Back to Journals » Clinical and Experimental Gastroenterology » Volume 9
Rectal budesonide and mesalamine formulations in active ulcerative proctosigmoiditis: efficacy, tolerance, and treatment approach
Authors Christophi G, Rengarajan A, Ciorba M
Received 1 October 2015
Accepted for publication 31 March 2016
Published 19 May 2016 Volume 2016:9 Pages 125—130
DOI https://doi.org/10.2147/CEG.S80237
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Andreas M. Kaiser
George P Christophi, Arvind Rengarajan, Matthew A Ciorba
Division of Gastroenterology, Washington University School of Medicine, St. Louis, MO, USA
Abstract: Ulcerative colitis (UC) is an immune-mediated disease of the colon that is characterized by diffuse and continuous inflammation contiguous from the rectum. Half of UC patients have inflammation limited to the distal colon (proctitis or proctosigmoiditis) that primarily causes symptoms of bloody diarrhea and urgency. Mild-to-moderate distal UC can be effectively treated with topical formulations (rectal suppositories, enemas, or foam) of mesalamine or steroids to reduce mucosal inflammation and alleviate symptoms. Enemas or foam formulations adequately reach up to the splenic flexure, have a minimal side-effect profile, and induce remission alone or in combination with systemic immunosuppressive therapy. Herein, we compare the efficacy, cost, patient tolerance, and side-effect profiles of steroid and mesalamine rectal formulations in distal UC. Patients with distal mild-to-moderate UC have a remission rate of approximately 75% (NNT =2) after treatment for 6 weeks with mesalamine enemas. Rectal budesonide foam induces remission in 41.2% of patients with mild-to-moderate active distal UC compared to 24% of patient treated with placebo (NNT =5). However, rectal budesonide has better patient tolerance profile compared to enema formulations. Despite its favorable efficacy, safety, and cost profiles, patients and physicians significantly underuse topical treatments for treating distal colitis. This necessitates improved patient education and physician familiarity regarding the indications, effectiveness, and potential financial and tolerability barriers in using rectal formulations.
Keywords: inflammatory bowel disease, treatment cost effectiveness, Crohn’s disease, ulcerative colitis, colon mucosa, proctitis suppositories, topical immunosuppressive therapy
Introduction
Inflammatory bowel disease (IBD) is a chronic immune-mediated disease of the gastrointestinal tract that affects more that 1.6 million Americans.1,2 Ulcerative colitis (UC) is characterized by diffuse, continuous, superficial, and ulcerating inflammation confined to the colon that causes rectal bleeding, diarrhea, and abdominal pain. The current working model of IBD pathogenesis posits a dysregulated immune response against gut microbiota in the presence of genetic defects, leading to exaggerated self-injurious inflammatory responses. Genome-wide association studies have identified IBD susceptibility genes, the majority of which are immunoregulatory.3,4 UC can have varied distribution and severity. Ulcerative proctitis (UP) and ulcerative proctosigmoiditis (UPS), defined as disease extending 15 and 40 cm from the anal verge, respectively, are seen in approximately 50% of UC patients.5 Left-sided colitis, seen in around 30% of UC patients, involves continues inflammation from the anus to the splenic flexure, and only 20% of UC patients have extensive colitis or pancolitis.6
The mainstay therapy for IBD involves anti-inflammatory immunosuppression dictated by the severity and location of disease. Moderate-to-severe disease is typically treated with immunosuppressive medications such as azathioprine, anti-TNF, and more recently, anti-integrin agents.7 Oral corticosteroids are limited to treating acute flares and have limited efficacy in maintaining remission.8 Rectally administered therapies can be effective in distal colitis and include suppositories for proctitis or enemas and foam preparations for proctosigmoiditis and left-sided colitis. However, because of lack of knowledge and familiarity regarding efficacy, safety, and patient tolerance, topical therapies are often underused in UC patients. The Swiss Inflammatory Bowel Disease Cohort study reports that only 26% of patients with mild-to-moderate proctitis were treated with topical therapy and only 13% of patients with active extensive colitis received treatment that included topical rectal therapy.9
Herein, we provide an updated literature review of the effectiveness, safety, tolerability, and cost of topical treatments for distal inflammatory colitis. We compare different formulations of topical therapies (ie, suppositories, enemas, and rectal foam) with a particular focus on how budesonide, a specific corticosteroid, compares to other treatments. Importantly, we provide a framework and treatment algorithm for distal UC.
Available topical therapies for distal colitis
Common therapies for the treatment of UP and UPS include 5-aminosalicylic acid (5-ASA) and steroids. Mesalamine and other 5-ASA substances are the first-line choice in treating mild-to-moderate UC, regardless of the physical extent of disease. Mesalamine has multiple reported anti-inflammatory effects that include inhibiting leukotriene and IL-1 production, impairing TNFα and NF-κB transcription signaling and having antioxidant properties by acting as a free-radical scavenger.10 Additionally, mesalamine reduces mucosal inflammation by acting on mucosal colonic epithelial cells and infiltrating leukocytes, with its clinical efficacy therefore correlating with its local concentration in the gut.
Oral mesalamine is effective and can induce remission in active UC; however, delivery of the active agent to the inflamed distal colon is limited. Intolerance to the sulfapyridine moiety of sulfasalazine is fairly common and may result in nausea, vomiting, dyspepsia, anorexia, and headache. More severe but less common adverse effects for sulfasalazine and melamine oral formulations include allergic reactions, pancreatitis, hepatotoxicity, drug-induced connective tissue disease, bone marrow suppression, interstitial nephritis, and hemolytic anemia or megaloblastic anemia.11 In a multicenter, double-blind study, patients with mild-to-moderate active UC were randomized to either oral mesalamine or placebo and were followed at 3- and 6-week time points. At 3 weeks, remission rates (defined by improved stool frequency, rectal bleeding, and sigmoidoscopic findings) were 32% for patients treated with 2.4 g/d of mesalamine vs 9% in the placebo arm, and at 6 weeks, efficacy increased to 49% vs 23%, respectively.12 However, in mild-to-moderate UP and UPS, topically administered 5-ASA (ie, suppository, enema, or rectal foam preparations) can be more efficacious both at generating a response and inducing remission than oral 5-ASA. A randomized, double-blinded trial demonstrated endoscopic remission and decreased rectal bleeding in patients with mild-to-moderate UC with rectal inflammation after a 4-week treatment period with 1 g mesalazine suppository once daily as compared to placebo (81.5% vs 29.7%, P<0.0001).13 However, suppositories rarely extend beyond 10–15 cm from the rectum, making them less attractive as a rectal formulation. A meta-analysis comparing rectal 5-ASA to placebo in patients with distal UC demonstrated that rectal 5-ASA was superior to placebo for inducing symptomatic remission (OR: 8.3, 95% CI: 4.3–16.1) and endoscopic remission (OR: 5.3, 95% CI: 3.2–8.9).14
Practice guidelines recommend using topical mesalamine agents as first line compared to topical steroids or oral aminosalicylates for the treatment of distal mild-to-moderate UC, and the combination of oral and topical aminosalicylates is more effective than either alone. 15 In addition, practice guidelines recommend mesalamine suppositories or enemas as the preferred agents to maintain remission in distal mild-to-moderate UC. Mesalamine suppositories maintain remission in 90% of patients with mild-to-moderate UP at 1 year, while mesalamine enemas maintain remission in 72% of patients with mild-to-moderate UPS when administered every other day at 1 year.16,17
Topical steroids are an alternative treatment for distal colitis, particularly if patients fail or do not tolerate 5-ASA therapy. They have long-ranging anti-inflammatory effects through various mechanisms, including expression of anti-inflammatory cytokine IL-10, inhibition of histone acetylation and immune cell apoptosis, and reduced signaling of inflammatory transcription factors such as NF-kB and AP-1. Oral corticosteroids are efficacious in controlling acute colitis flares, but 16% of patients show no response and 30% show only a partial response.8 Moreover, oral steroid use can have numerous side effects, spanning multiple organ systems: acne, moon facies, infection, hypertension, and hirsutism being among the most common. Notable effects from long-term corticosteroid use are hypertension, diabetes, adrenal insufficiency, osteoporosis, and psychosis.18 Given the side-effect profile, oral steroid therapy is limited to short-treatment intervals in patients with moderate-to-severe disease rather than long-term maintenance.16 Rectally applied steroids offer advantages as compared to orally administered drugs because they offer a more targeted treatment to the areas of active inflammation and generally have fewer systemic effects than oral corticosteroid use.19,20 Budesonide is a lipophilic agent with lower systemic bioavailability, which can potentially cause lower systemic side effects.
Efficacy of budesonide rectal foam
Budesonide, a high-potency, nonhalogenated, second-generation corticosteroid, can be used either topically or orally in patients with UC. The pharmacokinetic profile of budesonide rectal foam, specifically the extent of spread and length of persistence in the colon, make it an efficacious topical treatment. Using [99Tcm]-labeled budesonide foam in patients with moderate proctosigmoiditis or left-sided colitis, Brunner et al21 determined that budesonide spread 25.4±10.3 cm, reached the sigmoid colon in all patients, and had a mean colonic residence time of 5.3 hours. Sandborn et al19 compared rectal budesonide foam to placebo in two randomized, double-blind, side-by-side trials utilizing 546 patients with mild-to-moderate UP or UPS. All patients had disease extending at least 5 cm, but no >40 cm from the anal verge. The budesonide treatment arm received 2 mg/mL two times daily (BID) dosing of the foam for 2 weeks and then was switched to once daily dosing for 4 weeks. The primary end point was remission, defined by Mayo Score ≤1, no rectal bleeding, and either no change or an improvement in stool frequency. A combined 41.2% of patients demonstrated remission as compared to 24% of the placebo patients (P<0.0001). Interestingly, in subgroup analysis, budesonide rectal foam was still superior to placebo regardless of concurrent use of <4.8 g/d of oral mesalamine, suggesting that budesonide foam can have additive treatment effects in patients already receiving oral mesalamine treatment.
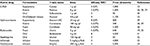
Comparison of budesonide with other corticosteroid rectal foam therapies, however, did not demonstrate increase in efficacy (Table 1). Bar-Meir et al20 investigated the differences between budesonide and hydrocortisone administration as rectal foam. This randomized, parallel-group, multicenter clinical trial included 251 patients with active mild-to-moderate UPS and demonstrated similar efficacy (remission rates of approximately 50%) following a 6-week treatment period with either steroid rectal foam. Thus, for patients with distal UC, hydrocortisone or budesonide rectal foam can be an efficacious therapeutic choice.
Patient safety, tolerance, and use of budesonide rectal foam
Multiple studies have shown that budesonide foam is safe for administration in UP and UPS, with minimal adverse effects and rare serious adverse effects. These adverse events are thought to be secondary to intestinal absorption of budesonide.21 The most common adverse effects include headache, nausea, decreased serum cortisol levels, and abdominal pain.18 In the randomized, side-by-side trial by Sandborn et al,19 serious adverse events occurred in 1%–2% of patients, rates that were not significantly higher than placebo and had no clear association with budesonide. Budesonide can cause transient decrease in cortisol levels in 16% of patients when administered as a BID dosing for 2 weeks. However, by the end of the 6-week trial, 94.2% of all patients in the budesonide treatment arm had normal cortisol levels. Altogether, the data support the fact that budesonide rectal foam is a safe treatment with minimal adverse events associated with its use.
Rectal foam formulations have been designed to provide a more uniform delivery to the left colon and to optimize retention. One advantage in using foam as opposed to enemas is the sheer volume of therapy (20–25 mL for foam vs 60–100 mL for enema). Because of the higher volume, urgency and abdominal/rectal discomfort tend to be more associated with enemas. A recent double-blind, double-dummy randomized trial by Gross et al22 compared remission rates and overall patient tolerability/satisfaction between budesonide enemas vs foam in the treatment of active UP or UPS. The study highlighted that though the overall remission rates were similar between the two treatment modalities (66% for enema vs 60% for foam), there was an overwhelming preference for the foam formulation (84%). This disparity in patient preference/satisfaction was due in part to higher rates of retention while using enemas as opposed to foam (39% compared to 11%, respectively), more unpleasant feelings (36% compared to 12%, respectively), and more rectal pain (18% compared to 10%, respectively).
Instructions to patients should include the importance of emptying bowels before administering the rectal foam and stress lubrication of the applicator. Patients should be advised to warm the canister in their hands while shaking it vigorously for 10–15 seconds prior to use and that application of the rectal foam can be done while in a standing, lying, or sitting position. Additionally, application of rectal foam should be performed in the morning and before bed the first 2 weeks of treatment, and then once daily in the evening for the next 4 weeks. Budesonide is metabolized via CYP3A4, and therefore, patients should be advised to avoid ketoconazole or grapefruit juice during treatment to prevent increased exposure.
Available formulations and cost of topical therapies
Both ASA and steroids come in different formulations, including suppositories, enemas, and more recently, foams. Efficacies and costs of these various formulations are summarized in Table 1. The extent and severity of UC and treatment response and duration among different study patient populations varied; therefore, direct comparisons of efficacy and overall health care cost among the different medications have to be done in relative terms. The extent and severity of the colonic inflammation dictates the formulation of topical therapy. Suppositories are more commonly used in mild-to-moderate cases of proctitis, while enemas and foams are typically used in more extensive disease, such as proctosigmoiditis and left-sided colitis. Immunomodulator treatment is often used in moderate-to-severe UC or mild-to-moderate disease that had minimal response to mesalamine formulations. Topical therapy in combination with immunomodulatory treatment provided further symptoms control in patients with active distal colitis.15
In the United States, the price of topical, oral, and parenteral biologic therapy for IBD varies and ranges from <$100 per month for sulfasalazine and azathioprine to several thousand dollars for biologic therapy (Table 2). Budesonide rectal foam is sold in kits that contain a canister of 33.4 g and applicators that deliver 14 2 mg doses. A 6-week course of budesonide foam is generally recommended to induce remission, with twice-daily dosing for the first 2 weeks, followed by once-a-day dosing for the remaining 4 weeks. Each of the budesonide foam kits costs approximately $320, making the recommended 6 week course cost $1,280. Mesalamine suppositories and enemas despite being on the market for decades cost $1,000–$1,600 per month when used once daily. Furthermore, an 80 kg person receiving 5 mg/kg of infliximab generates a drug cost of almost $47,000 in the first year of treatment.23 Similarly, vedolizumab, a gut-selective blockade of lymphocyte trafficking, is administered in 300 mg infusions every 8 weeks and a loading dose24. One 300 mg vedolizumab infusion costs $5,800, and the treatment during the first year costs $49,000.
Conclusion
Approximately half of patients with UC have distal colitis, causing symptoms of bloody diarrhea, tenesmus, and rectal pain. Despite the favorable efficacy, safety, and cost profile of topical treatments, only one in four patients with mild-to-moderate distal colitis is prescribed topical therapy. In mild-to-moderate UP or UPS, topical therapy with 5-ASA is recommended as a first-line agent and is cost-effective over other treatment options. Overall, mesalamine enemas can induce clinical and endoscopic remission in three out of four patients with minimal side effects. Advantages of topical therapy include a quicker response time and less frequent dosing schedule than oral therapy, as well as less systemic absorption. The choice of topical therapy is primarily guided by patient preference as well as by the proximal extent of disease. Some patients may achieve maximum benefit from combination of oral and topical therapy achieving clinical improvement, as well as an earlier response than either agent alone.25
Previous studies demonstrated that topical corticosteroids, whether hydrocortisone or budesonide, have not proven effective for maintaining remission in distal colitis.26,27 Recently, Sandborn et al19 demonstrated that rectal budesonide foam is effective at inducing remission in mild-to-moderate active UP or UPS and has better patient tolerability/satisfaction compared to enema formulations. Furthermore, in patients with incomplete response to topical or oral mesalamine, budesonide foam could be used in conjunction to induce remission. Alternatively, budesonide foam can be used as an adjunctive agent during acute flares in patients with distal colitis. Overall, it is important for physicians to understand and in turn educate patients about the effectiveness, safety, cost, and tolerability of topical therapies in active distal UC.
Acknowledgment
Dr Christophi is partially funded by the NIH grant DK007130.
Disclosure
The authors report no conflicts of interests in this work.
References
Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2066–2078. | ||
Malik TA. Inflammatory bowel disease: historical perspective, epidemiology, and risk factors. Surg Clin North Am. 2015;95:1105–1122. | ||
Christophi GP, Rong R, Holtzapple PG, Massa PT, Landas SK. Immune markers and differential signaling networks in ulcerative colitis and Crohn’s disease. Inflamm Bowel Dis. 2012;18:2342–2356. | ||
Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011;474:307–317. | ||
Rogler G. Medical management of ulcerative colitis. Dig Dis. 2009;27:542–549. | ||
Frei P, Biedermann L, Manser CN, et al. Topical therapies in inflammatory bowel disease. Digestion. 2012;86(Suppl 1):36–44. | ||
Danese S, Vuitton L, Peyrin-Biroulet L. Biologic agents for IBD: practical insights. Nat Rev Gastroenterol Hepatol. 2015;12:537–545. | ||
Faubion WA Jr, Loftus EV Jr, Harmsen WS, Zinsmeister AR, Sandborn WJ. The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology. 2001;121:255–260. | ||
Seibold F, Fournier N, Beglinger C, Mottet C, Pittet V, Rogler G. Topical therapy is underused in patients with ulcerative colitis. J Crohns Colitis. 2014;8:56–63. | ||
Gross V. Topical therapy. Dig Dis. 2012;30(Suppl 3):92–99. | ||
Ham M, Moss AC. Mesalamine in the treatment and maintenance of remission of ulcerative colitis. Expert Rev Clin Pharmacol. 2012;5:113–123. | ||
Sninsky CA, Cort DH, Shanahan F, et al. Oral mesalamine (Asacol) for mildly to moderately active ulcerative colitis. A multicenter study. Ann Intern Med. 1991;115:350–355. | ||
Watanabe M, Nishino H, Sameshima Y, Ota A, Nakamura S, Hibi T. Randomised clinical trial: evaluation of the efficacy of mesalazine (mesalamine) suppositories in patients with ulcerative colitis and active rectal inflammation – a placebo-controlled study. Aliment Pharmacol Ther. 2013;38:264–273. | ||
Marshall JK, Irvine EJ. Rectal aminosalicylate therapy for distal ulcerative colitis: a meta-analysis. Aliment Pharmacol Ther. 1995;9:293–300. | ||
Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105:501–523; quiz 524. | ||
Hanauer S, Good LI, Goodman MW, et al. Long-term use of mesalamine (Rowasa) suppositories in remission maintenance of ulcerative proctitis. Am J Gastroenterol. 2000;95:1749–1754. | ||
Kruis W, Schreiber S, Theuer D, et al. Low dose balsalazide (1.5 g twice daily) and mesalazine (0.5 g three times daily) maintained remission of ulcerative colitis but high dose balsalazide (3.0 g twice daily) was superior in preventing relapses. Gut. 2001;49:783–789. | ||
Kusunoki M, Moeslein G, Shoji Y, et al. Steroid complications in patients with ulcerative colitis. Dis Colon Rectum. 1992;35:1003–1009. | ||
Sandborn WJ, Bosworth B, Zakko S, et al. Budesonide foam induces remission in patients with mild to moderate ulcerative proctitis and ulcerative proctosigmoiditis. Gastroenterology. 2015;148:740–750. e2. | ||
Bar-Meir S, Fidder HH, Faszczyk M, et al. Budesonide foam vs. hydrocortisone acetate foam in the treatment of active ulcerative proctosigmoiditis. Dis Colon Rectum. 2003;46:929–936. | ||
Brunner M, Vogelsang H, Greinwald R, et al. Colonic spread and serum pharmacokinetics of budesonide foam in patients with mildly to moderately active ulcerative colitis. Aliment Pharmacol Ther. 2005;22:463–470. | ||
Gross V, Bar-Meir S, Lavy A, et al. Budesonide foam versus budesonide enema in active ulcerative proctitis and proctosigmoiditis. Aliment Pharmacol Ther. 2006;23:303–312. | ||
Christophi GP, Ciorba MA. Lower dose infliximab for ulcerative colitis: How low can we go and how much can be saved? J Clin Gastroenterol. 2015;49:539–540. | ||
Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369:699–710. | ||
Safdi M, DeMicco M, Sninsky C, et al. A double-blind comparison of oral versus rectal mesalamine versus combination therapy in the treatment of distal ulcerative colitis. Am J Gastroenterol. 1997;92:1867–1871. | ||
Cohen RD, Woseth DM, Thisted RA, Hanauer SB. A meta-analysis and overview of the literature on treatment options for left-sided ulcerative colitis and ulcerative proctitis. Am J Gastroenterol. 2000;95:1263–1276. | ||
Regueiro M, Loftus EV Jr, Steinhart AH, Cohen RD. Medical management of left-sided ulcerative colitis and ulcerative proctitis: critical evaluation of therapeutic trials. Inflamm Bowel Dis. 2006;12:979–994. | ||
Hartmann F, Stein J. Clinical trial: controlled, open, randomized multicentre study comparing the effects of treatment on quality of life, safety and efficacy of budesonide or mesalazine enemas in active left-sided ulcerative colitis. Aliment Pharmacol Ther. 2010;32:368–376. | ||
Marshall JK, Irvine EJ. Rectal corticosteroids versus alternative treatments in ulcerative colitis: a meta-analysis. Gut. 1997;40:775–781. | ||
Dick AP, Grayson MJ, Carpenter RG, Petrie A. Controlled trial of sulphasalazine in the treatment of ulcerative colitis. Gut. 1964;5:437–442. | ||
Sherlock ME, Seow CH, Steinhart AH, Griffiths AM. Oral budesonide for induction of remission in ulcerative colitis. Cochrane Database Syst Rev. 2010:CD007698. | ||
Chebli LA, Chaves LD, Pimentel FF, et al. Azathioprine maintains long-term steroid-free remission through 3 years in patients with steroid-dependent ulcerative colitis. Inflamm Bowel Dis. 2009;16:613–619. | ||
Rutgeerts P, Sandborn WJ, Feagan BG, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462–2476. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.