Back to Journals » Psychology Research and Behavior Management » Volume 16
Resilience in Informal Caregivers of Patients with Heart Failure in China: Exploring Influencing Factors and Identifying the Paths
Authors Peng Y, Xu Y, Yue L, Chen F, Wang J, Sun G
Received 18 January 2023
Accepted for publication 24 March 2023
Published 6 April 2023 Volume 2023:16 Pages 1097—1107
DOI https://doi.org/10.2147/PRBM.S405217
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Yuanyuan Peng,1 Yan Xu,1 Liping Yue,1 Fanglei Chen,1 Jie Wang,2 Guozhen Sun2,3
1Department of Nursing, School of International Medical Technology, Sanda University, Shanghai, People’s Republic of China; 2Department of Cardiology, the First Affiliated Hospital of Nanjing Medical University, Nanjing, People’s Republic of China; 3School of Nursing, Nanjing Medical University, Nanjing, People’s Republic of China
Correspondence: Guozhen Sun, Department of Cardiology, the First Affiliated Hospital of Nanjing Medical University, Nanjing, China; School of Nursing, Nanjing Medical University, Nanjing, People’s Republic of China, Tel +86 13851769549, Fax +86 25 6830348, Email [email protected]
Background: In the fight against heart failure (HF), informal caregivers are an indispensable part of the team. As a protective factor against stress, resilience can help to enhance caregivers’ psychological adaptation and ultimately increase the quality of care during the HF caregiving period. Recognizing its predictors and exploring how these variables interact could promote tailored strategies to enhancing caregivers’ resilience of HF patients. Thus, this study aimed to identify promoting and risk factors of resilience in informal caregivers of HF patients from the Chinese context and to understand the interactions between these factors and resilience.
Methods: This cross-sectional study was conducted from December, 2020 to March, 2022 among 210 caregivers in Nanjing, China. The General Information Questionnaire, the Connor-Davidson Resilience Scale, the General Self-Efficacy Scale, the Perceived Social Support Scale, the Positive and Negative Affect Scale, the Simplified Coping Style Questionnaire and the Family Hardiness Index were used in this survey. Data were analysed with Pearson’s correlation analysis, the multiple linear regression model and the structural equation modeling (SEM).
Results: The resilience of 210 Chinese HF caregivers was at the moderate and higher level (66.40± 15.08). The SEM had a good fit (root mean square error of approximation=0.047, comparative fit index=0.994, Tucker-Lewis index=0.987). Perceived social support (β=0.390, P< 0.001), positive coping style (β=0.159, P=0.019) and self-efficacy (β=0.332, P< 0.001) had positive direct effects on resilience among HF caregivers, separately. Both perceived social support (β=0.04, P< 0.001) and self-efficacy (β=0.07, P< 0.001) indirectly influenced resilience through positive coping style.
Conclusion: We recommended that multi-dimensional and greater social support, higher self-efficacy and especially, positive coping strategies should be offered or encouraged during the caregiving period, which may contribute to enhancing HF caregivers’ resilience.
Keywords: heart failure, caregivers, resilience, influencing factors, structural equation model, positive coping style, mediator
Introduction
Heart failure (HF), affecting nearly 38 million families worldwide and 13.7 million families in China, has been described as “an unconquered iceberg” of cardiovascular disease in the twenty-first century.1,2 A majority of Chinese patients with stable HF choose to recover at home.3 Nevertheless, HF is a prototypical chronic illness, meaning that rehabilitation is generally long, complex, unstable and slow.1 Hence, when struggling with heart failure, some family members choose to fight side by side with patients, who are referred to as informal caregivers. The effective management of the disease by informal caregivers is an indispensable prerequisite for improving the quality of life, physical and mental health of HF patients, and ultimately promoting patient outcomes.4 Informal caregivers play an important role in patients’ symptom monitoring, medication and dietary management, exercise rehabilitation, psycho-emotional support, and connection with the health-care system.5 However, caregivers usually endure a great burden and have a multitude of unmet needs owing to fluctuations in the trajectory of HF and changes in their lives,6,7 which contributes to the occurrence of anxiety, depression, psychological distress and intense stress.
To overcome these distresses and guarantee the quality of caregiving, caregivers should maintain stability both physically and mentally, and this process is described as “resilience.”8 According to literature, resilience refers to growth or adaptation through disruption, not just recovery or the ability to bounce back. Caregiver resilience has been defined as a process of confirming and developing resources and powers to control stress to achieve positive results and restore self-esteem, life satisfaction, and self-respect.9 Dias et al noted that resilience of caregivers should be defined in association with caregiving tasks, because it implies resistance to stress due to the perception of caregiving demands and burden.10 Resilience has been identified as a protective factor against caregiver stress, which helps to increase the quality of caregiver coping and overall adaptation to difficulties related to caregiving.11
Previous studies have shown that higher levels of caregiver resilience are associated with higher levels of quality of life, better mental health and lower caregiver burden.12 Although resilience of caregivers of HF patients is an important goal of care, a small body of research has focused on this domain. One published study used mixed methods design (quantitative and qualitative) talking about the level of resilience and its associated factors, such as depression, psychological outlook and physical weariness, in informal caregivers of HF patients from the European context.5 Hence, it is also necessary to gain a deeper understanding of resilience of HF caregivers from the Asian context.
The compensatory model of resiliency emphasizes promoting factors and risk factors of resilience and implies that the former can counteract the effects of the latter.13 Based on this model, we explored related factors of resilience of informal HF caregivers from the individual, family and societal perspective. In individual terms, promoting factors include positive coping style, positive emotions and higher self-efficacy; risk factors include negative coping style, negative emotions and lower self-efficacy. In family terms, promoting factors include family hardiness, which has been defined as a family’s ability to work together cohesively, combating stressors and finding solutions to problems.14 From a societal perspective, promoting factors include perceived social support.15 Until now, little is known about how resilience resources interact.16 Previous studies have shown coping strategies usually act as mediators of the mental health (ie, psychological resilience) of the carer.17 Therefore, we hypothesized that coping styles could also function as mediators between other variables and psychological resilience of informal caregivers of patients with heart failure.
Thus, our study has the following objectives: (a) to explore levels of psychological resilience in informal caregivers of HF patients from the Chinese context; (b) to identify promoting and risk factors of caregivers’ resilience; (c) to understand the interactions between these factors and resilience.
Materials and Methods
Design
Our survey was conducted in a Grade A hospital in Nanjing, Jiangsu province, China, between December 12, 2020, to March 14, 2022. The ethics committee of the First Affiliated Hospital of Nanjing Medical University approved this research [approval number: 2020-SR-378]. As a rule, for a multiple linear regression model, the sample size should be at least five to ten times larger than the number of independent variables.18 This study had approximately 27 variables. For the structural equation modeling, the sample size recommendation should be greater or equal to 200. Thus, after considering non-responding subjects, an estimated sample size of 205 was obtained.
Participants
Convenience sampling was applied to recruit caregivers. The participants in this study were recruited from the Department of Cardiovascular Medicine at the First Affiliated Hospital of Nanjing Medical University. If the caregivers met the following criteria, they were considered for this research: (a) were identified as family members or relatives of HF patients and undertook the main care, (b) the care recipients were diagnosed as HF with New York Heart Association (NYHA) classes ranging from II to IV, (c) 18 years or older, (d) able to provide written consent and voluntary participation. The exclusion criteria for caregivers were as follows: (a) the care he/she provided was paid, (b) with psychiatric diagnoses or cognitive impairment and (c) with severe somatic diseases, such as cancer and multiple organ failure.
Procedure
The lead researcher collected patients’ related clinical data, including the left ventricular ejection fraction (LVEF) and the NYHA functional class, from medical records. Two trained assistants used paper questionnaires to gather other data and the questionnaires were self-administered by participants. At the beginning of the study, the nurses explained the purpose of the study to the patients, assuring them that all of the information that they provided would remain anonymous and confidential. It took about 15–20 min for participants to complete this survey. In all, 220 questionnaires were distributed and filled out on site, and 210 valid ones were received (a response rate of 95.5%). This study was conducted in accordance with the principles of the Declaration of Helsinki.
Measurements
The General Information Questionnaire
This questionnaire includes items that describe participants’ sociodemographic characteristics and patients’ related factors, including sex, age, place of residence, marital status, education level, work status, monthly income in Chinese yuan, religious belief, presence of chronic diseases, caregiver relationship to patient and daily time of care.
Connor-Davidson Resilience Scale (CD-RISC)
In this study, caregiver resilience has been defined as a process of confirming and developing resources and powers to control stress to achieve positive results and restore self-esteem, life satisfaction, and self-respect.9 We used CD-RISC to measure it in an objective manner. CD-RISC is a classic and concise instrument designed to assess psychological resilience. A Chinese version of this scale was translated and modified by Xiaonan Yu in 2007.19 This version includes 25 items, covering the aspects of tenacity, strength, and optimism that are rated on a scale of 0–4 (0 = “not true at all” and 4 = “true nearly all the time”). Total scores range between 0 and 100, with higher total scores reflecting greater resilience. The Cronbach’s alpha value for this Chinese version of the CD-RICS was very satisfactory (α=0.91).
General Self-Efficacy Scale (GSES)
The Chinese version of GSES was translated by Caikang Wang in 2001,20 which is used to assess perceived general self-efficacy. This instrument consists of 10 items and each item is scored on a 4-point Likert-scale (1 = “not at all true” and 4 = “exactly true”). Total scores range between 10 and 40. Higher scores indicate a higher level of self-efficacy. The Cronbach’s alpha value was satisfactory (α=0.87).
Perceived Social Support Scale (PSSS)
The Chinese version of the PSSS, which is designed to measure perceived support obtained from family, friends, and significant others, was translated by Qianjin Jiang in 1996.21 The PSSS comprises 12 items and each item is rated on a 7-point Likert-scale (1 = “very strong disagree” and 7 = “very strong agree”). The scores range from 12 to 84, with higher sum scores indicating greater perceived social support. The Chinese version of the PSSS was validated and showed good internal reliability. The Cronbach’s alpha value was 0.88.
Positive and Negative Affect Scale (PANAS)
The Chinese version of the PANAS is a self-report instrument used to assess an individual’s real emotions experienced in the past 1–2 weeks, which was translated by Li Huang in 2003.22 This scale comprises two different dimensions: positive affect (PA) and negative affect (NA). A total of 20 items describe positive or negative emotions, with responses rated from 1 to 5 (1 = “very slightly” and 5 = “very much”). The range for each scale (10 items on each) is from 10 to 50. Higher values indicated higher levels of respondents’ positive or negative emotions. The Cronbach’s alpha value was proved to be very satisfactory (α=0.85 and 0.83 for positive and negative subscale, respectively).
Simplified Coping Style Questionnaire (SCSQ)
The Chinese version of the SCSQ is used to measure an individual’s coping style. Yaning Xie translated and modified it in 1998.23 A total of 20 items are included in this instrument, which are divided into two subscales: positive coping style (12 items) and negative coping style (8 items). Items are graded on a scale of 0–3 (0 = “never” and 3 = “always”). The range for each scale is from 0 to 36 and from 0 to 24, with higher sum scores of each subscale indicating the more frequent usage of that coping style. The Cronbach’s alpha value was satisfactory (α=0.89 and 0.78 for positive and negative subscale, respectively).
Family Hardiness Index (FHI)
The Chinese version of FHI is a self-report instrument that comprises 20 items that evaluate individual’s perceived family hardiness from aspects of commitment, challenge, and control. Yang Liu modified and tested this version among the parents of 330 hospitalized Chinese children in 2011.24 Each item is graded on a 4-point Likert-scale (1 = “false” and 4 = “true”). Scores range from 20 to 80, with higher scores indicating a higher level of family hardiness. The Cronbach’s alpha value obtained for the total Chinese scale was 0.80.
Data Analysis
IBM SPSS version 25.0 and IBM SPSS AMOS version 22.0 were used to analyze data. Descriptive statistics were applied to describe study variables. The independent-sample t-test and one-way ANOVA were used to compare psychological resilience scores among different demographic and clinical variables. Pearson correlation was used to analyse the association between psychological resilience and age, patients’ LVEF%, self-efficacy, perceived social support, emotions, coping styles and family hardiness of HF caregivers. Multiple linear regression analysis was performed to explore the promoting and risk factors of resilience among HF caregivers. For all analyses, P˂0.05 was considered to be statistically significant.
Structural Equation Modeling (SEM) was conducted to assess the inter-relationship between influencing factors and to explore the paths between influencing factors and psychological resilience. The fit of the model to the data was computed using the following: chi-squared/degree of freedom (CMIN/df), root mean square error of approximation (RMSEA), adjusted goodness-of-fit index (AGFI), goodness-of-fit index (GFI), comparative fit index (CFI), normed fit index (NFI), Tucker-Lewis index (TLI) and incremental fit index (IFI). According to conventional criteria, P-values of the chi-square test had to be >0.05. In general, CMIN/df ˂2, RMSEA˂0.05 and (GFI, AGFI, NFI, IFI, CFI and TLI) >0.9 indicate a good fit.25
Results
A Comparison of Resilience Scores Among HF Caregivers with Different Sociodemographic and Patients’ Related Characteristics
In this research, most caregivers were women (53.3%, N=112). The participants’ mean age (±SD) was 46.44±12.99 years, ranging between 18 and 77 years. More than a half participants were adult child caregivers. Most care recipients (119, 56.7%) were in the NYHA function class II and the mean LVEF was (53.79±14.71)%. The results of univariate analysis showed that gender (P=0.004), education level (P˂0.001), monthly income (P=0.004) and daily time of care (P=0.043) were independently correlated with resilience. Table 1 shows other sociodemographic and patients’ related characteristics.
 |
Table 1 Comparison of Resilience Scores Among Different Sociodemographic and Patients’ Related Characteristics Among HF Caregivers |
Correlations Between Resilience and Other Study Variables Among HF Caregivers
The mean total resilience score was 66.40±15.08 and the average score of each item for three dimensions was as follows: tenacity (2.65±0.65), strength (2.83±0.64) and optimism (2.36±0.71). The mean total scores for self-efficacy, perceived social support, positive and negative emotions, positive and negative coping style and family hardiness were 25.69±6.91, 66.15±12.33, 30.93±8.33, 21.15±7.20, 23.73±7.22, 9.63±4.92 and 59.72±10.90, respectively. As shown in Table 2, the results of the Pearson’s correlation analysis indicated that resilience was significantly and positively correlated with self-efficacy (r=0.523, P˂0.001), perceived social support (r=0.530, P˂0.001), positive emotions (r=0.317, P˂0.001), positive coping style (r=0.458, P˂0.001), negative coping style (r=0.162, P=0.019) and family hardiness (r=0.225, P=0.01).
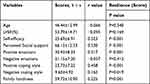 |
Table 2 Correlations Between Resilience and Other Study Variables Among HF Caregivers |
Multiple Linear Regression Analysis of Influencing Factors of Resilience Among HF Caregivers
Gender, education level, monthly income, daily time of care, self-efficacy, perceived social support, positive emotions, positive coping style, negative coping style and family hardiness were included in the multiple linear regression model (performed stepwise), while resilience was a dependent variable. As shown in Table 3, the results of the multiple linear regression analysis revealed that perceived social support, self-efficacy, gender and positive coping style of HF caregivers could affect resilience (β=0.368, 0.289, −0.141 and 0.162, respectively), and the total explanatory quantity of the four variables was 43.7%.
 |
Table 3 Multiple Linear Regression Analysis of Influencing Factors of Resilience Among HF Caregivers |
Outcomes of the Structural Equation Modeling
Structural Equation Modeling (SEM) was used to assess the links among perceived social support, self-efficacy, positive coping style and resilience. Based on a review of the literature and the results of multiple linear regression, we proposed the following hypotheses. H1: All these three factors show positive direct effects on resilience. H2: Positive coping style plays mediating roles between perceived social support, self-efficacy and resilience, separately.
Maximum likelihood (ML) estimation was used to find the best fit to the model parameters. Based on the critical ratio and modification indices, the final structural equation model is shown in Figure 1. Table 4 provides path coefficients between various structural variables. Fit indices of the model are presented as following: P=0.126>0.05, CMIN/df=1.455˂2, RMSEA=0.047˂0.05, GFI=0.978>0.9, AGFI=0.940>0.9, NFI=0.982>0.9, IFI=0.994>0.9, CFI=0.994>0.9, TLI=0.987>0.9. The index results indicated that the revised structural equation model had an adequate fit for the observable data.
 |
Table 4 The Path Coefficients Between Structural Variables |
 |
Figure 1 The Final Structural Equation Model. |
According to results of SEM: (1) Perceived social support (β=0.390), positive coping style (β=0.159) and self-efficacy (β=0.332) had positive direct effects on psychological resilience among HF caregivers, separately. (2) Perceived social support indirectly influenced psychological resilience (β=0.04) through the effect on positive coping style, indicating that positive coping style was a partial mediator. (3) Self-efficacy also indirectly influenced psychology resilience (β=0.07) through the effect on positive coping style and entailed partial mediation. A detailed overview of the results is given in Table 5.
 |
Table 5 Direct, Indirect and Total Effect of Protective Factors on Resilience Among HF Caregivers |
Discussion
This study assessed the resilience of informal caregivers of patients with heart failure from the Asian context and subsequently explored the path between psychological resilience and its influencing factors. In this study, the resilience of HF caregivers was at a moderate and higher level (The average score here was 66.40±15.08 and a cut-off score of 70 was identified as highly resilient caregivers),26 which is similar to the result obtained for HF caregivers from the European context (68.29±24),5 indicating a type of plasticity. As regards dimensions, our finding showed that the dimension of strength had the highest score (2.83±0.64) whereas the lowest score was found in the optimism dimension (2.36±0.71). From the results, on the one hand, caregivers of HF patients may gain strength and growth from long-term caregiving; on the other hand, due to the recurrent and progressive condition and high caregivers burden, it is difficult for caregivers to remain optimistic all the time.
In terms of sociodemographic characteristics, findings revealed that higher levels of resilience can be linked to male gender, higher education level and greater economic incomes. Generally, caregivers with higher levels of education and higher socioeconomic status might be better able to adapt with long-term caregiving.27 Of these, male gender came up as a protective factor associated with caregivers’ resilience through the linear regression analysis. Compared to female, male caregivers seem to be more exposed to environment full of stress and responsibility, which helps boost adaptability to adversity, hence exhibiting higher resilience.28,29 However, some studies demonstrated that gender does not seem to play a role in the levels of resilience.30 Thus, more research is needed on the relations among caregivers’ resilience and sociodemographic features. As regards care context characteristics, findings revealed that those who spent 6–12 h per day dedicated to care reported higher levels of resilience. It can be suggested that caregivers who spend too short caregiving time are usually tired of visiting back and forth; and for those paying too much time, the heavy burden and pressure will gradually shake the inner firmness and finally decrease the level of resilience. Therefore, caregivers should arrange the daily time of care reasonably to improve the quality and efficiency of care.
Positive emotions were found to be positively associated with caregivers’ resilience. Researchers discovered that family members were able to flexibly draw on high-level connections and to develop wider-than-usual ranges of percepts and ideas when they feel positive emotions, which building resilience or compressive capabilities.31 Surprisingly, our study found that caregivers’ negative coping style was also positively correlated with resilience, which is inconsistent with conclusions of previous studies.32,33 Meng et al mentioned that given different contexts, individuals and problems, the negative coping style might not always lead to a negative outcome.34 It is possible that such emotion-focused coping style (ie, smoking; trying to forget the whole thing.) could enable caregivers to achieve a temporary and rapid mental adaptation when facing patients hospitalized for HF exacerbation. However, in the long run, only adopting a positive coping style would be able to really solve the problem and promote resilience. According to the results of the correlation analysis, higher caregivers’ resilience was observed for higher family hardiness. Family hardiness is an important resistance and a family resource that plays a fundamental role in successful adaptation.35 This kind of capabilities and strengths of the entire family enables caregivers to receive more support and protection at the family level, which gives them confidence to face caregiving and subsequently boosts resilience. Hence, strategies designed to improve family hardiness should be promoted, for example, encouraging family members to view heart failure objectively and to adopt a more proactive position when facing the care context, which would help to promote mental adaptation and psychological resilience.36
Our findings revealed caregivers’ perceived social support along with their self-efficacy and positive coping style were all protective factors associated with resilience. A review pointed out that social support can provide individuals with information, emotional support and material assistance, which is closely related to psychological and physical health.37 For primary caregivers of patients with chronic diseases, social support is a strong backing when they face the care context, and has a significant effect on alleviating negative emotions caused by stressful events and improving resilience. In China, influenced by traditional values such as Confucius and Mencius, most caregivers consider it is their responsibility and obligation to take care of their loved ones, so they rarely seek help from other family members or social institutions (especially male caregivers), and therefore lack the ability to actively seek social support. One study demonstrated that adopting information means can effectively improve the social support of informal caregivers of HF patients, and the personalized intervention derived from this is worthy of further clinical verification, application and promotion.37 Durante et al suggested that personal strategies should be combined with social and community support and belongingness, which would ultimately enhance HF caregivers’ resilience.5
Caregivers’ self-efficacy is very important in family informal care, because its level can determine whether caregivers can master their caregiving roles well and complete the high quality of care task.38 Meanwhile, self-efficacy has been proved to reduce caregivers’ physiological stress response (ie, the activation of the hypothalamic–pituitary–adrenal axis (HPA) or the sympathetic nervous system). Caregivers with a high level of self-efficacy can effectively adjust for stress, facing reality with a positive attitude, changing their perceptions about matters of caregiving, and ultimately contributing to improving their own resilience.39 Hence, clinical staff can improve the self-efficacy of HF caregivers through health education, motivational interviewing, relaxation training and so forth, to further strengthening the resilience.38
Positive coping focuses on solving problems. Caregivers preferring to adopt a positive coping style are more likely to actively obtain disease information and make full use of the surrounding social support system during family caregiving, which can effectively reduce psychological stress and enhance coping effect, thus being psychologically beneficial for HF caregivers.
The structural equation model confirmed that the total effects of perceived social support and self-efficacy on caregivers’ resilience were 0.430 and 0.402, separately, which were the two major factors affecting caregivers’ resilience. Both of these two variables not only had positive impacts on resilience but also indirectly affected resilience through the positive coping style, where the positive coping style played a partial mediating role. The higher the level of social support perceived by caregivers, the more emotional and behavioral support they perceived and acquired from family, friends or social organizations. Therefore, when caring for loved ones, their positive coping strategies are enhanced, which can effectively reduce disease-related stress and negative emotions (ie, anxiety, depression and sense of uncertainty) arising from caregiving, then fostering psychological adaption. Self-efficacy of family caregivers refers to the confidence that they have in their ability to provide care (emotional or physical) to their ill family member,40 which can affect the use of coping styles.41 Caregivers with higher levels of self-efficacy tend to choose positive coping strategies to improve their adaptability and acquire growth in the care context, thus promoting the level of resilience.
It is worth noting that in the above two paths, both perceived social support and self-efficacy can ultimately affect the level of resilience through the mediating variable of positive coping style. This indicates that guiding family caregivers of HF patients to master correct coping skills and adopt efficient and healthy coping methods may be a key to enhancing their psychological adaptation.
We have to acknowledge several limitations. As noted above, our sample was taken from a Grade A hospital in Nanjing, Jiangsu province, which is considered to be one of the most developed areas in China. Hence, these results may not generalize to the entire Chinese population, which is comparatively more rural and remote. Additionally, most patients were experiencing the exacerbation of HF in this study, therefore requiring symptomatic treatment at the hospital. Caregivers’ perceptions of resilience may be disturbed by this condition. Furthermore, due to the cross-sectional design, our conclusions regarding causality remain controversial. Lastly, the quantitative design may not reflect participants’ inner true thoughts and emotions. Hence, it is also necessary to conduct a qualitative study to explore other possible promoting and risk factors of caregivers’ resilience in the future.
Conclusion
This study revealed that the psychological resilience of informal caregivers of patients with heart failure in China was at a moderate to higher level. Male gender, perceived social support, self-efficacy and positive coping style were all protective factors associated with caregivers’ resilience. Positive coping style partially mediated between perceived social support, self-efficacy, and caregivers’ resilience. Therefore, to enhance resilience, multi-dimensional and greater social support, higher self-efficacy and especially, positive coping strategies should be offered or encouraged during the caregiving period of HF patients. All in all, this study not only offers valuable insights into facilitating caregivers’ psychological adaption in the HF caregiving context but it also provides a theoretical reference for understanding and encouraging informal caregivers of HF patients from other Asian countries.
Acknowledgments
We would like to thank all the volunteers who participated in the present study.
Funding
This research was supported by grants from the National Natural Science Foundation of China (Project No. 72074124).
Disclosure
The authors report no conflicts of interest in this study.
References
1. Braunwald E. The war against heart failure: the Lancet lecture. Lancet. 2015;385(9970):812–824.
2. Hao G, Wang X, Chen Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012-2015. Eur J Heart Fail. 2019;21(11):1329–1337.
3. Chi C, Zhu JH, Chen H. Effect of comprehensive self-management on improving the prognosis of non-hospitalized heart failure patients. Chin Gen Pract. 2019;22(4):427–432.
4. Martensson J, Dracup K, Canary C, Fridlund B. Living with heart failure: depression and quality of life in patients and spouses. J Heart Lung Transplant. 2003;22(4):460–467.
5. Durante A, Ahtisham Y, Cuoco A, et al. Informal caregivers of people with heart failure and resilience: a convergent mixed methods study. J Adv Nurs. 2022;78(1):264–275.
6. Durante A, Greco A, Annoni AM, Steca P, Alvaro R, Vellone E. Determinants of caregiver burden in heart failure: does caregiver contribution to heart failure patient self-care increase caregiver burden? Eur J Cardiovasc Nurs. 2019;18(8):691–699.
7. Noonan MC, Wingham J, Taylor RS. ‘Who Cares?’ The experiences of caregivers of adults living with heart failure, chronic obstructive pulmonary disease and coronary artery disease: a mixed methods systematic review. BMJ Open. 2018;8(7):e20927.
8. Hwang IC, Kim YS, Lee YJ, et al. Factors associated with caregivers’ resilience in a terminal cancer care setting. Am J Hosp Palliat Care. 2018;35(4):677–683.
9. Chen SC, Huang BS, Hung TM, Lin CY, Chang YL, Chung CF. Factors associated with resilience among primary caregivers of patients with advanced cancer within the first 6 months post-treatment in Taiwan: a Cross-Sectional Study. J Nurs Scholarsh. 2020;52(5):488–496.
10. Dias R, Santos RL, Sousa MF, et al. Resilience of caregivers of people with dementia: a systematic review of biological and psychosocial determinants. Trends Psychiatry Psychother. 2015;37(1):12–19.
11. Trapp SK, Perrin PB, Aggarwal R, et al. Personal strengths and health related quality of life in dementia caregivers from Latin America. Behav Neurol. 2015;2015:507196.
12. Palacio GC, Krikorian A, Gómez-Romero MJ, Limonero JT. Resilience in caregivers: a systematic review. Am J Hosp Palliat Care. 2020;37(8):648–658.
13. Ostaszewski K, Zimmerman MA. The effects of cumulative risks and promotive factors on urban adolescent alcohol and other drug use: a longitudinal study of resiliency. Am J Community Psychol. 2006;38(3–4):237–249.
14. Woodson KD, Thakkar S, Burbage M, Kichler J, Nabors L. Children with chronic illnesses: factors influencing family hardiness. Issues Compr Pediatr Nurs. 2014;38(1):57–69.
15. Hynes L, Saetes S, McGuire B, Caes L. Child and family adaptation to juvenile idiopathic arthritis-A systematic review of the role of resilience resources and mechanisms. Front Psychol. 2019;10:2445.
16. Opsomer S, De Lepeleire J, Lauwerier E, Pype P. Resilience in family caregivers of patients diagnosed with advanced cancer - unravelling the process of bouncing back from difficult experiences, a hermeneutic review. Eur J Gen Pract. 2020;26(1):79–85.
17. Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22(4):337–356.
18. Wang X, Ji X. Sample size estimation in clinical research: from randomized controlled trials to observational studies. Chest. 2020;158(1S):S12–S20.
19. Yu XN, Zhang JX. The Application of the Connor-Davidson Resilience Scale (CD-RISC) in Mainland China. the 10th National Conference of Psychology. Shanghai: Academic Press; 2005.
20. Wang CK, Hu ZF, Liu Y. Evidences for reliability and validity of the Chinese version of general self-efficacy scale. Chine J Applied Psychol. 2001;7(1):37–40.
21. Huang L, Jiang QJ, Ren WH. The correlations between coping styles, social support and psychosomatic symptoms in cancer patients. Chin Mental Health J. 1996;10(4):160–166.
22. Huang L, Yang TZ, Ji ZM. Applicability of the positive and negative affect scale in Chinese. Chin Mental Health J. 2003;17(1):54–56.
23. Xie YN. A preliminary study on the reliability and validity of the simple coping style questionnaire. Chin J Clinical Psychol. 1998;2:53–54.
24. Liu Y, Yang JQ, Ye BL, Shen Q, Zhu JM, Chen MQ. Reliability and validity of the Chinese version of Family Hardiness Index. J Nurs Administrat. 2014;14(11):770–772.
25. Kline RB. Principles and Practice of Structural Equation Modeline. New York: The Guilford Press; 2011:3P.
26. Duran-Gomez N, Guerrero-Martin J, Perez-Civantos D, Lopez JC, Palomo-Lopez P, Caceres MC. Understanding resilience factors among caregivers of people with Alzheimer’s disease in Spain. Psychol Res Behav Manag. 2020;13:1011–1025.
27. Rosenberg AR, Starks H, Jones B. ”I know it when I see it”. The complexities of measuring resilience among parents of children with cancer. Support Care Cancer. 2014;22(10):2661–2668.
28. Lee YJ, Choi YS, Hwang IC, Kim HM, Hwang SW. Resilience at the end of life as a predictor for postloss growth in bereaved caregivers of cancer patients: a prospective pilot study. J Pain Symptom Manage. 2016;51(3):e3–e5.
29. Jones SB, Whitford HS, Bond MJ. Burden on informal caregivers of elderly cancer survivors: risk versus resilience. J Psychoco Oncol. 2015;33(2):178–198.
30. Toledano-Toledano F, Luna D, Moral DLRJ, et al. Psychosocial factors predicting resilience in family caregivers of children with cancer: a cross-sectional study. Int J Environ Res Public Health. 2021;18(2):748.
31. Garland EL, Fredrickson B, Kring AM, Johnson DP, Meyer PS, Penn DL. Upward spirals of positive emotions counter downward spirals of negativity: insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clin Psychol Rev. 2010;30(7):849–864.
32. Li S, Lin Z, Bian QG, Wang MF, Lin L, Zhang HJ. Correlations between resilience, social support and coping style of patients with inflammatory bowel disease. Chin Mental Health J. 2017;31(6):478–479.
33. Tang QF, Zhang GQ. The mediating role of resilience between social support and coping style among caregivers of cancer patients. Modern Preventive Med. 2017;44(24):4478–4481.
34. Meng HY, Chang XX, Gao YZ. Research status quo of coping styles and its related factors of chronic heart failure patients. Chine Nursing Res. 2007;21(31):2828–2830.
35. Ahlert IA, Greeff AP. Resilience factors associated with adaptation in families with deaf and hard of hearing children. Am Ann Deaf. 2012;157(4):391–404.
36. Wang WH, Jiang Z, Yang Z. A review on family resilience factors in families with a cancer patient. J Nurs Sci. 2015;30(23):17–19.
37. Xu YY, Yuan L, Zhang Z, Sun LN, Ding SZ. A review on resilience of primary caregivers of patients with chronic illness. Med Philosophy. 2019;40(24):44–47.
38. Xie WJ, Bai S, Liang GX, Tian Y. A review on self-efficacy of family caregivers of dementia patients. Chine J Gerontol. 2015;13:3779–3781.
39. Tang WJ, Qu WQ, Lu QF, Zhou Y. A review on caregivers’ self-efficacy. Guangxi Med J. 2018;40(14):1607–1610.
40. Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA Cancer J Clin. 2010;60(5):317–339.
41. Ma WN, Yang HF. Relationship among self-efficacy, coping style and mental health of high school students. China J Health Psychol. 2007;15(1):65–67.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
