Back to Journals » International Journal of General Medicine » Volume 15
Relationship Between the Use of Preprinted Physician Orders for Hospital-Acquired Fever and Time to Blood Culture Collection: A Single-Center Retrospective Cross-Sectional Study
Authors Harada T , Kosaka S, Hiroshige J, Watari T
Received 10 February 2022
Accepted for publication 16 June 2022
Published 2 July 2022 Volume 2022:15 Pages 5929—5935
DOI https://doi.org/10.2147/IJGM.S361882
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Taku Harada,1,2 Shintaro Kosaka,3 Juichi Hiroshige,1 Takashi Watari4,5
1Division of General Medicine, Showa Medical University Hospital, Tokyo, Japan; 2Division of Diagnostic and Generalist Medicine, Dokkyo Medical University Hospital, Tochigi, Japan; 3Department of Internal Medicine, Nerima Hikarigaoka Hospital, Tokyo, Japan; 4General Medicine Center, Shimane University Hospital, Shimane, Japan; 5Department of Medicine, University of Michigan Medical School, Ann Arbor, MI, USA
Correspondence: Taku Harada, Division of General Medicine, Showa University Koto Toyosu Hospital, 5-1-38 Toyosu Koto-ku, Tokyo, 135-8577, Japan, Tel +81-3-6204-6000, Fax +81-3-6204-6396, Email [email protected]
Purpose: Fever is relatively common in patients admitted to general wards. There is no standardized approach, and little is known about how physicians respond to fever. Additionally, preprinted physician orders are routinely used clinically in hospital medicine, and it is not clear how preprinted physician orders for fever affect the care of patients with fever. Therefore, we aimed to determine whether preprinted physician orders for inpatients have an effect on the time from fever measurement to blood culture collection.
Patients and Methods: This was a single-center, retrospective, cross-sectional study of patients with bacteremia. Between January 1, 2015 and December 31, 2019, 137 hospitalized febrile patients diagnosed with bacteremia by blood culture prepared from blood collected 72 h after hospitalization were included.
Results: Preprinted physician orders with instructions to call the physician if the patient has a fever were present for 59 patients. For preprinted physician orders with instructions to notify the physician about fever onset, 62.7% of the blood cultures were collected within 1 h of fever observation; when preprinted orders were not used, only 23.1% met the 1-h collection criterion. Multivariate analysis showed that preprinted physician orders were significantly associated with blood culture collection within 1 h from the reporting of fever (odds ratio, 4.94; 95% confidence interval, 2.27– 10.70).
Conclusion: Preprinted physician orders with instructions to notify the physician about fever onset were present for only 40% of our sample, and this was related to the time of blood culture collection.
Keywords: hospital-acquired fever, preprinted physician orders, bacteremia
Introduction
Fever is relatively common in patients admitted to general wards; however, studies on fever management are lacking. There is no standardized approach, and little is known about how physicians respond to fever and the diagnostic tests that are commonly used.1 In a systematic review by Kaul et al, the incidence of hospital-acquired fever ranged from 2% to 17%, with infections accounting for 37–74% of the cases.2 Invasive procedures are considered a risk factor for hospital-acquired infections, and the most common infections are pneumonia, urinary tract infections, and bloodstream infections.3 Therefore, these infections are the likely cause of hospital-acquired fever. However, the effects of early intervention in such cases have not been studied,1 and the actual response likely depends on the clinical situation. For example, some studies have shown no significant difference in the timing of antimicrobial administration within 24 h in patients with febrile neutropenia;4 however, for bacteremia caused by Staphylococcus aureus, even a delay of 1 day in the treatment increases the risk of death.5 Fever may be the only—albeit nonspecific—symptom of a catheter-related bloodstream infection (CRBSI). For clinically stable patients with a differential diagnosis of CRBSI, antimicrobial therapy may be deferred; however, a blood culture specimen is a prerequisite to this treatment-related decision.
Preprinted physician orders (known as Shijibo in Japan) provide an excellent opportunity to maximize patient safety and enhance communication among physicians, other medical staff, and patients.6 However, it is not clear how preprinted physician orders for fever affect the care of patients. Therefore, we conducted a single-center, retrospective, cross-sectional study of patients with bacteremia to determine whether preprinted physician orders for inpatients affect the time from the reporting of fever to blood collection for culture.
Materials and Methods
Study Design and Patients
This retrospective study included patients aged 16 years and older who developed bacteremia during hospitalization at Showa University Koto Toyosu Hospital between January 1, 2015, and December 31, 2019. The sample size could not be predicted due to the lack of prior studies. We collected data for a 5-year period starting in 2015, the year after the introduction of electronic medical records at Koto Toyosu Hospital.
We excluded patients in intensive care units, those with contamination (a patient was considered contaminated if the blood culture was positive for coagulase-negative Staphylococcus, Corynebacterium spp., Bacillus spp., Cutibacterium acnes, or Micrococcus spp.), those with bacteremia but no fever, patients being evaluated for known fever, those with only one set of ordered cultures, those with fever onset within 72 h of admission, patients who were terminally ill and admitted for palliative purposes, those with fever onset within 72 h of surgery, and those with non-blood samples. Patients were diagnosed with bacteremia even when two sets of blood cultures were positive for only one set of Enterococcus spp. and Viridian streptococci.7
The following data were collected retrospectively for all patients: age, sex, underlying disease, time from fever to blood culture collection (h), staff on night shift, antimicrobial use, antipyretic analgesic use, active advanced malignancy, indwelling devices (central venous catheter, peripherally inserted central catheter, urinary catheter, and ventilator), post-tracheostomy, the final diagnosis of fever, attending consultant’s department, and preprinted physician orders. The preprinted physician orders were divided into two categories depending on whether they contained instructions for the physician to be called if the patient develops a fever. Fever was defined as an axillary temperature of 38°C or higher. The attending consultant’s department was classified into internal medicine and non-internal medicine. Although there is controversy regarding the justification for a 1-h bundle for sepsis,8–10 the current guidelines recommend blood culture collection and antimicrobials within 1 h for patients with suspected sepsis.11 In addition, a recent multicenter prospective study reported that blood cultures and antimicrobials within 1 h of the 1-h bundle contributed to improved prognosis.12 Accordingly, because of the importance of blood culture collection for the workup of hospital-onset infections and early intervention for sepsis, the primary outcome was blood culture collection within 1 h of confirmation of fever.
Statistical Analysis
Chi-squared or Fisher’s exact tests were used to compare nominal variables. For continuous variables, t-tests or Wilcoxon rank-sum tests were used, as appropriate. We performed a univariate analysis for groups in which blood culture collection was performed within 1 h and after 1 h. Then, we performed a multivariate analysis to determine the association between blood culture collection within 1 h for the factors that showed p<0.1 and “night shift” which was considered clinically important and prevented multicollinearity. Statistical analyses were performed using the EZR (Easy R; Jichi Medical University, Saitama, Japan) software.13 All tests were two-sided, with statistical significance set at p <0.05.
Results
Of the 609 patients with positive blood culture results during hospitalization, 472 were excluded (intensive care units [n=192], contamination [n=52], bacteremia without fever [n=36], evaluated for known fever [n=83], only one set of cultures ordered [n=11], fever onset within 72 h of admission [n=72], terminally ill and admitted for palliative purposes [n=5], non-blood samples [n=21], and fever onset within 72 h of surgery [n=0]). Finally, we included 137 patients with bacteremia diagnosed by blood culture for initial fever after 72 h of hospitalization (Figure 1). The data of the two groups, those with preprinted physician orders (n=59) and those without (n=78), are shown in Table 1. The rate of blood culture collection within 1 h of fever was 62.7% (37/59) in the group with preprinted physician orders with instructions to notify the physician about fever onset and 23.1% (18/78) in the group without the orders.
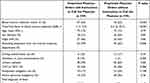 |
Table 1 Characteristics of Patients According to Preprinted Physician Orders for Fever |
 |
Figure 1 Participant flowchart. |
Univariate analysis of the groups in which blood cultures were collected within 1 hour and over 1 hour showed three items with p < 0.1 (Attending physicians from the internal medicine department, female, and preprinted physician orders with instructions to call the physician). Multivariate analyses were performed for these three items and for “night shift hours” which was considered clinically important. In the multivariate analysis, the use of preprinted physician orders with instructions to notify the physician about fever onset was significantly associated with blood culture collection within 1 h of observing fever (odds ratio [OR], 4.94; 95% confidence interval [CI] 2.27–10.70) (Table 2). Additionally, the factor regarding the attending consultant being from the internal medicine department was associated with blood culture not being collected within 1 h of observing fever (OR, 0.40; 95% CI, 0.18–0.87).
 |
Table 2 Comparison Between the Two Groups with Respect to Blood Culture Collection Within 1h and Over 1h |
Discussion
This study revealed that the current status of preprinted physician orders for fever and the setting of the preprinted physician orders may affect the timely diagnosis of nosocomial bacteremia. To the best of our knowledge, no study has examined the relationship between preprinted physician orders with instructions to call the physician if the patient becomes febrile and the time needed to collect blood cultures.
In this study, few blood cultures were collected within 1 h when the attending consultant was an internist. We assumed that internists would be quick at collecting blood cultures for infections that require early intervention, such as CRBSI and bacteremia; hence, this finding was unexpected. This may be because surgeons are generally in charge of postoperative patients, and their sense of responsibility and knowledge and experience in anticipating bacteremia after invasive procedures may have influenced the results. Since this was a single-center study, the heterogeneity of patient background should be considered, and these results should be verified through a survey of intervening physicians and a multicenter evaluation.
This study was not intended to provide an optimal solution for treating febrile patients. However, it is concerning that although 109 patients had an indwelling device, only 45 patients (41.3%) had preprinted physician orders with instructions to notify the physician about fever onset. Ideally, fever should be met with a rapid response in every case. However, the use of preprinted physician orders is both an art and a science, and uniformity may not be desirable.14 Hospitalists should be flexible, depending on the patient’s condition and risk. This study shows that it is desirable to use preprinted physician orders for those at a high risk of hospital-acquired infections.
This study has some limitations. First, this study evaluated only cases of bacteremia in a retrospective manner. Therefore, we could not determine how often bacteremia occurred among patients with fever. Additionally, cases in which patients were called in for fever but no blood culture was taken were not included. Ideally, all cases in which blood cultures were submitted should have been included; however, detailed information was not available for cases submitted for relatively routine testing. Second, we did not measure the respiratory rate; therefore, quick Sepsis-related Organ Failure Assessment (qSOFA) could not be used in clinical decision-making. In Japan, the lack of respiratory rate measurements in various settings, including hospital wards, is a major issue.15 This study was limited to fever because the limitations above were assumed during the design phase. However, it would be desirable to examine all vital signs, including respiratory rate, consciousness, qSOFA, and National Early Warning scores.16 Third, we did not examine potential correlations with prognosis; we believed it would be difficult to conduct a retrospective study because of confounding factors, such as comorbidities, clinical status, fever diagnosis, and initial treatment adequacy. Fourth, this was a single-center, retrospective study; therefore, measurement bias, selection bias, and unintended confounders could not be excluded. Fifth, the primary outcome of this study was the collection of blood culture within 1 h. The optimal approach for the management of fever in the hospital is unknown. Furthermore, the optimal time to collect blood cultures and administer antimicrobials for suspected sepsis is also controversial. There are reports that early antimicrobial administration for suspected sepsis does not improve prognosis17,18 and that the sepsis bundle has been reduced from 3 h to 1 h. The shortening of the length of stay to 1 h is controversial10 and studies have had conflicting results regarding the 1-h bundle for sepsis;12,19 however, in recent years, the 1 h bundle for sepsis is gaining recognition, additionally 1 h bundle is recommended within the Surviving sepsis campaign guidelines 2021.11 In addition, blood cultures are desirable for evaluation of nosocomial pneumonia, catheter-associated bloodstream infection, and catheter-associated urinary tract infection, which are the most frequent nosocomial infections. Accordingly, we determined that blood culture collection within 1 h was desirable. Sixth, the confounding factors included in this study may be insufficient. Ideally, it would be prudent to also consider factors such as patient health status (patients who are more ill are more likely to have preprinted orders and receive an earlier response) and physician characteristics (younger physicians who are more diligent and dedicated may be more likely to document printed instructions and respond to patients more quickly). However, the content of the instruction book can change on a daily basis, and we were unable to ascertain whether it was the admitting physician, attending consultant, or on-call physician who entered the information. We also could not assess the characteristics of the physicians who received the calls.
Future research should investigate whether nurses should notify physicians for in-hospital fevers, regardless of reprinted physician’s order. In addition, a large multicenter prospective study on hospital-onset fever considering the differences in preprinted physician orders between internists and non-internists, characteristics of the physicians who receive calls, patient background, and non-bacteremia cases should be conducted.
Conclusion
Preprinted physician orders with instructions to notify the physician about fever onset were present for only 40% of the sample and were related to the blood culture collection time. Depending on the risk of infection among hospitalized patients, it may be desirable to use preprinted physician orders with instructions to call the physician if the patient becomes febrile to facilitate timely acquisition of blood cultures. However, given the lack of research on the management of fever in hospitalized patients, further multicenter, large-scale studies must be carried out to optimize patient outcomes.
Abbreviations
CI, confidence interval; CRBSI, catheter-related bloodstream infection; OR, odds ratio; qSOFA, quick Sepsis-related Organ Failure Assessment.
Ethics Statement
This study was approved by the ethical review board of Showa University Koto Toyosu Hospital (No. 20T7045) and conducted as per the Declaration of Helsinki. The ethic committees approved the request to waive the informed consent. The research presented no risk of harm to subjects and involved no procedures for which written consent is normally required for this retrospective study. All data were anonymized or maintained with confidentiality.
Acknowledgment
We thank Editage (www.editage.jp) for English-language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
We have no potential conflicts of interest related to this manuscript. This study did not receive any funding.
References
1. Howard-Anderson J, Schwab KE, Chang S, Wilhalme H, Graber CJ, Quinn R. Internal medicine residents’ evaluation of fevers overnight. Diagnosis. 2019;6(2):157–163. doi:10.1515/dx-2018-0066
2. Kaul DR, Flanders SA, Beck JM, Saint S. Brief report: incidence, etiology, risk factors, and outcome of hospital-acquired fever: a systematic, evidence-based review. J Gen Intern Med. 2006;21(11):1184–1187. doi:10.1111/j.1525-1497.2006.00566.x
3. Trivalle C, Chassagne P, Bouaniche M, et al. Nosocomial febrile illness in the elderly: frequency, causes, and risk factors. Arch Intern Med. 1998;158(14):1560–1565. doi:10.1001/archinte.158.14.1560
4. Butts AR, Bachmeier CC, Dressler EV, et al. Association of time to antibiotics and clinical outcomes in adult hematologic malignancy patients with febrile neutropenia. J Oncol Pharm Pract. 2017;23(4):278–283. doi:10.1177/1078155216687150
5. Minejima E, Mai N, Bui N, et al. Defining the breakpoint duration of Staphylococcus aureus bacteremia predictive of poor outcomes. Clin Infect Dis. 2020;70(4):566–573. doi:10.1093/cid/ciz257
6. Ehringer G, Duffy B. Promoting best practice and safety through preprinted physician orders. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches. Rockville (MD): Agency for Healthcare Research and Quality; 2008.
7. Doern GV, Carroll KC, Diekema DJ, et al. Practical guidance for clinical microbiology laboratories: a comprehensive update on the problem of blood culture contamination and a discussion of methods for addressing the problem. Clin Microbiol Rev. 2019;33(1):e00009–19. doi:10.1128/CMR.00009-19
8. Kalantari A, Rezaie SR. Challenging the one-hour sepsis bundle. West J Emerg Med. 2019;20(2):185–190. doi:10.5811/westjem.2018.11.39290
9. CMS statistics reference booklet. Edition. Centers for Medicare & Medicaid Services; 2016. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMS-Statistics-Reference-Booklet/2016.html.
10. Spiegel R, Farkas JD, Rola P, et al. The 2018 surviving sepsis campaign’s treatment bundle: when guidelines outpace the evidence supporting their use. Ann Emerg Med. 2019;73(4):356–358. doi:10.1016/j.annemergmed.2018.06.046
11. Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–e1143. doi:10.1097/CCM.0000000000005337
12. Umemura Y, Abe T, Ogura H, et al. Hour-1 bundle adherence was associated with reduction of in-hospital mortality among patients with sepsis in Japan. PLoS One. 2022;17(2):e0263936. doi:10.1371/journal.pone.0263936
13. Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48(3):452–458. doi:10.1038/bmt.2012.244
14. Duffy B. The art and science of preprinted physician orders. J Healthc Qual. 2007;29(6):7–32. doi:10.1111/j.1945-1474.2007.tb00219.x
15. Watari T. Utilization of vital signs in clinical practice. J Jpn Soc Intern Med. 2019;108(12):2460–2466. (). doi:10.2169/naika.108.2460
16. Usman OA, Usman AA, Ward MA. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the emergency department. Am J Emerg Med. 2019;37(8):1490–1497. doi:10.1016/j.ajem.2018.10.058
17. Tantarattanapong S, Hemwej T. Door-to-antibiotic time and in-hospital mortality of elder patients presenting to emergency department with sepsis; a cross-sectional study. Arch Acad Emerg Med. 2021;9(1):e44. doi:10.22037/aaem.v9i1.1266
18. Alam N, Oskam E, Stassen PM, et al. Prehospital antibiotics in the ambulance for sepsis: a multicentre, open label, randomised trial. Lancet Respir Med. 2018;6(1):40–50. doi:10.1016/S2213-2600(17)30469-1
19. Baghdadi JD, Brook RH, Uslan DZ, et al. Association of a care bundle for early sepsis management with mortality among patients with hospital-onset or community-onset sepsis. JAMA Intern Med. 2020;180(5):707–716. doi:10.1001/jamainternmed.2020.0183
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
