Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Renoprotective effect of remote ischemic postconditioning in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention
Authors Cao B , Zhang C, Wang H, Xia M, Yang X
Received 3 December 2017
Accepted for publication 18 January 2018
Published 22 February 2018 Volume 2018:14 Pages 369—375
DOI https://doi.org/10.2147/TCRM.S158768
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Bangming Cao,* Chi Zhang,* Haipeng Wang, Ming Xia, Xiangjun Yang
Department of Cardiology, The First Affiliated Hospital of Soochow University, Suzhou, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Background: Whether upper arm remote ischemic postconditioning (RIPostC) exerts protection to kidney in patients with ST-elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PPCI) remains unknown.
Methods: Sixty-four patients with STEMI were randomized to PPCI + RIPostC (n=29) and PPCI (n=35) groups. RIPostC consisting of 4 cycles of 5 minutes occlusion/reperfusion by cuff inflation/deflation of the upper arm was started within 1 minute after the first balloon dilatation. Peripheral venous blood samples were collected before PPCI and at 0.5, 8, 24, 48, and 72 hours after PPCI to detect serum creatinine (SCr) and creatine kinase-MB (CK-MB). Acute kidney injury (AKI) rate and estimated glomerular filtration rate (eGFR) were calculated. The transthoracic echocardiography was performed 7 days after PPCI to assess left ventricular ejection fraction (LVEF).
Results: The patients in the PPCI + RIPostC group had a lower AKI rate compared with those in the PPCI group (P=0.04). The eGFR after PPCI increased in the PPCI + RIPostC group compared to the PPCI group (P<0.01). The peak of CK-MB concentration in the PPCI + RIPostC group was significantly lower than that in the PPCI group (P<0.01). The area under the curve of CK-MB decreased in the PPCI + RIPostC group compared with that in the PPCI group. LVEF in the PPCI + RIPostC group was significantly higher than that in the PPCI group (P=0.04).
Conclusion: Upper arm RIPostC exerts renal and cardiac protection following cardiac ischemia–reperfusion in patients with STEMI.
Keywords: myocardial ischemia reperfusion, ST-segmental elevation myocardial infarction, primary percutaneous coronary intervention, remote ischemic postconditioning
Introduction
ST-elevation myocardial infarction (STEMI) is one of the leading causes of mortality and morbidity worldwide. Rapid reperfusion of the ischemic myocardium can rescue the jeopardized myocardium and reduce infarction size (IS). Emergency percutaneous coronary intervention (PCI) is the first recommended therapy for STEMI.1 Contrast agent for coronary angiography (CAG) can lead to worsening of renal function. Contrast medium-induced acute kidney injury (CI-AKI) is a frequent complication of PCI2–4 and is a predictor of long-term mortality.5
Reperfusion to the ischemic myocardium may abrogate myocardial salvage and even induce further injury, which is termed as ischemia–reperfusion injury (IRI), accounting for up to 50% of the final myocardial IS.6 Novel strategies for reducing myocardial IRI and CI-AKI have been tested. Ischemic postconditioning as a series of repetitive cycles of brief reperfusion alternating with brief reocclusion immediately after the reopening of the culprit vessel showed promising prospects.7,8 However, postconditioning failed in some experimental and clinical studies,9,10 including the largest randomized DANAMI-3-iPOST trial.11
Remote ischemic conditioning (RIC) by brief episodes of ischemia/reperfusion of remote tissues or organs can precede (precondition),12 during (percondition),13,14 or follow (postcondition)15 the coronary occlusion. RIC appears to be promising in clinical setting.16–20 However, Verouhis et al21 (RECOND trial) showed that 7 cycles of lower limb RIC with at least 1 cycle initiated prior to reperfusion failed to reduce myocardial Infarction (MI) size in anterior STEMI patients.
Clinical trials of patients receiving elective PCI have shown that RIC can reduce the incidence of contrast-induced nephropathy (CIN).22,23 Remote ischemic perconditioning (RIPerC) was found to be protective against contrast-induced AKI.24,25 Crimi et al26 reported that lower limb remote ischemic postconditioning (RIPostC) exerted the role of protecting kidney in patients with baseline estimated glomerular filtration rate (eGFR) <77 mL/min/1.73 m2. Till now, there is no trial about whether upper arm RIPostC can reduce contrast-related CI-AKI or CIN in patients with STEMI.
Our research focused on the effect of upper arm RIPostC on renal and cardiac functions in patients with STEMI undergoing primary percutaneous coronary intervention (PPCI).
Methods
Study population
This research protocol complied with the Declaration of Helsinki (revised version, 1996) and was approved by the ethics committee of The First Affiliated Hospital of Soochow University (2015027). All participants signed a written informed consent. The patient’s age ranged from 18 to 80 years. All patients presented within 6 hours of symptom onset. The inclusion criteria were as follows: 1) older than 18 years and 2) chest pain for >30 minutes accompanied by new ST elevation in at least 2 contiguous leads >0.2 mV or new bundle branch block. The exclusion criteria were as follows: 1) chronic kidney disease; 2) eGFR <60 mL/min/1.73 m2; 3) hemodialysis; 4) coma or cardiogenic shock; 5) pregnancy; 6) patients who have received trimethoprim or glibenclamide, which may affect distant ischemic adaptation; 7) severe peripheral arterial disease; and 8) a history of myocardial infarction or coronary artery bypass surgery. Group details are shown in Figure 1.
Study design
This was a single-center, prospective, randomized controlled study. Patients with STEMI were enrolled from January 2015 to June 2016 and subjected to PPCI. The patients were then randomly divided into conventional PPCI or PPCI + RIPostC group. All patients were pre-treated with aspirin 300 mg, clopidogrel 600 mg, or ticagrelor 180 mg loading dose orally and 70 IU/kg unfractionated heparin. Ioversol alcohol (Jiangsu Hengrui Pharmaceutical Co., Ltd.) was used in CAG. Thrombectomy and inhibitors of glycoprotein IIb/IIIa were used if necessary. After PPCI, patients were given lifelong 100 mg aspirin daily combined with 75 mg clopidogrel daily or ticagrelor 90 mg twice a day for 12 months.
RIPostC protocol
All the eligible patients were prepared with a limb cuff wrapped around the upper arm before arterial puncture. In the treatment group, the protocol was started within 1 minute after the first balloon dilatation. The upper arm was exposed to 4 cycles of ischemia/reperfusion, each cycle including 5 minutes cuff inflation at 200 mmHg, followed by 5 minutes complete deflation.
Blood analysis
Serum creatine phosphokinase isoenzyme (creatine kinase-MB [CK-MB])
Blood samples were collected before PPCI and at 0.5, 8, 24, 48, and 72 hours after PPCI. The serum samples were centrifuged at 3,000 rpm for 10 minutes. Serum CK-MB concentrations were measured using a VITROS 350 dry biochemical analyzer. GraphPad Prism 5.02 was used to measure area under the curve (AUC).
Serum creatinine (SCr)
Blood samples were collected before PPCI and at 24 and 72 hours after PPCI, and then the samples were centrifuged at 3,000 rpm for 10 minutes. The supernatant was used to measure SCr using the VITROS 350 biochemical analyzer. The Modification of Diet in Renal Disease (MDRD) formula was used to calculate eGFR. The incidence of AKI was calculated based on preoperative SCr and the highest SCr within 72 hours postoperatively. Contrast-associated AKI was defined as SCr levels increased by 25% or the concentrations of SCr increased by 44 μmol/L compared with preoperation. ΔeGFR was calculated according to preoperative eGFR and minimum eGFR within 72 hours after PCI.
Ultrasonography (UCG)
The patients underwent UCG on the 7th day after PPCI by the doctor, who was unaware of the patient’s treatment, using a GE Vivid 7 Color Ultrasound Imager. The left ventricular ejection fraction (LVEF) was measured by the double plane Simpson method.
Statistical analysis
Data analyses were performed by SPSS 21. Continuous variables were expressed as mean ± SD, and the categorical variables were expressed as percentage. Student’s t-test was used for the continuous variables conformed to normal distribution. The Mann–Whitney U test was used for continuous variables not conformed to normal distribution. The Chi-square test was performed for categorical variables. P<0.05 was statistically significant.
Results
A total of 64 patients were finally enrolled in the study. Of whom, 29 patients underwent PPCI + RIPostC and 35 cases just PPCI. The average age of the 2 groups was 58.93±12.82 and 59.24±10.45 years, respectively. There were 24 males in the PPCI + RIPostC group and 32 males in the PPCI group. There were no significant differences in age and sex ratio between the 2 groups. The clinical features of patients are summarized in Table 1.
All patients received PPCI. Symptom-to-balloon time as a surrogate for total ischemic time in PPCI + RIPostC and PPCI groups were 351±132 and 346±141 minutes, respectively (P=0.90). Patients presented with single culprit vessel, and 24 and 32 cases were included in the PPCI + RIPostC and PPCI groups, respectively. The culprit vessels in PPCI + RIPostC and PPCI groups were as follows: left anterior descending (LAD) artery that was involved in 15 and 18 cases, respectively; right coronary artery (RCA) in 12 and 10 cases, respectively; and left circumflex artery (LCX) in 2 and 7 cases, respectively. The 2 groups were similar in terms of vascular disease (P=0.26). Killip classes on admission were as follows: 28 cases Killip I in the PPCI + RIPostC group and 34 cases Killip I in the PPCI group, with no significant difference between the 2 groups (P=0.36). Postoperative Thrombolysis in Myocardial Infarction (TIMI) 3 flow in the PPCI + RIPostC group was 24 cases and in the PPCI group was 32 cases; TIMI 2 in the 2 groups were 3 and 2 cases, respectively; TIMI 1 in the 2 groups were 2 cases and 1 case, respectively; and no TIMI 0 in both groups after operation. There was no significant difference in postoperative TIMI between the 2 groups (P=0.57). Stent implantation was done in 26 cases in the PPCI + RIPostC group and 33 cases in the PPCI group, and there was no significant difference in the implantation rate between the 2 groups (P=0.65). The contrast dose applied in 2 groups were similar, 88.12±23.05 mL in the PPCI + RIPostC group and 91.50±20.02 mL in the PPCI group (P=0.36).
Postoperative clinical results
Preoperative CK-MB levels were similar in both groups. Serum CK-MB levels at 0.5, 8, 24, 48, and 72 hours after PCI in both groups are shown in Table 2. The levels of CK-MB in the PPCI group at all time points were higher than those in the PPCI + RIPostC group. However, 24 and 48 hours had no significant difference (P>0.05). Postoperative CK-MB peak in the PPCI + RIPostC group decreased significantly compared to the PPCI group (327.60±45.83 vs 395.21±65.42 ng/mL, P<0.01). CK-MB in both groups peaked at 8 hours after PCI. The curve of CK-MB levels at each time point is shown in Figure 2A.
The AUC of CK-MB was calculated by the trapezoidal method. The median AUC for the PPCI + RIPostC group was 754.10 (468.30–893.92). The median AUC for the PPCI group was 807.00 (693.30–1,136.00). The infarct size in the PPCI + RIPostC group was significantly smaller than that in the PPCI group (U=273.50, P=0.04) (Figure 2B).
Echocardiographic results
The postoperative LVEF in the PPCI + RIPostC group was 51.91%±9.42%, which is higher than 47.32%±6.30% in the PPCI group (P=0.04).
Kidney function and AKI
A total of 14 patients had AKI after PPCI, manifested as increased SCr and decreased glomerular filtration rate (11 cases [31.43%] in the PPCI group and 3 cases [10.34%] in the PPCI + RIPostC group). The incidence of AKI in PPCI was significantly higher than that in the PPCI + RIPostC group (P<0.05).
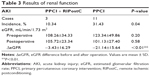
Preoperative eGFRs in PPCI + RIPostC and PPCI groups were 108.26±34.33 and 123.34±49.86 mL/min/1.73 m2, respectively (P=0.20). Postoperative eGFR of the PPCI + RIPostC group was 105.72±23.34 mL/min/1.73 m2, significantly higher than 101.13±27.40 mL/min/1.73 m2 in the PPCI group. ΔeGFRs were −3.43±16.29 and −21.14±15.64 mL/min/1.73 m2 in PPCI + RIPostC and PPCI groups, respectively (P<0.01). eGFR had a tendency to decrease after operation in both groups, with a more significant decrease in the PPCI group. The results of renal function in both groups are shown in Table 3.
Discussion
Our research shows that upper arm RIPostC could mitigate CK-MB release and preserve the LVEF, which might protect the patients with STEMI from IRI. Upper arm RIPostC could also reduce the AKI rate and ameliorate eGFR decline in patients with STEMI. To the best of our knowledge, this is the first research to report the protective role of upper arm RIPostC in cardiac and renal functions in patients with STEMI undergoing PPCI.
In our research, the peak serum CK-MB in the PPCI + RIPostC group was significantly lower compared with the PPCI group. The median AUC of CK-MB over 72 hours in the PPCI + RIPostC group was less than that in the conventional PPCI group. Upper arm RIPostC could reduce the enzymatic IS, which might protect the ischemic myocardium from IRI in patients with STEMI. The culprit vessels in our research include not only LAD artery but also circumflex and RCA. While in the study performed by Crimi et al,20 only occluded LAD artery was included. The majority of published clinical studies have used a manual blood pressure cuff or an automated cuff device to investigate the efficacy of limb RIC; however, lower limb RIC is difficult to be executed sometimes in patients with large lower limb diameter. It is difficult to achieve full blood flow blocking in RIC for certain obese individuals because the lower femoral artery is not as superficial as the brachial artery. Nevertheless, it is simple and convenient to implement the RIC on the upper limb.
Another finding in this research was the detection of SCr in the patients, which could reveal the incidence of CI-AKI. The incidence of AKI in the PPCI group was significantly higher than that in the PPCI + RIPostC group. eGFR had a trend of reduction in both groups, while the PPCI group decreased more significantly. The results suggested that RIPostC might reduce the incidence of AKI in patients with STEMI. Recent studies have found AKI in patients with coronary artery disease (CAD), and especially in patients with STEMI, IRI may have an effect on kidney.27 Both heart and kidneys are the target organs to be protected for patients with STEMI undergoing PCI. Hydration is currently considered an effective method of reducing the incidence of contrast-induced nephropathy (CIN) and has yielded good results in large-scale clinical trials.28 However, for patients with STEMI, preoperative and postoperative hydration is often difficult to be implemented in view of the preoperative time window and cardiac insufficiency.29
Regarding the effects of RIC on renal protection, a number of randomized controlled studies in the setting of CAG and PCI have provided encouraging results. In elective CAG, Er et al22 randomized 100 patients with impaired renal function to standard care or standard care plus RIC by transient and repetitive arm ischemia through 4 cycles of 5 minutes inflation alternated by 5 minutes deflation of a blood pressure cuff. The incidence of AKI was 12% in the RIC group and 40% in the control group. Igarashi et al23 studied 60 patients with moderately impaired renal function (eGFR between 30 and 60 mL/min/1.73 m2), who were scheduled for CAG or PCI. The results showed that 8 patients (26.9%) in the control group suffered AKI but only 2 patients in the RIPreC group (7.7%). Deftereos et al30 reported that RIC during PCI exerted protective function in 225 patients with non-ST-elevation myocardial infarction (NSTEMI). The reduction in the rate of AKI was translated into a trend (of borderline significance) toward better 30-day clinical outcome. However, there are potential safety issues with intermittent balloon inflations in coronary arteries, such as additional myocardial injury and thrombus microembolization. In the trial by Lavi et al,31 patients with stable or unstable angina combined with negative Troponin T at baseline were included in the study. RIC on lower limb showed no protective role against incidence of AKI. Yamanaka et al24 evaluated 94 patients with STEMI who underwent three 5-minute RIC cycles on the upper arm (initiated with diagnosis and continued intraprocedurally and prior to reperfusion) and found that RIC protected against CI-AKI. In a recent study by Olafiranye et al,25 RIC applied in patients with STEMI was found to be associated with lower incidence of AKI and in-hospital mortality. Our research, to some extent, is in consistent with the post hoc analysis by Crimi et al,26 where lower limb RIPostC had protective effect on kidney in patients with baseline eGFR <77 mL/min/1.73 m2.
The cause of CI-AKI is thought to be renal ischemia with toxicity on tubular epithelial cells and vascular endothelial cells. Due to their complex microvascular network and high energy demand, kidneys are sensitive to ischemic injury, which is a major pathophysiological basis of CI-AKI. Endothelial dysfunction, oxidative damage, and sympathetic activation are common pathways involved in IRI of both heart and kidneys.32 RIPostC, RIPerC, as well as RIPreC may share some common features with respect to the mechanism of RIC. The signal transfer to the heart or other organs is through neuronal and humoral communications.33 RIPostC is non-invasive, easily feasible, safe, and inexpensive. Taking existing tantalizing evidence into consideration, there is a need for prospective randomized clinical studies.
This study has few limitations. The potential protective effect of RIPostC on different culprit coronary arteries is not yet clear. The effect of RIPostC by upper arm versus lower limb or joint arm and leg together remains to be elucidated. The baseline renal function in patients enrolled in our research was normal or mildly impaired, with an eGFR >60 mL/min/1.73 m2. Moderate or severely impaired renal function or those hemodialysis excluded. Nevertheless, patients with chronic renal insufficiency, especially those with eGFR <30 mL/min/1.73 m2, might develop a decrease in renal GFR or increase in creatinine clearance. The incidence of CIN could be higher clinically, and further RIPostC studies are deserved. As a suboptimal biomarker, SCr cannot rapidly reflect the degree of kidney injury.23 More sensitive biomarkers such as neutrophil gelatinase-associated lipocalin, urinary liver-type fatty acid-binding protein, and cystatin C are needed to evaluate renal function in future studies. Several other factors such as the level of ions (K, Ca, Mg, and iron), phosphate levels, pH, parathyroid hormone, inflammatory markers, as markers of ventricular arrhythmia risk in renal failure,34 need to be considered in further studies. Our research might not be robust enough to draw a conclusion due to the small sample size.
Conclusion
Upper arm RIPostC imposed to patients with STEMI during PCI could not only reduce the enzymatic IS and preserve LVEF but also decrease the incidence of AKI and lessen the decline of eGFR. The results demonstrated that upper arm RIPostC may protect against myocardial IRI and exert renal protection. Large prospective randomized clinical trials are needed to repeat the results. The implication of our study for clinical practice is that patients with STEMI may benefit from upper arm RIPostC for cardiac and renal protection.
Disclosure
The authors report no conflicts of interest in this work.
References
Andersen HR, Nielsen TT, Rasmussen K, et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349(8):733–742. | ||
Best PJ, Lennon R, Ting HH, et al. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2002;39(7):1113–1119. | ||
McCullough PA, Stacul F, Becker CR, et al. Contrast-Induced Nephropathy (CIN) Consensus Working Panel: executive summary. Rev Cardiovasc Med. 2006;7(4):177–197. | ||
Hertzberg D, Ryden L, Pickering JW, Sartipy U, Holzmann MJ. Acute kidney injury-an overview of diagnostic methods and clinical management. Clin Kidney J. 2017;10(3):323–331. | ||
Margolis G, Vig S, Flint N, et al. Prognostic implications of chronic kidney disease on patients presenting with ST-segment elevation myocardial infarction with versus without stent thrombosis. Cardiorenal Med. 2017;7(2):150–157. | ||
Yellon DM, Hausenloy DJ. Myocardial reperfusion injury. N Engl J Med. 2007;357(11):1121–1135. | ||
Zhao ZQ, Corvera JS, Halkos ME, et al. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2003;285(2):H579–H588. | ||
Staat P, Rioufol G, Piot C, et al. Postconditioning the human heart. Circulation. 2005;112(14):2143–2148. | ||
Freixa X, Bellera N, Ortiz-Perez JT, et al. Ischaemic postconditioning revisited: lack of effects on infarct size following primary percutaneous coronary intervention. Eur Heart J. 2012;33(1):103–112. | ||
Hahn JY, Song YB, Kim EK, et al. Ischemic postconditioning during primary percutaneous coronary intervention: the effects of postconditioning on myocardial reperfusion in patients with ST-segment elevation myocardial infarction (POST) randomized trial. Circulation. 2013;128:1889–1896. | ||
Engstrom T, Kelbaek H, Helqvist S, et al. Effect of ischemic postconditioning during primary percutaneous coronary intervention for patients WITH ST-segment elevation myocardial infarction: a randomized clinical trial. JAMA Cardiol. 2017;2(5):490–497. | ||
Przyklenk K, Bauer B, Ovize M, Kloner RA, Whittaker P. Regional ischemic “preconditioning” protects remote virgin myocardium from subsequent sustained coronary occlusion. Circulation. 1993;87(3):893–899. | ||
Kerendi F, Kin H, Halkos ME, et al. Remote postconditioning. Brief renal ischemia and reperfusion applied before coronary artery reperfusion reduces myocardial infarct size via endogenous activation of adenosine receptors. Basic Res Cardiol. 2005;100(5):404–412. | ||
Schmidt MR, Smerup M, Konstantinov IE, et al. Intermittent peripheral tissue ischemia during coronary ischemia reduces myocardial infarction through a KATP-dependent mechanism: first demonstration of remote ischemic perconditioning. Am J Physiol Heart Circ Physiol. 2007;292(4):H1883–H1890. | ||
Andreka G, Vertesaljai M, Szantho G, et al. Remote ischaemic postconditioning protects the heart during acute myocardial infarction in pigs. Heart. 2007;93(6):749–752. | ||
Botker HE, Kharbanda R, Schmidt MR, et al. Remote ischaemic conditioning before hospital admission, as a complement to angioplasty, and effect on myocardial salvage in patients with acute myocardial infarction: a randomised trial. Lancet. 2010;375(9716):727–734. | ||
White SK, Frohlich GM, Sado DM, et al. Remote ischemic conditioning reduces myocardial infarct size and edema in patients with ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2015;8(1 pt B):178–188. | ||
Yellon DM, Ackbarkhan AK, Balgobin V, et al. Remote ischemic conditioning reduces myocardial infarct size in STEMI patients treated by thrombolysis. J Am Coll Cardiol. 2015;65(25):2764–2765. | ||
Hausenloy DJ, Kharbanda R, Rahbek Schmidt M, et al. Effect of remote ischaemic conditioning on clinical outcomes in patients presenting with an ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Eur Heart J. 2015;36(29):1846–1848. | ||
Crimi G, Pica S, Raineri C, et al. Remote ischemic post-conditioning of the lower limb during primary percutaneous coronary intervention safely reduces enzymatic infarct size in anterior myocardial infarction: a randomized controlled trial. JACC Cardiovasc Interv. 2013;6(10):1055–1063. | ||
Verouhis D, Sorensson P, Gourine A, et al. Effect of remote ischemic conditioning on infarct size in patients with anterior ST-elevation myocardial infarction. Am Heart J. 2016;181:66–73. | ||
Er F, Nia AM, Dopp H, et al. Ischemic preconditioning for prevention of contrast medium-induced nephropathy: randomized pilot RenPro Trial (Renal Protection Trial). Circulation. 2012;126(3):296–303. | ||
Igarashi G, Iino K, Watanabe H, Ito H. Remote ischemic pre-conditioning alleviates contrast-induced acute kidney injury in patients with moderate chronic kidney disease. Circ J. 2013;77(12):3037–3044. | ||
Yamanaka T, Kawai Y, Miyoshi T, et al. Remote ischemic preconditioning reduces contrast-induced acute kidney injury in patients with ST-elevation myocardial infarction: a randomized controlled trial. Int J Cardiol. 2015;178:136–141. | ||
Olafiranye O, Ladejobi A, Wayne M, et al. Renal protection using remote ischemic peri-conditioning during inter-facility helicopter transport of patients with ST-segment elevation myocardial infarction: a retrospective study. J Interv Cardiol. 2016;29(6):603–611. | ||
Crimi G, Ferlini M, Gallo F, et al. Remote ischemic postconditioning as a strategy to reduce acute kidney injury during primary PCI: a post-hoc analysis of a randomized trial. Int J Cardiol. 2014;177(2):500–502. | ||
Tehrani S, Laing C, Yellon DM, Hausenloy DJ. Contrast-induced acute kidney injury following PCI. Eur J Clin Invest. 2013;43(5):483–490. | ||
Maioli M, Toso A, Leoncini M, Micheletti C, Bellandi F. Effects of hydration in contrast-induced acute kidney injury after primary angioplasty: a randomized, controlled trial. Circ Cardiovasc Interv. 2011;4(5):456–462. | ||
Busch SV, Jensen SE, Rosenberg J, Gogenur I. Prevention of contrast-induced nephropathy in STEMI patients undergoing primary percutaneous coronary intervention: a systematic review. J Interv Cardiol. 2013;26(1):97–105. | ||
Deftereos S, Giannopoulos G, Tzalamouras V, et al. Renoprotective effect of remote ischemic post-conditioning by intermittent balloon inflations in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol. 2013;61(19):1949–1955. | ||
Lavi S, D’Alfonso S, Diamantouros P, et al. Remote ischemic postconditioning during percutaneous coronary interventions: remote ischemic postconditioning-percutaneous coronary intervention randomized trial. Circ Cardiovasc Interv. 2014;7(2):225–232. | ||
Seeliger E, Sendeski M, Rihal CS, Persson PB. Contrast-induced kidney injury: mechanisms, risk factors, and prevention. Eur Heart J. 2012;33(16):2007–2015. | ||
Heusch G, Botker HE, Przyklenk K, Redington A, Yellon D. Remote ischemic conditioning. J Am Coll Cardiol. 2015;65(2):177–195. | ||
Mozos I. Laboratory markers of ventricular arrhythmia risk in renal failure. Biomed Res Int. 2014;2014:509204. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.