient. Microbiol Spectr. 2022;25:e0262421. doi:10.1128/spectrum.02624-21
53. Rawson TM, Brzeska-Trafny I, Maxfield R, et al. A practical laboratory method to determine ceftazidime-avibactam-aztreonam synergy in patients with New Delhi Metallo-beta-lactamase (NDM) producing Enterobacterales infection. J Glob Antimicrob Resist. 2022;29:558–562. doi:10.1016/j.jgar.2022.01.025
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.