Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Relationships between heart rate target determined in different exercise testing in COPD patients to prescribed with individualized exercise training
Authors Fabre C, Chehere B, Bart F, Mucci P, Wallaert B, Grosbois JM
Received 10 December 2016
Accepted for publication 7 February 2017
Published 16 May 2017 Volume 2017:12 Pages 1483—1489
DOI https://doi.org/10.2147/COPD.S129889
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Claudine Fabre,1 Baptiste Chehere,1 Frédéric Bart,2 Patrick Mucci,1 Benoit Wallaert,3 Jean Marie Grosbois2,4
1University of Lille, EA-7369 – URePSSS, Unité de Recherche Pluridisciplinaire Sport, Santé, Société, Faculté des Sciences du Sport et de l’EP, Ronchin, 2Centre Hospitalier Béthune, Service de Pneumologie et d’Allergologie, Rue Delbecque, Beuvry, 3CHRU Lille – Service de Pneumologie et Immunoallergologie, Centre des Compétences des Maladies Pulmonaires Rares, Hôpital Calmette, CHRU Lille and Hospital Center Regional University De Lille, Lille, 4FormAction Santé, ZA du Bois, Pérenchies, France
Background: It has been scientifically proven that pulmonary rehabilitation improves exercise tolerance and facilitates the carrying out of daily physical activities. To optimize the physical and physiological benefits, it is necessary to individualize the training intensity for each patient. The aim of this study is to compare the heart rate (HR) responses to three exercise modalities measuring aerobic fitness in chronic obstructive pulmonary disease patients, in order to easily prescribe individual target HRs for endurance training.
Patients and method: Fifty COPD patients (mean age: 60.1±8.5 years) were included in the study. Each patient carried out a cardiopulmonary exercise test, a 6-minute walk test (6MWT) and a 6-minute stepper test (6MST). During these tests, HR was recorded continuously. After the cardiopulmonary exercise test, the HR was noted at the ventilatory threshold (VT) and at the end of the two exercise field tests (6MWTpeak and 6MSTpeak). The values of the HR during the last 3 minutes of both field tests were averaged (6MWT456 and 6MST456). Finally, the HR at 60% of the HR reserve was calculated with the values of the HR measured during 6MWT and 6MST (HRr60%walk, HRr60%step).
Results: The HRs measured during the 6MST were significantly higher than those measured during the 6MWT. The HRr60%step was not significantly different from 6MWT456 and 6MWTpeak HR (P=0.51; P=0.48). A significant correlation was observed between 6MWT456 and 6MWTpeak (r=0.58). The 6MWT456 and 6MWTpeak HR were correlated with HRr60%step (r=0.68 and r=0.62). The VT could be determined in 28 patients. The HRVT was not different from 6MWT456, 6MWTpeak, and HRr60%step (P=0.57, P=0.41 and P=0.88) and was correlated to 6MWT456, 6MWTpeak, and HRr60%step (r=0.45, r=0.40, r=0.48).
Conclusion: An individualized target HR for endurance training can be prescribed from the HR measured during routine tests, such as 6MWT or 6MST.
Keywords: cardiopulmonary exercise testing, chronic obstructive pulmonary disease, 6-minute walk test, 6-minute stepper test, endurance training
Introduction
Exercise training is a major component of pulmonary rehabilitation (PR) allowing an enhancement of the ability to perform activities of daily life and quality of life in patients. An appropriate prescription of exercise during PR is important in ensuring the reduction of dyspnea and asthenia, and peripheral adaptations, especially improvement of muscular function in patients with chronic obstructive pulmonary disease (COPD).1 In order to prescribe and individualize physical activities, the patient’s exercise capacity needs, therefore, to be assessed. A variety of exercise tests are available for COPD, and chosen according to selected objectives.
The prescription of endurance exercise is composed of various parameters: frequency, intensity, duration, type (continuous or interval training) and modality (walking, cycling, stepping and so on). Currently, to prescribe and adjust personalized intensity of the exercise during a PR program, cardiopulmonary exercise testing (CPET)2–4 is resorted to because of its usefulness in determining the mechanisms of exercise intolerance. Following the CPET, the physiologist use a workload based on a percentage of the peak workload2–6 or on a percentage of maximal oxygen uptake observed (VO2peak).2,7 More conveniently, the heart rate (HR) can be used also to prescribe an intensity, as the HR at the ventilatory threshold (HRVT)8 or a percentage of the peak HR.9 The drawback of CPET is the need for trained physiologists to supervise exercise, expensive and specific equipment, and ultimately the HRVT may be undetectable. Thus, despite the proven benefits of retraining in COPD patients, it is probable that, in some cases, the inability to perform a CPET is a barrier to the best prescription of exercise intensity.
Field tests are routinely used to evaluate the functional benefits following a PR program in patients with chronic lung disease,10 such as the 6-minute walk test (6MWT)11–14 or the incremental shuttle walking test.15 In clinical practice, the 6-minute stepper test (6MST) has been recently proposed as a convenient method to evaluate exercise tolerance because the test can be easily implemented, is inexpensive and feasible to be performed at medical offices or patients’ homes.16–19 Finally, these tests can be performed in total safety. Despite their usability, field tests are missing in the practical recommendations for prescribing the intensity of retraining during PR.2–4 Yet, in patients with chronic heart failure, different field tests are used as alternatives to aerobic exercise prescription.20,21 The HR measured at the end of 6MWT (6MWTpeak), which is not different from that of the HRVT, may be used as reference intensity in patients with chronic heart failure.20,21 It would be interesting to find from the HR during the 6MWT and the 6MST a fast marker for medical doctors and patients to prescribe and adjust the intensity of retraining, in different medical offices or in patients’ homes.
Previous studies showed that the HR is higher at the end of 6MST (6MSTpeak) compared with the 6MWTpeak.22,23 This difference could be because of the mobilized muscle mass differences during both tests, resulting in a higher exercise intensity during the 6MST.23 We hypothesized that, 1) the 6MWTpeak and the HRVT are not significantly different; and 2) using a percentage of HR reserve to the 6MST, it is possible to derive an HR similar to the HRVT. Thus, the aim of this study is to compare the response of HR during two field tests to the HRVT measured during a CPET in order to prescribe easily, at home or in medical offices, an individual intensity of exercise in a COPD population.
Material and methods
Subjects
This monocentric retrospective study included 50 patients with mild-to-severe COPD, managed by outpatient PR. The severity of COPD was evaluated by the Global Initiative for Chronic Obstructive Lung Disease stage (Stage I: mild, FEV1/FVC <0.70 and FEV1 ≥80% predicted; Stage II: moderate, FEV1/FVC <0.70 and 50% ≤ FEV1 <80% predicted; Stage III: severe, FEV1/FVC <0.70 and 30% ≤ FEV1 <50% predicted; Stage IV: very severe, FEV1/FVC <0.70 and FEV1 <30% predicted or FEV1 <50% predicted plus chronic respiratory failure).24 All patients included in this study had pre-rehabilitation 6MWT, 6MST, and CPET assessment data available. The study protocol was approved by the Observational Research Protocol Evaluation Committee of the French Language Society of Pulmonology, France (CEPRO n° 2011–036). All the participants provided written informed consent to take part in this study. Inclusion criteria were: stable disease without exacerbation for at least 4 weeks, and no muscular, cardiovascular or neurological problems that limited the performance of a physical exercise. Patients on oxygen therapy were not included in the study. The characteristics of the patients are presented in Table 1.
Protocol
Each patient completed a spirometry (Ergocard, Medisoft, Sorinnes, Belgium) followed by three assessments of aerobic fitness: a CPET on a cycle ergometer (Ergometrics 800, Ergoline, Bitz, Germany), a 6MWT and a 6MST. For safety reasons, the CPET was carried out first, to detect any cardiovascular abnormalities, thus removing contraindications to the exercise. Two to five days later, patients performed a 6MWT and 6MST, always in this order. A rest period between the two tests was established for at least 30 minutes to enable the return of the heart rate to the resting value.
Cardiopulmonary exercise testing
CPET was performed according to an incremental protocol on a cycle ergometer (Ergometrics 800), with blood pressure and electrocardiographic monitoring (Medcard®; Medisoft, Dinant, Belgium), according to the usual guidelines.25 The protocol included a 3-minute rest period, a 3-minute unloaded pedaling period, an incremental ramp exercise (10–15 W/min) pursued to a symptom-limited end point, and a 3-minute recovery time. Inspired and expired gases were collected by a mouthpiece connected to a gas analyzer. Gas exchange was measured breath-by-breath by a computerized system (Ergocard, Medisoft). The exercise was stopped when the subjects, in spite of verbal encouragement, were unable to maintain the imposed pedaling rhythm of 55–60 revolutions per minute. All CPET were limited by dyspnea, fatigue, or both. The oxygen saturation (SpO2) was measured using a portable oximeter (Nonin Oxymontre 3100; Nonin, Plymouth, MN, USA).
Determination of the HR at the ventilatory threshold (VT)
At the end of the CPET, VT was determined by two blinded and independent investigators; VT was defined by an increase in the respiratory equivalent for oxygen with no increase in the respiratory equivalent for carbon dioxide.26 The HRVT was recorded.
Field tests
The six-minute walk test
The 6MWT was performed over a rectangular distance of 70 m in the respiratory medicine department. With the exception of this point, the American Thoracic Society guidelines for 6MWT were followed.27
The six-minute stepper test
The stepper (Go Sport, Grenoble, France) was placed on the ground facing a wall to allow patients to maintain their balance by placing their fingers on the wall.18,28 The step height was set at 20 cm. Patients received standardized instructions adapted from the 6MWT instructions,29 advising them to make the greatest number of steps they could in 6 minutes.
For the two field tests, the protocol included a 3-minute rest period and a 6-minute walking or stepping period. During these periods, continuous monitoring of HR and SpO2 were recorded by a pulse oximeter (Nonin Oxymontre 3100).
No encouragement during these two tests was given; the only indication provided was the remaining time, every minute. The values of the HR of both tests during the last 3 minutes of exercise were averaged (6MWT456 and 6MST456). The peak HR at the end of exercise was noted (6MWTpeak and 6MSTpeak).
Calculation of the target HR at 60% of the heart rate reserve (HRr)
The HRr was calculated as the HR at the sixth minute (HRpeak) – resting HR (HRrest). According to the formula of Karvonen et al,30 60% of HRr corresponds to the following equation: HRr60% = (HRpeak – HRrest) * 0.6+ HRrest. HRrest was measured in a sitting position; HRpeak was the maximum HR measured at the end of the 6MWT and 6MST (6MWTpeak and 6MSTpeak).
Statistical analysis
Data are reported by means ±95% confidence intervals (CIs). The normal distribution of the data was verified by the Kolmogorov-Smirnov test before the interpretation of the analysis of variance (ANOVA). To compare the evolution of HR at rest and at each minute of 6MWT and 6MST, we used an ANOVA on rank for repeated measures (time and test). When the ANOVA test was significant at P<0.05, Tukey’s post hoc test for multiple comparisons was applied. To compare the following variables with each other: 6MWTpeak, 6MSTpeak, 6MWT456, 6MST456, HRVT, HRr60%walk, and HRr60%step, a one-way ANOVA for repeated measures was applied.
Pearson’s correlation coefficient was used to evaluate correlations between the different heart rates of the various exercise tests performed by the patients (CPET, 6MWT, and 6MST). A linear regression was performed to analyze the independent correlations between the HR averages during the last 3 minutes of each test and the HR calculated at 60% HRr. A correlation >0.90 was considered very high; between 0.70 and 0.89 as high; and between 0.50 and 0.69 as moderate.31 The significance level was set at 5%.
Results
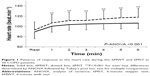
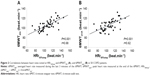
The characteristics of the 50 COPD patients included in this study are presented in Table 1. The responses of the HR to the different evaluation tests are reported in Table 2. The HRs measured during the 6MST were significantly higher than those measured during the 6MWT (Figure 1). However, the HRr60%step was not significantly different from 6MWT456 and 6MWTpeak (P=0.51; P=0.48, respectively). In the same way, 6MWT456 and 6MWTpeak were significantly correlated with HRr60%step (r=0.68, P<0.001; r=0.62, P<0.001, respectively, Figure 2). The HRr60%walk was significantly different from 6MWTpeak, 6MWT456, 6MST456, and 6MSTpeak (P=0.001).
Among the 50 patients, the VT could be determined in only 28 COPD patients. The HRVT (106 beat.minute−1, CI 95% 80–134) was not significantly different from 6MWT456, 6MWTpeak, and HRr60%step (P=0.57, P=0.41, and P=0.88, respectively) but significantly different from HRr60%walk (P=0.001). In these 28 COPD patients, the HRVT was significantly correlated to 6MWT456, 6MWTpeak, and HRr60%step (r=0.45, P=0.02; r=0.40, P=0.03; r=0.48, P=0.02, respectively, Figure 3).
Discussion
The aim of our study was to compare the responses of HR during three exercise tests (6MWT, 6MST and CPET) and to compare these responses in order to prescribe an easily individualized target HR for endurance training. The main result of this study is that, from a field test of 6 minutes (6MWT or 6MST), it is possible to use heart rate, 6MWT456 and 6MWTpeak, or HRr60%step, as a simple marker for the prescription of exercise intensity for an individualized endurance training in patients with COPD.
The review of Achten and Jeukendrup32 has demonstrated the utility of using HR to individualize, at best, training intensity. HR is easily programmable, and COPD patients can use it immediately to adjust the workout intensity during complex exercises, such as interval training or walking outdoors on uneven terrain, with a HR monitor or other connected objects. Finally, data regarding the HR can be downloaded, which makes possible the analysis of training sessions in the absence of a professional on site.
Interest in using HRVT as a training intensity marker has been demonstrated in the associated literature with cardiorespiratory and metabolic adaptations and exercise tolerance following an aerobic training program.8,33,34 So, our results show no significant differences between the HRVT, the 6MWT456, and the 6MWTpeak. Our results demonstrate that the 6MWT456 and 6MWTpeak can be prescribed as a target for personalized exercise intensity as demonstrated in previous studies in patients with heart failure.20,21 However, as previously mentioned, the walking test requires a corridor at least 30 m long, which may be limiting under certain conditions in medical offices and at home. Looking at the measured HRs on a stepper, our results showed a correlation between the HRVT and the HRr60%step, indicating that the 6MST can be used to prescribe individualized exercise intensity. This result is interesting because of the fact that the major limitation to prescribe an individualized intensity at home or medical offices can be avoided. We expected a difference in measured HRs between stepper and walking tests because, in the literature, HRpeak is always higher for the stepper than for the walking test.22,23 This difference could be because of the mobilized muscle mass differences during both tests resulting in a higher exercise intensity during the 6MST.23
In the literature, there are numerous methods described that determine target HRs for endurance training. The intensity of exercise training can be defined by metabolic equivalent of task (METS), calculated as a percentage of VO2max, a percentage of VO2 reserve, or even as a percentage of the theoretical maximum HR.35 The choice, in our study, to focus exclusively on the HR arises from the observation that this variable is easily specified by the clinician, understandable and observable for the patient, easy to measure (by HR sensor or pulse taken at the wrist), can be used in a variety of environments and during many forms of exercise (biking, walking, gardening), and easy and cheap to use when the patient is alone at the exit of the PR program. Thereby, Simmons et al36 demonstrated the utility of using the HR as a marker for the intensity of the exercise.
Some methodological limitations of this study must be presented. The HR measurement is influenced by many factors. First, in our study, the HR was measured in laboratory conditions where the environment was controlled. However, away from this controlled environment, many factors such as wind, cold, or heat can influence the rhythm of the HRs. Second, there is a HR variability between the morning and the afternoon.37 Finally, after several minutes of exercise’ of mild-to-moderate intensity, there is a gradual decrease in stroke volume associated with an increase in HR; this instability is termed cardiac drift. Rowell 38 hypothesized that this drift is related to the combination of water loss and peripheral vasodilation induced by exercise. Thus, a 15% increase in HR during exercise can be noted. Keeping in mind these alterations, it is possible to give patients not a target HR, but rather a range bracket of HR during training. Most HR sensors are able to program training intensity to match the target HR ±5 beats per minute. This technique is proposed in daily practice to our COPD patients.
In conclusion, our results demonstrate that exercise training intensity can be individually prescribed from the HR measured during routine tests such as the 6MWT or 6MST. If the spatial conditions allow, the 6MWT456 and 6MWTpeak can be used as a target HR for the prescription of the intensity of exercise. When space is restricted, the 6MST can be used to prescribe the exercise training intensity using the HRr60%step.
Author contributions
CF, BC, FB, BW, and JMG substantially contributed to conception and design, acquisition of data, or analysis and interpretation of data. CF, BC, FB, PM, and BW drafted the article or revised it critically for important intellectual content. CF, BC, FB, PM, BW and JMG made the final approval of the version to be published. CF, BC, FB, PM, BW and JMG, agreed all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. All authors contributed toward data analysis, drafting and critically revising the paper and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;(2):CD003793. | ||
Zainuldin R, Mackey MG, Alison JA. Optimal intensity and type of leg exercise training for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;(11):CD008008. | ||
Nici L, Donner C, Wouters E, et al. American Thoracic Society/European Respiratory Society Statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173(12):1390–1413. | ||
Gloeckl R, Marinov B, Pitta F. Practical recommendations for exercise training in patients with COPD. Eur Respir Rev. 2013;22(128):178–186. | ||
Troosters T, Casaburi R, Gosselink R, Decramer M. Pulmonary rehabilitation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;172(1):19–38. | ||
Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society Statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. | ||
Cooper CB. Exercise in chronic pulmonary disease: aerobic exercise prescription. Med Sci Sports Exerc. 2001;33(7 Suppl):S671–S679. | ||
Vallet G, Ahmaïdi S, Serres I, et al. Comparison of two training programmes in chronic airway limitation patients: standardized versus individualized protocols. Eur Respir J. 1997;10(1):114–122. | ||
Breyer MK, Breyer-Kohansal R, Funk GC, et al. Nordic walking improves daily physical activities in COPD: a randomised controlled trial. Respir Res. 2010;11:112. | ||
Mador MJ, Modi K. Comparing various exercise tests for assessing the response to pulmonary rehabilitation in patients with COPD. J Cardiopulm Rehabil Prev. 2016;36(2):132–139. | ||
Redelmeier DA, Bayoumi AM, Goldstein RS, Guyatt GH. Interpreting small differences in functional status: the six minute walk test in chronic lung disease patients. Am J Respir Crit Care Med. 1997;155(4):1278–1282. | ||
Puhan MA, Mador MJ, Held U, Goldstein R, Guyatt GH, Schünemann HJ. Interpretation of treatment changes in 6-minute walk distance in patients with COPD. Eur Respir J. 2008;32(3):637–643. | ||
Holland AE, Hill CJ, Rasekaba T, Lee A, Naughton MT, McDonald CF. Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91(2):221–225. | ||
Puhan MA, Chandra D, Mosenifar Z, et al; National Emphysema Treatment Trial (NETT) Research Group. The minimal important difference of exercise tests in severe COPD. Eur Respir J. 2011;37(4):784–790. | ||
Singh SJ, Morgan MD, Hardman AE, Rowe C, Bardsley PA. Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airflow limitation. Eur Respir J. 1994;7:2016–2020. | ||
Rammaert B, Leroy S, Cavestri B, Wallaert B, Grosbois JM. Home-based pulmonary rehabilitation in idiopathic pulmonary fibrosis. Rev Mal Respir. 2011;28(7):e52–e57. | ||
Grosbois JM, Gicquello A, Langlois C, et al. Long-term evaluation of home-based pulmonary rehabilitation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:2037–2044. | ||
Grosbois JM, Riquier C, Chehere B, et al. Six-minute stepper test: a valid clinical exercise tolerance test for COPD patients. Int J Chron Obstruct Pulmon Dis. 2016;11:657–663. | ||
Pichon R, Couturaud F, Mialon P, et al. Responsiveness and minimally important difference of the 6-minute stepper test in patients with chronic obstructive pulmonary disease. Respiration. 2016;91(5):367–373. | ||
Oliveira MF, Zanussi G, Sprovieri B, et al. Alternatives to aerobic exercise prescription in patients with chronic heart failure. Arq Bras Cardiol. 2016;106(2):97–104. | ||
Gremeaux M, Hannequin A, Laurent Y, Laroche D, Casillas JM, Gremeaux V. Usefulness of the 6-minute walk test and the 200-metre fast walk test to individualize high intensity interval and continuous exercise training in coronary artery disease patients after acute coronary syndrome: a pilot controlled clinical study. Clin Rehabil. 2011;25(9):844–855. | ||
Delourme J, Stervinou-Wemeau L, Salleron J, Grosbois JM, Wallaert B. Six-minute stepper test to assess effort intolerance in interstitial lung diseases. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29(2):107–112. | ||
Chéhère B, Bougault V, Gicquello A, Wallaert B. Cardiorespiratory response to different exercise tests in interstitial lung disease. Med Sci Sports Exerc. 2016;48(12):2345–2352. | ||
Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. | ||
American Thoracic Society, American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167(2):211–277. | ||
Wasserman K, Whipp BJ, Koyl SN, Beaver WL. Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol. 1973;35(2):236–243. | ||
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. | ||
Coquart JB, Lemaître F, Castres I, Saison S, Bart F, Grosbois JM. Reproducibility and sensitivity of the 6-minute stepper test in patients with COPD. COPD. 2015;12(5):533–538. | ||
Borel B, Fabre C, Saison S, Bart F, Grosbois JM. An original field evaluation test for chronic obstructive pulmonary disease population: the six-minute stepper test. Clin Rehabil. 2010;24(1):82–93. | ||
Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn. 1957;35(3):307–315. | ||
Munro BH. Statistical Methods for Health Care Research. New York: Lippincott Williams & Wilkins; 2005. | ||
Achten J, Jeukendrup AE. Heart rate monitoring: applications and limitations. Sports Med Auckl NZ. 2003;33(7):517–538. | ||
Alfaro V, Torras R, Prats MT, Palacios L, Ibáñez J. Improvement in exercise tolerance and spirometric values in stable chronic obstructive pulmonary disease patients after an individualized outpatient rehabilitation programme. J Sports Med Phys Fitness. 1996;36(3):195–203. | ||
Serres I, Varray A, Vallet G, Micallef JP, Préfaut C. Improved skeletal muscle performance after individualized exercise training in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 1997;17(4):232–238. | ||
American Thoracic Society. Pulmonary rehabilitation-1999. American Thoracic Society. Am J Respir Crit Care Med. 1999;159(5 Pt 1):1666–1682. | ||
Simmons DN, Berry MJ, Hayes SI, Walschlager SA. The relationship between %HRpeak and %VO2peak in patients with chronic obstructive pulmonary disease. Med Sci Sports Exerc. 2000;32(5):881–886. | ||
Kervio G, Carre F, Ville NS. Reliability and intensity of the six-minute walk test in healthy elderly subjects. Med Sci Sports Exerc. 2003;35(1):169–174. | ||
Rowell LB. Human cardiovascular adjustments to exercise and thermal stress. Physiol Rev. 1974;54(1):75–159. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.