Back to Journals » Patient Preference and Adherence » Volume 17
Relationship Between Medication Literacy and Beliefs Among Persons with Type 2 Diabetes Mellitus in Guangdong, China
Authors Jiang S , Zhu Z , Liao G , Huang Y , Li L , Zeng K
Received 7 May 2023
Accepted for publication 8 August 2023
Published 18 August 2023 Volume 2023:17 Pages 2039—2050
DOI https://doi.org/10.2147/PPA.S420383
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Qizhi (Cathy) Yao
Sifen Jiang,1,* Zhuoqi Zhu,2,* Guisheng Liao,3,* Yanling Huang,1 Lichang Li,4 Kun Zeng1
1School of Nursing, Guangdong Pharmaceutical University, Guangzhou, People’s Republic of China; 2School of Public Health, Guangxi Medical University, Guangxi, People’s Republic of China; 3Emergency Outpatient, Dongguan Eighth People’s Hospital, Dongguan, People’s Republic of China; 4Endocrinology Department, Dongguan Eighth People’s Hospital, Dongguan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kun Zeng, School of Nursing, Guangdong Pharmaceutical University, No. 283, Jianghai Avenue, Haizhu District, Guangzhou City, Guangdong Province, 510310, People’s Republic of China, Tel +86 13790300213, Email [email protected]
Purpose: To establish the relationship between medication literacy and medication beliefs among persons with type 2 diabetes mellitus (T2DM).
Patients and methods: A cross-sectional survey of 246 patients with T2DM was conducted between April and November 2022 at a tertiary hospital in Dongguan City, Guangdong Province, China. Subsequently, these patients were administered the General Information Questionnaire, the Chinese version of Medication Literacy Assessment Scale, and the Chinese version of Beliefs about Medicines Questionnaire-Specific via survey.
Results: The medication literacy score of patients with T2DM was 7.82± 3.007, and the medication beliefs score was 2.26± 4.011. The Pearson correlation analysis revealed a statistically significant but weakly positive correlation (r = 0.271, P < 0.001) between medication literacy and beliefs among patients diagnosed with T2DM. However, there was no significant correlation found between medication literacy and necessity (r = − 0.021, P > 0.05), while a lowly negative correlation was observed between medication literacy and concerns (r = − 0.307, P < 0.001). Moreover, the multiple linear regression analysis indicated that medication literacy, age, education level, and duration of medication usage were all significant factors influencing patients’ medication beliefs (all P < 0.05). Together, these variables accounted for 15.3% of the total variance observed in the regression equation.
Conclusion: The study found a positive correlation between medication literacy and beliefs, and a negative correlation between medication literacy and concerns. These results indicate that enhancing medication literacy can improve medication adherence among individuals with T2DM by reducing concerns and strengthening medication beliefs.
Keywords: type 2 diabetes mellitus, T2DM, medication literacy, medication beliefs, medication adherence, correlation
Introduction
According to the 2021 data from the International Diabetes Federation,1 approximately 537 million adults worldwide suffer from diabetes mellitus. Type 2 Diabetes Mellitus (T2DM) constitutes over 90% of the total diabetes mellitus population, and China has the most significant number of diabetes mellitus patients, with around 116 million cases. Patients with T2DM can suffer from various complications when their blood glucose is poorly controlled. These complications increase the mortality and disability rate and significantly reduce the patient’s quality of life.2 Medication is one of the most critical therapeutic measures for T2DM, and adherence to medication is essential for glycemic control. Good adherence is not only a critical factor in ensuring medication effectiveness but also lowers the risk of diabetic co-morbidities, death rates, and treatment costs.3,4 However, research has found that the medication adherence of T2DM patients in China is not optimistic, with the rate of poor medication adherence ranging from 19.9% to 77.68%.5,6 Poor medication adherence endangers the patient’s health and places a significant financial burden on the healthcare system;7,8 improving patient adherence is critical.
Medication beliefs are an individual’s attitudes toward medication adherence’s benefits and potential harms.9 Beliefs about medication are a modifiable factor that significantly predicts adherence more than other social and clinical factors,10,11 so identifying modifiable beliefs about medication may be an effective way to improve medication adherence. Horne created the Beliefs about Medicines Questionnaire (BMQ) in 1999.9 The BMQ scale is divided into two subscales: Beliefs about Medicines Questionnaire-General (BMQ-G) and Beliefs about Medicines Questionnaire-Specific (BMQ-S). The BMQ-G assesses whether a person believes that taking medication in general is harmful (general harm) and that doctors overuse medication (general overuse). The BMQ-S assesses whether patients believe medications are necessary to maintain their current and future health (necessity) or whether they are concerned about the existing and potentially adverse consequences of medication use (concerns). Both of these subscales can be employed independently or jointly to assess the medication beliefs of patients with chronic ailments, and the BMQ-S has been considered to be a more reliable indicator of adherence than those from the BMQ-G.12 The BMQ scale has been extensively utilized in China, particularly in chronic illnesses like diabetes, stroke, and rheumatoid arthritis. Its reliability and validity have been demonstrated to be satisfactory.13
Medication literacy, the capacity to receive, effectively comprehend, and correctly process critical pharmacological information to make informed decisions,14 can also predict how well patients will take their medications.15 Professor Sauceda and his team at the University of Texas created a single-dimensional Medication Literacy Assessment in English and Spanish (MedLitRxSE).16 The tool above aims to evaluate patients’ medication literacy levels by measuring their ability to read, understand, calculate, and deal with medication-related issues. Zheng has translated and adapted the scale into Chinese and validated it for use in Chinese patients, demonstrating good applicability.17
Current studies on medication literacy and beliefs in China have primarily focused on investigating the current situation and influencing factors.18,19 Some scholars have found that medication literacy among Chinese patients with chronic diseases is intermediate; gender, education level, annual income, disease duration, social support, the number of medications and health problems significantly influence medication literacy.20,21 Jiang conducted a study on 180 elderly patients with T2DM and discovered that the participants’ necessity beliefs were 21.87±2.15, concerns beliefs were 19.78±2.41, and that both could have a significant impact on medication adherence, with concerns beliefs having a more substantial influence.22 According to studies, elements like education level, family income, and disease duration can affect patients’ beliefs about medication.19,23
Medication literacy and beliefs are significant predictors of patient medication adherence. However, few studies have examined the influence of medication literacy on beliefs among T2DM patients or the relationship between the two. Therefore, this study takes medication literacy and beliefs in patients with T2DM as an entry point to explore the current situation and analyze the relationship between them. The study’s findings will serve as a dependable scientific guide for improving medication adherence in T2DM patients.
Materials and Methods
Participants
T2DM patients were chosen for this study from the outpatient and inpatient departments of a tertiary hospital in Dongguan City between April 2022 and November 2022. Eligible patients, either outpatients or inpatients, were selected for the study through convenience sampling. The inclusion criteria were: ① age≥ 18 years; ② patients who met the diagnostic criteria for T2DM according to the World Health Organization (WHO);24 ③ a history of at least three months of diabetes mellitus, excluding newly diagnosed patients; ④ take at least one hypoglycemic agent orally, including using insulin injections; ⑤ sign informed consent and voluntarily participate in this study. The exclusion criteria were: ① the presence of acute and severe diseases; ② the presence of severe mental disorders, intellectual disabilities, or language communication disorders; ③ currently or previously engaged in medical work.
Sample Size Calculation
In estimating the sample size, the primary reference is the sample estimation method of Castro and Kendall, which ensures that the sample size reaches at least 10–15 times the number of variables.25 There were 15 variables in this study; considering the validity of the questionnaire during the survey process, another 10% enlarged the sample size, and 165-248 patients should be collected to meet the needs. A total of 250 questionnaires were distributed in this study since four patients had problematic answers, of which 246 were considered valid, resulting in a valid return rate of 98.4%.
Methods
Two scales and a questionnaire were utilized in the present study. The General Information Questionnaire covered sociodemographic data (such as gender, age, and education level) as well as clinical indicators (such as duration of medication usage, classification of drugs, and the existence of chronic complications of diabetes).
The current study adopted the Chinese version of Medication Literacy Assessment Scale;17 the test-retest reliability of the scale stands at 0.885, while the split-half reliability stands at 0.840. The scale consists of 14 items, with 1 point for each item answered correctly and 0 points for incorrect answers; the maximum score for the scale is 14 points; higher scores indicate superior medication literacy. A score ranging from 0 to 3 is considered low medication literacy; 4 to 10 denotes moderate medication literacy; and a score exceeding 10 points represents high medication literacy. The Cronbach’s alpha coefficient for the scale in this study was 0.691.
Tang and her team translated and revised the BMQ-S, creating the Chinese version of Beliefs about Medicines Questionnaire-Specific.26 The content validity index for each item ranged from 0.857 to 1.000, with an average content validity index of 0.980. This version effectively assesses patients with T2DM and was utilized in the present study. The Chinese version of BMQ-S comprises two dimensions, necessity and concerns, with five items each. The scale uses a 5-point Likert scoring system, ranging from 1 point for “strongly disagree” to 5 points for “strongly agree.” Each dimension has a maximum score of 25 points, indicating an escalation in the patient’s perceived level of necessity or concerns with increasing scores. According to the formula “medication beliefs score = total necessity score minus total concerns score”, a positive score indicates that the advantages or necessity of medication are more significant than any potential drawbacks or concerns. The Cronbach’s alpha coefficient for the scale in this study was 0.733.
Data Collection
The participants were meticulously selected by the specified inclusion and exclusion criteria (consecutive sampling) until the desired sample size was reached. Before distributing the questionnaires, the objectives and significance of the study were clearly explained to the participants. Additionally, the participants were requested to provide their understanding and cooperation by signing the informed consent form. The investigator distributed the questionnaires and provided standardized instructions for their completion. The questionnaires were distributed, collected on-site, and promptly checked by the investigator to address missing responses. This approach led to a high questionnaire recovery rate and increased efficiency.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics 26.0. The mean ± standard deviation was used to express measurement data that followed a normal distribution, while frequency and percentage were used for count data. The study employed an independent sample t-test to compare two groups and utilized one-way ANOVA analysis to compare multiple groups. Pairwise comparisons between groups were performed using the LSD method. Pearson correlation was employed to evaluate the association between medication literacy and beliefs, and multiple linear regression analysis was used to determine the factors influencing medication beliefs. A statistically significant difference was considered as P < 0.05. Additionally, Cronbach’s alpha coefficient was used to determine the internal consistency and reliability of the Chinese version of BMQ-S and MedLitRxSE.27
Results
Patient Characteristics
Of the 246 patients with T2DM, 125 were male, 51.2% of individuals were over 60 years old, the average education level was junior high school or below (71.1%), the majority of occupations were inactive (jobless or retired) (65.9%), 30.9% had been taking their medications for more than ten years, and 37.4% had taken at least three different medications. Table 1 contains the remaining characteristics.
 |
Table 1 Distribution of Patients According to Sociodemographic and Clinical Characteristics (N=246) |
Medication Literacy and Beliefs Scores of T2DM Patients
Among 246 patients with T2DM, the mean medication literacy score was 7.82±3.007. Specifically, 8.9% of the patients had low medication literacy, 72.4% demonstrated moderate medication literacy, and 18.7% exhibited high medication literacy. The medication beliefs score of T2DM patients was 2.26±4.011, with a total score of necessity being 18.30±2.958 and a total score of concerns being 16.04±3.747. The patient necessity scores exceeded the concerns scores, indicating a positive attitude towards medication adherence. Participants perceived the benefits of complying with the prescribed medication regimen to outweigh the potential harm.
Univariate Analysis of Medication Beliefs in Patients with T2DM
As indicated in Table 2, the findings of the univariate analysis revealed that age, education level, duration of medication usage, and the existence of chronic complications of diabetes were statistically significant in the outcomes of medication beliefs. The study results indicated that higher medication beliefs scores were associated with older age, higher educational levels, longer medication usage duration, and the presence of chronic complications in patients.
 |
Table 2 Univariate Analysis of Medication Beliefs in Patients with T2DM (N=246) Unit: Score |
Correlation Analysis of Medication Literacy and Beliefs in T2DM Patients
Based on the findings of this study (Table 3), among T2DM patients, a statistically significant but weakly positive correlation was observed between medication literacy and beliefs scores (r = 0.271, P < 0.001). However, there was no significant correlation between medication literacy scores and necessity (r = −0.021, P > 0.05). On the other hand, a lowly negative correlation was observed between medication literacy and concerns (r = −0.307, P < 0.001).
 |
Table 3 Correlation Analysis of Medication Literacy and Beliefs |
Analysis of Factors Influencing Medication Beliefs in Patients with T2DM
The independent variables considered for multiple linear regression analysis were age, education level, duration of medication usage, presence of chronic complications of diabetes, and medication literacy scores; the medication beliefs scores served as the dependent variable. The factors assigned in the multiple linear regression model were as follows: age: <60 years = 1, ≥60 years = 2; education level: junior high school and below = 1, high school/special secondary/technical school = 2, college and above = 3; duration of medication usage: <5 years = 1, 5–10 years = 2, >10 years = 3; chronic complications of diabetes: no = 1, yes = 2; the medication literacy was substituted into the original values.
The multicollinearity test in this study showed that all VIFs were less than 5, considering there was no multicollinearity between the independent variables. The findings revealed that age, education level, duration of medication usage, and medication literacy accounted for 15.3% of the variance in medication beliefs within this population (Table 4). A high score of medication belief significantly was correlated with older age, a high level of education, a longer duration of medication usage, and higher medication literacy. Furthermore, the results of the multiple linear regression analysis for necessity and concerns in T2DM patients revealed that age significantly influenced necessity (β= 0.163, P < 0.05), while concerns was affected by education level (β= −0.150, P < 0.05).
 |
Table 4 Multiple Linear Regression Analysis of Factors Influencing Medication Beliefs in Patients with T2DM (N=246) |
Discussion
Current Status of Medication Literacy in Patients with T2DM
The mean medication literacy score for 246 patients was 7.82±3.007, indicating an intermediate level of their ability to comprehend drug-related knowledge and make informed medication decisions. Among the participants, 8.9% had low medication literacy, 72.4% showed moderate medication literacy, and 18.7% exhibited high medication literacy. In contrast, Liu found that patients with T2DM had a medication literacy score of 9.44±3.28, with 95.0% of the participants demonstrating a moderate or adequate level of medication literacy, significantly surpassing the results of the present study.28 This discrepancy could be attributed to the higher proportion of older and less educated participants in our study. The higher medication literacy scores in this study, compared to Qiao’s study on patients with coronary artery disease, may be attributed to variations in medication literacy influenced by the study population, diseases, and commonly used medications.20
Medication literacy is an essential consideration in the development, implementation, and evaluation of medication adherence interventions. Jiang conducted an analysis of the correlation between medication literacy and treatment adherence in diabetic patients, revealing a positive association.29 This suggests that improving medication literacy in diabetic patients can enhance treatment adherence. Zhang’s research revealed a positive correlation between medication literacy and quality of life among hypertensive patients.30 Higher levels of medication literacy promote doctor-patient communication, increase understanding of the disease and medication, enhance medication adherence and safety, and improve self-management skills, ultimately leading to an enhanced quality of life.30,31
A systematic review has identified patients’ age and education levels as the most common demographic factors influencing medication literacy.32 As age increases, elderly patients’ comprehension, attention, and memory decline to varying degrees, coupled with a greater number of prescribed medications and complex medication regimens, leading to their limited knowledge about medication management.33 People with low levels of education have difficulty understanding treatment regimens during the diagnosis and treatment of disease, do not understand the proper use of medications, and are more inclined to have lower levels of medication literacy.33 Additionally, inadequate provision of comprehensive information about relevant medications by healthcare professionals and the inability of patients to accurately comprehend and disregard information about medications are vital factors contributing to low medication literacy.34 Patients with lower medication literacy demonstrate inadequate self-administration behavior in medication therapy, including medication errors, self-medication abuse, and overdose use.32 These behaviors diminish the effectiveness of medications, raise the risk of adverse drug reactions, and ultimately jeopardize the patient’s health.35 Interventions to improve patient medication literacy are critical to ensure medication safety. Li conducted a 12-week interactive medication literacy intervention for coronary artery disease patients; significant improvements were observed in patients’ medication skills, literacy, self-efficacy, and medication safety behaviors as a result of the intervention.36
Current Status of Medication Beliefs and Their Influencing Factors in Patients with T2DM
The Necessity-Concerns Framework (NCF), derived from the Health Belief Model, has demonstrated utility in elucidating the rationales behind individual nonadherence to medication.10 This model posits that an individual’s adherence to medication is contingent upon a balance between the imperative for medication to ameliorate health and concerns regarding potential adverse effects of medication. Necessity beliefs are considered to positively influence individuals’ medication adherence, while concerns beliefs are believed to negatively impact individuals’ adherence to medication.
The current study observed patients exhibit a medication beliefs score of 2.26±4.011, which exceeded the outcomes of the research by Pan.37 This disparity may be attributed to the fact that the population in the latter research comprised individuals with chronic co-morbidities who suffered from multiple chronic diseases and had relatively intricate medication regimens, posing greater challenges during the medication process. Consequently, their concerns surpassed necessity, while their medication beliefs were more vulnerable to compromise. In this study, the patients exhibited lower medication beliefs scores than those observed in the study of Parkinson’s disease (PD) patients.38 The difference could be explained by the fact that PD is a chronic, progressive, and incurable neurodegenerative condition requiring heavy reliance on medications to manage symptoms, unlike diabetes, which can be controlled with diet and exercise in its early stages. Consequently, individuals with PD tend to hold stronger beliefs about medication usage. A comprehensive meta-analysis of 96 peer-reviewed studies, encompassing over 24,000 patients from 18 countries with 24 long-term conditions, revealed a significant association between non-adherence to medication and patients’ beliefs about medicines.39 Further research indicated that excellent medication adherence is positively associated with stronger necessity and weaker concerns.40 Wu’s study showed that increased general harm beliefs directly reduce medication adherence and also have an indirect effect on adherence through self-efficacy.41 Additionally, Horne proved that significant concerns beliefs were linked to worsening disease activity, clinical status, and poor quality of life in rheumatoid arthritis patients.42
The results of the present study evinced that patients’ total score of medication beliefs and necessity increased with age, which is congruent with the findings of Brazilian scholars.7 This may be attributed to increased demand for hypoglycemic drugs as patients age, given that they experience difficulty controlling their blood glucose levels via diet and exercise. Furthermore, education level was also found to be one of the determinants of patients’ medication beliefs, as lower education levels were associated with a weaker capacity to acquire medication knowledge and a lack of accurate information regarding medications, ultimately leading to heightened medication apprehension and negative medication beliefs.23 Additionally, patients with a longer duration of medication usage exhibited higher medication beliefs scores, possibly because such patients had more time and opportunities to receive education about the disease and medication from healthcare professionals throughout long-term medication usage, culminating in a correct apprehension of the significance of hypoglycemic drugs for current and future health. Besides the factors examined in this study, Horne’s research revealed that environmental factors, such as the presence of social support and the quality of communication with healthcare providers, had an impact on perceptual factors (beliefs).43 Consequently, favorable environmental factors are conducive to patients developing positive beliefs about medication use.
Italian researchers have classified patients into four distinct subgroups, taking into account their attitudes towards the necessity and concerns associated with medication use: Skeptical (low necessity and high concerns), Ambivalent (high necessity and high concerns), Indifferent (low necessity and low concerns), and Accepting (high necessity and low concerns). They also found that individuals in the Accepting group exhibited the highest adherence to medication, whereas those in the Skeptical group demonstrated the lowest adherence.44 In this study, a score of 15 on the subscale was used as the threshold for categorizing necessity or concerns as high or low, and patients were also categorized into four groups: Skeptical (3.7%), Ambivalent (62.6%), Indifferent (7.7%), and Accepting (26.0%) (Figure 1). The percentage of participants in the high necessity and high concerns (Ambivalent) group was higher in this study compared to the study by Khdour.45 This discrepancy could be attributed to the older age and generally low educational level of the subjects in this study, which led to a greater perceived necessity and concerns about medication use. The study findings indicate that patients generally held positive attitudes towards the necessity of medication use. However, they also expressed concerns about the potential adverse effects of hypoglycemic drugs and the impact of medication adherence on their daily lives. Evidence suggested that participants in the Ambivalent group were more receptive to behavioral change, indicating that the chances of successful intervention implementation may increase with positive attitude changes.46 Therefore, it is crucial to proactively identify factors influencing concerns beliefs and implement targeted interventions. These interventions may include improving patient medication instruction, emphasizing medication importance, and correcting adverse perceptions to reduce concerns and enhance medication adherence.
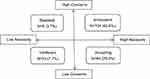 |
Figure 1 Distribution of the beliefs and attitudes of patients toward medication. |
Medication Literacy Affects Beliefs of T2DM Patients
The correlation analysis for this study showed that medication literacy was not substantially connected with necessity in individuals with T2DM; however, it was negatively connected with concerns and positively associated with medication beliefs. Regression analysis revealed that medication literacy significantly influences patients’ medication beliefs (β = 0.285, P < 0.001). Therefore, the study revealed that medication literacy primarily influenced patients’ concerns and subsequent medication beliefs, aligning with previous findings by Visscher and Kale,47,48 who identified a correlation between low levels of health literacy and heightened medication concerns. Patients with low medication literacy lack the knowledge and access necessary to understand medication principles, resulting in high concerns and a limited understanding of medication-related information. As medication concerns can affect patients’ decisions regarding self-management and health promotion, special attention should be given to patients with low medication literacy.
The Knowledge-Attitude-Behavior Model (KAB Model) suggests that accumulating health-related knowledge can lead to changes in health-related beliefs, which can influence health behaviors.49 Medication literacy is necessary for patients to properly understand their medications and treatments, and when patients have the correct knowledge of their medications and treatments, they influence their medication beliefs and treatment decisions.
According to the Hierarchical Model of Medication Adherence (HMMA), medication adherence follows a five-level model. The first four tiers encompass health literacy, illness beliefs, medication beliefs, and self-efficacy, with medication adherence as the ideal behavior at the top of the model.50 The model suggests that individuals should have sufficient health literacy before their beliefs are influenced, and only when the first three tiers reach a certain level will patient self-efficacy play the greatest role in medication adherence. Good health literacy is essential for patients’ medication adherence, and medication literacy is an important aspect of health literacy in the pharmacy field. In conclusion, medication literacy plays a pivotal role in shaping patients’ medication beliefs and, consequently, their medication adherence, thereby directly impacting the effectiveness of diabetes management.
Limitations
Moreover, there are certain limitations to this study. Initially, the study population’s scope is limited, limiting the study’s conclusion. Secondly, this cross-sectional study can merely analyze the factors related to medication beliefs but not the causal relationship. Finally, factors such as medication literacy, age, education level, and duration of medication use account for only 15.3% of the total variability. The remaining variability may be attributed to other factors not included in the analysis. In future research, it is important to explore additional factors that may influence patients’ medication beliefs in order to fully explain the variations observed. Additionally, conducting longitudinal studies can help investigate whether there is a causal relationship between medication literacy and beliefs.
Conclusion
This study revealed a positive correlation between medication literacy and medication beliefs, a negative correlation with concerns, and no correlation with necessity. Participants generally exhibited moderate medication literacy but also expressed ambivalence in their beliefs. Additionally, those with low literacy levels tended to have higher concerns scores. These findings underscore the significance of integrating medication literacy into patient education and intervention strategies. Enhancing medication literacy can positively impact medication beliefs, alleviate concerns, and ultimately improve medication adherence and health outcomes.
Abbreviations
T2DM, Type 2 Diabetes Mellitus; WHO, World Health Organization; MedLitRxSE, Medication Literacy Assessment in English and Spanish; BMQ-G, Beliefs about Medicines Questionnaire-General; BMQ-S, Beliefs about Medicines Questionnaire-Specific; NCF, The Necessity-Concerns Framework; KAB Model, The Knowledge-Attitude-Behavior Model; HMMA, The Hierarchical Model of Medication Adherence.
Ethics Approval
This study was conducted under the Declaration of Helsinki. The Dongguan Eighth People’s Hospital Ethics Committee reviewed and approved this study (approval number: LL2022053001). Following a concise overview of the study’s background, purpose, investigation, as well as associated risks and benefits, participants willingly provided their informed consent. Throughout the research, strict confidentiality measures were implemented to safeguard all patient-related information.
Acknowledgments
Grateful acknowledgments are extended to the investigators and patients of Dongguan Eighth People’s Hospital.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sun H, Saeedi P, Karuranga S, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. doi:10.1016/j.diabres.2021.109119
2. Lin X, Xu Y, Pan X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):14790. doi:10.1038/s41598-020-71908-9
3. Al-ruthia YS, Hong SH, Graff C, et al. Examining the relationship between antihypertensive medication satisfaction and adherence in older patient. Res Social Adm Pharm. 2017;13(3):602–613. doi:10.1016/j.sapharm.2016.06.013
4. Kennedy-martin T, Boye KS, Peng X. Cost of medication adherence and persistence in type 2 diabetes mellitus: a literature review. Patient Prefer Adherence. 2017;11:1103–1117. doi:10.2147/PPA.S136639
5. Xu N, Xie S, Chen Y, et al. Factors influencing medication non-adherence among Chinese older adults with diabetes mellitus. Int J Environ Res Public Health. 2020;17(17). doi:10.3390/ijerph17176012
6. Zhang Y, Han X, Lin JY. Compliance of blood glucose control and drug compliance in elderly patients with type 2 diabetes mellitus. South China J Prev Med. 2021;47(06):727–730.
7. Saraiva EMS, Coelho JLG, Dos Santos Figueiredo FW, et al. Medication non-adherence in patients with type 2 diabetes mellitus with full access to medicines. J Diabetes Metab Disord. 2020;19(2):1105–1113. doi:10.1007/s40200-020-00612-2
8. Cutler RL, Fernandez-Llimos F, Frommer M, et al. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8(1):e016982. doi:10.1136/bmjopen-2017-016982
9. Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. doi:10.1080/08870449908407311
10. Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. doi:10.1016/S0022-3999(99)00057-4
11. Emilsson M, Gustafsson PA, Öhnström G, et al. Beliefs regarding medication and side effects influence treatment adherence in adolescents with attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry. 2017;26(5):559–571. doi:10.1007/s00787-016-0919-1
12. Unni E, Shiyanbola OO, Farris KB. Change in medication adherence and beliefs in medicines over time in older adults. Glob J Health Sci. 2015;8(5):39–47. doi:10.5539/gjhs.v8n5p39
13. Wei L, Champman S, Li X, et al. Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: a cross-sectional study in China. BMJ Open. 2017;7(10):e17293. doi:10.1136/bmjopen-2017-017293
14. Pouliot A, Vaillancourt R, Stacey D, et al. Defining and identifying concepts of medication literacy: an international perspective. Res Social Adm Pharm. 2018;14(9):797–804. doi:10.1016/j.sapharm.2017.11.005
15. Zheng F, Ding S, Lai L, et al. Relationship between medication literacy and medication adherence in inpatients with coronary heart disease in Changsha, China. Front Pharmacol. 2020;10:1537. doi:10.3389/fphar.2019.01537
16. Sauceda JA, Loya AM, Sias JJ, et al. Medication literacy in Spanish and English: psychometric evaluation of a new assessment tool. Journal of the American Pharmacists Association. 2012;52(6):e231–e240. doi:10.1331/JAPhA.2012.11264
17. Zheng F, Zhong ZQ, Ding SQ, et al. Modification and evaluation of assessment of medication literacy. J Cent South Univ. 2016;41(11):1226–1231. doi:10.11817/j.issn.1672-7347.2016.11.019
18. Cui YP, Lou PY, Xu XL, et al. Studying on the status of medication literacy of the elderly and its influencing factors-sampled with Shandong Province. Chin Health Ser Manag. 2021;38(6):477–480.
19. Zhang C. Analysis of the current status of medication beliefs and influencing factors in patients with type 2 diabetes. Chin Gen Pract Nurs. 2022;20(4):557–559. doi:10.12104/j.issn.1674-4748.2022.04.033
20. Qiao L, Ding S, Zhong Z, et al. Association between social support and medication literacy in Chinese patients with coronary heart disease. Front Cardiovasc Med. 2021;8:705783. doi:10.3389/fcvm.2021.705783
21. Chang X, Wang K, Wang Y, et al. Medication literacy in Chinese patients with stroke and associated factors: a cross-sectional study. Int J Environ Res Public Health. 2022;20(1). doi:10.3390/ijerph20010620
22. Jiang XW. The Relationship Between Health Literacy and Medication Adherence Among Older Patients with Type 2 Diabetes Mellitus: Medication Beliefs Acting as Mediators. Shandong university; 2021.
23. Wang ZJ, Zhou YQ, Sun YJ, et al. Belief about medication in schizophrenia patients and lts influencing factors. Chin Gen Pract. 2018;21(11):1330–1335.
24. Alberti KGMM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–553. doi:10.1002/(sici)1096-9136(199807)15:7<539::aid-dia668>3.0.co;2-s
25. Castro AL, Kendall MC. Sample size and the establishment of safety in perioperative medicine. Actas Urol Esp. 2018;42(9):610. doi:10.1016/j.acuro.2018.05.007
26. Tang J, Gao LL, Hu XL, et al. The reliability and validity of the Chinese version of beliefs about medicines questionnaire-specific among patients with type 2 diabetes mellitus. J Nurs Sci. 2019;34(21):25–28. doi:10.3870/j.issn.1001-4152.2019.21.025
27. Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi:10.1016/j.jclinepi.2006.03.012
28. Liu H, Yao Z, Shi S, et al. The mediating effect of self-efficacy on the relationship between medication literacy and medication adherence among patients with type 2 diabetes. Patient Prefer Adherence. 2023;17:1657–1670. doi:10.2147/PPA.S413385
29. Jiang M. Study About the Correlation Between Drug Literacy, Internal Strength and Treatment Compliance in Brittle Diabetic Patients. Yanbian University; 2020.
30. Zhang KX, Lin Q, Liao XT, et al. Correlation between medication literacy, medication compliance and quality of life in elderly hypertensive patients in community. Occup Health. 2021;37(18):2546–2551.
31. Chang FC, Chi HY, Huang LJ, et al. Developing school-pharmacist partnerships to enhance correct medication use and pain medication literacy in Taiwan. J Am Pharm Assoc. 2015;55(6):595–602. doi:10.1331/JAPhA.2015.15053
32. Pantuzza LLN, Nascimento E, Botelho SF, et al. Mapping the construct and measurement of medication literacy: a scoping review. Br J Clin Pharmacol. 2020;87(3):754–775. doi:10.1111/bcp.14490
33. Plaza-Zamora J, Legaz I, Osuna E, et al. Age and education as factors associated with medication literacy: a community pharmacy perspective. BMC Geriatr. 2020;20(1):501. doi:10.1186/s12877-020-01881-5
34. Sun WC. A Study on the Status of Stakeholders’ Perception of Medication Safety Risk Communication. Beijing University of Chinese Medicine; 2013.
35. Custodis F, Rohlehr F, Wachter A, et al. Medication knowledge of patients hospitalized for heart failure at admission and after discharge. Patient Prefer Adherence. 2016;10:2333–2339. doi:10.2147/PPA.S113912
36. Li N. The Influence of Interactive Medication literacy Intervention on Medication Safety in Patients with Coronary Heart Disease. University Of South China; 2021.
37. Pan WY, Zhang CH, Zhang ZX, et al. Analysis of drug self-management level and influencing factors in hospitalized middle-aged and elderly patients with chronic comorbidities. Chin Nurs Res. 2022;36(19):3534–3539.
38. Kim SR, Kim JY, Kim HY, et al. Factors associated with medication beliefs in patients with Parkinson’s disease: a cross-sectional study. J Mov Disord. 2021;14(2):133–143. doi:10.14802/jmd.20147
39. Horne R, Chapman SC, Parham R, et al. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PLoS One. 2013;8(12):e80633. doi:10.1371/journa-l.pone.0080633
40. Sweileh WM, Zyoud SH, Abu NR, et al. Influence of patients’ disease knowledge and beliefs about medicines on medication adherence: findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health. 2014;14:94. doi:10.1186/1471-2458-14-94
41. Wu J, Shen J, Tao Z, et al. Self-efficacy as moderator and mediator between medication beliefs and adherence in elderly patients with type 2 diabetes. Patient Prefer Adherence. 2023;17:217–226. doi:10.2147/PPA.S382362
42. Horne R, Albert A, Boone C.Relationship between beliefs about medicines, adherence to treatment, and disease activity in patients with rheumatoid arthritis under subcutane-ous anti-TNFαtherapy. Patient Prefer Adherence. 2018;12:1099–1111. doi:10.2147/PPA.S166451
43. Horne R, Cooper V, Wileman V, et al. Supporting adherence to medicines for long-term conditions: a perceptions and practicalities approach based on an extended common-sense model. Eur Psychol. 2019;24:82–96.
44. Tibaldi G, Clatworthy J, Torchio E, et al. The utility of the necessity—concerns framework in explaining treatment non-adherence in four chronic illness groups in Italy. Chronic Illn. 2009;5(2):129–133. doi:10.1177/1742395309102888
45. Khdour MR, Awadallah HB, Alnadi MA, et al. Beliefs about medicine and glycemic control among type 2 diabetes patients: a cross-sectional study in West Bank, Palestine. J Prim Care Community Health. 2020;11:921849713. doi:10.1177/2150132720971919
46. Wan B, Cheung W, Ball PA, et al. Beliefs about medicines among Hong Kong hospital outpatients. Int J Pharm Pract. 2017;25(6):447–453. doi:10.1111/ijpp.12353
47. Visscher BB, Steunenberg B, Zwikker H, et al. The impact of health literacy on beliefs about medication in a Dutch medication-using population. Eur J Clin Pharmacol. 2021;77(8):1219–1224. doi:10.1007/s00228-021-03105-0
48. Kale MS, Federman AD, Krauskopf K, et al. The association of health literacy with illness and medication beliefs among patients with chronic obstructive pulmonary disease. PLoS One. 2015;10(4):e123937. doi:10.1371/journal.pone.0123937
49. Han HR, Kim KB, Kang J, et al. Knowledge, beliefs, and behaviors about hypertension control among middle-aged Korean Americans with hypertension. J Community Health. 2007;32(5):324–342. doi:10.1007/s10900-007-9051-y
50. Unni E, Bae S. Exploring a new theoretical model to explain the behavior of medication adherence. Pharmacy. 2022;10(2):43. doi:10.3390/pharmacy10020043
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
