Back to Journals » Psychology Research and Behavior Management » Volume 12
Reconceptualizing attrition in Parent–Child Interaction Therapy: “dropouts” demonstrate impressive improvements
Authors Lieneman CC , Quetsch LB, Theodorou LL, Newton KA , McNeil CB
Received 4 March 2019
Accepted for publication 7 May 2019
Published 22 July 2019 Volume 2019:12 Pages 543—555
DOI https://doi.org/10.2147/PRBM.S207370
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Einar Thorsteinsson
Video abstract presented by Corey C. Lieneman.
Views: 27347
Corey C Lieneman,1 Lauren B Quetsch1,2, Laurie L Theodorou,3 Kathleen A Newton,3 Cheryl B McNeil1
1Department of Psychology, West Virginia University, Morgantown, WV, USA; 2Department of Psychiatry, University of Arkansas for Medical Sciences, Little Rock, AR, USA; 3Oregon Health Authority, Salem, OR, USA
Purpose: Behavior disorders in early childhood are linked to a variety of negative outcomes for both children and families. Parent–Child Interaction Therapy (PCIT), an evidence-based parent-training program, demonstrates large effect sizes in reducing child problem behavior for dyads who complete treatment; however, a high number of families seeking treatment in community-based settings terminate from PCIT prior to meeting the protocol’s strict graduation criteria. The purpose of this study was to examine the impact of PCIT on child behavior problems for families who received at least a small dose of PCIT but not enough to meet the strict mastery criteria required for graduation.
Patients and methods: This study employed one of the largest community research samples conducted with PCIT (2,787 children and their families across the state of Oregon, 1,318 with usable data) to determine how PCIT impacts both graduates and early terminators.
Results: While families who graduated from PCIT (17.7% of the sample) demonstrated a very large effect size in problem behavior intensity improvements (d=1.65), families who terminated treatment early, but after attending at least four treatment sessions (51.7% of the sample), still showed significant improvements in behavior problems with a medium-to-large effect size (d=0.70). In contrast, very early terminators (those attending fewer than four treatment sessions, 0.3% of the sample), demonstrated little improvement at the time of dropout from services (d=0.12).
Conclusion: Though early terminators in PCIT have previously been identified as treatment failures, the present study discusses the reconceptualization of “dropouts” in relation to some positive evidence of treatment outcomes, the implications for community-based service delivery, and possible future directions.
Keywords: PCIT, state-wide implementation, behavior disorders, community effectiveness
Introduction
If left untreated, behavior problems in early childhood are associated with a variety of immediate and long-term negative outcomes. For example, young children with behavior disorders are more likely to experience physical and emotional abuse, peer rejection, academic difficulties, and other mental health problems (eg, depression, anxiety).1–3 Later in life, those who suffered from behavior disorders in childhood are more likely to engage in physical violence, delinquency, and substance abuse,4–6 and to suffer from other mental health problems (eg, personality disorders, depression).7,8
Fortunately, participation in short-term behavioral parent training programs can reduce child behavior problems to sub-clinical thresholds. For example, a meta-analysis of one behavioral parent-training program, Parent–Child Interaction Therapy (PCIT), demonstrated very large effect sizes (Cohen’s d=1.65) in reducing problem behavior as measured by the Eyberg Child Behavior Inventory (ECBI).9 Cohen’s d is a standardized effect size used to signify the strength in differences between means and can be used to compare treatment efficacy across studies. In this case, Cohen’s d indicates the size of the difference between pre- and post-treatment ECBI Intensity Scale scores while taking into account the variability and size of the samples; the larger the effect size, the larger the improvements in child behavior (d=0.01, very small; 0.20, small; 0.50, medium; 0.80, large; 1.20, very large; 2.0, huge).10,11 For representative effect sizes from other mental health treatment modalities, see Table 1. Considering PCIT’s relatively short-term duration (12–20 weekly, 1 hour sessions), the outcomes are even more striking.
 |
Table 1 Effect size comparisons across treatment modalities |
Unfortunately, not all families who seek treatment are able to reach graduation. Concerns have been raised over the high attrition rate in community-based behavioral parent training programs. Studies of community-based PCIT have reported dropout rates ranging from 12–67%.12–14 These high rates of attrition are related to parenting stress levels15,16 and treatment barriers17,18 experienced by the populations served by PCIT. The typical PCIT caregiver is a single mother with young children and many barriers to treatment attendance that may cause the family to discontinue therapy before graduation, including childcare needs, transportation difficulties, and pregnancy.19,20 Graduation from PCIT requires that families satisfy strict criteria surrounding mastery of caregiver skills, confidence in handling child behavior, and specific subthreshold levels of child behavior problems. While graduation criteria are important in determining when maximum therapeutic benefits have been achieved, dichotomous classification of clients as either “graduates/completers” or “dropouts/early terminators” may be detrimental to our understanding of treatment outcomes. In this paper, families who discontinued treatment before meeting graduation criteria are described as “early terminators” to avoid stigma associated with the term “dropout” and to recognize that there are a variety of reasons families leave therapy. Because many families discontinue treatment before graduation but after some level of meaningful change (eg, caregiver skill acquisition, improvement in child behavior) has occurred, it is crucial to understand more about the benefits achieved by families who terminate treatment early.
In summary, PCIT is a powerful intervention for families who complete the service, but a large proportion of families who seek treatment only receive part of the intervention. The purpose of this study was to examine the impact of PCIT on child behavior problems for families who received at least a small dose of PCIT but not enough to meet the strict mastery criteria required for graduation. Along these lines, researchers investigated how treatment outcomes for PCIT graduates and early terminators compared with those of other common interventions.
The present study evaluated the differences in child outcomes for graduates and early terminators in a state-wide implementation of PCIT in Oregon. The goals of the present study were to (1) understand correlations among key demographic and behavior change variables across this large community-based PCIT sample, (2) determine the amount of change in disruptive behavior intensity for children who received PCIT across the state of Oregon within groups for both graduates and early terminators, (3) compare the amount of behavior change between groups experienced by those in the graduate versus early terminator group, and (4) provide information about the average amount of child behavior change associated with different lengths of treatment for both graduates and early terminators. It was hypothesized that families in both groups, graduates and early terminators, would experience significant decreases in problem behavior but that graduates would report significantly more behavior change than early terminators.
Methods
Participants
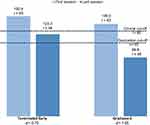
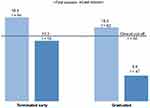
This study examined one of the largest samples in the history of PCIT research, which included 2,787 caregiver–child dyads across the state of Oregon. Participating families were referred to community mental health agencies (rural=649; urban=2,138) for behavioral parent training using PCIT. See Figures 1 and 2 for data on level of caregiver-reported child behavior problems. Participants included one child of unknown gender, 1,776 male (63.7%) and 1,010 female (36.2%) children, ranging in age from 24–84 months (X̄=58.66 months, SD=14.75 months). The majority of participants identified as white/Caucasian (53.5%), while approximately 1.8% identified as American Indian or Alaska Native, 1.4% identified as black/African American, 0.9% identified as “other or more than one race," and 0.3% identified as Asian or Pacific Islander; the race of the remaining participants was unknown or missing (42.1%). Additionally, 53.4% of the population identified as non-Hispanic, and 14.2% identified as Hispanic; ethnicity data were not available for the remaining participants. Primary child mental health diagnoses as coded by each agency included: (1) attention-deficit/hyperactivity disorder (ADHD; 10.1%), (2) mood/anxiety disorder (9.2%), (3) disruptive behavior disorder (9.1%), (4) developmental disability (1.6%), (5) relational/attachment problem (1.2%), (6) unspecified/adjustment disorder (34.8%), and missing diagnosis (34.0%). Caregivers included 2,143 females (76.9%), 588 males (21.1%), and 56 individuals for whom gender was not reported (2.0%). Of these caregivers, 81.0% were biological parents, 5.7% were grandparents, 3.1% were step-parents or caregivers’ significant others, 1.4% were other family members, 0.9% were adoptive parents, 0.3% were other non-relatives (eg, foster parents), and 7.6% did not report or were missing this information.
Procedure
All families who sought PCIT services in participating agencies in the state of Oregon received PCIT as usual. A state-affiliated agency collected participant and treatment data as part of routine procedures. These data were reported by community-based clinicians as required by their agencies; clinicians were not specifically trained in research or data collection methods. As a result, large portions of data were missing (eg, demographics). Data were deidentified and stored in the state-affiliated agency’s database. After approval from the state agency and the primary researchers’ Institutional Review Board at West Virginia University, available data were analyzed and interpreted. All study procedures were post-hoc and observational in nature.
Parent–Child Interaction Therapy (PCIT)
PCIT is an evidence-based treatment for disruptive behavior problems in children, aged 2–7 years.21,22 Therapists observe sessions through a one-way mirror, providing caregivers with real-time feedback through a bug-in-the-ear system while they interact with their child. PCIT progresses through two phases, Child-Directed Interaction (CDI) and Parent-Directed Interaction (PDI), in which caregivers learn play therapy and operant conditioning skills through live coaching. Increased positivity and attachment security in caregiver–child relationships are the foci of CDI. During CDI, caregivers acquire skills around praise, verbal reflection, imitation, behavioral description, and enjoyment, otherwise known as “PRIDE” skills. In the second phase of treatment, PDI, focus shifts to improving child compliance and remaining behavior problems. PCIT has a large evidence base demonstrating impressive effect sizes in a wide variety of populations and contexts.23–26 Please see Parent–Child Interaction Therapy27 for a more detailed description of PCIT.
Measures
Demographics
Through routine reporting procedures required by a state-affiliated agency, community-based mental health clinics providing PCIT reported demographics including child age, gender, ethnicity, race, and primary language, as well as caregiver gender and relationship to the identified child. Clinics also provided the site names and counties where each family received PCIT. Clinics were identified as either urban (<10 miles from population centers of 40,000 or more), rural (>10 miles from population centers of 40,000 or more), or frontier (counties with fewer than six people per square mile) based on definitions provided by the Oregon Office of Rural Health.28
Number of sessions
The number of sessions attended by each family was recorded.
Graduation status
Participants who met mastery criteria outlined in the PCIT Protocol21 were considered to have “graduated” from the PCIT program (0=did not graduate, 1=graduated). These criteria include (1) mastery of CDI skills, (2) mastery of PDI skills, (3) ECBI Intensity Scale scores of child behavior problems at or below a raw score of 114 (ie, one-half standard deviation below the clinical cut-off), and (4) caregiver-reported confidence in managing child behavior.
Eyberg Child Behavior Inventory (ECBI)
The ECBI is a 36-item caregiver-report measure of child behavior problems rated for frequency (Intensity Scale) and whether the behaviors are experienced as problematic by the caregiver (Problem Scale).29 Each question on the Intensity Scale uses a 7-point Likert-type scale ranging from “never” to “always”, with higher scores indicating more intense behavior problems. The Problem Scale uses a dichotomous “yes” or “no” rating with higher total scores indicative of more problematic behaviors. The ECBI is normed for children aged 2–16 years and has demonstrated adequate reliability and validity.29,30 An ECBI Intensity Scale change score was created by subtracting the ECBI Intensity Scale score reported at the child’s last session from the ECBI Intensity Scale score reported at the child’s first session. Negative ECBI change scores indicated that the child’s behavior worsened from first to last session, while positive scores indicated improved behavior according to caregiver report. The ECBI Intensity Scale score was selected as the focus of several analyses over the ECBI Problem Scale score, due to (1) the Intensity Scale score being tracked on a weekly basis as part of the treatment protocol, and (2) the Intensity Scale score being an integral component of the mastery criteria for graduation from PCIT.
Results
ECBI Intensity Scale scores from both first and last sessions were necessary to create ECBI Intensity Scale change scores. Of the 2,787 caregiver-child dyads included in the study, participants missing one or both of these scores were excluded from analyses (825 families; 29.6% of the total sample). The graduation statuses for an additional 17 families (0.6% of the total sample) were unknown and, therefore, excluded from analyses. Finally, the number of sessions was missing for 627 families (22.5% of the total sample) who were excluded, for a total sample size of 1,318 children (47.3%).
Preliminary analyses
The number of sessions attended was negatively skewed. A square root transformation was performed to account for skewness in primary analyses. All assumptions of the proceeding analyses were met unless otherwise specified.
Correlations
For our first aim, bivariate correlations among gender, age, number of sessions, graduation status, ECBI Intensity Scale score change, and ECBI Problem Scale score change were analyzed. Younger children were more likely than older children to graduate from PCIT; however, this correlation accounted for less than 1% of the variance and is likely an artifact of our large sample size. Overall, those who attended more sessions were more likely to graduate and experience larger decreases in ECBI Intensity and Problem Scale scores than those who attended fewer sessions. Larger changes in ECBI Intensity Scale scores were also associated with graduating from treatment. All other correlations were non-significant (see Table 2).
 |
Table 2 Correlations and descriptive statistics for key study variables (N=914) |
Note on meaningful number of sessions
To estimate meaningful changes likely resulting from PCIT treatment, analyses below focus on data from families who attended four or more total sessions. It was assumed that the first one, two, or three sessions likely involved assessments and introduction to behavioral parenting skills (ie, CDI teach session). Following the CDI teach session, coaching sessions begin, providing families with live feedback and coaching of newly-learned skills. Therefore, session four (the point at which coaching probably commenced) was estimated to be the first possible time point at which any meaningful skill acquisition and resultant child behavior change could have been recorded. There were n=914 families (69.3% of the above sample of families with useable data) who attended at least four sessions. Of these remaining families, 681 (74.5%) terminated treatment early (before meeting PCIT graduation criteria), and 233 (25.5%) graduated from treatment. Within this sample of families who attended at least four sessions, those who ultimately graduated from PCIT completed an average of 20.5 sessions, ranging from 5–71 sessions, while those who terminated treatment early completed an average of 10.8 sessions, ranging from 4–47 sessions.
Within-groups behavior change for graduates, early terminators
To address our second aim, paired samples t-tests were analyzed to determine ECBI Intensity Scale score changes from first to last sessions within each group (graduates and early terminators who completed at least four sessions) separately. As hypothesized, each group showed statistically significant improvement in caregiver-reported problem behavior from intake to last session. ECBI Intensity Scale scores for graduates (n=233) decreased from x̄=139.0 (t=62) at pre-treatment to x̄=88.8 (t=48) at last session attended, t(232)=22.78; p<0.001, while these scores for those who terminated treatment early but attended at least four sessions (n=681) decreased from x̄=150.4 (t=65) at pre-treatment to x̄=123.3 (t=58) at last session attended, t(680)=20.87; p<0.001). See Figures 1 and 2 for graphical depictions of ECBI Intensity and Problem Scale score changes for each group. Comparatively, for those who terminated after attending three or fewer sessions (n=404), ECBI Intensity scores decreased from x̄=149.3 (t=65) at pre-treatment to x̄=145.3 (t=64) at last session attended, (t (403)=4.17; p<0.001.
Effect sizes, using Cohen’s d, were also calculated separately for those who graduated, those who terminated treatment early after attending at least four sessions, and both groups combined, using ECBI Intensity Scale score changes from first to last sessions. While families who remained in treatment until meeting graduation requirements demonstrated very large effect sizes in problem behavior intensity improvements (d=1.65), families who terminated treatment early but after attending a minimum of four treatment sessions still showed a medium-to-large effect size for improvements in behavior problems (d=0.70), as demonstrated by ECBI Intensity Scale score changes. In general, all families who attended at least four sessions (ie, a combined sample of graduates and early terminators) reported large effect sizes in ECBI Intensity Scale score change from first to last sessions (d=0.86).10 In contrast, those who terminated after attending three or fewer sessions showed a very small-to-small effect size (d=0.11) for ECBI Intensity score change. See Table 1 for comparisons among these and representative effect sizes from other treatment outcome studies.
Between-groups behavior change for graduates, early terminators
To examine our third aim, independent-samples t-tests were conducted comparing ECBI Intensity Scale score changes for those who graduated with those who terminated treatment early after attending at least four treatment sessions. As hypothesized, the average size of ECBI Intensity Scale score change was significantly larger for those who graduated (x̄=50.2; SD=33.6) than for those who terminated early (x̄=27.1; SD=33.9; t(912)=-9.00; p<0.001). Further, those who eventually terminated treatment early but after at least four sessions had significantly higher ECBI Intensity Scale scores at intake (x̄=150.4; SD=36.3) than did those who eventually graduated (x̄=139.0; SD=31.3; t(912)=4.28; p<0.001). At the last session, ECBI Intensity Scale scores were significantly lower on average for those who graduated (x̄=88.8; SD=29.4) compared with those who terminated early after four sessions (x̄=123.3; SD=41.1; t(912)=11.83; p<0.001).
Behavior change and number of sessions
To address our final aim, mean ECBI Intensity Scale score changes were graphed according to the number of sessions completed for treatment graduates and all early terminators; decreases were depicted as positive numbers (eg, mean ECBI Intensity Scale score change from 180 at first session to 130 at last session was graphed as a decrease of +50 ECBI raw score points). Figure 3 depicts the average ECBI Intensity Scale score decrease for families based on the session number after which they discontinued treatment. These change scores were divided into separate lines for those families whose last session was a graduation session and those whose last session represented early termination from treatment. Even for families who did not graduate, there was clear incremental benefit to attending additional sessions from 4–6 sessions up to 10–12 sessions. This group also appeared to benefit from additional sessions between 22–24 sessions through 31–33 sessions. Following 33 sessions, those who terminated early showed decreasing gains as measured by the ECBI Intensity Scale. The shortest treatment duration to reach graduation in this sample was five sessions. Of those who graduated, 72% of families did so between 10–12 and 22–24 sessions, 26% graduated after 25 or more sessions, and 3% graduated in fewer than 10 sessions. For graduates, all treatment lengths resulted in average ECBI Intensity Scale score decreases of more than 40 points except for the five families who graduated in 7–9 sessions. At each respective treatment length, those who graduated experienced larger decreases in ECBI Intensity Scale scores on average than those who did not graduate (with the exception of the five families who graduated in 7–9 sessions).
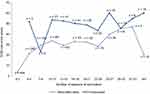 |
Figure 3 Decrease in raw ECBI Intensity Scale score from first to last PCIT visit.Abbreviations: ECBI, Eyberg Child Behavior Inventory; PCIT, Parent–Child Interaction Therapy. |
Discussion
Summary
The current findings indicate impressive treatment benefits (ie, medium-to-large effect sizes) for caregiver-reported child behavior problems after completion of as few as four sessions of PCIT. In other words, significant improvements in children’s behavior were experienced even by families who terminated early, prior to graduation from PCIT. These results are particularly important given that the majority of families (74.5%) discontinued treatment prior to meeting the designated PCIT graduation criteria, a finding that is consistent with previous investigations of attrition in community-based PCIT samples from the US.15,31,32 While both graduates and early terminators who attended at least four sessions demonstrated significant improvements in caregiver reports of child behavior problems, those families who graduated showed significantly larger improvements and significantly lower levels of child behavior problems at termination compared with those who terminated early. Those who terminated early after attending fewer than four sessions of PCIT reported minimal if any improvements. Data from this sample also revealed that families who dropped out of treatment early began with significantly higher levels of child behavior problems than did those who graduated from PCIT. When graphed, ECBI Intensity Score change by number of total sessions completed for each group showed greater change for graduates at nearly every terminal treatment duration. Moreover, both groupsgenerally showed more improvement with longer treatment durations. Simple correlations echoed findings that longer treatment duration and attainment of graduation were related to better treatment outcomes.
“Dropout” does not equate “failure”
Previous research has demonstrated that PCIT is a powerful intervention for those who complete it,9 but this study showed treatment effectiveness even for families who do not graduate from PCIT. In many cases, it is considered a failure when a family leaves PCIT before graduation, but these results indicate that even small doses of PCIT are associated with significant improvements in functioning. Our findings are in line with previous research. In a community-based study in which only 20% of families completed the full course of PCIT, Stokes et al33 found that the entire sample of families still demonstrated an effect size of d=0.74 for child behavior improvements at 7.5 months post-treatment follow-up. This medium-to-large effect size is particularly impressive considering that 75% of the follow-up sample had dropped out of PCIT prematurely. Current findings regarding rapid improvements early in treatment also reflect those noted by Hakman et al.34 In their child welfare-based trial of PCIT, evidence of dramatic change in positive and negative caregiver skills occurred as early as the first and second CDI coaching sessions. This timeline corresponds to changes recorded by sessions denoted as three or four in the current study. Although the present study did not employ a control group, pretreatment ECBI Intensity Scale scores from our early terminators group are comparable to those found in randomized controlled trials.35,36 These trials demonstrated that no-treatment or attention-only waitlist control families experienced little to no change in ECBI Intensity Scale scores over a 12-week period. Interpreted in this context, the current data showing clinically significant improvement of medium-to-large effect sizes for those who terminated treatment should not be ignored.
Our findings have important implications for policy-makers, managed care organizations, children’s mental health administrators, and leaders in early childhood programming. Specifically, the finding that small doses (as few as four sessions) of this low-cost intervention significantly improved child behavior problems despite high treatment attrition rates suggests that the overall success rate of PCIT is even higher than previously reported. From a cost-effectiveness standpoint, the results provide additional evidence that leaders in early childhood mental health should take steps to increase implementation of PCIT, as relatively few families currently have access to this well-established intervention. If this treatment were made more readily available to families in need through services like Head Start, Birth to Three, Early Intervention, Early Special Education, preschools, kindergartens, and pediatric primary care, society could stand to gain considerably. Decreases in negative outcomes of early childhood behavior disorders such as delinquency, violence, substance abuse, academic failure, and mental health problems would translate into decreased costs to society measured financially and by quality-of-life.37–40 Even child abuse and neglect could be mitigated with more widespread implementation of PCIT.41,42
Effectiveness despite attrition
Evidence of treatment effectiveness for families who end treatment early is especially promising given the challenge posed by attrition in this population. Generally, attrition in community-based behavioral health is problematic; however, there are several theoretical reasons why attrition in parent training programs for young children with behavior problems is particularly high. Families with one or more children presenting with extremely challenging behaviors may have difficulties in consistently bringing their children to therapy sessions. Families in this stage of life typically juggle many competing demands for their time, energy, and resources, like childcare for other young children in the family, pregnancy, nursing, challenging developmental milestones (eg, toilet-training), relatively frequent child illnesses, and early stage careers. Additionally, many families accessing behavioral parent training can be characterized as having low-socioeconomic status. Multiple factors make treatment completion more difficult for these families, such as single-parent status, low caregiver-to-child ratio, other mental health diagnoses, difficulties staying in contact with therapists (eg, disruptions in phone service, residential instability), and disruptions in child placements.20,43,44
Given the multitude of behavioral challenges and competing demands, a family that quickly experiences significant improvements in behavior at the start of therapy might discontinue treatment immediately, prioritizing other demands. Fernandez and Eyberg20 found that 10% of families who dropped out of PCIT early stated satisfactory behavior improvements as their primary reason for discontinuing treatment. Liebsack45 found that, of those who discontinued PCIT prematurely, their therapists also believed PCIT was no longer needed about 17% of the time. Another factor affecting attrition is that PCIT represents an active treatment, in which caregivers are expected to participate and complete daily, at-home practice sessions. Given the aforementioned stressors faced by many PCIT families, caregiver requirements are often perceived as overwhelming in comparison to other treatments focusing primarily on therapist–child dynamics. According to therapist-report, 17% of non-completers left treatment early because PCIT was too demanding for them, and 42% left because of low caregiver interest or motivation.45 To address the lack of interest, several models of PCIT have successfully incorporated components targeting increased caregiver motivation and engagement with the ultimate goal of reducing attrition.46,47
Attrition rates for parent training programs aimed at young children with behavior problems appear to be comparatively high because they are frequently contrasted with those of individual treatments for adults. For example, meta-analyses have provided evidence of attrition rates in Cognitive-Behavioral Therapy (CBT) for adults at 23–26%.48,49 For many reasons (eg conflicting schedules, child care requirements), treatment completion may be easier for individuals than when attendance and coordinated efforts by multiple family members are required. Finally, PCIT, in particular, sets high standards for graduation (eg, ECBI scores well-below the clinical cut-off for child behavior problems, strict skill mastery criteria for caregivers). Using these criteria as benchmarks for successful treatment completion means that some families experiencing remarkable improvements in presenting problems or satisfaction with their children’s subsequent levels of functioning are considered to have “dropped-out” of treatment prematurely. When evaluating the overall effectiveness of PCIT, this study suggests that more attention should be paid to child behavior improvements and parental skill acquisition at the time of discharge than to the actual graduation rates, given that reliance on strict graduation standards may lead to under-reporting of actual treatment success.
Graduates show even greater improvements
Although families in both groups (graduates and early terminators) demonstrated significant treatment effects, families who graduated experienced significantly greater improvements and left treatment with significantly lower ratings of child behavior problems than did families who terminated early. It should be noted, however, that families who terminated early also began with significantly greater child behavior problems, which may partially explain their higher scores at termination. While PCIT can be an effective treatment even for those who do not graduate, there is incremental benefit to completing treatment. This finding coincides with positive bivariate correlations linking greater ECBI Intensity and Problem Scale score improvements to both graduation status and greater number of treatment sessions (see Table 2).
Given the many treatment barriers described above and in the literature,17,20 it is understandable that many families seeking PCIT services continue to struggle with attaining graduation criteria in PCIT. To better meet the needs of these families, some efforts have been made in PCIT research to investigate the efficacy of a modified treatment protocol to give families access to the powerful tools provided in CDI and PDI, in fewer sessions. Graziano et al50 investigated the utility of a shorter treatment approach (Intensive PCIT) specifically designed for high-stress families likely to discontinue treatment quickly. This approach employed 90 minute-sessions, 5 days per week for 2 weeks. When this intensive commitment is not feasible, families at high risk of early termination might benefit from a version of PCIT offering fewer initial sessions of CDI (eg, four sessions), followed by the usual PDI delivery, with a final return to focus on CDI and PDI until mastery is achieved. This would ensure that families have at least some opportunity to learn effective discipline strategies before leaving therapy. However, research is needed before any major change to the structure of PCIT for these families is warranted.
Baseline differences between groups
Baseline levels of behavior problems, an important marker for clinicians, may warrant further attention based on current findings. Significantly higher levels of child behavior problems reported by families in the early terminators group as compared with the graduates group may be related to additional or more severe barriers to treatment. Perhaps caregiver-reports of more intense problems are reflective of greater overall life stress which, in turn, impacts the ability to complete treatment. Quick and drastic decreases in problem behavior often experienced in the first few sessions of PCIT may provide sufficient relief to families who are experiencing many other pressing problems (eg, unemployment, caring for multiple young children, health problems). Therefore, clinicians should focus on problem-solving concerning barriers to treatment early in the intervention process for families reporting the most severe child behavior problems.
The literature regarding child behavior problem intensity at intake among graduates and early terminators in PCIT is variable. In line with current findings, Werba et al15 found that treatment completers began with lower ECBI Intensity Scale scores than did those who eventually dropped out early. Contrary to results of the present study, other researchers have found that those who graduated from PCIT reported higher ECBI Intensity Scale scores at intake than those who dropped out of treatment prematurely in the US31 and elsewhere (the Netherlands;19 Taiwan).51 Cultural context may differentially impact the relation between baseline ECBI scores and the probability of treatment graduation, as countries outside of the US tend to have lower rates of attrition from PCIT as well.19,51–53
Change scores related to the number of treatment sessions
Figure 3 depicts decreases in raw ECBI Intensity Scale score from first to last PCIT visit. In general, as is also reflected in bivariate correlations, families tended to show incremental improvements as measured by caregiver-reported behavior problems as the number of sessions attended increased. Families who graduated from treatment tended to experience greater improvements at nearly every treatment duration compared with those who terminated treatment early. Early terminators also showed marked decreases in overall improvement following 33 sessions of PCIT. As this treatment length is well outside of the suggested treatment length for PCIT, other factors may contribute to a decline in treatment effectiveness in these cases (eg, sporadic attendance, drift from PCIT protocol fidelity, other treatment barriers). Of those who graduated, the majority (>70%) required 10–24 sessions to do so, but about 26% of graduates required 25 or more sessions to graduate. Therefore, to receive the maximum treatment benefits, PCIT should be provided through graduation or as long as families are able to attend treatment. Providers should adhere to protocol and seek supervision and consultation concerning treatment targets, especially as treatment length increases. These data are useful for community agencies, clinicians, managed care companies, and other behavioral healthcare funding agencies because they provide evidence that (1) even if families terminate from treatment early, incremental improvements are evident with additional sessions attended up to about 33 sessions, (2) if possible, it is beneficial for families to remain in treatment until meeting graduation criteria, and (3) there is variability in the number of sessions required to reach graduation, so it would be detrimental to restrict services to a pre-determined low number of sessions.
Limitations
Excluding families from analyses based on missing data (ie, pre- and/or post-ECBI Intensity Scale scores, graduation status, number of sessions) confounded our results. It is possible that families with missing data differed meaningfully from those with complete data. Similarly, effect sizes from this study should be interpreted with caution as they only include data from those families who attended at least four treatment sessions, which we estimated to be the smallest possible dose of PCIT. It is important to remember that all outcome measures in the study were reported by caregivers only. Caregiver reports may be biased in many ways; for example, caregivers might show inflated estimates of behavior problem severity because of parenting stress, or may overestimate behavior improvements due to sunk costs in therapy.54–56 Because this study analyzed an existing, community-based data set, researchers had little control over and few measurements of treatment fidelity, data reporting procedures, and variability across agencies and populations. Additionally, with no control group, it is difficult to determine how treatment outcomes would compare with outcomes of no treatment. Although effect sizes from the present study are compared with those from other treatment modalities, the use of a control group would have more accurately estimated group differences. Finally, without follow-up, it is unclear how the improvements in behavior problems reported by caregivers in this sample maintain over time or translate into other positive outcomes for families.
Conclusion
This investigation shows that, while families who graduated from PCIT in this sample demonstrated a very large effect size in problem behavior intensity improvement, families who terminated treatment early, but after attending at least four treatment sessions, still showed significant improvements in behavior problems with a medium-to-large effect size. Although early terminators in PCIT have previously been identified as treatment failures, the present study provides reason to reconceptualize “dropouts” in relation to evidence of positive treatment outcomes. These findings are important considerations in the funding and provision of this evidence-based treatment in community settings.
Authors’ Information
Corey C Lieneman, MS, is a doctoral student in the Clinical Child Psychology Program at West Virginia University. Lauren B Quetsch, MS, is a doctoral student in the Clinical Child Psychology Program at West Virginia University and clinical psychology doctoral intern at the University of Arkansas for Medical Sciences. Laurie L Theodorou, LCSW, is an Early Childhood Mental Health Policy Specialist at the Oregon Health Authority. Kathleen A Newton, MPH, is a lead research analyst at the Oregon Health Authority. Cheryl B McNeil, PhD, is a professor of psychology at West Virginia University.
Disclosure
Ms Laurie L Theodorou was employed by the Oregon Health Authority (OHA) as a Policy Analyst for the Child and Family Behavioral Health unit. One of her primary tasks is to oversee the OHA grants to agencies across Oregon with the goal of increasing access of high fidelity PCIT to Medicaid eligible families. Dr Cheryl B McNeil received Book royalties from Springer Science Publishers, and grants from SAMHSA for PCIT training for therapists at FMRS in Beckley. Lauren B Quetsch also received Book royalties from Springer Science Publishers for her work in PCIT. The authors report no other conflicts of interest in this work.
References
1. Boylan K, Vaillancourt T, Boyle M, Szatmari P. Comorbidity of internalizing disorders in children with oppositional defiant disorder. Eur Child Adolesc Psychiatry. 2007;16(8):484–494. doi:10.1007/s00787-007-0624-1
2. Evans SC, Pederson CA, Fite PJ, Blossom JB, Cooley JL. Teacher-reported irritable and defiant dimensions of oppositional defiant disorder: social, behavioral, and academic correlates. Sch Ment Heal A Multidiscip Res Pract J. 2016;8(2):292–304. doi:10.1007/s12310-015-9163-y
3. Sari Gokten E, Saday Duman N, Soylu N, Uzun ME. Effects of attention-deficit/hyperactivity disorder on child abuse and neglect. Child Abuse Negl. 2016;62:1–9. doi:10.1016/j.chiabu.2016.10.007
4. Broidy LM, Nagin DS, Tremblay RE, et al. Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: a six-site, cross-national study. Dev Psychol. 2003;39(2):222–245.
5. Plattner B, Steiner H, The SSL, et al. Sex-specific predictors of criminal recidivism in a representative sample of incarcerated youth. Compr Psychiatry. 2009;50(5):400–407. doi:10.1016/j.comppsych.2008.09.014
6. Vogel M, Messner SF. Social correlates of delinquency for youth in need of mental health services: examining the scope conditions of criminological theories. Justice Q. 2012;29(4):546–572. doi:10.1080/07418825.2011.582879
7. Burke JD, Hipwell AE, Loeber R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. J Am Acad Child Adolesc Psychiatry. 2010;49(5):484–492.
8. Burke JD, Stepp SD. Adolescent disruptive behavior and borderline personality disorder symptoms in young adult men. J Abnorm Child Psychol. 2012;40(1):35–44. doi:10.1007/s10802-011-9558-7
9. Ward M, Theule J, Cheung K. Parent–child interaction therapy for child disruptive behaviour disorders: a meta-analysis. Child Youth Care Forum. 2016;45(5):675–690. doi:10.1007/s10566-016-9350-5
10. Cohen J. Statistical Power Analysis for the Behavioral Sciences.
11. Sawilowsky S. New Effect Size Rules of Thumb. J Mod Appl Stat Methods. 2009;8:597–599. doi:10.22237/jmasm/1257035100
12. Lyon AR, Budd KS. A community mental health implementation of Parent-Child Interaction Therapy (PCIT). J Child Fam Stud. 2010;19(5):654–668. doi:10.1007/s10826-010-9353-z
13. Phillips J, Morgan S, Cawthorne K, Barnett B. Pilot evaluation of parent child interaction therapy? delivered in an Australian community early childhood clinic setting. Aust N.Z.J. Psychiatry. 2008;42:712–719.
14. Danko CM, Brown T, Van Schoick L, Budd KS. Predictors and correlates of homework completion and treatment outcomes in parent–child interaction therapy. Child Youth Care Forum. 2016;45(3):467–485. doi:10.1007/s10566-015-9339-5
15. Werba BE, Eyberg SM, Boggs SR, Algina J. Predicting outcome in parent-child interaction therapy: success and attrition. Behav Modif. 2006;30(5):618–646. doi:10.1177/0145445504272977
16. Ros R, Hernandez J, Graziano PA, Bagner DM. Parent training for children with or at risk for developmental delay: the role of parental homework completion. Behav Ther. 2016;47(1):1–13. doi:10.1016/j.beth.2015.08.004
17. de Haan AM, Boon AE, Jtvm DJ, Hoeve M, Vermeiren RRJM. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin Psychol Rev. 2013;33(5):698–711. doi:10.1016/j.cpr.2013.04.005
18. Comer JS, Furr JM, Miguel EM, et al. Remotely delivering real-time parent training to the home: an initial randomized trial of Internet-delivered parent-child interaction therapy (I-PCIT). J Consult Clin Psychol. 2017;85(9):909–917. doi:10.1037/ccp0000230
19. Abrahamse ME, Niec LN, Junger M, Boer F, Lindauer RJL. Risk factors for attrition from an evidence-based parenting program: findings from the Netherlands. Child Youth Serv Rev. 2016;64:42–50. doi:10.1016/j.childyouth.2016.02.025
20. Fernandez MA, Eyberg SM. Predicting treatment and follow-up attrition in parent-child interaction therapy. J Abnorm Child Psychol. 2009;37(3):431–441. doi:10.1007/s10802-008-9281-1
21. Eyberg S, Funderburk B. Parent-Child Interaction Therapy Protocol. Gainesville, FL: PCIT International; 2011.
22. Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J Clin Child Adolesc Psychol. 2008;37(1):215–237. doi:10.1080/15374410701820117
23. Girard E, Wallace NM, Morgan S, Kohlhoff J, McNeil CB. Parent-Child Interaction Therapy with Toddlers: Improving Attachment and Emotion Regulation. New York, NY: Springer; 2018. doi:10.1007/978-3-319-93251-4
24. Lieneman CC, Brabson LA, Highlander A, Wallace NM, McNeil CB. Parent–child interaction therapy: current perspectives. Psychol Res Behav Manag. 2017;10:239–256. doi:10.2147/PRBM.S91200
25. McNeil CB, Quetsch LB, Anderson CM, eds. Handbook of Parent-Child Interaction Therapy (PCIT) for Children on the Autism Spectrum. New York, NY: Springer; 2018.
26. Niec LN, ed. Handbook of Parent-Child Interaction Therapy: Innovations and Applications for Research and Practice. New York, NY: Springer; 2018.
27. McNeil CB, Hembree-Kigin TL. Parent–Child Interaction Therapy.
28. Oregon Office of Rural Health. Rural Definitions. Available from: http://www.ohsu.edu/xd/outreach/oregon-rural-health/data/rural-definitions/index.cfm.
29. Eyberg SM, Pincus D. Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Intentory-Revised: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1999.
30. Eisenstadt TH, McElreath LH, Eyberg S, McNeil CB. Interparent agreement on the eyberg child behavior inventory. Child Fam Behav Ther. 1994;16(1):21–27. doi:10.1300/J019v16n01_02
31. Lanier P, Kohl PL, Benz J, Swinger D, Moussette P, Drake B. Parent-child interaction therapy in a community setting: examining outcomes, attrition, and treatment setting. Res Soc Work Pract. 2011;1(6):689–698. doi:10.1177/1049731511406551
32. Pearl E, Thieken L, Olafson E, et al. Effectiveness of community dissemination of parent–child interaction therapy. Psychol Trauma Theory, Res Pract Policy. 2012;4(2):204–213. doi:10.1037/a0022948
33. Stokes JO, Wallace NM, McNeil CB. Effectiveness of community-delivered parent-child interaction therapy compared to usual care. Child Fam Behav Ther. 2018;40(4):279–305. doi:10.1080/07317107.2018.1522232
34. Hakman M, Chaffin M, Funderburk B, Silovsky JF. Change trajectories for parent-child interaction sequences during parent-child interaction therapy for child physical abuse. Child Abuse Negl. 2009;33(7):461–470. doi:10.1016/j.chiabu.2008.08.003
35. Thomas R, Zimmer-Gembeck MJ. Accumulating evidence for parent-child interaction therapy in the prevention of child maltreatment. Child Dev. 2011;82(1):177–192. doi:10.1111/j.1467-8624.2010.01548.x
36. Thomas R, Zimmer-Gembeck MJ. Parent-child interaction therapy: an evidence-based treatment for child maltreatment. Child Maltreat. 2012;17(3):253–266. doi:10.1177/1077559512459555
37. Goldfine ME, Wagner SM, Branstetter SA, Mcneil CB. Parent-child interaction therapy: an examination of cost-effectiveness. J Early Intensive Behav Interv. 2008;5(1):119–141. doi:10.1037/h0100414
38. Jones DE, Greenberg M, Crowley M. Early social-emotional functioning and public health: the relationship between kindergarten social competence and future wellness. Am J Public Health. 2015;105(11):2283–2290. doi:10.2105/AJPH.2015.302630
39. Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. Bmj. 2001;323(7306):191. doi:10.1136/bmj.323.7306.191
40. Trautmann S, Rehm J, Wittchen H-U. The economic costs of mental disorders. EMBO Rep. 2016;17(9):1245–1249. doi:10.15252/embr.201642951
41. Chaffin M, Silovsky JF, Funderburk B, et al. Parent-child interaction therapy with physically abusive parents: efficacy for reducing future abuse reports. J Consult Clin Psychol. 2004;72(3):500–510. doi:10.1037/0022-006X.72.3.500
42. Timmer SG, Urquiza AJ, Zebell NM, McGrath JM. Parent-child interaction therapy: application to maltreating parent-child dyads. Child Abuse Negl. 2005;29(7):825–842. doi:10.1016/j.chiabu.2005.01.003
43. Kazdin AE, Mazurick JL. Dropping out of child psychotherapy: distinguishing early and late dropouts over the course of treatment. J Consult Clin Psychol. 1994;62(5):1069–1074.
44. Liebsack BK. Attrition in Parent-Child Interaction Therapy [thesis]. Morgantown: West Virginia University; 2016.
45. Liebsack BK. The Parent-Child Interaction Therapy Family Experiences and Feedback Study: A Follow-Up Examination of Attrition in an Evidence-Based Treatment in Community Settings Statewide [dissertation]. Morgantown: West Virginia University; 2018.
46. Chaffin M, Funderburk B, Bard D, Valle LA, Gurwitch R. A combined motivation and parent-child interaction therapy package reduces child welfare recidivism in a randomized dismantling field trial. J Consult Clin Psychol. 2011;79(1):84–95. doi:10.1037/a0021227
47. Webb HJ, Thomas R, McGregor L, Avdagic E, Zimmer-Gembeck MJ. An evaluation of parent-child interaction therapy with and without motivational enhancement to reduce attrition. J Clin Child Adolesc Psychol. 2017;46(4):537–550. doi:10.1080/15374416.2016.1247357
48. Fernandez E, Salem D, Swift JK, Ramtahal N. Meta-analysis of dropout from cognitive behavioral therapy: magnitude, timing, and moderators. J Consult Clin Psychol. 2015;83(6):1108–1122. doi:10.1037/ccp0000044
49. Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621–632.
50. Graziano PA, Bagner DM, Slavec J, et al. Feasibility of intensive parent-child interaction therapy (I-PCIT): results from an open trial. J Psychopathol Behav Assess. 2015;37(1):38–49. doi:10.1007/s10862-014-9435-0
51. Chen Y-C, Fortson BL. Predictors of treatment attrition and treatment length in Parent-Child Interaction Therapy in Taiwanese families. Child Youth Serv Rev. 2015;56:28–37.
52. Bjorseth A, Wichstrom L. Effectiveness of Parent-Child Interaction Therapy (PCIT) in the treatment of young children’s behavior problems. a randomized controlled study. PLoS One. 2016;11(9):e0159845. doi:10.1371/journal.pone.0159845
53. Leung C, Tsang S, Heung K, Yiu I. Effectiveness of Parent—child Interaction Therapy (PCIT) among Chinese families. Res Soc Work Pract. 2009;19(3):304–313. doi:10.1177/1049731508321713
54. Arkes HR, Blumer C. The psychology of sunk cost. Organ Behav Hum Decis Process. 1985;35(1):124–140. doi:10.1016/0749-5978(85)90049-4
55. Coleman MD. Sunk cost, emotion, and commitment to education. Curr Psychol A J Divers Perspect Divers Psychol Issues. 2010;29(4):346–356. doi:10.1007/s12144-010-9094-6
56. Neece CL, Green SA, Baker BL. Parenting stress and child behavior problems: a transactional relationship across time. Am J Intellect Dev Disabil. 2012;117(1):48–66. doi:10.1352/1944-7558-117.1.48
57. Menting ATA, Orobio de Castro B, Matthys W. Effectiveness of the Incredible Years parent training to modify disruptive and prosocial child behavior: a meta-analytic review. Clin Psychol Rev. 2013;33(8):901–913. doi:10.1016/j.cpr.2013.07.006
58. Lieberman AF, Ghosh, Ippen C,VAN, Horn P. Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2006;45(8):913–918. doi:10.1097/01.chi.0000222784.03735.92
59. Nowak C, Heinrichs N. A comprehensive meta-analysis of Triple P-Positive Parenting Program using hierarchical linear modeling: effectiveness and moderating variables. Clin Child Fam Psychol Rev. 2008;11(3):114–144. doi:10.1007/s10567-008-0033-0
60. Ray DC, Armstrong SA, Balkin RS, Jayne KM. Child centered play therapy in the schools: review and meta-analysis. Psychol Sch. 2015;52(2):107–123. doi:10.1002/pits.21798
61. Arnberg A, Ost L-G. CBT for children with depressive symptoms: a meta-analysis. Cogn Behav Ther. 2014;43(4):275–288. doi:10.1080/16506073.2014.947316
62. Meszaros A, Czobor P, Balint S, Komlosi S, Simon V, Bitter I. Pharmacotherapy of adult attention deficit hyperactivity disorder (ADHD): a meta-analysis. Int J Neuropsychopharmacol. 2009;12(8):1137–1147. doi:10.1017/S1461145709990198
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.