Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 13
Relationship Between Maternal Dental Anxiety and Children’s Dental Caries in the Eastern Province of Saudi Arabia
Authors Alhareky M, Nazir MA , AlGhamdi L, Alkadi M, AlBeajan N, AlHossan M, AlHumaid J
Received 7 March 2021
Accepted for publication 1 May 2021
Published 18 May 2021 Volume 2021:13 Pages 187—194
DOI https://doi.org/10.2147/CCIDE.S310026
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Christopher E. Okunseri
Muhanad Alhareky,1 Muhammad Ashraf Nazir,1 Lamia AlGhamdi,2 Mariam Alkadi,2 Noura AlBeajan,2 May AlHossan,2 Jehan AlHumaid1
1Department of Preventive Dental Sciences, College of Dentistry, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 2College of Dentistry, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
Correspondence: Muhammad Ashraf Nazir
Department of Preventive Dental Sciences, College of Dentistry, Imam Abdulrahman Bin Faisal University, P. O. Box 1982, Dammam, 31441, Saudi Arabia
Tel +966-38574928
Email [email protected]
Purpose: Dental anxiety is a barrier to dental care utilization and is associated with poor oral health outcomes. The aim of the study was to assess the relationship between dental anxiety of mothers and dental caries of their children in the Eastern Province, Saudi Arabia.
Methodology: A cross-sectional study was conducted on a sample of mother–child pairs (N= 199) in Dammam, AlKhobar, and Dhahran, Saudi Arabia. Dental caries experience among children was determined using dmft/DMFT indexes following the World Health Organization’s guidelines. Maternal dental anxiety was assessed by using the Modified Dental Anxiety Scale (MDAS).
Results: The mean ages of mothers and children were 33.98 ± 5.41 and 6.74 ± 2.29 years, respectively. The mean dmft score was 4.3 ± 3.99 in primary dentition and the mean maternal dental anxiety score was 13.89 ± 5.33. Ninety-two percent of mothers had low to extreme dental anxiety and only 8% reported no dental anxiety. Dental caries experience in primary teeth was higher in children of dentally anxious mothers (mean dmft 4.45 ± 3.92) than the children of mothers who were non-anxious (mean dmft 2.56 ± 4.59) (P=0.07). The mean maternal anxiety score was significantly higher in children with untreated decay in primary dentition (14.49 ± 5.08) than those with sound primary dentition (12.24 ± 5.67) (P = 0.008). The study also found a statistically significant correlation between maternal dental anxiety and untreated decay in the primary dentition (Pearson’s r =0.171, P = 0.015).
Conclusion: Dental anxiety was highly prevalent among mothers in the present study. There was a significant relationship between maternal dental anxiety and untreated decay in the primary dentition. Awareness should be raised among dentally anxious mothers to reduce the burden of dental caries in their children.
Keywords: caries, dental fear, access to oral care, children
Introduction
Dental anxiety is a common problem and it takes fourth place among common fears.1 According to international and local literature, the prevalence of higher levels of dental anxiety ranges from 11.6% % to 19.1% in adults.2–4 Dental anxiety is a barrier to dental treatment utilization as patients avoid visiting dental offices unless they suffer from severe pain.1,5 Globally, high dental anxiety and dental phobia result in 6–15% of the adult population avoiding dental care.6 A recent study in Saudi Arabia reported dental phobia in 16.1% of pregnant women which was related to reduced regular dental check-ups.7 Dental anxiety is a major challenge in pediatric dental practice which affects almost 10–43% of children.8,9 There is also evidence about a significant and negative correlation between dental anxiety and oral health related quality of life among children.10 Uncooperative behavior of children during dental treatment is related to the severity of anxiety, psychological functioning, and experience of last dental attendance.11,12 The children in Saudi Arabia suffer from an increased burden of dental caries with prevalence estimates of 80% for primary teeth and 70% for permanent teeth thus requiring preventive and restorative dental care.13
Parents’ dental anxiety was found to influence children’s dental anxiety14,15 and more female than male children demonstrated dental fear.16 In addition, studies have investigated an association between the parental/maternal dental anxiety and dental caries in children in different parts of the world.1,14,17 It was reported that parents with lower dental anxiety had children without fillings in primary or permanent teeth than the parents of children who had fillings.18 A previous study demonstrated an association between maternal dental anxiety and untreated caries in children.19 In a recent study, a statistically significant correlation was found between parental anxiety and active caries in children.20 Literature also indicates that maternal dental anxiety and caries experience in children significantly affect child’s oral health-related quality of life.21
There is a high prevalence of dental anxiety in adults and dental caries in children in Saudi Arabia. However, studies are scant in the Saudi population about maternal dental anxiety and its association with dental caries in children. Hence, we hypothesized that maternal dental anxiety could inversely affect the caries status of children. Addressing the factors that influence children’s oral health is helpful in order to provide them with good oral health and better quality of life with public health actions focused on the behaviors of parents and children. Therefore, the study findings may guide policy and preventive measures to reduce maternal dental anxiety and improve children’s oral health. The study aimed to assess the relationship between the dental anxiety of mothers and the dental caries of their children in the Eastern Province, Saudi Arabia. The study also evaluated the factors related to children’s caries experience.
Materials and Methods
Ethical Considerations
This study (IRB-2019-02-139) was approved by the Human Research Ethics Committee of the Imam Abdulrahman Bin Faisal University (IAU), Dammam, Saudi Arabia. The consent was obtained from mothers to agree on voluntary participation in the study. It contained information regarding the objectives, procedure, and potential benefits of the study. The mothers were ensured that refusal to participate in the study would have no negative impact on the services provided to their children in the clinic and the confidentiality of their information.
Study Design and Participants
A cross-sectional study was conducted on a convenience sample of male and female children (3–12 years old) and their mothers. In order to determine the sample size needed for this study, a 95% confidence level with a 5% margin of error was applied in the population (N ≈ 2,000, response distribution 85%) surrounding the area served by the Family and Community Medicine Clinics (FAMCO) at the IAU. This suggested a sample size of 200 child and mother pairs required for the study which is similar to the sample sizes used in previous studies.17,20,22 The children with the written consent form of their parents/legal guardians were included in the study. The assent of children was obtained before performing their clinical oral examination. The study complied with the ethical guidelines of the Helsinki Declaration. The children were excluded from this study if they had a systemic disease or received dental treatment in the last 3 months.
Clinical Examination and Measuring Instrument
Clinical oral examination of children and the administration of questionnaires among mothers took place at FAMCO clinics. Dental caries at the level of cavitation was assessed using the World Health Organization (WHO) criteria. Children’s caries experience was calculated using the decayed, missing, and filled teeth (dmft/DMFT) index.23 Two calibrated examiners performed dental caries assessment (Kappa > 0.70).
Participating mother responded to interview questionnaire related to demographic information and dental visits. They also provided their responses to the items of the Modified Dental Anxiety Scale (MDAS) which was used to measure their dental anxiety. The MDAS consists of five items related to dental anxiety when planning to visit the dentist the next day, sitting in the waiting area, having scaling and polishing, drilling of a tooth, and having a local anesthetic injection. Dental researchers and clinicians frequently use MDAS because it is a brief and quick instrument and does not cause anxiety in patients. A 5 point Likert scale is used for each item which ranges from not anxious=1 to extremely anxious=5. The responses of each participant for 5 items are summed to calculate the total score of MDAS which ranges from 5 to 25.24,25 The participants with MDAS score of 5 are categorized as not having dental anxiety, 6–10 low anxiety, 11–14 moderate anxiety, 15–18 high anxiety, and ≥19 extreme anxiety.26 The psychometric properties of the MDAS were evaluated in populations from Ireland, Finland, and the United Arab Emirates and the scale had high internal consistency and good construct validity.21 In Saudi Arabia, Bahammam and Hassan, also confirmed excellent internal consistency and criterion validity of the Arabic version of the MDAS.22 Mothers responded to the Arabic version of MDAS. Pre-testing of the questionnaire was done before its final administration among participating mothers.
Study Variables
Maternal anxiety, untreated decay, and caries experience were important variables in the study. Other variables included parental education, type of residence, insurance, pain on eating in the last 6 months, and visit to the dentist. Based on the median of dmft score, low (dmft = 0–4) and high caries experience (dmft = 5–20) categories of children were created, and maternal dental anxiety score was compared in these categories to evaluate the relationship between maternal dental anxiety and caries experience in primary dentition. Similarly, two categories of mothers not having anxiety (5) versus having anxiety (6–25) based on the MDAS score were created and the means of dmft/DMFT scores were compared to measure the relationship between maternal dental anxiety and caries experience of children.
Statistical Methods
Data were entered in MS Excel (2010) and analyzed by Statistical Package for Social Sciences (SPSS) for Windows, version 22 (IBM Corp., Armonk, N.Y., USA). The means and standard deviations of DMFT/dmft index, age, and MDAS scores were calculated. Frequencies and proportions were calculated for categorical variables such as parental education, type of residence, dental visits, etc. Independent samples t-test was used to compare mean dmft scores in two categories of participants. The evaluation of the relationship between maternal dental anxiety and untreated decay in children was conducted using an independent samples t-test. A one-way ANOVA test was performed to assess mean differences in dmft scores in different categories of the participants according to parental education. The correlations between age and dmft/DMFT scores and between MDAS score and dmft score were calculated using Pearson’s correlation test. A p-value ˂0.05 was used for statistical testing.
Results
The study included data of 199 children and their mothers with mean ages of 6.74 ± 2.29 and 33.98 ± 5.42 years, respectively. Most parents had a college/university level of education. Dental insurance was reported by 45.7% of the mothers. Half the children (51.3%) had pain on eating in the last 6 months and 38.7% visited a dentist. Most children (73.4%) demonstrated untreated decay in primary dentition and 26.6% of children had sound primary dentition. Whereas 17.1% had untreated decay in the permanent dentition. The mean dmft score was 4.3 ± 3.99 in primary teeth while the mean DMFT score was 0.43 ± 1.08 in permanent teeth. The mean dental anxiety score of mothers was 13.89 ± 5.33 (Table 1).
 |
Table 1 Distribution of Study Variables Among Study Participants |
Dental caries experience in the primary dentition was significantly related to mothers’ education (P= 0.005) demonstrating low dmft score related to high education. Children living in their own houses showed greater caries experience in the primary dentition (dmft= 4.95 ± 4.67) than those who lived in rented houses (dmft= 3.73 ± 3.21) (P= 0.033). Dental caries experience in primary dentition was significantly lower in children with dental insurance (dmft= 3.54 ± 3.70) than those without insurance (dmft= 4.94 ± 4.14) (P= 0.013). The mean dmft score was significantly higher in children with pain on eating in the last 6 months (5.88 ± 4.10) than those without pain (2.64 ± 3.14) (P < 0.001). The children who visited a dentist demonstrated a lower mean dmft score (3.61± 3.63) than those who did not attend a dentist (4.74 ± 4.17) (P = 0.053) (Table 2). The study also found statistically significant positive correlation between age and dmft (Pearson’s r = 0.161, P = 0.023) and DMFT (Pearson’s r = 0.474, P < 0.001) among children.
 |
Table 2 Relationship Between Study Variables and Caries Experience (dmft) in Children |
Figure 1 shows the mean score of each item of the MDAS scale among mothers in the study. Anxiety due to local anesthetic injection had the highest mean score (3.35), and it was followed by anxiety due to tooth drilling (3.18). The lowest dental anxiety was reported for scaling and polishing and dental treatment the next day (2.42). Figure 2 shows the distribution of dental anxiety levels among mothers. Dental anxiety was observed in 92% of mothers with 26.6% showing low anxiety, 16.10% moderate anxiety, 27.6% high anxiety, and 21.60% extreme anxiety. Only 8% of mothers demonstrated no dental anxiety.
 |
Figure 1 Mean score of items of MDAS questionnaire among participating mothers. |
 |
Figure 2 Distribution of dental anxiety levels among participating mothers. |
Caries experience in primary teeth was higher in children of dentally anxious mothers (mean dmft 4.45 ± 3.92) than the children of mothers who were non-anxious (mean dmft 2.56 ± 4.59) (P = 0.07). Similarly, the mean DMFT score was higher in children of dentally anxious mothers than the children of non-anxious mothers (P = 0.826) (Table 3).
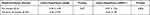 |
Table 3 Relationship Between Maternal Dental Anxiety and Children’s Caries Experience |
It was found that maternal dental anxiety was significantly lower among children with low caries experience (MDAS =13.21± 5.38) than children with high caries experience (MDAS =14.76 ± 5.16) (P = 0.04) (Figure 3).
 |
Figure 3 Relationship between maternal dental anxiety and caries experience in children. |
In Table 3, the mean maternal anxiety score was compared between children who had untreated decay versus who had sound primary and permanent dentitions. The mean maternal dental anxiety score was significantly higher in children with untreated decay in primary dentition (14.49 ± 5.08) than those with sound primary dentition (12.24 ± 5.67) (P = 0.008). However, maternal dental anxiety scores did not differ in children with and without untreated decay in permanent dentition (P = 0.714) (Table 4). Moreover, the study found a statistically significant correlation between maternal dental anxiety and untreated decay in the primary dentition (Pearson’s correlation coefficient = 0.171, P = 0.015).
 |
Table 4 Relationship Between Maternal Dental Anxiety and Children’s Untreated Decay |
Discussion
In the present study, high and extreme dental anxiety was found in 27.6% and 21.60% of mothers, respectively. These prevalence estimates are higher than reported in other studies of adult populations using the MDAS scale.2–4 In Saudi Arabia, 17.1% and 12.4% of patients from outpatient clinics from a dental college were found to be highly and extremely anxious, respectively.4 A previous study showed that high dental anxiety was found in 19.1% and extreme dental anxiety in 12.5% of patients attending a dental school in Iran.3 The prevalence of high maternal dental anxiety was shown to be 10.7% in the Indian population.22 The Adult Dental Health Survey in the UK showed the distribution of high dental anxiety in 11.6% of the population and females demonstrated significantly greater high dental anxiety (16.7%) than males (6.9%).2 Similarly, the mean dental anxiety score in our sample of mothers was 13.89 (SD ± 5.33), which is higher than reported in females in studies from China,27 Greece,28 U.K,2 and Iran.3
Recently, Goyal et al conducted a study on 200 mother–child pairs in India and found that children of mothers with extreme dental anxiety demonstrated the highest caries experience and maternal dental anxiety was significantly related to children’s caries experience in the primary dentition (P < 0.001). The study also demonstrated the highest score of the Modified Gingival Index in children of mothers with extreme dental anxiety and the lowest score in children of mothers with no dental anxiety.22 Additionally, the studies by Khawja et al17 and Ain et al1 showed a significant positive association between maternal anxiety and dental caries in Indian children. In a study of 235 children in Croatia by Gavic et al the parental anxiety level was shown to be a significant predictor variable that affected the incidence of active caries in children.20
A review confirms that dental anxiety leads to irregular dental visits, delay and canceled appointment, and low patient satisfaction with dental care.29 According to the vicious cycle of dental anxiety by Armfield et al, individuals with dental anxiety avoid seeking dental care which aggravates their dental problems (oral diseases, infections, pain, and oral dysfunctions). The multitude of these problems further exacerbates dental anxiety and the negative behavior of avoidance of dental visits.30 Unless appropriate measures are taken to manage dental anxiety, its untoward consequences keep adding more dental and psychological problems to patients. When mothers’ do not visit dentists because of their dental anxiety, then their behavior of dental care avoidance may also continue for their children thus contributing to the increased burden of oral disease in them. Furthermore, dental anxiety runs in families as a recent study reported that dental anxiety has 30% heritability, therefore, these genetic influences are important in the development of dental anxiety in parents and their children.31 The relationship between dental anxiety in children with dental anxiety in their parents and irregular dental attendance was reported by Milsom et al, who confirmed that dentally anxious children were 1.6 times more likely to have dentally anxious parents and 3.33 times more likely to perform irregular dental visits.32 The interplay of culture, gender, age, genetics should be considered because these factors may affect expression and measurement of dental anxiety in children.9,31 In Saudi Arabia, extreme dental anxiety/phobia affected a considerable population of pregnant women (16.1%) and most participants (83.6%) did not recognize the importance of regular dental checkup.7 Therefore, dental visit avoidance behavior due to dental anxiety in mothers may also affect dental attendance patterns of their children resulting in poor oral health (untreated decay). This may explain why dentally anxious mother had children with increased caries experience in the present study.
About half the sample of children in our study had pain on eating in the last 6 months. Despite dental pain is a distressing experience for children and a worrying situation for the family, however, only about one-third of children utilized dental care in the present study. The high occurrence of untreated decay in both primary and permanent dentitions in the present study may account for a large number of children suffering from dental pain.33 The importance of visiting the dentist was emphasized in a previous study where visiting the dentist before one year was significantly associated with a reduced likelihood (odds ratio: 0.34, 95% CI: 0.24, 0.49) of having pain than attending a dental office after a year.34 Our study also shows reduced dental caries experience in the primary dentition of children who visited a dentist. These findings underscore the need for visiting dentists to prevent caries and other oral problems including pain. Other factors that have the greatest influence on inequalities in dental caries in children in Saudi Arabia include fluoride levels, oral hygiene behaviors, dietary habits, and feeding practices.11
Considering the findings of this study, it is important to emphasize better oral health education of parents to encourage dental attendance of their children for positive oral health outcomes. Dental home should be started early in life and dentally anxious mothers should be involved in implementing prevention strategies to have dental visits more appealing to their children. Dental care providers should utilize appropriate strategies to reduce dental anxiety among adult female patients which has a significant influence on the oral health of their children. The present study provided a snapshot of attitudes and behaviors of mothers regarding dental anxiety, and dental attendance and caries experience in their children in Saudi Arabia.
However, there are certain limitations to the present study. The deficiencies in sampling and representativeness should be considered when interpreting the study results. The generalizability of the study findings to the populations in other regions of Saudi Arabia should be avoided because data were collected from the participants living in a large metropolitan city in the country. Other limitations of the study which could bias its results include cross-sectional study design and self-reported data. In the future, a nationally representative sample of mothers and children should be used to investigate the influence of maternal dental anxiety including sociodemographic factors on caries and other oral conditions in children.
Conclusion
Our study found a high occurrence of maternal dental anxiety and dental caries in children. The children of dentally anxious mothers demonstrated higher caries experience in primary dentitions than the children of non-anxious mothers. The study also found a statistically significant relationship between maternal dental anxiety and untreated decay in the primary dentition. Dental professionals should identify dentally anxious mothers, provide them quality treatment ensuring high satisfaction, and raise awareness about the importance of routine dental care to achieve optimal oral health for their children.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ain TS, Sultan S, Gowhar O, Ravishankar T. Maternal dental anxiety as a risk factor for dental caries in children: a cross-sectional study. Int J Res Med Sci. 2016;4:4867–4872. doi:10.18203/2320-6012.ijrms20163782
2. Humphris G, Crawford JR, Hill K, Gilbert A, Freeman R. UK population norms for the modified dental anxiety scale with percentile calculator: adult dental health survey 2009 results. BMC Oral Health. 2013;13:29. doi:10.1186/1472-6831-13-29
3. Saatchi M, Abtahi M, Mohammadi G, Mirdamadi M, Binandeh ES. The prevalence of dental anxiety and fear in patients referred to Isfahan Dental School, Iran. Dent Res J. 2015;12(3):248–253.
4. Fayad MI, Elbieh A, Baig MN, Alruwaili SA. Prevalence of dental anxiety among dental patients in Saudi Arabia. J Int Soc Prev Community Dent. 2017;7(2):100–104. doi:10.4103/jispcd.JISPCD_19_17
5. Goettems ML, Ardenghi TM, Romano AR, Demarco FF, Torriani DD. Influence of maternal dental anxiety on oral health-related quality of life of preschool children. Qual Life Res. 2011;20(6):951–959. doi:10.1007/s11136-010-9816-0
6. Eli I, Uziel N, Blumensohn R, Baht R. Modulation of dental anxiety–the role of past experiences, psychopathologic traits and individual attachment patterns. Br Dent J. 2004;196(11):689–694. doi:10.1038/sj.bdj.4811352
7. Nazir M, Alhareky M. Dental phobia among pregnant women: considerations for healthcare professionals. Int J Dent. 2020;2020:4156165. doi:10.1155/2020/4156165
8. Cianetti S, Lombardo G, Lupatelli E, et al. Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 2017;18(2):121–130. doi:10.23804/ejpd.2017.18.02.07
9. Folayan MO, Idehen EE, Ojo OO. The modulating effect of culture on the expression of dental anxiety in children: a literature review. Int J Paediatr Dent. 2004;14(4):241–245. doi:10.1111/j.1365-263X.2004.00563.x
10. Buldur B, Güvendi ON. Conceptual modelling of the factors affecting oral health-related quality of life in children: a path analysis. Int J Paediatr Dent. 2020;30(2):181–192. doi:10.1111/ipd.12583
11. Buldur B. Pathways between parental and individual determinants of dental caries and dental visit behaviours among children: validation of a new conceptual model. Community Dent Oral Epidemiol. 2020;48(4):280–287. doi:10.1111/cdoe.12530
12. Versloot J, Veerkamp J, Hoogstraten J. Dental anxiety and psychological functioning in children: its relationship with behaviour during treatment. Eur Arch Paediatr Dent. 2008;9(Suppl 1):36–40. doi:10.1007/BF03262654
13. Al Agili DE. A systematic review of population-based dental caries studies among children in Saudi Arabia. Saudi Dent J. 2013;25(1):3–11. doi:10.1016/j.sdentj.2012.10.002
14. Olak J, Saag M, Honkala S, et al. Children’s dental fear in relation to dental health and parental dental fear. Stomatologija. 2013;15(1):26–31.
15. Buldur B, Armfield JM. Development of the Turkish version of the index of dental anxiety and fear (IDAF-4C+): dental anxiety and concomitant factors in pediatric dental patients. J Clin Pediatr Dent. 2018;42(4):279–286. doi:10.17796/1053-4628-42.4.7
16. Majstorovic M, Morse DE, Do D, et al. Indicators of dental anxiety in children just prior to treatment. J Clin Pediatr Dent. 2014;39(1):12–17. doi:10.17796/jcpd.39.1.u15306x3x465n201
17. Khawja SG, Arora R, Shah AH, Wyne AH, Sharma A. Maternal dental anxiety and its effect on caries experience among children in Udaipur, India. J Clin Diagn Res. 2015;9(6):Zc42–5. doi:10.7860/JCDR/2015/13647.6103
18. Shin WK, Braun TM, Inglehart MR. Parents’ dental anxiety and oral health literacy: effects on parents’ and children’s oral health-related experiences. J Public Health Dent. 2014;74(3):195–201. doi:10.1111/jphd.12046
19. Goettems ML, Ardenghi TM, Romano AR, Demarco FF, Torriani DD. Influence of maternal dental anxiety on the child’s dental caries experience. Caries Res. 2012;46(1):3–8. doi:10.1159/000334645
20. Gavic L, Tadin A, Mihanovic I, Gorseta K, Cigic L. The role of parental anxiety, depression, and psychological stress level on the development of early-childhood caries in children. Int J Paediatr Dent. 2018;28(6):616–623. doi:10.1111/ipd.12419
21. Esa R, Jamaludin M, Yusof ZYM. Impact of maternal and child dental anxiety on oral health-related quality of life of 5–6-year-old preschool children. Health Qual Life Outcomes. 2020;18(1):319. doi:10.1186/s12955-020-01565-z
22. Goyal J, Menon I, Singh RP, et al. Association between maternal dental anxiety and its effect on the oral health status of their child: an institutional cross sectional study. J Family Med Prim Care. 2019;8(2):535–538. doi:10.4103/jfmpc.jfmpc_415_18
23. World Health Organization. Oral Health Surveys: Basic Methods.
24. Humphris GM, Freeman R, Campbell J, Tuutti H, D’Souza V. Further evidence for the reliability and validity of the modified dental anxiety scale. Int Dent J. 2000;50(6):367–370. doi:10.1111/j.1875-595x.2000.tb00570.x
25. Bahammam MA, Hassan MH. Validity and reliability of an Arabic version of the modified dental anxiety scale in Saudi adults. Saudi Med J. 2014;35(11):1384–1389.
26. Giri J, Pokharel PR, Gyawali R, Bhattarai B. Translation and validation of modified dental anxiety scale: the Nepali version. Int Sch Res Notices. 2017;2017:5495643. doi:10.1155/2017/5495643
27. Yuan S, Freeman R, Lahti S, Lloyd-Williams F, Humphris G. Some psychometric properties of the Chinese version of the modified dental anxiety scale with cross validation. Health Qual Life Outcomes. 2008;6:22. doi:10.1186/1477-7525-6-22
28. Coolidge T, Arapostathis KN, Emmanouil D, et al. Psychometric properties of Greek versions of the modified corah dental anxiety scale (MDAS) and the dental fear survey (DFS). BMC Oral Health. 2008;8:29. doi:10.1186/1472-6831-8-29
29. Armfield JM, Heaton LJ. Management of fear and anxiety in the dental clinic: a review. Aust Dent J. 2013;58(4):390–407. doi:10.1111/adj.12118
30. Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health. 2007;7:1. doi:10.1186/1472-6831-7-1
31. Randall CL, Shaffer JR, McNeil DW, et al. Toward a genetic understanding of dental fear: evidence of heritability. Community Dent Oral Epidemiol. 2017;45(1):66–73. doi:10.1111/cdoe.12261
32. Milsom KM, Tickle M, Humphris GM, Blinkhorn AS. The relationship between anxiety and dental treatment experience in 5-year-old children. Br Dent J. 2003;194(9):503–506. doi:10.1038/sj.bdj.4810070
33. Nazir MA. Patterns of dental visits and their predictors among male adolescents. Dent Med Probl. 2018;55(2):185–190. doi:10.17219/dmp/87023
34. Nazir MA. Factors associated with dental pain related to last dental visit among adult patients. Dent Med Probl. 2018;55(1):63–68. doi:10.17219/dmp/83039
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
