Back to Journals » Patient Preference and Adherence » Volume 16
Relationship Between Family Caregiver Burden and Medication Adherence in Patients with Mechanical Valve Replacement: A Structural Equation Model
Authors Liu L, Huang W, Huang Z , Liu J, Zheng X, Tang J, Wu Y, Wang X, Liao Y, Cong L
Received 21 July 2022
Accepted for publication 30 November 2022
Published 20 December 2022 Volume 2022:16 Pages 3371—3382
DOI https://doi.org/10.2147/PPA.S383269
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Qizhi (Cathy) Yao
Lijuan Liu,1,2,* Wenzhuo Huang,1,2,* Zhuoer Huang,1,3 Jiaxin Liu,1,3 Xiaoyuan Zheng,1 Jing Tang,1,2 Ying Wu,1 Xiaohui Wang,1 Yongzhen Liao,4 Li Cong1
1School of Medicine, Hunan Normal University, Changsha, People’s Republic of China; 2Teaching and Research Section of Clinical Nursing, Xiangya Hospital of Central South University, Changsha, People’s Republic of China; 3Xiangya School of Nursing, Central South University, Changsha, People’s Republic of China; 4Shunde Polytechnic, Foshan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Li Cong, School of Medicine, Hunan Normal University, Changsha, People’s Republic of China, Tel/Fax +86-0731-88912446, Email [email protected]
Background: Oral anticoagulant is a necessary long-term treatment after mechanical valve replacement (MVR), and medication adherence has a great impact on patients with MVR. Although family caregiver burden is negatively correlated with medication adherence, little is known about the underlying mechanism.
Purpose: To test whether family caregiver burden influences medication adherence through post-traumatic growth or medication literacy in patients with MVR.
Patients and Methods: A total of 206 patients after MVR were included in this cross-sectional study from July 2021 to December 2021. Data regarding medication adherence, family caregiver burden, post-traumatic growth, and medication literacy were collected by questionnaires. Data were analyzed through SPSS, and pathway analysis was conducted by using AMOS, based on the bootstrapping method.
Results: Post-traumatic growth was positively associated with medication adherence (r = 0.284, P < 0.05). Post-traumatic growth independently mediated the association of family caregiver burden on medication adherence [β = 0.32, 95% confidence intervals: (− 0.016, − 0.008)]. The mediated effect value for post-traumatic growth was 0.07, accounting for 24.14% of the total effect. The model’s fit indices were adequate.
Conclusion: The mediating effect of post-traumatic growth between family caregiver burden and medication adherence existed in patients with MVR. Interventions considering post-traumatic growth may be useful to increase medication adherence and improve patient rehabilitation.
Keywords: medication adherence, family caregiver burden, post-traumatic growth, medication literacy, mediation analyses, mechanical valve replacement
Introduction
Valvular heart disease (VHD) is one of the most common cardiac surgical diseases and is the leading reason for loss of physical function, decreased quality of life, and reduced life expectancy in patients.1 Mechanical valve replacement (MVR) is the fundamental treatment for severe VHD.2 According to statistics,3 in 2020, heart valve replacement surgeries accounted for 29.6% of the total number of cardiac surgeries, ranking first in China. In addition, to reduce the risk of valve thrombosis and subsequent embolism, the European Society of Cardiology (ESC) and European Association for Cardio-Thoracic Surgery (EACTS) guideline recommends long-term treatment with warfarin as an anticoagulant in patients undergoing MVR.4 Therefore, the dose of warfarin should be adjusted by closely monitoring the international standards to reduce complications.5 However, due to the low medication compliance of patients, the efficacy and safety of warfarin therapy cannot be guaranteed, which increases the incidence of bleeding and thromboembolism and ultimately leads to valve failure, heart failure, reoperations, increased medical costs, decreased quality of life and even death.6 Thus, enhancing medication adherence in patients who need to take warfarin for life to maintain valve function is essential for postoperative cardiac rehabilitation.
Family support is regarded as a critical factor in facilitating the recovery of patients.7 Family caregivers, the primary person of caring for and supporting patients, provide up to 90% of the long-term care needed by patients, and the quality of in-home care is closely related to patient’s health.8 However, many family caregivers are untrained and often ill-prepared to take on caregiving tasks, such as providing wound care and overseeing complex medication management.9 Caregiver burden refers to the multifaceted biological, psychological, and social experiences felt by caregivers, which are related to imbalances in caregiver needs, support, and resources.8,10 The majority of informal family caregivers have experienced severe fatigue, stress, anxiety, and depression associated with emotional disturbances and caregiving burdens that impact their lives and health.11 Research showed12 that caregivers of schizophrenic patients with high anxiety and stress can increase caregiver burden and reduce the medication adherence of patients. Ni et al13 found that good family functioning can enhance the family caregivers’ ability to give practical support, such as supervising medication-adverse reactions, which is a positive predictor of medication adherence in patients with MVR. However, the research exploring the potential mechanisms which underline the relationship between family caregiver burden and medication adherence remains limited.
Positive psychological capital is the organizational application of positive psychology, which refers to the positive state of individual psychological development, consisting of self-efficacy, optimism, hope, and resilience.14 Researchers have recognized the link between psychological health and cardiovascular disease (CVD) for a long time, but most focused on the impact of negative emotions on disease in patients,15 while recent evidences suggest that positive psychological factors are associated with reduced risk of heart attack, stroke, and cardiovascular death.16–18 The positive psychological changes of patients are considered to be a protective factor against family caregiver burden.19 Post-traumatic growth (PTG) means the positive changes after the individual has experienced a challenge or trauma, and social support is one of the essential resilience factors.20,21 Currently, there are few studies on the positive effects of PTG on patients after MVR. However, Rahimi and Eraslan et al found a significant negative relationship between PTG and family caregiver burden in patients with myocardial infarction or cancer.22,23 Furthermore, some studies have showed that reducing family caregiver burden by improving social support can enhance patients’ PTG levels, which in turn increases patients’ confidence in the disease and adherence, thus positively affecting the prognosis of diseases.21,24,25 Therefore, this study proposes that PTG may play a mediating role between family caregiver burden and medication adherence in patients after MVR.
Medication literacy (ML), as a component of health literacy, refers to the cognitive and social skills necessary for individuals to obtain, understand, communicate, calculate and process patient-specific information about medications to make informed medication and health decisions, so that patients can take drugs safely and effectively.26 Individual and social factors are widely accepted to influence person to develop and maintain medication literacy, such as age, medication dosage, education level, and family support.18,27,28 Recent evidence suggested a weak positive relationship between health literacy and medication adherence,29 but a study from China reported a significant association between ML and medication adherence.30 These show that the extent of interaction between ML and medication adherence is still uncertain. Furthermore, a study by Qiao et al showed that social support is positively associated with ML in patients.18 In other words, family caregivers are unable to provide comprehensive medication information and emotional support, which will lead to medication errors or adverse emotions in patients31 and may increase the risk of cardiovascular adverse events, such as rehospitalization and death, thus increasing the burden on family caregivers.32 Therefore, this study proposes that ML may play a mediating role between family caregiver burden and medication adherence in patients after MVR.
In conclusion, this study aims to construct a mediation model to further explore the influence of family caregiver burden on medication adherence and its internal mechanism of Chinese patients after MVR, to improve the quality of life during recovery. Specifically, we would examine the idea that the family caregiver burden would be associated with medication adherence through PTG or ML (Figure 1).
 |
Figure 1 The hypothesized mediation model. Abbreviations: PTG, Post-traumatic Growth; ML, Medication Literacy. |
Materials and Methods
Design and Setting
A cross-sectional study was conducted in the department of cardiac surgery at three tertiary first-class hospitals in Changsha, which is located in central China, from July 2021 to December 2021. A convenience sampling method was used to select tertiary first-class hospitals, and a cluster sampling method was used to recruit MVR patients. Cardiac surgery nurses receiving comprehensive instruction and unified training served as research assistants for questionnaire collection. They were able to follow the standardized procedure in the process of collecting the questionnaires. In this study, a mediation model was constructed to examine the role of PTG or ML on the relationship between family caregiver burden and medication adherence. The study was approved by the Research Ethics Committee of Hunan Normal University (No.2022-274).
Participants and Procedures
The inclusion criteria were: (1) patients with preoperative diagnosis of valvular heart disease who underwent MVR under general anesthesia and extracorporeal circulation; (2) agreed to participate in this study; (3) aged 18 years or older; (4) no serious postoperative complications (eg, haemorrhage, cerebral infarction, acute heart failure, acute respiratory distress syndrome, paravalvular leakage, or cardiac arrest), prothrombin time and international normalized ratio were normal at discharge; and (5) were able to read and understand the questionnaires, had a nice communication ability. Patients with mental illness or cognitive impairment were excluded. Eligible patients were informed about the purposes, contents, and investigation procedures of this study, and signed informed consent before the investigation. All paper-based questionnaires were completed by patients and their caregivers on-site. All questionnaires were reclaimed on the spot after completion and were checked for missing items. If there were missing items in the returned questionnaire, it was invalid questionnaire.
Sample Size
Based on Harrell’s suggested rule of thumb33 and each variable in the linear regression model has a minimum of 10 subjects, the sample size was estimated to be 200. Besides, taking into account a 10% invalid questionnaire rate, the sample size was estimated to be 220.
Data Collection Tools
Participant Characteristics
The general information questionnaire was designed by ourselves to obtain characteristics, including gender, age, marital status, residential address, lifestyle, occupation, education level, medical payment method, personal monthly income, combined with other diseases or not, preoperative medication or not, type of medicine, number of doses per day, side effects of anticoagulants, and received health education on anticoagulant drugs or not.
Medication Adherence (The Chinese Revised Version of 8-Item Morisky Medication Adherence Scale, C-MMAS-8)
The 8-Item Morisky Medication Adherence Scale was designed by Morisky et al,34 which was developed from the MMAS-4.35 The scale was initially applied to patients with hypertension,36,37 and the Chinese version was revised by Si et al in 2012.38 The scale includes 8 items, 1 to 7 of them need to be scored in the way of “yes” or “no” (“yes” = 0 and “no” = 1). Article 5 adopts the methods of reverse scoring, and article 8 adopts a Likert 5-level scoring system. The total score of 8 or more is high medication adherence, 6–<8 is medium, and below <6 is low. This study used the Chinese revised version, which was used to assess the compliance of patients after MVR, and Cronbach’s α coefficient for the scale was 0.81.38
Family Caregiver Burden (Zarit Caregiver Burden Interview, ZBI)
Zarit Caregiver Burden Interview (ZBI) was used to assess family caregiver burden.39 It was designed on the basis of the nursing burden measurement theory proposed by Zarit et al in the 1980s. In 2006, Wang et al40 translated the ZBI into a Chinese version, and the overall scale Cronbach’s α coefficient was 0.87, indicating good reliability. The scale includes two dimensions, personal burden and responsibility burden. Personal burden consists of Items 1, 4, 5, 8, 9, 14, 16, 17, 18, 19, 20, 21, responsibility burden consists of Items 2, 3, 6, 11, 12, 13, Item 22 is the total care burden felt by the caregiver, which is rated on a 5-point Likert scale ranging from 0 to 4 (0 = “never” to 4 = “often”). The total score of ZBI ranges from 0 to 88, less than 21 indicates no or mild burden, 21 to 39 indicates moderate burden, and a score of 40 and above indicates severe burden. The Chinese revision is being widely used in China for patients with cardiovascular diseases and has shown good reliability and validity.41
Post-Traumatic Growth (Post-Traumatic Growth Inventory, PTGI)
The Post-traumatic Growth Inventory was designed by Tedeschi and Calhoun, who were American psychologists in 1996.42 The Chinese version was translated and revised by Wang et al in 2011.43
It is used to assess the positive changes and growth of individuals after trauma. The scale has 5 dimensions 21 self-reported items, including 7 items of “relating to others” (6, 8, 9, 15, 16, 20, 21), 5 items of new possibilities (3, 7, 11, 14, 17), 4 items of personal strength (4, 10, 12, 19), 3 items of appreciation of life (1, 2, 13), 2 items of spiritual change (5, 18). Using the Likert 6-level scoring method from 0 to 5 (“no change at all” = 0 to “very many such changes” = 5) assessed each item. The total score ranges from 0 to 105, 0–35 is divided into “low” level, 36–71 is divided into “medium” level, and 72–105 is divided into “high level”. The higher the score, the better the post-traumatic growth level. The revised Chinese version is appropriate for the area of cardiovascular disease in China, and its reliability and validity are acceptable.44
Medication Literacy (Medication Literacy Assessment in Spanish and English, MedLitRxSE)
The questionnaire was compiled by Professor Maniaci of Mayo Hospital in the United States,45 and Zheng et al46 sinicized it according to Chinese national conditions and cultural characteristics. The content of the Chinese version involves evaluating the ability to understand, calculating and processing drug information. A two-point system was used to score (“correct” = 1 and “error” = 0), and the higher the total score, the higher the level of patient’s medication literacy. The test–retest reliability was 0.885, the split-half reliability was 0.840, and the K-R value was 0.820. For this study, the revised Chinese version was adopted and Cronbach’s α coefficient of this scale was 0.80 in patients after MVR.13
Statistical Analyses
Uniform coding after questionnaire recovery, data were analyzed using SPSS 23.0 and AMOS 22.0. For continuous data, variables were described as the means and standard deviations (SDs), and the differences between groups were compared using independent sample t-test. For categorical data, variables were described as counts and percentages, and the differences between groups were compared using the chi-square (χ2) test. Multiple stepwise regression was used to explore significant predictors of medication adherence. Pearson correlation was used to assess the relationship among medication adherence, family caregiver burden, PTG, and ML. In this study, a structural equation model (SEM) with maximum likelihood estimation was used to test the hypotheses outlined in the conceptual model (Figure 1). The model fit was assessed based on the following model-fit indices:47 chi-square (χ2), goodness of fit index (GFI), adjusted goodness-of-fit-index (AGFI), incremental fit index (IFI), comparative fit index (CFI), Tucker-Lewis index (TLI), normed fit index (NFI), and root mean square error of approximation (RMSEA). According to the hypothesized model, we calculated the mediating effect on PTG and ML in the relationship between family caregiver burden and medication adherence, respectively. The bootstrapping method is used to analyze the indirect mediation effects of post-traumatic growth. All P ≤ 0.05 (two-sided) was considered statistically significant.
Results
Characteristics of Patients Effect Main Variables
A total of 210 questionnaires were distributed in this study, 206 valid questionnaires were recovered, and 4 invalid questionnaires were excluded. Finally, the effective response rate was 98.09%. Among the 206 participants, the average age was 54.78 ± 11.43, of which 97 (47.1%) participants were male, 109 (52.9%) were female, 96.1% were taking only one anticoagulant drug (warfarin). The characteristics of patients are presented in Table 1. The univariate analysis showed that male patients had significantly higher levels of medication adherence compared to the females (P = 0.035). Also, patients with health insurance had greater medication adherence (P = 0.020). Medical payment method (P = 0.004) and type of anticoagulant medication (P = 0.008) were associated with family caregiver burden, marital status (P = 0.026) and primary caregiver (P = 0.000) were associated with ML, and all variables were not statistically correlated with PTG (P > 0.05) (Table 1).
 |
Table 1 Comparison of Medication Adherence, Family Caregiver Burden, Post-Traumatic Growth and Medication Literacy (n = 206, |
Multiple Stepwise Regression Analysis of Medication Adherence
The analysis showed that the family caregiver burden (P = 0.001), PTG (P = 0.001), gender (P = 0.026), and medical payment method (P = 0.044) were the interfering factors of medication adherence in patients after MVR (adjusted R2 = 0.164; P < 0.001). Marital status, type of anticoagulant, and ML were not associated with medication adherence (Table 2).
 |
Table 2 Multiple Stepwise Regression Analysis of Medication Adherence in Patients (n = 206) |
Mean Scores and Correlation Matrix of Main Variables
The means and standard deviations of medication adherence, PTG, family caregiver burden, and ML are shown in Table 3. Family caregiver burden was negatively associated with medication adherence (r = −0.310, P < 0.01), while PTG was positively related to medication adherence (r = 0.284, P < 0.01). PTG was negatively correlated with family caregiver burden (r = −0.226, P < 0.01) (Table 3).
 |
Table 3 Mean Scores and Correlation Matrix of Medication Adherence, Family Caregiver Burden, Post-Traumatic Growth and Medication Literacy (n = 206) |
Structural Equation Model of Medication Adherence
Structural equation model was performed to test the path relationship among medication adherence, post-traumatic growth, and family caregiver burden. The model was calculated using the maximum likelihood ratio, and the mediating effect test was performed using the bootstrapping method. The final model showed good model-fit indices (χ2 /df = 2.662, GFI = 0.915, AGFI = 0.903, IFI = 0.910, CFI = 0.909, TLI = 0.914, NFI = 0.940, RMSEA = 0.078). The results showed that family caregiver burden negatively predicted medication adherence and post-traumatic growth (β = −0.36, β = −0.24, P < 0.001), post-traumatic growth positively predicted medication adherence (β = 0.32, P < 0.001). Moreover, the mediated effect value for post-traumatic growth was 0.07, accounting for 0.07/0.29 × 100% = 24.14% of the total effect. All paths are shown in Figure 2. Standardized direct, indirect and mediated effects are summarized in Table 4.
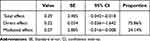 |
Table 4 Direct, Indirect and Total Effects of Variables in the Model |
Discussion
Non-adherence to medication in post-operative MVR patients can lead to poor clinical outcomes, higher disease mortality, and unnecessary health care expenditures,48 so it is essential to enhance long-term survival by improving medication adherence in this patient population. The mean medication adherence score was 5.72 ± 1.79, with 43.7% of participants in low adherence, which was higher than the 13.2% to 33.26% in studies conducted in China and other countries,49,50 this difference may be related to the study region, design and sample size. However, it still indicated that medication adherence was suboptimal and improving medication adherence in patients after MVR was a significant problem to be solved urgently. At the same time, our results showed that gender and medical payment methods were independent factors affecting medication adherence, which was consistent with previous studies. Vervloet et al found that female patients have lower adherence to cardiovascular medications compared to males.51 Several other studies have indicated poor medication adherence in female patients due to medication susceptibility, medication side effects, and perception of taking medication.52–54 In addition, a systematic evaluation also pointed out that poor medication adherence was associated with high out-of-pocket expenditures, low income, financial flexibility, or lack of medication insurance.55 This study found the relationship among medication adherence, family caregiver burden, PTG, ML and provided a basis for understanding the influencing factors that may improve medication adherence in patients after MVR. The equation modeling results demonstrated that family caregiver burden and PTG were critical predictors of medication adherence. Specifically, the family caregiver burden had a direct effect on medication adherence and an indirect effect on medication adherence through PTG.
The caregiving capacity of family caregivers was one of the important factors to facilitate patients’ adherence, and poor medication adherence was associated with family caregiver burden.12 Our findings demonstrated that family caregiver burden was a negative predictor of medication adherence in patients after MVR. As reported in previous studies, family caregivers played a critical role in monitoring medication adherence and medication side effects. Caregivers with heavy burdens may lack knowledge and skills in medication management, which leads to poor medication adherence in patients.13,56,57 In conclusion, healthcare providers should assess the family caregiver burden level of patients before instructing medication self-management and pay more attention to patients with higher family caregiving burdens. Furthermore, during the nursing care, healthcare providers should keep pace with the health status and needs of family caregivers, actively provide resources and assistances to them, and encourage caregivers to express their negative emotions, which will strengthen their role in ensuring optimal medication adherence for patients after MVR.
Additionally, in this study, PTG was a mediating variable in the influence of family caregiver burden on medication adherence in patients after MVR. In other words, low burden of family caregiver helped to improve the PTG level of patients, which impacted the medication adherence. Hu et al found that caregivers with heavy burdens were more likely to experience negative emotions such as anxiety and depression, which reduced their motivation to care. They were unable to provide adequate medication information and emotional support to patients, thus affecting the treatment and recovery.58 Furthermore, as previously reported, patients’ PTG levels could be enhanced by increasing social support, and patients with higher PTG levels were more confident in better health outcomes and medication adherence.59,60 Above all, healthcare professionals can improve the PTG levels of patients with MVR by reducing family burden, increasing social support, and focusing on positive psychological changes.
In the conceptual model, medication literacy was an important predictor of medication adherence, and previous studies supported this hypothesis.6,13 However, our study did not find a direct effect of ML on medication adherence and also failed to find a mediating role for medication literacy as a mediator of family caregiver burden and medication adherence. It probably relates to the following reasons: (1) ML assessment focuses on the reading comprehension and computational skills of the subjects and evaluates medication information, not accurately assesses the extent of the correlation between medication adherence and ML; and (2) The mean value of ML score in this study is 9.05 ± 3.71, which is higher than prior study,13 and the difference is probably related to the study population, design and degree of education.27 However, 74.6% of the patients felt various difficulties to some extent in adhering to regular and quantitative medication, which was mainly related to the anxiety caused by the fear of adverse drug reactions, thus affecting the level of PTG and the adherence of medication in patients after MVR. Although medication literacy has not direct or indirect effects on medication adherence, healthcare providers should also focus on the patients’ medication literacy to further improve the level of medication adherence.
Conclusion
Our study identified some factors associated with medication adherence in patients after MVR and clarified the relationship among them. Meantime, the mediating effect of post-traumatic growth between family caregiver burden and medication adherence existed in patients with MVR, thus providing a new perspective on intervention studies related to medication adherence and a basis for developing intervention programs aimed at improving patients’ medication adherence. Furthermore, the intervention that considering post-traumatic growth may be useful to increase medication adherence and improve patient rehabilitation.
Abbreviations
VHD, Valvular heart disease; MVR, Mechanical valve replacement; PTG, Post-traumatic growth; ML, Medication literacy; CVD, Cardiovascular disease; SEM, Structural equation model; SD, standard deviation; ZBI, Zarit Caregiver Burden Interview; PTGI, The Post-traumatic Growth Inventory; C-MMAS-8, The Chinese Revised Version of 8-Item Morisky Medication Adherence Scale; SE, standard error; CI, confidence interval.
Data Sharing Statement
The original contributions presented in this study are included in the article, which can be further queried to the corresponding authors.
Ethics Approval and Participate
The study involving human subjects was reviewed and approved by the Research Ethics Committee of Hunan Normal University. Patients provided their written informed consent for participation in this study.
Acknowledgment
We are grateful to the School of Medicine, Hunan Normal University for funding and giving ethical clearance to conduct this research. Additionally, we would like to express our gratitude to the hospital staff and the participants in this study. The MMAS-8 Scale, content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from MMAR, LLC., Donald E. Morisky, ScD, ScM, MSPH, USA; [email protected]
Funding
This study was funded by National Students’ Platform for Innovation and Entrepreneurship Training Program (No.202110542025).
Disclosure
The authors declare that the study was conducted without any business or financial relationship that could be interpreted as potential conflicts of interest.
References
1. Coffey S, Roberts-Thomson R, Brown A, et al. Global epidemiology of valvular heart disease. Nat Rev Cardiol. 2021;18(12):853–864.
2. Zhu Z, Li C, Shen J, et al. New internet-based warfarin anticoagulation management approach after mechanical heart valve replacement: prospective, multicenter, randomized controlled trial. J Med Internet Res. 2021;23(8):e29529. doi:10.2196/29529
3. Hao X, Hei FL, Hou XT. White book of Chinese cardiovascular surgery and extracorporeal circulation in 2020. Chin J Extracorporeal Circ. 2021;19(05):257–260.
4. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561–632.
5. Nelson WW, Desai S, Damaraju CV, et al. International normalized ratio stability in warfarin-experienced patients with nonvalvular atrial fibrillation. Am J Cardiovasc Drugs. 2015;15(3):205–211.
6. Park S, Jang I. Factors affecting medication adherence in patients with mechanical heart valves taking warfarin: the role of knowledge on warfarin, medication belief, depression, and self-efficacy. Int J Environ Res Public Health. 2021;18(10):5214.
7. Cardoso-Moreno MJ, Tomas-Aragones L. The influence of perceived family support on post surgery recovery. Psychol Health Med. 2017;22(1):121–128. doi:10.1080/13548506.2016.1153680
8. Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052–1060. doi:10.1001/jama.2014.304
9. Magasi S, Buono S, Yancy CW, Ramirez RD, Grady KL. Preparedness and mutuality affect quality of life for patients with mechanical circulatory support and their caregivers. Circ Cardiovasc Qual Outcomes. 2019;12(1):e004414. doi:10.1161/CIRCOUTCOMES.117.004414
10. Sherwood PR, Given CW, Given BA. Caregiver burden and depressive symptoms: analysis of common outcomes in caregivers of elderly patients. J Aging Health. 2005;17(2):125–147. doi:10.1177/0898264304274179
11. Pereira BDS, Fernandes NDS, de Melo NP, Abrita R, Grincenkov F, Fernandes N. Beyond quality of life: a cross sectional study on the mental health of patients with chronic kidney disease undergoing dialysis and their caregivers. Health Qual Life Outcomes. 2017;15(1):74. doi:10.1007/s40256-015-0120-9
12. Kretchy IA, Osafo J, Agyemang SA, Appiah B, Nonvignon J. Psychological burden and caregiver-reported non-adherence to psychotropic medications among patients with schizophrenia. Psychiatry Res. 2018;259:289–294. doi:10.1016/j.psychres.2017.10.034
13. Ni H, Lin Y, Peng Y, Li S, Huang X, Chen L. Relationship between family functioning and medication adherence in Chinese patients with mechanical heart valve replacement: a moderated mediation model. Front Pharmacol. 2022;13:817406. doi:10.3389/fphar.2022.817406
14. Youssef-Morgan CM, Luthans F. Psychological capital and well-being. Stress Health. 2015;31(3):180–188. doi:10.1002/smi.2623
15. Tully PJ, Baumeister H, Bennetts JS, Rice GD, Baker RA. Depression screening after cardiac surgery: a six month longitudinal follow up for cardiac events, hospital readmissions, quality of life and mental health. Int J Cardiol. 2016;206:44–50. doi:10.1016/j.ijcard.2016.01.015
16. Boehm JK, Soo J, Chen Y, et al. Psychological well-being’s link with cardiovascular health in older adults. Am J Prev Med. 2017;53(6):791–798. doi:10.1016/j.amepre.2017.06.028
17. Kubzansky LD, Huffman JC, Boehm JK, et al. Positive psychological well-being and cardiovascular disease: JACC health promotion series. J Am Coll Cardiol. 2018;72(12):1382–1396. doi:10.1016/j.jacc.2018.07.042
18. Qiao L, Ding S, Zhong Z, Liu X, Lai L, Zheng F. Association between social support and medication literacy in Chinese patients with coronary heart disease. Front Cardiovasc Med. 2021;8:705783. doi:10.3389/fcvm.2021.705783
19. Eleuteri S, Bellanti G, Falaschi P. Hip fracture: preliminary results supporting significative correlations between the psychological wellbeing of patients and their relative caregivers. J Gerontol Geriatr. 2016;64:104–111.
20. Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–471. doi:10.1007/BF02103658
21. Li Y, Qiao Y, Luan X, Li S, Wang K. Family resilience and psychological well-being among Chinese breast cancer survivors and their caregivers. Eur J Cancer Care. 2019;28(2):e12984. doi:10.1111/ecc.12984
22. Rahimi R, Heidarzadeh M, Shoaee R. The relationship between posttraumatic growth and social support in patients with myocardial infarction. Can J Cardiovasc Nurs. 2016;26(2):19–24.
23. Eraslan P, Ilhan A, Eraslan E, Karacin C, Cakmak Oksuzoglu OB. The relationship between caregiver burden and posttraumatic growth in caregivers of patients with metastatic cancer. Cureus. 2022;14(3):e23622. doi:10.7759/cureus.23622
24. Kim H, Son H. Moderating effect of posttraumatic growth on the relationship between social support and quality of life in colorectal cancer patients with ostomies. Cancer Nurs. 2021;44(3):251–259. doi:10.1097/NCC.0000000000000887
25. Costa ALS, Heitkemper MM, Alencar GP, Damiani LP, Silva RMD, Jarrett ME. Social support is a predictor of lower stress and higher quality of life and resilience in Brazilian patients with colorectal cancer. Cancer Nurs. 2017;40(5):352–360. doi:10.1097/NCC.0000000000000388
26. Pouliot A, Vaillancourt R, Stacey D, Suter P. Defining and identifying concepts of medication literacy: an international perspective. Res Social Adm Pharm. 2018;14(9):797–804. doi:10.1016/j.sapharm.2017.11.005
27. Plaza-Zamora J, Legaz I, Osuna E, Perez-Carceles MD. Age and education as factors associated with medication literacy: a community pharmacy perspective. BMC Geriatr. 2020;20(1):501. doi:10.1186/s12877-020-01881-5
28. Ma G, Luo A, Shen Z, Duan Y, Shi S, Zhong Z. The status of medication literacy and associated factors of hypertensive patients in China: a cross-sectional study. Intern Emerg Med. 2020;15(3):409–419. doi:10.1007/s11739-019-02187-0
29. Oscalices MIL, Okuno MFP, Lopes M, Batista REA, Campanharo CRV. Health literacy and adherence to treatment of patients with heart failure. Rev Esc Enferm USP. 2019;53:e03447. doi:10.1590/S1980-220X2017039803447
30. Zheng F, Ding S, Lai L, et al. Relationship between medication literacy and medication adherence in inpatients with coronary heart disease in Changsha, China. Front Pharmacol. 2019;10:1537. doi:10.3389/fphar.2019.01537
31. Mira JJ, Lorenzo S, Guilabert M, Navarro I, Perez-Jover V. A systematic review of patient medication error on self-administering medication at home. Expert Opin Drug Saf. 2015;14(6):815–838. doi:10.1517/14740338.2015.1026326
32. Cajita MI, Cajita TR, Han HR. Health literacy and heart failure: a systematic review. J Cardiovasc Nurs. 2016;31(2):121–130. doi:10.1097/JCN.0000000000000229
33. Harrell FE
34. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–354.
35. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi:10.1097/00005650-198601000-00007
36. Berlowitz DR, Pajewski NM, Kazis LE, Bolin L, Conroy LB, Fitzpatrick P. Intensive blood-pressure treatment and patient-reported outcomes. N Engl J Med. 2017;377(21):2097. doi:10.1056/NEJMc1712573
37. Bress AP, Bellows BK, King JB, Hess R, Beddhu S, Zhang Z. Cost-effectiveness of intensive versus standard blood-pressure control. N Engl J Med. 2017;377(8):745–755. doi:10.1056/NEJMsa1616035
38. Si ZX, Guo LX, Zhou M, Cao GQ. Reliability and validity of the modified morisky medication adherence scale applied to patients on warfarin therapy after mechanical heart-valve replacement. J Nurs Sci. 2012;27(22):23–26.
39. Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist. 1986;26(3):260–266. doi:10.1093/geront/26.3.260
40. Wang L, Yang XS, Hou Z, Feng QL. Application and evaluation of Chinese version of zarit caregiver burden interview. Chin J Public Health. 2006;22(08):970–972.
41. Hu X, Dolansky MA, Su Y, Hu X, Qu M, Zhou L. Effect of a multidisciplinary supportive program for family caregivers of patients with heart failure on caregiver burden, quality of life, and depression: a randomized controlled study. Int J Nurs Stud. 2016;62:11–21. doi:10.1016/j.ijnurstu.2016.07.006
42. Tedeschi RG, Cann A, Taku K, Senol-Durak E, Calhoun LG. The posttraumatic growth inventory: a revision integrating existential and spiritual change. J Trauma Stress. 2017;30(1):11–18. doi:10.1002/jts.22155
43. Wang J, Chen Y, Wang YB, Liu XH. Revision of the posttraumatic growth inventory and testing its reliability and validity. J Nurs Sci. 2011;26(14):26–28.
44. Zhao Y, Zhang A. Influence of self-management behavior and anxiety-depression in patients with percutaneous coronary intervention on post-traumatic growth. Chin Nurs Res. 2016;30(16):1941–1944.
45. Sauceda JA, Loya AM, Sias JJ, Taylor T, Wiebe JS, Rivera JO. Medication literacy in Spanish and English: psychometric evaluation of a new assessment tool. J Am Pharm Assoc. 2012;52(6):e231–e240.
46. Zheng F, Zhong ZQ, Ding SQ, Luo AJ, Liu ZN. Modification and evaluation of assessment of medication literacy. J Cent South Univ. 2016;41(11):1226–1231.
47. McNeish D, An J, Hancock GR. The thorny relation between measurement quality and fit index cutoffs in latent variable models. J Pers Assess. 2018;100(1):43–52. doi:10.1080/00223891.2017.1281286
48. Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015:217047. doi:10.1155/2015/217047
49. Wang X, Xu B, Liang H, et al. Distribution characteristics and factors influencing oral warfarin adherence in patients after heart valve replacement. Patient Prefer Adherence. 2018;12:1641–1648. doi:10.2147/PPA.S172223
50. Thomson Mangnall LJ, Sibbritt DW, Al-Sheyab N, Gallagher RD. Predictors of warfarin non-adherence in younger adults after valve replacement surgery in the South Pacific. Heart Asia. 2016;8(2):18–23. doi:10.1136/heartasia-2016-010751
51. Vervloet M, Korevaar JC, Leemrijse CJ, Paget J, Zullig LL, van Dijk L. Interventions to improve adherence to cardiovascular medication: what about gender differences? A systematic literature review. Patient Prefer Adherence. 2020;14:2055–2070. doi:10.2147/PPA.S260562
52. Kiely KM, Brady B, Byles J. Gender, mental health and ageing. Maturitas. 2019;129:76–84. doi:10.1016/j.maturitas.2019.09.004
53. Karalis DG, Wild RA, Maki KC, et al. Gender differences in side effects and attitudes regarding statin use in the understanding statin use in America and gaps in patient education (USAGE) study. J Clin Lipidol. 2016;10(4):833–841. doi:10.1016/j.jacl.2016.02.016
54. Bandiera C, Lam L, Locatelli I, et al. Understanding reasons and factors for participation and non-participation to a medication adherence program for patients with diabetic kidney disease in Switzerland: a mixed methods study. Diabetol Metab Syndr. 2022;14(1):140. doi:10.1186/s13098-022-00898-7
55. Holbrook AM, Wang M, Lee M, et al. Cost-related medication nonadherence in Canada: a systematic review of prevalence, predictors, and clinical impact. Syst Rev. 2021;10(1):11. doi:10.1186/s13643-020-01558-5
56. Xu M, Markstrom U, Lyu J, Xu L. Detection of low adherence in rural tuberculosis patients in China: application of morisky medication adherence scale. Int J Environ Res Public Health. 2017;14(3):248.
57. Park EO, Yates BC, Meza J, Kosloski K, Pullen C. Spousal caregivers of coronary artery bypass surgery patients: differences between caregivers with low vs. high caregiving demands. Rehabil Nurs. 2016;41(5):260–269. doi:10.1002/rnj.252
58. Hu P, Yang Q, Kong L, Hu L, Zeng L. Relationship between the anxiety/depression and care burden of the major caregiver of stroke patients. Medicine. 2018;97(40):e12638. doi:10.1097/MD.0000000000012638
59. Zhang L, Lu Y, Qin Y, Xue J, Chen Y. Post-traumatic growth and related factors among 1221 Chinese cancer survivors. Psychooncology. 2020;29(2):413–422. doi:10.1002/pon.5279
60. Tomita M, Takahashi M, Tagaya N, Kakuta M, Kai I, Muto T. Structural equation modeling of the relationship between posttraumatic growth and psychosocial factors in women with breast cancer. Psychooncology. 2017;26(8):1198–1204. doi:10.1002/pon.4298
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


