Back to Journals » Clinical Ophthalmology » Volume 16
Refractive and Visual Outcomes After Implantation of a Secondary Sulcus Intraocular Lens with an Extended Depth of Focus
Authors Gundersen KG , Potvin R
Received 12 March 2022
Accepted for publication 31 May 2022
Published 9 June 2022 Volume 2022:16 Pages 1861—1869
DOI https://doi.org/10.2147/OPTH.S366145
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Kjell Gunnar Gundersen,1 Richard Potvin2
1IFocus Øyeklinikk AS, Haugesund, Norway; 2Science in Vision, Bend, OR, USA
Correspondence: Kjell Gunnar Gundersen, IFocus Øyeklinikk AS, Sørhauggata 111, Haugesund, 5527, Norway, Tel +47 808900, Email [email protected]
Purpose: To evaluate the range of vision, visual function, and quality of vision after implantation of a secondary extended depth of focus intraocular lens (EDOF IOL) implanted in the sulcus.
Setting: One clinical practice in Haugesund, Norway.
Design: Prospective single arm non-interventional study.
Methods: Eligible subjects presenting for surgery, or who had previous successful primary cataract or refractive lens exchange surgery in both eyes were subsequently implanted with the AddOn® secondary EDOF IOL in the sulcus. Manifest refraction and visual acuity at distance, intermediate and near were measured 3 months after surgery, along with the monocular defocus curve. Subjects also completed a visual function and a quality of vision questionnaire.
Results: The study included 32 eyes of 16 subjects. At 3 months postoperative, the mean refraction spherical equivalent (MRSE) was − 0.16 ± 0.30 D, with a residual cylinder of 0.29 ± 0.27 D. The mean monocular uncorrected VA was 0.1 logMAR (20/25) or better at all test distances. The monocular defocus curves showed a depth of focus of 2.0 D. For every category except reading fine print, all but one subject (94%) had no difficulty or little difficulty with near tasks. Glare and halos were the most common visual disturbances, with no reports of starbursts. There was no evidence of any intralenticular opacification in any of the eyes, and no evidence of iris chafing/depigmentation.
Conclusion: This secondary EDOF IOL provided excellent distance and intermediate vision, and very good near vision to subjects. Subject reported near visual function was also very good and visual disturbances were limited. This lens appears to be a good option for patients who would like to improve their range of vision. Results appear as good or better than those reported for primary EDOF lenses.
Keywords: sulcus, secondary IOL, AddOn EDOF, EDOF, extended depth of focus
Plain Language Summary
Many patients at the time of cataract surgery choose a single-vision intraocular lens (monofocal IOL) to correct their distance vision in both eyes. Some, after surgery, desire better intermediate and near vision. For these patients, a secondary lens can be implanted in the eye, on top of the first, adding optical elements to achieve this objective. One such option is an extended depth of focus (EDOF) IOL, which is designed to increase the patient’s range of vision. This design is different from a multifocal IOL, which has distinct focal points for intermediate and/or near vision. EDOF IOLs appear less likely to produce visual disturbances than multifocal IOLs. This study was designed to determine if a secondary EDOF lens could increase the range of vision of patients previously implanted with a monofocal IOL without producing unacceptable visual disturbances.
Our results showed that the secondary lenses implanted provided patients with good intermediate and near vision. With the exception of reading small print, all but one of the subjects reported little or no difficulty with near and intermediate tasks, with low levels of reported visual disturbances.
Introduction
Patients presenting for cataract surgery with a monofocal intraocular lens (IOL) implant targeted for emmetropia can generally expect good distance vision postoperatively, though intermediate and near vision may not be as clear. Some of these patients may later be interested in having better intermediate and/or near vision. One option to achieve this goal is a secondary IOL implant.
It has been more than 20 years since secondary (piggyback) lenses were implanted to provide improved intermediate and near vision to pseudophakic patients.1,2 Challenges with power calculation appeared to limit adoption.1 There was also a general concern about the potential for interlenticular opacification with piggyback IOLs, which made lens placement and selection of lens material important considerations.3 The potential for iris depigmentation from chafing was also a concern, as it could lead to elevated intraocular pressure as a consequence of pigment deposition in the trabecular meshwork.4,5 These considerations necessitated unique designs for sulcus IOLs, such as rounding the optic edges to reduce friction effects.4
More recent studies have shown that the improved optical designs and materials have made secondary IOL implantation a generally safe and effective procedure.6 Secondary IOLs may be used successfully for the correction of residual ametropia,7–9 including astigmatism,10–13 though with some toric lens designs rotational stability has been problematic.12 Secondary IOLs have also been demonstrated to be a safe and effective alternative for providing multifocal vision for patients previously implanted with monofocal IOLs; clinical outcomes for secondary multifocal IOL implantation appear equivalent to those achieved with primary multifocal implantation.14–16
An alternative to a multifocal IOL, which is designed to provide distinct foci for intermediate and/or near vision, is an extended depth of focus (EDOF) IOL. These lenses use optical principles to extend the depth of field of the primary focal point, without introducing excessive image degradation. They generally provide better intermediate and near vision than a monofocal IOL.17 The limitations on extending the depth of field results in worse near vision than a trifocal or bifocal IOL, but EDOF lenses have generally been associated with lower levels of visual disturbance.18 Satisfaction with both lens types appears high.
The lens studied here (AddOn® EDOF IOL, 1stQ GmbH, Mannheim, Germany) was designed to provide patients who were previously implanted with a monofocal IOL targeted for distance the potential to extend their range of vision, while also correcting any residual refractive ametropia. It may also be implanted at the same time as a primary IOL, allowing reversal of the procedure if visual disturbances or ocular health require it. Figure 1 shows an image of the lens. It is made from a hydrophilic acrylic material and has a convex anterior and concave posterior to reduce the potential for contact with the primary IOL. The edges are rounded and polished. The base lens design has been shown to provide stable clinical outcomes in both a spherical and toric configuration.9,11 A trifocal version of the lens has also been shown to provide good clinical outcomes.19 In the EDOF design, four diffractive rings configured using a proprietary design (elevated phase shift, or EPS) are used to extend the depth of focus. A spherical refractive correction from −5.0 to +5.0 can be incorporated into the lens to address residual refractive errors that may be present after primary IOL implantation.
 |
Figure 1 The AddOn® EDOF sulcus lens (courtesy 1stQ GmbH, used with permission). |
This study was designed to evaluate the visual and refractive outcomes, visual function, and quality of vision after sulcus implantation of the secondary EDOF lens described above.
Methods
This study was prospective single arm study of refractive, visual, and subjective quality outcomes after sulcus implantation of a secondary EDOF IOL. The study was reviewed and approved by an institutional review board (REK, Norway). All enrolled subjects signed an informed consent document. The study was conducted in accordance with the tenets of the Declaration of Helsinki, International Harmonization (ICH) Guidelines and good clinical practice. The subjects self-selected for the IOL in question and were then invited to participate in the study. As such, the study did not involve an intervention, so registration with a clinical trial registry was not required. Data are not available for sharing.
Eligible subjects were those who had previous successful primary cataract or refractive lens exchange (RLE) surgery in both eyes, with bilateral implantation of monofocal IOLs targeted for emmetropia. Also eligible were those subjects interested in an EDOF correction that could be reversed if the subject was unhappy with the result; these subjects had the primary and secondary IOL implanted during the same surgery. All subjects had to be interested in better intermediate and near vision after surgery (extending their range of vision). Subjects who had prior surgical complications or pathology that might affect best-corrected visual acuity (eg, amblyopia) were excluded.
In addition to the above, patients had to be appropriate candidates for a sulcus IOL, with a pseudophakic anterior chamber depth of more than 3.2 mm, no evidence of glaucoma and no corneal (eg, guttatta) or retinal issues. The mesopic pupil size had to be <5 mm, to reduce the potential for dysphotopsia.
Subjects were bilaterally implanted with sulcus EDOF lenses using the usual standard of care in the practice. EDOF IOL power was calculated using the dedicated online calculator. The manifest refraction and monocular visual acuities at distance (4m), intermediate (60 cm) and near (40 cm) were evaluated 3 months post secondary IOL implantation. The 3-month visit also include measurement of the distance-corrected monocular defocus curve and administration of two questionnaires: the Quality of Vision questionnaire20 and the National Eye Institute Visual Function Questionnaire (NEI-VFQ) near vision subscale.
The primary measure of interest was the criterion specified in the American Academy of Ophthalmology (AAO) consensus statement for EDOF lenses that at least 50% of eyes achieve a monocular distance corrected intermediate visual acuity (DCIVA) of logMAR 0.2 (20/32) or better.21 Relevant additional measures from the consensus statement were also evaluated when the collected data allowed. These included the effective range of vision and a proxy comparison between CDVA of the EDOF lens with a monofocal control.
A slit lamp examination was conducted to determine if any iris depigmentation due to chafing or any intralenticular opacification was evident. Each visit also included checking for adverse events.
An analysis of variance was used to compare parametric variables, with a specified statistical significance of p < 0.05.
Results
Sixteen subjects (32 eyes) were enrolled, and all subjects completed the study. There were 12 males and four female subjects. The average age was 64 ± 8 years, with a range of from 46 to 76. The primary lenses implanted were 72% (23/32) Acrysof® (Alcon, Fort Worth, USA) and 22% (7/32) Micropure (BVI, Waltham, USA), both of which are made of hydrophobic acrylic material. The remaining two lenses could not be identified as they were implanted at a different surgery center. All primary lenses were implanted in the bag. Biometric details, primary IOL power and surgery timing details are shown in Table 1. The EDOF lens was implanted in a combined procedure (simultaneous surgery) in 31% of eyes (10/32).
 |
Table 1 Biometric, Surgery and Timing Data |
At 3 months postoperative, the mean refraction spherical equivalent (MRSE) was −0.16 ± 0.30 D (range −0.875 to +0.50 D), with a residual cylinder of 0.29 ± 0.27 D (range 0.0 to 1.0 D). Thirty of 32 eyes (94%) had an MRSE within 0.50 D of plano, and 28 of 32 eyes (88%) had a residual cylinder of 0.50 D or less. Twenty-six eyes (81%) met both criteria. There was no statistically significant difference in the MRSE (p = 0.57) or the refractive cylinder (p = 0.31) between eyes undergoing simultaneous surgery and those that had a secondary surgery at a later date, though the number of eyes in each sample size in this stratification may be too small to be meaningful.
Figure 2 shows the uncorrected and distance-corrected monocular visual acuity at various test distances, measured 3 months after secondary EDOF lens implantation. There was a statistically significant difference between uncorrected and distance corrected VA at 4 m (p < 0.01), but no difference at 60 cm (p = 0.83) or 40 cm (p = 0.30). The mean monocular uncorrected VA was 0.1 logMAR (20/25) or better at all test distances. At 60 cm, 91% of eyes (58/64) had a DCIVA of 0.2 logMAR or better. Twenty-two of 32 subjects (69%) had an uncorrected monocular UDVA of 0.1 logMAR or better, with 31 of 32 (97%) having a CDVA of 0.1 logMAR or better. There was no statistically significant difference in the uncorrected (p = 0.24) or corrected (p = 0.33) distance vision between the eyes undergoing simultaneous surgery and those that had a secondary surgery at a later date.
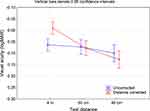 |
Figure 2 Monocular visual acuity at different test distances. Abbreviation: logMAR, log of the minimum angle of resolution. |
The AAO consensus document requires a comparison of the CDVA of the EDOF lens to the CDVA from a monofocal control. In the current study, ten eyes had the IOL implanted in the sulcus in a separate surgery after the primary cataract surgery, with a plano sphere power in the EDOF lens. For these eyes, it was possible to compare the best distance visual acuity (CDVA) pre- and post-EDOF implantation. These eyes effectively served as their own controls, to test the difference between CDVA with a monofocal (preop) and an EDOF lens (postop). A repeated measures analysis of variance showed no statistically significant difference between the two values, though the pre-implant CDVA was about 2 logMAR letters (just under half a line) better than the post-implant CDVA (−0.05 ± 0.05 vs −0.01 ± 0.05, p = 0.055).
Figure 3 shows the mean monocular distance-corrected defocus curve for the IOL. The depth of focus as measured using the AAO criteria (range of lens powers from zero to the last power with a mean VA of 0.2 logMAR or better) was 2.0 D.
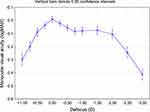 |
Figure 3 Monocular distance corrected defocus curve. Abbreviations: logMAR, log of the minimum angle of resolution; D, diopter. |
Results from the NEI-VFQ near vision subscale are shown in Table 2. For every category except reading fine print, all but one subject (94%) had no difficulty or little difficulty with near tasks. Reading small print was reported as the most difficult task and was the only task where any subject reported extreme difficulty performing it; only one subject reported extreme difficulty.
 |
Table 2 NEI-VFQ Near Vision Subscale Scores (n = 16) |
Figure 4 shows the mean response scores (with the standard error) related to each of the specific visual disturbances included in the Quality of Vision questionnaire. The mean frequency scores were all below 1. Mean severity scores were lower than the mean frequency scores for all disturbances, and the mean degree of bother reported was less than 0.5 in all cases. Glare and halos were reported to be the most frequent, most severe, and most bothersome visual disturbances. All but two subjects (14/16, 88%) reported that glare was “not at all” or “a little” bothersome. All but one subject (15/16, 94%) reported the same for halos. There were no reports of starbursts.
 |
Figure 4 Mean response scores by visual disturbance for the Quality of Vision questionnaire*. *(A) Frequency, (B) severity, (C) degree of bother, graded on a 0–3 ordinal scale, lower being better. |
There was no evidence of any intralenticular opacification in any of the eyes, and no evidence of iris chafing/depigmentation. There were no adverse events at the time of surgery or at any of the postoperative visits. There were no reports of dysphotopsia. No subject that underwent a combined primary/EDOF lens surgery requested removal of the EDOF lens.
Discussion
The results presented here are the first clinical and visual outcomes to be reported after implantation of the AddOn EDOF sulcus IOL. They demonstrate that the lens exceeded the AAO consensus criteria for EDOF lenses that were tested in the study. Ninety-one percent of eyes had a monocular DCIVA of better than or equal to 0.2 logMAR (20/32), compared to the suggested 50% in the consensus document. The change in mean CDVA of eyes with a monofocal IOL which were then implanted with the EDOF lens was about 0.04 logMAR, less than the 0.1 maximum suggested in the consensus document. The depth of focus calculated using the consensus document recommendation was 2.0 D.
The physiological performance of the lens in the sulcus was consistent with results reported previously for other versions of the lens (monofocal, monofocal toric, multifocal).9,11,19 Interlenticular opacification, deposits and iris depigmentation, potential issues with a secondary IOL, were not observed. Results here appear as good or better than reported for an aggregate data set of several different sulcus lenses.22
The distance visual acuity results for this study appear consistent with those reported for several primary EDOF lenses (near 0.0 logMAR distance-corrected and between 0.0 and 0.1 logMAR uncorrected).23–25 In all cases, the range of vision achieved by subjects in the current study was greater than reported for these other IOLs. The defocus curve appears as good or better than an aggregate curve derived from multiple EDOF studies, indicating that the range of focus achieved with this EDOF lens is consistent with those achieved with primary EDOF IOLs.26 It is important when making comparisons to remember that different studies will have different inclusion/exclusion criteria, testing procedures and subject populations.
The reported quality of vision was very good, with low levels of visual disturbances. Results appear slightly better than those recently reported (using the same questionnaire and reporting methodology) for a primary EDOF lens with a wavefront shaping technology incorporated.27,28 They also appear better than reported for a diffractive EDOF lens with a different design, again using the same questionnaire and reporting methodology.29
There are limitations to the current study. There was no control group, though in one calculation the subjects served as their own controls. The number of subjects/eyes was relatively low. The scope of the study was limited, so the AAO criteria evaluated with reference to EDOF lenses were not the complete set recommended in the consensus document.21 Specific testing methodologies also varied slightly from those suggested. Additional testing such as aberrometry and contrast sensitivity was not performed.
In summary, the secondary sulcus EDOF IOL investigated here provided excellent distance and intermediate vision, and good near vision to subjects, with a range of vision (VA better than or equal to 0.2 logMAR) of around 2 D. Subjective reported near visual function was also very good, and visual disturbances were limited. This lens appears to be a good option for pseudophakic patients who had a monofocal IOL previously implanted and who would like to improve their range of vision, or for those who would like an extended range of vision with the potential to reverse the procedure if visual disturbances are problematic. Clinical results appear as good or better than those achieved with a primary EDOF IOL.
Acknowledgment
Steffen Østenstad, MSc, of iFocus Øyeklinikk AS assisted with diagnostic testing and data collection/checking. Bjørn Gjerdrum, PhD, of iFocus Øyeklinikk AS provided editorial assistance.
Funding
This work was supported by an investigator-initiated study grant funded by 1stQ.
Disclosure
Dr. Gundersen is a consultant to Alcon, Staar, Santen, Centricity, and Glaukos. Dr Potvin reports grants from 1stQ Gmbh, during the conduct of the study; personal fees from Alcon, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Donoso R, Rodríguez A. Piggyback implantation using the AMO array multifocal intraocular lens. J Cataract Refract Surg. 2001;27(9):1506–1510. PMID: 11566539. doi:10.1016/s0886-3350(01)00862-8
2. Gerten G, Kermani O, Schmiedt K, Farvili E, Foerster A, Oberheide U. Dual intraocular lens implantation: monofocal lens in the bag and additional diffractive multifocal lens in the sulcus. J Cataract Refract Surg. 2009;35(12):2136–2143. PMID: 19969220. doi:10.1016/j.jcrs.2009.07.014
3. Gayton JL, Apple DJ, Peng Q, et al. Interlenticular opacification: clinicopathological correlation of a complication of posterior chamber piggyback intraocular lenses. J Cataract Refract Surg. 2000;26(3):330–336. PMID: 10713224. doi:10.1016/s0886-3350(99)00433-2
4. Chang SH, Lim G. Secondary pigmentary glaucoma associated with piggyback intraocular lens implantation. J Cataract Refract Surg. 2004;30(10):2219–2222. PMID: 15474839. doi:10.1016/j.jcrs.2004.03.034
5. Iwase T, Tanaka N. Elevated intraocular pressure in secondary piggyback intraocular lens implantation. J Cataract Refract Surg. 2005;31(9):1821–1823. PMID: 16246790. doi:10.1016/j.jcrs.2005.06.034
6. Vounotrypidis E, Schuster I, Mackert MJ, Kook D, Priglinger S, Wolf A. Secondary intraocular lens implantation: a large retrospective analysis. Graefes Arch Clin Exp Ophthalmol. 2019;257(1):125–134. doi:10.1007/s00417-018-4178-3
7. Hassan AH, Sayed KM, ElAgooz M, Elhawary AM. Refractive results: safety and efficacy of secondary piggyback Sensar™ AR40 intraocular lens implantation to correct pseudophakic refractive error. J Ophthalmol. 2016;2016:4505812. PMID: 27313869; PMCID: PMC4904093. doi:10.1155/2016/4505812
8. Karjou Z, Jafarinasab MR, Seifi MH, Hassanpour K, Kheiri B. Secondary piggyback intraocular lens for management of residual ametropia after cataract surgery. J Ophthalmic Vis Res. 2021;16(1):12–20. PMID: 33520123; PMCID: PMC7841270. doi:10.18502/jovr.v16i1.8244
9. Gundersen KG, Potvin R. A review of results after implantation of a secondary intraocular lens to correct residual refractive error after cataract surgery. Clin Ophthalmol. 2017;11:1791–1796. PMID:29042749; PMCID: PMC5633306. doi:10.2147/OPTH.S144675
10. Ferreira TB, Pinheiro J. Clinical results with a supplementary toric intraocular lens for the correction of astigmatism in pseudophakic patients. Eur J Ophthalmol. 2015;25(4):302–308. PMID: 25633616. doi:10.5301/ejo.5000564
11. Gundersen KG, Potvin R. Refractive and visual outcomes after implantation of a secondary toric sulcus intraocular lens. Clin Ophthalmol. 2020;14:1337–1342. PMID: 32546940; PMCID: PMC7244900. doi:10.2147/OPTH.S255725
12. McLintock CA, McKelvie J, Gatzioufas Z, Wilson JJ, Stephensen DC, Apel AJG. Outcomes of toric supplementary intraocular lenses for residual astigmatic refractive error in pseudophakic eyes. Int Ophthalmol. 2019;39(9):1965–1972. PMID: 30374760. doi:10.1007/s10792-018-1027-7
13. McLintock CA, McKelvie J, Niyazmand H, Apel AJ. Outcomes of a toric monofocal piggyback intraocular lens for residual astigmatic refractive error in pseudophakic eyes. Curr Eye Res. 2021:1–7. PMID: 34906017. doi:10.1080/02713683.2021.2007534
14. Cassagne M, Porterie M, Gauthier L, et al. Primary sulcus implantation of a diffractive multifocal pseudophakic piggyback intraocular lens. J Cataract Refract Surg. 2018;44(3):266–273. doi:10.1016/j.jcrs.2017.11.019
15. Schrecker J, Langenbucher A. Visual performance in the long term with secondary add-on versus primary capsular bag multifocal intraocular lenses. J Refract Surg. 2016;32(11):742–747. PMID: 27824377. doi:10.3928/1081597X-20160630-02
16. Liekfeld A, Ehmer A, Schröter U. Visual function and reading speed after bilateral implantation of 2 types of diffractive multifocal intraocular lenses: add-on versus capsular bag design. J Cataract Refract Surg. 2015;41(10):2107–2114. PMID: 26703286. doi:10.1016/j.jcrs.2015.10.055
17. Pedrotti E, Chierego C, Talli PM, et al. Extended depth of focus versus monofocal IOLs: objective and subjective visual outcomes. J Refract Surg. 2020;36(4):214–222. PMID: 32267951. doi:10.3928/1081597X-20200212-01
18. Rodov L, Reitblat O, Levy A, Assia EI, Kleinmann G. Visual outcomes and patient satisfaction for trifocal, extended depth of focus and monofocal intraocular lenses. J Refract Surg. 2019;35(7):434–440. PMID: 31298723. doi:10.3928/1081597X-20190618-01
19. Albayrak S, Comba ÖB, Karakaya M. Visual performance and patient satisfaction following the implantation of a novel trifocal supplementary intraocular lens. Eur J Ophthalmol. 2021;31(5):2346–2352. PMID: 33158370. doi:10.1177/1120672120969042
20. McAlinden C, Pesudovs K, Moore JE. The development of an instrument to measure quality of vision: the Quality of Vision (QoV) questionnaire. Invest Ophthalmol Vis Sci. 2010;51(11):5537–5545. doi:10.1167/iovs.10-5341
21. MacRae S, Holladay JT, Glasser A, et al. Special report: American Academy of Ophthalmology task force consensus statement for extended depth of focus intraocular lenses. Ophthalmology. 2017;124(1):139–141. PMID: 27743644. doi:10.1016/j.ophtha.2016.09.039
22. Rocha-de-Lossada C, Zamorano-Martín F, Piñero DP, Rodríguez-Vallejo M, Fernández J. Systematic review of the use of supplemental multifocal intraocular lenses in the ciliary sulcus for presbyopia correction. J Refract Surg. 2021;37(12):830–835. PMID: 34914553. doi:10.3928/1081597X-20210920-01
23. Ang RE, Picache GCS, Rivera MCR, Lopez LRL, Cruz EM. A comparative evaluation of visual, refractive, and patient-reported outcomes of three Extended Depth of Focus (EDOF) intraocular lenses. Clin Ophthalmol. 2020;14:2339–2351. PMID: 32921975; PMCID: PMC7457879. doi:10.2147/OPTH.S255285
24. Reinhard T, Maier P, Böhringer D, et al. Comparison of two extended depth of focus intraocular lenses with a monofocal lens: a multi-centre randomised trial. Graefes Arch Clin Exp Ophthalmol. 2021;259(2):431–442. PMID: 32915276; PMCID: PMC7843553. doi:10.1007/s00417-020-04868-5
25. Spadea L, Giannico MI, Formisano M, Alisi L. Visual performances of a new extended depth-of-focus intraocular lens with a refractive design: a prospective study after bilateral implantation. Ther Clin Risk Manag. 2021;17:727–738. PMID: 34295162; PMCID: PMC8291859. doi:10.2147/TCRM.S320422
26. Liu J, Dong Y, Wang Y. Efficacy and safety of extended depth of focus intraocular lenses in cataract surgery: a systematic review and meta-analysis. BMC Ophthalmol. 2019;19(1):198. PMID: 31477053; PMCID: PMC6719364. doi:10.1186/s12886-019-1204-0
27. Arrigo A, Gambaro G, Fasce F, Aragona E, Figini I, Bandello F. Extended depth-of-focus (EDOF) AcrySof® IQ Vivity® intraocular lens implant: a real-life experience. Graefes Arch Clin Exp Ophthalmol. 2021;259(9):2717–2722. PMID: 34050809. doi:10.1007/s00417-021-05245-6
28. Gundersen KG, Potvin R. Clinical outcomes and quality of vision associated with bilateral implantation of a wavefront shaping presbyopia correcting intraocular lens. Clin Ophthalmol. 2021;15:4723–4730. PMID: 34983995; PMCID: PMC8699763. doi:10.2147/OPTH.S342947
29. Monaco G, Gari M, Di Censo F, Poscia A, Ruggi G, Scialdone A. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43(6):737–747. PMID: 28732606. doi:10.1016/j.jcrs.2017.03.037
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Efficacy of a Secondary Trifocal Sulcus IOL in Providing Near and Intermediate Vision in Patients with Prior Myopic Laser Vision Correction and Cataract Surgery
Gundersen KG, Gjerdrum B, Potvin R
Clinical Ophthalmology 2022, 16:2219-2226
Published Date: 8 July 2022
