Back to Journals » Clinical Ophthalmology » Volume 12
Relationship between preoperative axial length and myopic shift over 3 years after congenital cataract surgery with primary intraocular lens implantation at the National Institute of Ophthalmology of Peru, 2007–2011
Authors Valera Cornejo DA , Flores Boza A
Received 26 September 2017
Accepted for publication 13 December 2017
Published 23 February 2018 Volume 2018:12 Pages 395—399
DOI https://doi.org/10.2147/OPTH.S152560
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Diego Alejandro Valera Cornejo,1 Abel Flores Boza2
1Research Department, Vista Clinic, 2Pediatric Ophthalmology Department, National Institute of Ophthalmology of Peru, Lima, Peru
Objective: To determine the relationship between the preoperative axial length and the myopic shift over 3 years after congenital cataract surgery with primary intraocular lens implantation and other related factors.
Methods: In this retrospective cohort study, the axial length was measured and assigned into 2 groups (>21.5 mm and ≤21.5 mm), visual axis obscuration, laterality of cataract, age of surgery and follow-up time were assessed and compared to the myopic shift.
Results: The mean myopic shift was 3.6 (standard deviation [SD]: 2.3) diopters (D) in all patients; 3.2 (3.3) and 3.9 (3.2) D for each group respectively (p=0.359). In unilateral cataracts the mean myopic shift was 6.3 D and in bilateral cases was 3.0 D (p=0.001). In bilateral cataracts, the shift was 2.6 D (SD: 2.0) and 3.4 D (SD: 1.8), respectively (p=0.098).
Conclusion: There was no relationship between the initial axial length and the myopic shift in all patients. Unilateral cataracts had a greater myopic shift over 3 years.
Keywords: axial length, eye, refraction, ocular, cataract, congenital, pseudophakia, child
Introduction
In children, 10%–38% of blindness is caused by congenital cataract.1,2 Primary intraocular lens (IOL) implantation with primary posterior capsulorhexis and anterior vitrectomy in pediatric cataract has been the choice of surgical procedure since quite some time now in patients aged <2 years.3 However, the age at which IOL needs to be implanted is still debatable especially due to its complications.4
How the presence of cataract, surgical removal of it and insertion of an IOL (pseudophakia) may affect the ocular growth, and its subsequent refractive change is poorly understood.5 Several factors such as time of surgery, aphakia, pseudophakia, laterality, visual deprivation and axial length have been reported to influence axial growth and visual prognosis.6–8 Several studies show much variability on how axial growth behaves in pseudophakic children after surgery.9–15
Regarding refractive change, most patients report an expected myopic shift from around −2.00 to −6.00 diopters (D)9,12,16,17 due to increased axial growth during the first 3 years of life.14 Although the factors that are related to this refractive change have not been evaluated in detail, some studies suggest that eyes with a longer axial length would have less axial growth after surgery and therefore less myopic shift.18
It is necessary to obtain a final refractive objective that leads or brings the child closer to emmetropia (ideal ophthalmological condition without the use of spectacles) in adulthood; as the pseudophakic eye of a young child grows, we anticipate a large myopic shift, therefore, the selection of an IOL power that results in a large hyperopic error in the immediate postoperative period is recommended,9,19,20 for which, the child would need to wear spectacles, but there is no consensus on how hyperopic the IOL should be.
Therefore, the objective of this study was to evaluate the relationship between pre operative axial length and the myopic shift; this would be useful to determine the ideal pseudophakic refractive target and the final visual state that could bring closer to emmetropia in adulthood. The secondary end point was to identify other possible factors that could be associated with greater myopic shift.
Materials and methods
Design and subjects
An analytical retrospective cohort study was performed. The medical records of patients who underwent congenital cataract surgery with IOL implantation in the pediatric ophthalmology service at the National Institute of Ophthalmology of Peru during the period of 2007–2011 were reviewed.
Patients younger than 4 years who underwent cataract surgery with primary IOL implantation, primary posterior capsulorhexis and anterior vitrectomy were included. Patients who had cataracts of another etiology or other associated ocular pathology (persistent hyperplastic primary vitreous, congenital glaucoma, microcornea and retinopathy of prematurity) were excluded.
The data on the variables of interest was collected from the clinical records of the Institute. Prior to surgery, all patients underwent keratometry measurements using the Retinomax handheld system (Nikon Instruments, Melville, NY, USA), and A-Scan ultrasound and B ultrasonography (Aviso; Quantel Medical, Bozeman, MT, USA) for axial length measurement and evaluation of the posterior pole, respectively, were performed by a skilled ophthalmologist in the operating room under general anesthesia.
Information on immediate refraction (spherical equivalent in diopters) was taken after surgery (1–5 months) and after 3 years, and then the myopic shift was calculated at this time. In addition, the mean myopic shift was correlated with the following variables: axial length (major and minor equal to 21.5 mm), visual axis obscuration (present or absent), cataract laterality (unilateral or bilateral), time of surgery (≤12 years and >12 years) and total follow-up time (months).
The population was divided into 2 groups: patients with an axial length of >21.5 (group 1) and patients with an axial length of ≤21.5 mm (group 2). The mean myopic shift was estimated to be 2.5 D (standard deviation [SD]: 2) and 3.8 D (SD: 2) in group 1 and group 2, respectively. With this, a sample size of 76 patients was estimated, with a power of 80%, a 95% confidence interval and a 5% error. The sample was randomly selected (probabilistic sampling), and the sample unit was the operated eyes of congenital cataract.
Surgical procedure and IOL selection
All patients underwent general anesthesia. A clear corneal 2.75 mm incision and side port paracentesis were made. Ophthalmic viscoelastic device (OVD) (sodium chondroitin sulfate 4.0%–sodium hyaluronate 3.0% Viscoat; Alcon Laboratories, Inc., Fort Worth, TX, USA) was injected into the anterior segment, and anterior continuous curvilinear capsulorrhexis was done. Hydrodissection was performed by injecting balanced salt solution (BSS) through a 30-gauge cannula into the peripheral cortex, and then the lens was aspirated by phacoaspiration through clear corneal side ports with Infiniti Ozil IP Vision System (Alcon Laboratories, Inc.) followed by the implantation of a 1 piece foldable hydrophobic IOL AcrySof IQ® SN60WF (Alcon Laboratories, Inc.) into the bag. Before IOL placement, a primary posterior capsulorhexis was performed, and anterior vitrectomy through the pars plana/plicata was done at the end of the surgery. Side port wounds were hydrated with BSS, and the main wound was closed with 10–0 nylon suture.
The IOL power was calculated based on the Haigis-L formula targeting a 9 D undercorrection for infants 3–6 months of age, a 7 D undercorrection for infants 7–12 months of age, a 5 D undercorrection for infants 1–2 years of age, a 4 D undercorrection for infants 2–3 years of age and a 3 D undercorrection for infants 3–4 years of age.
Statistics
The description of the results was made using mean value as a measure of central tendency and SD as a measure of dispersion. Categorical variables were described using frequency and percentage measures. Student’s t-test was used to compare the mean values of the variables and a regression analysis was performed. All analyses were performed using STATA 12 (StataCorp LP, College Station, TX, USA).
Ethical considerations
The study complied with the Declaration of Helsinki. The ethics committee of the National Institute of Ophthalmology approved the study, and patient consent to review their medical records was not required. Confidentiality of patient identity was ensured.
Results
The total population was 370 patients. Of these, 80% had a diagnosis of interest and only 26% met the inclusion criteria with a total of 76 eyes from 46 patients. Of the total, 43.2% were male the mean age of surgery was 25.3 months (SD: 16.5 months). The mean preoperative axial length was 21.2 mm (SD: 2.4 mm) and 56.6% had an axial length of <21 mm; the average of the first refraction achieved was 3.3 D (SD: 3.2 D), in 4.7 months (SD: 5.9 months), and the mean IOL implanted was 24.0 D (SD: 5.79).
In addition, the mean total postoperative follow-up time was 39.7 months (SD: 14.1 months); bilateral cataract was present in 82.9% of patients and visual axis obscuration in 42% (Table 1).
  | Table 1 Baseline characteristics (n=76) |
The mean myopic shift at 3 years in all patients was 3.6 D (SD: 2.3 D), but in group 1 it was 3.2 D (SD: 3.3) and in group 2 it was 3.9 D (SD: 3.2) (p=0.359). In bilateral cataracts, this shift was 2.6 D (SD: 2.0) and 3.4 D (SD: 1.8), respectively, in each group (p=0.098) (Tables 2 and 3). The mean follow-up time in bilateral cataracts was 38.9 months (SD: 12.9 months) with a mean myopic shift of 3.0 D, and it was 43.6 months (SD: 19.2 months) in unilateral cataracts with a mean myopic shift of 6.3 D (p=0.001) (Table 2). In this type of cataract, a greater myopic shift was observed in both groups (6.7 D [SD: 6.7] and 6.1 D [SD: 6.3], p=0.882) with a mean follow up time of 43.6 (SD: 19.2) months.
  | Table 2 Relationship between axial length and others factors associated with average myopic shift (diopters) in children with pseudophakia (n=76) |
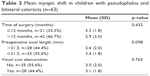  | Table 3 Mean myopic shift in children with pseudophakia and bilateral cataracts (n=63) |
It was observed that the myopic shift had a tendency to have a direct relationship with the time after the surgery being 1.95 D (at 1–2 years), 3.46 D (at 2–3 years) and 3.84 D (at 3 years) (Figure 1).
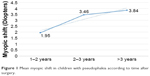  | Figure 1 Mean myopic shift in children with pseudophakia according to time after surgery. |
In the regression analysis, no relationship between the myopic shift and the initial axial length was found in all the patients (R2=0.03; p=0.13), but a tendency to show a negative correlation was seen (Figure 2).
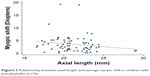  | Figure 2 Relationship between axial length and average myopic shift in children with pseudophakia (n=76). |
Discussion
During development, the axial length is continuously increasing being much more in the first years of life; it is believed that the presence of cataract, removal of it or presence of IOL would affect this growth. This study included congenital cataracts with no other associated pathology in children younger than 4 years, which would be the period of greater ocular growth. The reason for choosing an axial length of 21.5 mm was because Hussain et al21 findings in apparently normal children were 20 mm at 12 months of age and 21 mm at 4 years; in addition to this, Apaza et al22 found an average axial length of 21.4 mm in children younger than 5 years with congenital cataract.
There was no statistically significant relationship between initial axial length and myopic shift at 3 years (3.2 [3.3] vs 3.9 [3.2] p=0.359) in all patients; however, in the bilateral cataract group, there was a tendency of greater myopic shift with smaller axial lengths (2.6 [2.0] vs 3.4 [1.8] p=0.098); no studies have analyzed these 2 variables, but there are some studies that analyze the ocular growth after the surgery with great variability of results.9–15 This trend would be in agreement with what was found by Trivedi and Wilson,18 which suggested that eyes with a longer axial length would have less growth after surgery. However, many studies do not show any changes in axial growth after surgery. Griener et al23 found less axial growth. Hutchinson et al24 and Hussin and Markham14 did not find this relationship.
In our study, there was a significant relationship with the laterality of cataract and myopic shift, with unilateral cataracts being the group with the greatest myopic shift at 3 years. This finding also coincides with those of Hoevenaars et al,25 Kora et al26 and Vasavada et al,27 who found greater axial growth in unilateral cataracts. Kim et al28 found a greater myopic change in amblyopic eyes.
There were no differences in relation to the time of the surgery; however, many authors show the greatest myopic shift in the first years of life. The studies carried out by Nischal et al,29 Crouch et al,17 Inatomi et al,12 Lambert et al15 and Hoevenaars et al25 showed that there is a greater myopic shift in patients younger than 2 years. In our study, the patients were <4 years old, so there was no comparison with older patients; in addition, pathologies associated with other causes of opacity were excluded.
In this study, there was no relationship with visual axis obscuration since in all cases the visual axis was surgically cleared in the first months of being established. Some argue that the visual deprivation due to the visual axis obscuration would increase myopic shift.27 Our mean myopic shift was 3.6 D at 3 years, and the results are similar to several studies.29 In addition, it was also observed that the longer the follow-up time, the myopic shift increased, being greater in the first 2–3 years of life and then decreasing after this age; this is also evident in other studies,17,29 since this is the age of greatest axial growth in the child.
It is important to note that this is the only study that has sought to relate preoperative axial length and myopic shift, and other variables such as unilaterality have been found to be related to greater myopic shift. This will help us get closer to having a better IOL prediction to place in these patients. This is a great strength of this study despite the variability in the refraction data due to the fact that it had several operators during its measurement and could have some influence in the final results of the study.
Conclusion
It is necessary to have tools that help us predict a better postoperative refraction and to choose an IOL, which could lead the child to emmetropia as close as possible.
There was no relationship between the myopic shift and the initial axial length in all the patients, but in the bilateral cataract group, a tendency to greater myopic shift with smaller axial lengths was found; hence, this variable should be investigated more in this group.
Finally, it was concluded that laterality is a useful variable in predicting myopic shift, and hence, a more hyperopic refractive target in children with unilateral cataracts is recommended.
Disclosure
The authors report no conflicts of interest in this work.
References
Rahi JS, Dezateux C; British Congenital Cataract Interest Group. Measuring and interpreting the incidence of congenital ocular anomalies: lessons from a national study of congenital cataract in the UK. Invest Ophthalmol Vis Sci. 2001;42(7):1444–1448. | ||
Hosal BM, Biglan AW, Elhan AH. High levels of binocular function are achievable after removal of monocular cataracts in children before 8 years of age. Ophthalmology. 2000;107(9):1647–1655. | ||
Ochoa-Gómez ML, Fabila-Maya M, Ruiz-Quintero NC, Ruiz-Esmenjaud S, Navarro-López P, Garibay-Velázquez B. Manejo quirúrgico y complicaciones de la catarata congénita. Experiencia de cinco años en la Asociación para Evitar la Ceguera en México [Surgical management and complications of congenital cataract. Five years experience in the Asociacion para Evitar la Ceguera Mexico]. Rev Mex Oftalmol. 2003;77(5):180–183. Spanish. | ||
Plager DA, Lynn MJ, Buckley EG, Wilson ME, Lambert SR; Infant Aphakia Treatment Study Group. Complications in the first 5 years following cataract surgery in infants with and without intraocular lens implantation in the Infant Aphakia Treatment Study. Am J Ophthalmol. 2014;158(5):892–898. | ||
Nihalani BR, VanderVeen DK. Comparison of intraocular lens power calculation formulae in pediatric eyes. Ophthalmology. 2010;117(8):1493–1499. | ||
Rajavi Z, Mokhtari S, Sabbaghi H, Yaseri M. Long-term visual outcome of congenital cataract at a Tertiary Referral Center from 2004 to 2014. J Curr Ophthalmol. 2016;27(3–4):103–109. | ||
Rong X, Ji Y, Fang Y, Jiang Y, Lu Y. Long-term visual outcomes of secondary intraocular lens implantation in children with congenital cataracts. PLoS One. 2015;10(7):e0134864. | ||
Bao YZ, Chen Y, Wu X, Miao H. Long-term outcome after bilateral cataract surgery in infants with congenital cataract. Zhonghua Yan Ke Za Zhi. 2013;49(5):395–398. | ||
Flitcroft DI, Knight-Nanan D, Bowell R, Lanigan B, O’Keefe M. Intraocular lenses in children: changes in axial length, corneal curvature, and refraction. Br J Ophthalmol. 1999;83(3):265–269. | ||
Filipek E, Koraszewska-Matuszewska B, Samochowiec-Donocik E, Nawrocka L, Pieczara E. Variability of the eyeballs axial length in children with pseudophakia. Klin Oczna. 2006;108(7–9):301–305. | ||
Zhou J, Zhou L, Wu Y, Hu D, Hui Y. Ocular axial length and refractive changes in pediatric pseudophakia. Yan Ke Xue Bao. 2000;16(4):270–275. | ||
Inatomi M, Kora Y, Kinohira Y, Yaguchi S. Long-term follow-up of eye growth in pediatric patients after unilateral cataract surgery with intraocular lens implantation. J AAPOS. 2004;8(1):50–55. | ||
Tartarella MB, Carani JCE, Scarpi MJ. The change in axial length in the pseudophakic eye compared to the unoperated fellow eye in children with bilateral cataracts. J AAPOS. 2014;18(2):173–177. | ||
Hussin HM, Markham R. Changes in axial length growth after congenital cataract surgery and intraocular lens implantation in children younger than 5 years. J Cataract Refract Surg. 2009;35(7):1223–1228. | ||
Lambert SR, Lynn MJ, DuBois LG, et al. Axial elongation following cataract surgery during the first year of life in the infant Aphakia Treatment Study. Invest Ophthalmol Vis Sci. 2012;53(12):7539–7545. | ||
Awner S, Buckley EG, DeVaro JM, Seaber JH. Unilateral pseudophakia in children under 4 years. J Pediatr Ophthalmol Strabismus. 1996;33(4):230–236. | ||
Crouch ER, Crouch ER, Pressman SH. Prospective analysis of pediatric pseudophakia: myopic shift and postoperative outcomes. J AAPOS. 2002;6(5):277–282. | ||
Trivedi RH, Wilson ME. Changes in interocular axial length after pediatric cataract surgery. J AAPOS. 2007;11(3):225–229. | ||
Cassidy L, Rahi J, Nischal K, Russell-Eggitt I, Taylor D. Outcome of lens aspiration and intraocular lens implantation in children aged 5 years and under. Br J Ophthalmol. 2001;85(5):540–542. | ||
Lambert SR, Buckley EG, Plager DA, Medow NB, Wilson ME. Unilateral intraocular lens implantation during the first six months of life. J AAPOS. 1999;3(6):344–349. | ||
Hussain RN, Shahid F, Woodruff G. Axial length in apparently normal pediatric eyes. Eur J Ophthalmol. 2014;24(1):120–123. | ||
Apaza VA, Flores-Boza A, Arakaki MB, Dueñas E, Calisaya PL. Cambios Refractivos en Niños Post-Operados de Catarata Congénita con Implante Primario de Lente Intraocular en Instituto Nacional de Oftalmología, Lima, Perú. Rev Institucional Del INO. 2013;1(3):34–34. Spanish. | ||
Griener ED, Dahan E, Lambert SR. Effect of age at time of cataract surgery on subsequent axial length growth in infant eyes. J Cataract Refract Surg. 1999;25(9):1209–1213. | ||
Hutchinson AK, Wilson ME, Saunders RA. Outcomes and ocular growth rates after intraocular lens implantation in the first 2 years of life. J Cataract Refract Surg. 1998;24(6):846–852. | ||
Hoevenaars NED, Polling JR, Wolfs RCW. Prediction error and myopic shift after intraocular lens implantation in paediatric cataract patients. Br J Ophthalmol. 2011;95(8):1082–1085. | ||
Kora Y, Shimizu K, Inatomi M, Fukado Y, Ozawa T. Eye growth after cataract extraction and intraocular lens implantation in children. Ophthalmic Surg. 1993;24(7):467–475. | ||
Vasavada AR, Raj SM, Nihalani B. Rate of axial growth after congenital cataract surgery. Am J Ophthalmol. 2004;138(6):915–924. | ||
Kim DH, Kim JH, Kim SJ, Yu YS. Long-term results of bilateral congenital cataract treated with early cataract surgery, aphakic glasses and secondary IOL implantation. Acta Ophthalmol. 2012;90(3):231–236. | ||
Nischal KK, Solebo L, Russell-Eggitt I. Paediatric IOL implantation and postoperative refractive state: what role do study methodology and surgical technique play? Br J Ophthalmol. 2010;94(5):529–531. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
