Back to Journals » International Journal of Nanomedicine » Volume 19
Recent Development and Applications of Polydopamine in Tissue Repair and Regeneration Biomaterials
Authors Guo K, Wang Y, Feng ZX, Lin XY, Wu ZR , Zhong XC, Zhuang ZM, Zhang T, Chen J, Tan WQ
Received 26 September 2023
Accepted for publication 29 December 2023
Published 25 January 2024 Volume 2024:19 Pages 859—881
DOI https://doi.org/10.2147/IJN.S437854
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Eng San Thian
Kai Guo,1,* Yong Wang,1,* Zi-Xuan Feng,1 Xiao-Ying Lin,1 Zhang-Rui Wu,1 Xin-Cao Zhong,1 Ze-Ming Zhuang,1 Tao Zhang,1 Jian Chen,2 Wei-Qiang Tan1
1Department of Plastic Surgery, Sir Run Run Shaw Hospital Zhejiang University School of Medicine, Hangzhou, Zhejiang Province, People’s Republic of China; 2Department of Ultrasonography, The Fourth Affiliated Hospital of Zhejiang University School of Medicine, Yiwu, Zhejiang Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jian Chen, Department of Ultrasonography, The Fourth Affiliated Hospital of Zhejiang University School of Medicine, Yiwu, Zhejiang Province, People’s Republic of China, Email [email protected] Wei-Qiang Tan, Department of Plastic Surgery, Sir Run Run Shaw Hospital Zhejiang University School of Medicine, Hangzhou, Zhejiang Province, People’s Republic of China, Email [email protected]
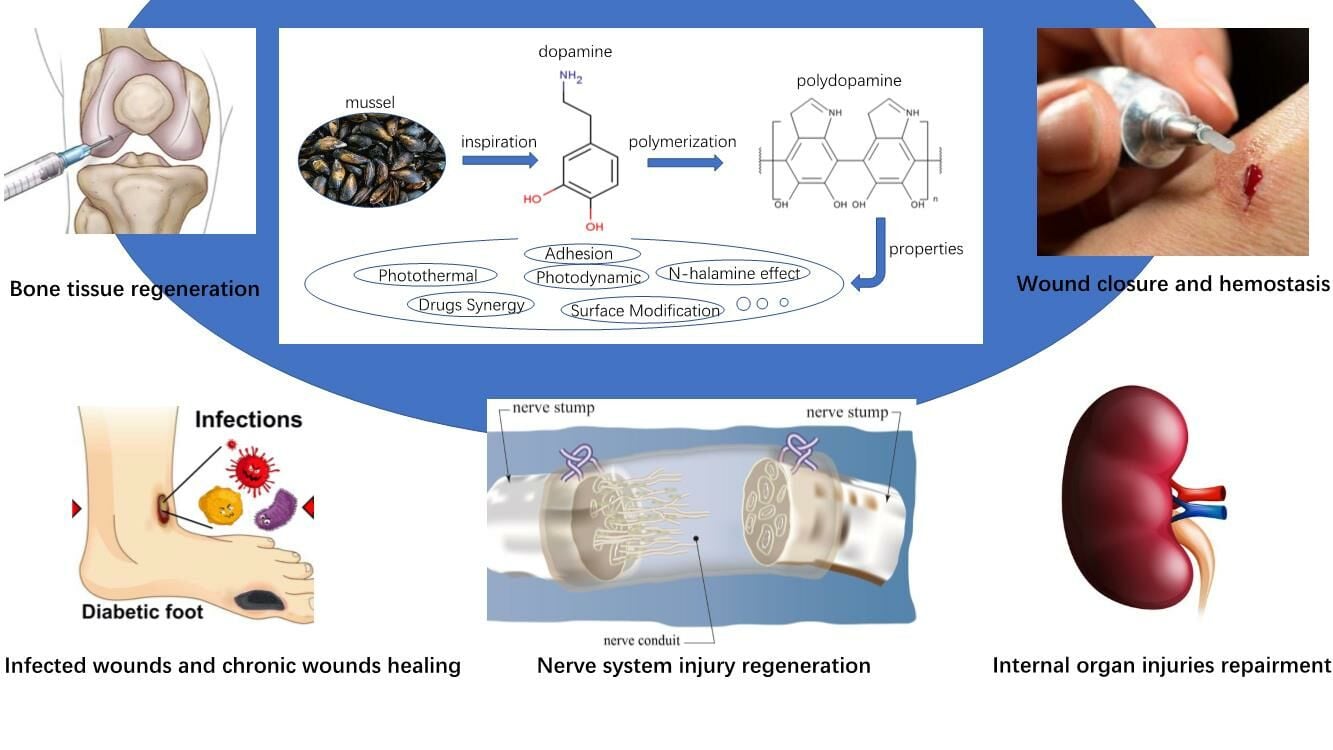
Abstract: The various tissue damages are a severe problem to human health. The limited human tissue regenerate ability requires suitable biomaterials to help damage tissue repair and regeneration. Therefore, many researchers devoted themselves to exploring biomaterials suitable for tissue repair and regeneration. Polydopamine (PDA) as a natural and multifunctional material which is inspired by mussel has been widely applied in different biomaterials. The excellent properties of PDA, such as strong adhesion, photothermal and high drug-loaded capacity, seem to be born for tissue repair and regeneration. Furthermore, PDA combined with different materials can exert unexpected effects. Thus, to inspire researchers, this review summarizes the recent and representative development of PDA biomaterials in tissue repair and regeneration. This article focuses on why apply PDA in these biomaterials and what PDA can do in different tissue injuries.
Keywords: polydopamine, biomaterial, tissue damage, tissue regeneration
Graphical Abstract:
Introduction
Accident trauma, inflammation, aggressive tumors, infectious diseases, and acquired or congenital abnormalities may cause severe damage to tissue.1–3 Unfortunately, the limited self-healing ability of tissues means that if the damage surpasses the ability of self-healing, the tissue damage will not heal, the healing process will be prolonged, and tissue function will be compromised. Biomaterials can play a role in various tissue repair and regeneration stages, such as carrying drugs to promote tissue growth, providing antibacterial, antioxidant, anti-inflammatory properties, and substituting defective tissue, among others.4–8 To achieve optimal healing of damaged tissues, it is essential to match the functions of the biomaterial to the multiple factors influencing the healing process. Moreover, it is crucial for biomaterials to be low-toxic or, ideally, non-toxic. Thus, researchers prefer materials that possess a range of properties suitable for tissue repair and regeneration, such as materials inspired and derived from nature.
Over the past decade, mussel-inspired and melanin-like materials have gained increasing attention in the biomaterials science community.9,10 The reality is that despite being inspired by different natural entities, the functional chemical components of these two types of materials are the same. Marine mussels are capable of secreting various types of foot proteins that allow them to adhere to different foreign surfaces, including the skin of marine animals, rocks, and metal ships.11 Six types of mussel foot proteins have been identified, with the most abundant being 3,4-dihydroxy-l-phenylalanine (DOPA), glycine, lysine, tyrosine, and asparagine.12,13 Melanin-like materials typically encompass eumelanin, neuromelanin, allomelanin, and pheomelanin.14,15 A schematic representation of the elements of melanin-like and mussel-inspired materials as Figure 1. The high concentration of catechol from DOPA and amine groups in these foot proteins gives them strong adhesive properties.16 They can convert specific spectrum’s photon energy into heat and chemical energy.17,18 Additionally, the polymer’s possession of free phenolic groups confers it with the ability to scavenge various reactive oxygen and nitrogen species.19,20 Moreover, owing to the abundance of binding groups, such as amines and catechols, among others, they exhibit exceptional chelating capacity.21 The aforementioned properties make mussel-inspired and melanin-like materials promising platform for several important biomedical applications, including tissue adhesion, drug-delivery systems, antioxidant therapy, and phototherapy systems. These materials were initially obtained from sources such as human hair, sepia ink, grape extracts, oligomeric proanthocyanidins, and others.22–24 The limited availability of raw materials and the difficulty in obtaining them are two significant challenges for their usage in clinical applications. According to Lee et al, dopamine (DA) was found to be a suitable replacement for natural materials, as it possesses both catechol and amine functionalities.25 DA is well-known as a neurotransmitter in human body and associate with disease like Parkinson’s disease.26 Surprisingly, they discovered that the straightforward structure of DA serves as a potent building block, facilitating the spontaneous deposition of thin polymer films on nearly any material surface. Moreover, these deposited films can be readily tailored to fulfill a wide array of functional applications.25 Commercial DA hydrochloride is produced by chemical synthesis and can be stored easily.27 The DA hydrochloride will self-polymerize into PDA nanoparticles (NPs) in alkaline environment. PDA NPs with mesoporous structures were obtained after removing the alkaline solution.28,29 Zeng et al reported an average nanoparticle diameter of approximately 200 nm,30 and while Yuan et al measured the average pore diameter to be around 16.676 nm in their study.28 Even though many details of the PDA function and structure still remain to explore, there is little doubt that PDA have same properties for tissue repair and regeneration as mussel-inspired and melanin-like materials.
 |
Figure 1 Schematic representation of the elements of melanin-like and mussel-inspired materials. |
Several researchers have reviewed the PDA biomaterials related to tissue repair and regeneration.31–33 However, the emphasis of these reviews has been primarily on the wound-healing properties inherent in PDA or on the overall ability of these biomaterials composed of multiple materials and PDA to facilitate tissue regeneration. However, as the application of PDA becomes more widespread, recent articles on biomaterials incorporating PDA have investigated additional strategies for applying PDA. These strategies are not just simple combinations of different functional materials with PDA to enhance its ability to promote tissue repair, but rather incorporating PDA as a part of a biological material system, leveraging not only its own function but also the interaction between PDA and other materials for greater impact. Therefore, this review analyzes the latest representative PDA application strategies in biomaterials (Table 1) incorporating PDA for tissue regeneration and provides some inspiration for subsequent researchers who want to use PDA for tissue regeneration.
 |
Table 1 Selected and Representative PDA Related Materials in Tissue Repair and Regeneration |
The Biomaterial for Wound Closure and Hemostasis with Adhesion Ability of PDA
As the scientists first noticed, PDA is an excellent adhesion material. PDA contains quinone, catechol, imine, amine functional groups and abundant π-conjugated structures.34 The abundant π electrons in PDA confer it with a strong binding capacity for various molecules possessing π electrons through π-π stacking and π-cation interactions.35
Tissue Adhesion Biomaterials with PDA for Wound Closure
Over the past few decades, medical tissue adhesives have been applied in surgical operations, especially when traditional suturing is not impractical or ineffective.36 Currently, in many surgical procedures, the most commonly used tissue adhesives include fibrin glues, albumin-glutaraldehyde adhesives, and cyanoacrylates.37 Nevertheless, the unstable efficacy, potential allergic reactions, and high toxicities associated with aldehyde-containing products severely restrict the clinical application of these tissue adhesives.38–40
As early as 2016, Fan et al designed a DA conjugated gelatin macromer double-crosslinked tissue adhesive intended for internal medical use.41 Chen et al reported a strategy by horseradish peroxidase cross linking γ-glutamic acid conjugated with DA as a tissue adhesive for wound closure.42 Pandey et al introduced PDA on the simple HA and cross-linker adhesion system resulting in a significant increase in the adhesion of the material. To create a mussel-inspired HA-DA product, DA was grafted onto the hyaluronic acid (HA) backbone through (1-ethyl-3-(3-dimethylaminopropyl) carbodiimide-N-hydroxy-succinimide) EDC-NHS carbodiimide chemistry under aqueous conditions.43 Upon introducing PDA to this HA-DA adhesive, the adhesion capability of the glue experiences a significant enhancement. The tissue adhesive properties of PDA NPs exhibit a correlation between higher adhesive strength and smaller particle size (Figure 2A). Although the adhesive ability of PDA still remains a lot to explore, the current studies are enough to prove PDA is an excellent material for wound closure, even better than some conventional materials.
 |
Figure 2 (A) Schematic illustration of the usage and probable working principle of cross-linker adhesion system. The tissue adhesive properties of PDA NPs exhibit a correlation between higher adhesive strength and smaller particle size (*p<0.05). Reproduced with the permission from Pandey N, Soto-Garcia L, Yaman S, et al. Polydopamine nanoparticles and hyaluronic acid hydrogels for mussel-inspired tissue adhesive nanocomposites. Biomater Adv. 2022;134:112,589.43 Copyright © 2022, with permission from Elsevier. (B and C) Porous carboxymethyl chitin microspheres with PDA (CMCHm-PDA) have better hemostatic performance (clotting time and blood loss) than a wide use commercial hemostatic agents Yunnan Baiyao® (*p<0.05). Adapted from Carbohydrate Polymers, Volume 270, Leng F, Chen F, Jiang X. Modified porous carboxymethyl chitin microspheres by an organic solvent-free process for rapid hemostasis. Pages 118348. 44 Copyright © 2021, with permission from Elsevier. |
However, there are still some problems waiting to be solved, such as making products more conventional to apply in clinics and easily stored. Experiments should not only focus on the mechanical strength and physicochemical properties of PDA, but also consider its ability to support cell proliferation and tissue regeneration for effective wound closure. The process of wound closure not only closes the wound by adhesive simply, but also includes the following cell proliferation and tissue regeneration to close the wound in a real sense. Therefore, in addition to just in vitro tissue, we should test the healing effects of adhesion materials in vivo.
Hemostatic Biomaterials with PDA
PDA not only has the ability to adhere broken vessels and stop bleeding, but also effectively combines with conventional hemostatic materials that lack tissue and vessel adhesion abilities, such as chitosan,45 silica NPs,46 and graphene oxide (GO).47 Furthermore, PDA can endow various clinical tools with hemostatic properties, such as needles,48 hydrogels, and sponges.49
The widely used commercial hemostatic materials have certain drawbacks. For instance, QuickClot©, which has been extensively used in warfare and saved many soldiers during the Gulf War,50 can cause scorching of the wound area and trigger allergic reactions due to heat release during the hemostatic process.51 In addition, the presence of oxygen-containing groups in a new promising hemostatic agent, GO, raises concerns about toxicity.52
Gong et al designed a hydroxyapatite hemostatic material with PDA.53 They work out that the best ratio of nano hydroxyapatite and DOPA hydrochloride is 20:1. The hemostatic capacity between a popular commercial production Celox and this composite was studied. The PM has better performance in the longest hemostatic time, the blood loss and uncontrolled bleeding circumstance than Celox and control. Although Celox is popular in clinical use, it was reported to perform poorly on uncontrolled bleeding.54 For this circumstance, Leng et al modified porous carboxymethyl chitin microspheres with PDA (CMCHm-PDA). This material displayed better hemostatic performance than two wide use commercial hemostatic agents Yunnan Baiyao® or /and Quickclean® in three kinds of rat bleeding models (tail amputation model, liver injure model and femoral arterial/venous cutting model), especially for CMCHm-PDA, the bleeding time was only 45s in the femoral artery/vein cut model (Figure 2B and C).44 For conventional hemostatic material, Cao et al design a multifunctional hemostatic sponge modified by PDA. Furthermore, in rat tail amputation models, the sponge demonstrated a superior hemostatic effect compared to conventional gauze. This enhancement can be attributed to the improved procoagulant activity and increased adhesion of red blood cells and platelets to the sponge.55,56
PDA Carries a Comprehensive Range of Drugs That Promote Tissue Regeneration and Repair
PDA has a strong binding capacity for a variety of drugs that facilitate tissue repair, like various metal ions, antibiotics, proteins, exosomes, etc.57–63
A Variety of Protein-Based Growth Factors Combine with PDA for Tissue Growth
For achieving more desirable tissue growth, the method commonly employed in tissue repair, particularly in osseointegration, is the local delivery of growth factor agents.64 Due to the short half-life and rapid clearance of protein-based growth factors from the body, traditional methods involving covalent or weak electrostatic encapsulation of proteins into natural hydrogels might lead to reduced bioactivity or potentially trigger side effects in vivo.65,66 The latest researches on PDA and protein-based growth factors have shown that these problems can be effectively addressed and perfectly combined PDA.
Bone morphogenetic protein-2 (BMP-2) is an essential factor known for promoting osteogenesis and has found widespread use in clinical applications for bone repair and regeneration.67,68 The remarkable bone regenerative ability of BMP-2 has captivated numerous researchers to incorporate it into biomaterials. Studies have shown that BMP-2 can activate cellular pathways associated with osteogenesis and effectively enhance bone formation in animal experiments.69,70 Wu et al designed a kind of biomimetic hydrogel may be used as a translational potential material to promote the construction and regeneration of mandibular bones. They combined PDA to scavenge reactive oxygen species (ROS) and heparin (PDAH) to prolong and control BMP-2 release (Figure 3A).71 Heparin, a naturally occurring glycosaminoglycan, possesses a high negative charge and exhibits a strong affinity for a class of positively charged growth factors.72–75 DA can undergo a chemical reaction with heparin through the interaction between the carboxyl groups or sulfate groups of heparin and the amino groups of PDA polymers. Typical images indicated that with the further increase of heparin concentration, the mixtures tend to form NP aggregates with the smaller particle size. In details, the BMP-2 absorption efficiencies on the PDA and PDAH NPs were 68.2% and 90.03%, respectively. Therefore, heparin-functionalized PDA NPs can enhance the loading capacity of BMP-2. Additionally, due to the strong affinity interactions between BMP-2 and heparin, these NPs can sustain the release of BMP-2 over time.76
 |
Figure 3 (A) PDA/heparin nanoparticles were prepared to improve the encapsulation efficiency and control BMP-2 release behavior. Reproduced from Wu Y, Li X, Sun Y, et al. Multiscale design of stiffening and ROS scavenging hydrogels for the augmentation of mandibular bone regeneration. Bioact Mater. 2023;20:111–125.71 Copyright © 2022 KeAi, open access. (B) Fabrication of bone morphogenetic protein-2 (BMP2)-functionalized 3D-printed P34HB scaffold via polydopamine surface modification.77 (C) The amount of attached BMP2 was observed to increase with the increasing initial concentration of BMP-2.77 (D) Percentage of released BMP2 from BMP2-functionalized 3D-printed P34HB scaffolds during 30 days incubation in PBS buffer.77 (B–D) Used with permission of Royal Society of Chemistry, from Zhang X, Li J, Chen J, et al. Enhanced bone regeneration via PHA scaffolds coated with polydopamine-captured BMP2. J Mater Chem B. 022;10(32):6214–6227.77 ; permission conveyed through Copyright Clearance Center, Inc. (E) Schematic illustration showing the PDA coating of porous microspheres and the subsequent exosome adsorption via bioinspired dopamine chemistry. Gao YK, Yuan ZY, Yuan XJ, et al. Bioinspired porous microspheres for sustained hypoxic exosomes release and vascularized bone regeneration. Bioact Mater. 2022;14:377–388. doi:10.1016/j.bioactmat.2022.01.041.78 Copyright © 2022 KeAi, open access. |
The conservative chemical structures of biomaterials, coupled with the lack of simple and moderate modification methods and the instability of bioactive substances (particularly growth factors), result in poor osteoinductive signals. This ultimately hinders cell adhesion, growth, and differentiation, leading to hindered bone restoration and regeneration. Zhang et al built a scaffold coated with PDA, the PDA can capture BMP-2 in BMP-2 solution (Figure 3B).77 The amount of attached BMP-2 was observed to increase with the increasing initial concentration of BMP-2 (Figure 3C). The release of BMP-2 from the scaffolds exhibited no burst effect, with only 4.72 ± 1.55% of BMP-2 released within the first 24 hours. Furthermore, the released BMP-2 percentage remained stable over the course of 30 days, leading to a cumulative release percentage of 86.64 ± 1.53% (Figure 3D). For repairing bone defects resulting from surgery, conventional implants like titanium-based alloys and emerging materials like polyetheretherketone (PEEK) have become the essential materials used in orthopedic and dental implants.79 The highly adhesive PDA layer on the substrate not only imparts a hydrophilic surface to the substrate,80,81 but also provides a secondary reaction platform for immobilizing growth factors like BMP-2. This is possible due to the abundant catechol and amine groups in PDA, which can react with amine- and thiol-containing substances through Michael addition or Schiff base reactions.82–84 BMP-2 can be combined with other sustained-release drug carriers, such as polylactic acid-glycolic acid (PLGA), which offers flexible regulation through adjustments in the lactide/glycolide ratio and the polymer molecular weight.85 Then the microsphere carriers bond to the PDA coating of the PEEK surface after plasma pretreatment. The strategy of combining BMP-2 and PDA to promote bone healing may also provide implications for other drugs combined with PDA to promote bone healing.
PDA and Exosomes Binding Promotes Tissue Repair
Exosomes are small extracellular vesicles (30–150 nm in diameter) secreted by cells, demonstrating promising therapeutic potential as alternatives to living cells. They possess equivalent or even superior efficacy while requiring no external maintenance.86,87 In tissue regeneration, the therapeutic efficacy of exosomes is often limited by their low retention and instability.88,89 Hydrogels have been utilized as exosome carriers, enabling the encapsulation of exosomes, thereby facilitating the delivery of exosomes to the target site and enhancing their local retention.90,91 Indeed, exosomes encapsulated in hydrogels often face challenges with long-term preservation, as they cannot be effectively stored over extended periods. To preserve exosomes using the lyophilization method, the addition of cryoprotectants becomes necessary to maintain their stability.92 Surface adsorption via affinity coatings, which avoids the need for the lyophilization step, could be a more gentle and friendly approach for transporting delicate exosomes. This method offers a promising alternative for preserving and delivering exosomes without subjecting them to potentially damaging freeze-drying processes.93
In their study, Gao et al conducted a comparison of the loading efficiency and release kinetics of different surface coating methods, which included PDA, polyethyleneimine, tannic acid (TA), and heparin coatings (Figure 3E).94–96 The PDA and TA coatings demonstrated sustained release of exosomes for over one week, which was attributed to the adhesive properties of the catechol groups in these coatings. They utilized bioinspired injectable porous PDA-modified poly(lactic-co-glycolic acid) microspheres, which led to enhanced loading efficiency, an optimized release profile, and preserved bioactivity of the exosomes microspheres.78
Combination of PDA and Bioactive Natural Molecules Drugs for Tissue Repair
Many natural drugs are being discovered in the field of wound repair, but their diverse mechanisms of action require a powerful drug carrier with controlled release capabilities to carry out their effects. There have been many studies showing that PDAs have this capability.
Luteolin (LUT, a quorum sensing inhibitor) is a natural polyphenol flavonoid that exhibits promising characteristics as a natural drug for inhibiting the colony effect of bacterial biofilms. It demonstrates excellent capabilities in inhibiting and dispersing biofilms.97 Hu et al was loaded in PDA NPs to form PDA-LUT nanosystem.57 In response to the weak acidic environment of biofilm infections, LUT undergoes controlled release and selectively targets bacterial biofilms and pathogenic bacteria. This targeted action hinders the communication of bacterial quorum sensing signals, rendering them in a sensitive state.
Curcumin, a polyphenolic compound primarily extracted from the rhizome of turmeric, has been reported to alleviate injury through its anti-inflammatory, anti-oxidation, and free radical scavenging properties.98 In a study conducted by Chen et al, curcumin-loaded mesoporous PDA NPs were prepared and intratracheally administered to the lung for the prevention and treatment of radiation pneumonitis.99 The mesoporous structure of PDA offered a large inner space and numerous surface pores, resulting in high drug loading efficiency for curcumin. Additionally, the amorphous state of curcumin in PDA improved its dissolution and release, facilitating quick prevention and treatment upon pulmonary delivery.
The absence of a scientific drug-release system led to unstable drug release, resulting in the wastage of valuable Chinese herbal medicines and causing various discomforts to the patients. PDA as a highly binding material could provide a platform for the orderly release of many of these natural drugs.
PDA Applications for Building Controlled Drug Release Materials
Thermosensitive and Intelligent Drugs Delivery System Control by PTT Temperature-Response of PDA
To ensure effective and safe treatment of a damaged wound, it is crucial to design a drug release modulation system that allows for controlled release of the required medication. The approach taken for drug release modulation should be tailored to the specific drug being used, as different drugs have varying mechanisms of action and optimal release profiles.100 For instance, growth-promoting drugs may require a sustained release over an extended period, while antibiotics may need to be released fully and rapidly to achieve optimal efficacy. If the drug release is not properly controlled, there is a risk that the medication may be ineffective or even contribute to drug resistance. To achieve controlled drug release, researchers have developed various drug delivery systems that utilize pH, ultrasound, or near-infrared (NIR) laser stimuli. These systems enable a controllable release of bioactive components in response to specific triggers, enhancing the therapeutic efficacy and minimizing drug wastage.101 However, traditional drug delivery systems often lack sensitivity and have limited short-term release capabilities. Fortunately, PDA can offer several benefits in drug delivery. Not only can PDA increase the amount of drug adsorption, but its PTT properties also enable the controlled release and accumulation of drugs. Indeed, the incorporation of PDA in drug delivery systems can lead to localized temperature increases. This property can be utilized to increase the rate of drug diffusion or enable an on-off effect, which can be activated on demand by irradiating the sample with a specific stimulus, such as near-infrared (NIR) light. This controlled drug release mechanism holds great promise for targeted and efficient drug delivery applications.102,103 NIR irradiation has been shown to enhance antibiotic delivery, possibly due to physical interactions between the drug and the PDA that are sensitive to temperature changes. In fact, studies have demonstrated that the release rate of antibiotics dissolved in hydrogel with PDA under NIR is faster than without NIR.104 These findings suggest that PDA can play a critical role in the development of smart drug release control biomaterials.
Che et al designed a biomimetic and bioactive scaffold with intelligently pulsatile teriparatide delivery for local and systemic osteoporosis regeneration. They have utilized thermosensitive liposomes (TSLs) as temperature-reactive media.105 These TSLs can be easily controlled by temperature, allowing for stable drug retention at lower temperatures and rapid drug release at higher temperatures. This temperature-sensitive behavior offers a versatile and precise drug delivery mechanism that can be tailored to specific therapeutic needs.106 Moreover, when the temperature of the system rises above the transition temperature, the extravasation of TSLs is significantly enhanced, leading to an immediate and rapid release of payloads.107 This makes TSLs a promising candidate for controlled drug delivery, as they offer the ability to trigger drug release at the desired location and time by manipulating temperature. Liposomes are structures that can quickly recover to a dense form and remain stable with little drug release once the temperature drops below the transition temperature. In order to manage the TSLs reaction, PDA can be used as a heater under NIR, which can penetrate deep tissues and provide acute temperature control.108 Recent studies have shown that using this technique, drug release from TSLs can be pulsatile and closely aligned with the average release rate over a 14-day period, in contrast to groups without NIR control, which released 34.7% of drugs within the first two days. Another strategy for controlling drug release is to combine TSLs with materials that respond to the PTT temperature-stimulated response. Exactly, phase-change materials like lauric acid and stearic acid (PCM) can serve as thermal response “gatekeepers” in drug delivery systems. When these materials are combined with PDA and subjected to NIR irradiation, and the temperature rises above their melting point (39−40 °C), the PCM undergoes a gradual melting process. This temperature-triggered melting, in turn, sequentially triggers the release of antibiotic drugs that are concealed within the material, allowing for controlled and targeted drug delivery. This approach could offer new possibilities for developing targeted and effective drug delivery systems.30
Metal ions, particularly silver (Ag), have been extensively studied and have been shown to possess broad-spectrum bacteriostatic properties. Ag has been demonstrated to penetrate bacterial cell membranes, disrupt internal proteins and genetic material, and ultimately lead to bacterial death.109,110 Despite these advantages, the accumulation of metal ions and their cytotoxicity remains a significant concern as a potential side effect.111 Recent studies show different strategies benefit from the PTT property. In 2013, Zhang et al synthesized hybrid materials consisting of Ag NPs, PDA, and graphene nanosheets as a novel antibacterial material.112 Indeed, PDA exhibits excellent biocompatibility, which can help reduce the cytotoxicity of Ag+ and facilitate its combination with other materials.113 In a recent study by Yang et al, they developed a “Ag+ self-rechargeable” stubborn infected cutaneous nanofibrous membrane designed to recover released metal ions, which helps moderate their toxicity and replenish the antibacterial capacity of metal ion therapy. This innovative approach offers a sustainable and effective solution for combating bacterial infections while minimizing the harmful effects of metal ions on surrounding healthy tissues.114 They reach the metal ions self-rechargeable ability by combining PDA and photodynamic therapy (PDT, photosensitizers yield ROS under light irradiation with an accommodative wavelength) materials (Figure 4A–D). PDA’s redox-active catechol group undergoes spontaneous oxidation to quinone, which acts as a reducing agent to convert Ag+ ions to Ag0 NPs on the surface of PDA when exposed to moderate solution conditions (Figure 4C).115,116 Under NIR irradiation, the Ag NPs on the surface of PDA are oxidized back into Ag+ ions and subsequently released into the wound again (Figure 4B). This process ensures that the synergistic therapy remains potent and effective, while maintaining a rechargeable function to sustain the antibacterial capacity over time. The ability to recycle and reuse the released metal ions enhances the overall therapeutic efficacy and makes the system more practical for long-term applications (Figure 4D).
 |
Figure 4 (A) Illustration of the manufacturing procedure of the “self-rechargeable” membranes.114 (B) Diagram of the photothermal and photodynamic mechanism of the “self-rechargeable” system.114 (C) Antimicrobial and “self-rechargeable” effects.114 (D) In the “recycle-release” process, the “self-rechargeable” ability will gradually diminish, but PDA can slow this down significantly.114 Reproduced from Yang Y, Zhou X, Chan YK, et al. Photo-Activated Nanofibrous Membrane with Self-Rechargeable Antibacterial Function for Stubborn Infected Cutaneous Regeneration. Small. Mar 2022;18(12):e2105988.114 © 2022 Wiley-VCH GmbH. |
pH-Responsive Bacteria Reactive Biomaterials with PDA
Bacterial growth during wound infection can result in tissue hypoxia, leading to glycolysis and acidification of the surrounding environment. The pH of infected wounds can drop to approximately 5.5.117,118 The pH changes in infected wounds can be designed with a number of pH-responsive biomaterials for monitoring bacterial changes in wounds with PDA. Correct, PDA exhibits high sensitivity to acidic pH, which enables it to act as a switch for controlling drug release. In acidic environments, such as those found in certain disease sites or endosomes, PDA undergoes changes in its structure or properties, triggering the release of drugs from the carrier system. This pH-responsive behavior makes PDA an attractive candidate for targeted drug delivery, allowing for the release of drugs precisely at the intended site of action.119,120
When exposed to a weak alkaline environment at room temperature, DA can undergo spontaneous polymerization and form a PDA film. This PDA film can effectively encapsulate drugs, providing a versatile and simple method for drug delivery and controlled release applications.121 In the acidic microenvironment of biofilms with a pH below 6.0, the outer layer of PDA degrades. This degradation process exposes the inner drugs within the PDA film to bacteria present in the deeper layers of the biofilm (Figure 5A). The pH-responsive nature of this strategy allows for on-demand drug release in situ, precisely targeting the biofilm microenvironment, and facilitating biofilm dispersion. This pH-responsive approach holds great promise for combating bacterial infections associated with biofilms, as it enhances drug delivery efficiency and the therapeutic effect. This pH-responsive strategy is well-suited for on-demand drug release in situ and biofilm dispersion.61
 |
Figure 5 (A) Illustration of the pH-responsive nanocomposites (PDA@Kana-AgNP) coated with PDA based on kanamycin in combination with AgNPs. Reprinted from Colloids and Surface B: Biointerfaces, Volume 208, Li X, Li B, Liu R, Dong Y, Zhao Y, Wu Y. Development of pH-responsive nanocomposites with remarkably synergistic antibiofilm activities based on ultrasmall silver nanoparticles in combination with aminoglycoside antibiotics. Pages 112112.61 Copyright © 2021, with permission from Elsevier. (B) Bacterial infection triggers TCPP release to restore red fluorescence emission under illumination at 410 nm, and hydrogels generate antibacterial PDT under illumination at 660 nm. Hydrogels with wrapped bacterial debris are removed under illumination at 808 nm and changed into fresh hydrogel dressings to promote wound healing. Reproduced with permission from Ran P, Zheng H, Cao WX, et al. On-Demand Changeable Theranostic Hydrogels and Visual Imaging-Guided Antibacterial Photodynamic Therapy to Promote Wound Healing. Acs Appl Mater Inter. 2022.122 Copyright © 2022 American Chemical Society. (C) PES-release behavior from MPDA@ZIF-8/PES NPs at different pH without NIR irradiation.123 (D) PES-release behavior of MPDA@ZIF-8/PES NPs at different pH under NIR irradiation.123 Used with permission of the Royal Society of Chemistry from Peng D, Liu G, He Y, et al. Fabrication of a pH-responsive core-shell nanosystem with a low-temperature photothermal therapy effect for treating bacterial biofilm infection. Biomater Sci. 2021;9(22):7483–7491. 123 Copyright © 2021, permission conveyed through Copyright Clearance Center. |
A kind of pH-responsive bacteria monitoring wound hydrogel was developed by Ran et al using Tetrakis(4-carboxyphenyl)porphyrin (TCPP) and PDA122 (Figure 5B). TCPP generates a strong red fluorescence, but under physiological conditions, the fluorescence of TCPP is quenched by PDA NPs. However, in the acidic microenvironment of bacterial infection, TCPP is released from PDA NPs, leading to the restoration of fluorescence emissions, which enables real-time diagnosis under 410 nm illumination.124
Peng et al developed a pH-responsive core-shell nanosystem designed to exhibit a low-temperature photothermal therapy (PTT) effect to treat bacterial biofilm-infection. This innovative nanosystem demonstrates effective potential in treating bacterial biofilm infections. The pH-responsive nature of the nanosystem allows for controlled drug release in acidic microenvironments, while the low-temperature PTT effect enhances its therapeutic efficacy against biofilm-associated infections.123 Pifithrin-μ (PES) is a heat-shock protein inhibitor. In their research, Peng et al proposed integrating PES into the PTT system. They hypothesized that by doing so, the inclusion of PES could reduce the tolerance of bacteria to heat, consequently decreasing the temperature required for PTT to eliminate biofilms. This approach aims to enhance the treatment efficacy of bacterial infections by making the PTT system more effective in eradicating biofilms. They prepared zeolite-based imidazole framework (ZIF-8)-coated PDA core–shell NPs and then loaded PES. ZIF-8 is a type of pH-responsive metal–organic framework. It remains stable in physiological environments but degrades in an acidic environment. This degradation leads to the release of zinc ions, which can have various therapeutic effects and applications in drug delivery, tissue engineering, and other biomedical fields. The pH-responsive behavior of ZIF-8 makes it a promising candidate for targeted drug delivery and controlled release systems that can selectively release drugs in response to the acidic microenvironment of specific disease sites (Figure 5C and D). The outer shell ZIF-8 was used to load PES. The release of PES could be achieved by the degradation of the outer shell under the stimulation of the acidic environment caused by bacterial infection. Then, the released PES acted on the biofilm and reduced the heat tolerance of the bacteria in the biofilm. Therefore, through the combined action of PES and localized PTT stimulation, the biofilms were effectively ablated, and the bacteria were eliminated. This innovative approach allowed for low-temperature PTT, making it a promising strategy for the treatment of bacterial biofilm infections.
Multi-Layers Structure Tissue Regeneration Biomaterials with PDA
Tissue regeneration is a complex process that requires biomaterials to meet various demands, including moistness, cell adhesion, water absorption, and drug chelation. It is challenging for individual materials to possess all of these characteristics simultaneously. Therefore, the current approach is to combine different materials and optimize their interaction to achieve proper tissue regeneration. When modifying the surface of inert and non-bioactive tissue repair materials, a single biomaterial modification may not achieve the desired effect. Multiple modifications or the combination of different modification strategies may be necessary to achieve the desired properties.125 To achieve the desired properties, layer-by-layer (LBL), core-shell, multi-layers, sandwich-like, and other techniques have been developed to layer different materials in an orderly fashion.126–128 Among these techniques, the PDA coating has garnered more attention as a surface modification due to its essential roles in multilayer structures.129–131
Layer-by-Layer Structure
LBL assembly, a highly promising technique, involves the fabrication of thin multilayer coatings through the electrostatic mutual attraction of oppositely charged polyelectrolytes. This approach allows for precise control over the coating thickness and composition, making it an attractive option for various applications, including drug delivery, tissue engineering, and surface modification.132,133 Yin et al successfully modified the surface of high-density polyethylene (HDPE) using three different functional biomaterials through LBL modification.125 They used PDA as an adhesive material to modify the surface of 3D-printed HDPE scaffold as the base layer, providing a platform for further LBL modification with bioactive factors. ε-Polylysine (EPL), a small antibacterial cationic peptide with a large positive charge, and fibrin, essential for vascular and endothelial tissue regeneration with a small negative charge, were used as the subsequent layers.134–137 EPL was able to react with the amino groups of the PDA layer to form the EPL layer, and the EPL and fibrin LBL coating was successfully generated through the interaction resulting from the electrostatic absorption principle.138 For LBL modification on titanium implants, Zhao et al found that using PDA as the base layer resulted in an interconnected network of type I collagen (COL1) on the surface, with a higher COL1 content and satisfactory layer stability compared to the group without the PDA basement.139
Sandwich-Like Structure
Wu et al utilized a sandwich structure consisting of PDA and carboxymethyl chitosan (CCS) layers to achieve long-term stable delivery of bone morphogenetic protein BML-284 (BML).126 The PDA layer serves as a platform for immobilizing BML via Schiff base formation and physical adsorption, as well as electrostatic and chemical interactions between the PDA and the –NH2 of BML. The CCS layer contains carboxymethyl groups that are negatively charged and can interact electrostatically with positively charged drugs such as BML.140 This allows the BML to be released from the hybrid films in a controlled manner, with its release further restricted within the scaffold for sustained delivery through the combined electrostatic and chemical interactions between BML and CCS. This approach has great potential for achieving long-term stable delivery of various bioactive factors in tissue regeneration applications.
Core-Shell Sturcture
Polypyrrole (PPy) is a typical conductive polymer. Recently, the incorporation of PPy-PDA NPs has been shown to enhance the PTT conversion capacity of scaffolds, leading to improved sterilization efficacy.141 Electrospun poly(l-lactide) (PLLA) nanofibers have been widely used in various tissues regeneration but limited by its poor hydrophilicity.142–145 Therefore, Xiong et al made a core-shell structure to fix the PLLA shortcoming and add PPy functions.128 PDA modification of PLLA fibers, when polymerized in situ, can act as an effective binder between PPy and PLLA, while also synergistically enhancing the hydrophilicity, biocompatibility, and endogenous conductivity of composite materials.
Self-Healing and Shape-Memory PDA Biomaterials
The self-repairing ability of hydrogels can help maintain the material’s integrity at the wound site, which is crucial in preventing foreign material from entering the wound and causing infection.146 Moreover, self-healing hydrogels can adapt to the wound’s shape and provide a scaffold for new tissue growth.147 The self-healing property of hydrogels is accomplished by reassociating catechol groups via dynamic Schiff bonds, π-π stacking, and hydrogen bonding interactions between polymer chains.148 PDA is enriched with diverse functional groups, including benzene rings, catechol, and amine groups, enabling it to establish a wide range of interactions with the polymer matrix. These interactions comprise both covalent and noncovalent bonding, such as hydrogen bonds, coordination, and π–π stacking.149 Certainly, the incorporation of PDA into hydrogels or polyurethane offers a valuable means of enhancing their mechanical properties. This is attributed to the intermolecular interactions facilitated by PDA, which aid in effective energy dissipation during tensile deformation. As a result, the materials exhibit improved toughness and resistance to mechanical stress. This property renders PDA a promising component for various engineering and biomedical applications, where superior mechanical performance is essential.150,151
Rao et al successfully combined PDA and CCS to develop a self-healing wound hydrogel.148 The presence of amino groups in CCS chains enables them to react with the aldehyde functional groups of other polymers, forming dynamic Schiff base bonds that contribute to the material’s self-healing ability.152 The self-healing ability of 0.4 wt% of DA-CCS hydrogels was achieved at room temperature within 2 hours, where the hydrogel was cut into two halves and rejoined automatically within this time frame.
In another study, Dai et al designed a novel shape memory polyurethane based on PDA and polycaprolactone (PCL) prepolymer, which was responsive to NIR light (Figure 6A and B).153 PCL is a widely used synthetic polymer in biomedical applications due to its low melting temperature (around 50 °C) and excellent biocompatibility.154 The phenolic hydroxyl groups in PDA NPs participated in the chain extension reaction with the isocyanate bonds of PCL to obtain higher dispersibility, which prevented any reduction in mechanical properties or conversion efficiency.155 The PCL-PDA polyurethanes were softened at 46 °C and shaped into a specific form, which was then fixed in an ice water bath (Figure 6A). Upon exposure to a 46 °C water bath, the material was able to recover its original shape. This novel shape memory polyurethane could be controlled using NIR light to transfer heat and regulate temperature to control shape (Figure 6B).
 |
Figure 6 (A) PCL–PDA 1 was wound on a round rod at 60 °C and then submerged in an ice water bath for 5 min to obtain a spiral shape. At last, the sample was placed in a 60 °C water bath, and it recovered its permanent shape.153 (B) Digital photos of NIR light-triggered shape memory behavior of PCL–PDA 1 polyurethane in vitro and in vivo.153 Reproduced with permission from Dai S, Yue S, Ning Z, Jiang N, Gan Z. Polydopamine Nanoparticle-Reinforced Near-Infrared Light-Triggered Shape Memory Polycaprolactone-Polydopamine Polyurethane for Biomedical Implant Applications. ACS Appl Mater Interfaces. 2022;14(12):14668–14676.153 Copyright © 2022 American Chemical Society. |
PDA Absorbs Some of the Inflammatory Factors at the Site of Injury
PDA as Cell Free DNA Scavenger in Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune disease that differs from other bone injuries such as bone fractures, bone defects, and bone tumors. Accumulating evidence suggests that cell-free DNA is a major factor in the development of RA,156,157 making the scavenging of cell-free DNA a promising approach for treating this disease. However, the use of cationic nanoparticles for this purpose has been limited by their high cytotoxicity.158 PDA has been shown to be an effective gene binding nanocarrier with low toxicity.159 Chen et al have developed an injectable PDA-based nanoparticle system for scavenging cell-free DNA in joints (Figure 7A). The abundant catechol and imine groups of the NPs were first activated by 1,1’-carbonyldiimidazole and then modified with dimethylamino groups (DP-M or DP-B) with varying charge density, by reacting with amino groups of 3-dimethylamino-1-propylamine (M) or 3,3-iminobis(N,N-dimethylaminopropyl) (B), to bind negatively charged cell-free DNA. Cytotoxicity tests showed that the PDA NPs exhibited almost no cytotoxicity, and at concentrations below 100 μg/mL, they showed protective effects against LPS-induced cells by preventing inflammation. The concentration of cell-free DNA in the serum of healthy individuals was found to be only 9 μg/mL, whereas it increased sharply to 52 μg/mL in the RA model group. However, after treatment with PDA NPs, the concentration of cell-free DNA remained high (33 μg/mL), but it was almost close to normal levels in the RA+DP-B group (13 μg/mL).160 This suggests that PDA-based NPs can scavenge cell-free DNA and thus have potential as a therapeutic modality for RA.
 |
Figure 7 (A) Schematic illustration of in vivo RA therapy effect of dimethylamino group (3- dimethylamino- 1- propylamine (M) or 3, 3- iminobis (N, N- dimethylaminopropyl) (B)) modified polydopamine (DPs). The DPs were intra articular (IA) injected into the knee joint of CIA rat and strongly bound with cfDNA to lower the expression of inflammatory factors: MMP-13, TNF-α, IL-6 and IL-1β for RA therapy. Reproduced from Chen Y, Wang Y, Jiang X, et al. Dimethylamino group modified polydopamine nanoparticles with positive charges to scavenge cell-free DNA for rheumatoid arthritis therapy. Bioact Mater. 2022;18:409–420. 160 Copyright © 2022 KeAi, open access. (B) Schematic illustration of PDA@MF NPs treatment for ROS-related kidney diseases.161 (C) Bio-distribution of PDA NPs and PDA@MF NPs was examined via in vivo imaging instruments.161 (D) H&E analysis of kidneys in different groups.161 Adapted from Zheng B, Deng G, Zheng J, et al. Self-polymerized polydopamine-based nanoparticles for acute kidney injury treatment through inhibiting oxidative damages and inflammatory. Int J Biochem Cell Biol. 2022;143:106141. 161 Copyright © 2022, with permission from Elsevier. |
PDA as ROS Scavenger
Uncontrolled inflammatory responses triggered by pathogens can lead to excessive production of ROS, which in turn can result in chronic or non-healing wounds. Thankfully, antioxidants can effectively inhibit alveolar bone resorption by attenuating the excessive production of ROS.162,163 Traditional natural enzymes often function as ROS scavengers, but their poor stability and potential high-dose toxicity pose significant obstacles in preventing ROS-related diseases. As an alternative, PDA has emerged as a promising antioxidant for various therapeutic applications, such as periodontal disease, skin lesions, and ischemic stroke. Its use addresses the limitations associated with traditional enzymes, making it a potential solution for ROS-related conditions.19,164,165
Li et al design a high efficiency ROS eliminate system.166 The elimination of ROS is accomplished by the catechol groups present in PDA, which are converted to quinone groups. Additionally, PDA-reduced GO facilitates electron transfer to the quinone groups, leading to the reduction of quinone groups back to catechol groups. This process enables PDA to continuously remove ROS generated by wound tissue.
Pharmacological inhibitors or siRNA targeting mTOR have been demonstrated to effectively reduce ROS formation and mitigate proinflammatory processes.167 Shi et al loaded rapamycin (Rapa) which is an inhibitor of mTOR and PDA into PDA to construct mPDA@Rapa for the treatment of Spinal cord injury (SCI).168 Both the mPDA group and mPDA@Rapa group exhibited significantly reduced ROS levels, which can be attributed to the ROS scavenging ability of mPDA. Additionally, in the Rapa and mPDA@Rapa treated groups, the expression of mTOR protein decreased. Consequently, the ROS level in the Rapa group also showed a slight reduction due to the inhibition of mTOR by Rapa. Therefore, PDA not only possesses strong ROS scavenging ability by itself, but also can be combined with other drugs to obtain stronger anti-ROS effect.
PDA Related Biomaterial for Internal Organ Repairment
Acute kidney injury (AKI) is a sudden episode of kidney failure or kidney damage, which triggers a series of biological events including excessive production of ROS and hypoxia.161 To address this, Zheng et al developed PDA NPs for scavenging excessive ROS and producing oxygen in AKI (Figure 7B). They used biocompatible manganese ferrite (MF) NPs as treatment agents to continuously generate oxygen in the inflammatory area. Although it is challenging to apply biomaterials to internal organs, PDA-related biomaterials have shown great ROS scavenging properties in acute peritonitis and acute lung injury, suggesting their potential for use in other internal organs (Figure 7C). The MF NPs were verified to be 5 nm in size and were dispersed into DA hydrochloride solution to construct PDA-encapsulated MF nanocomposites (PDA@MF). The PDA@MF NPs were monodispersed and had an average diameter of 140 nm. The researchers evaluated the kidney function of an AKI mouse model after PDA@MF NPs treatment and found that both plasma creatinine and blood urea nitrogen levels were significantly decreased compared with the control group. The pathological situation was greatly alleviated with the addition of PDA@MF NPs, suggesting PDA@MF NPs contributed to the maintaining of renal tissue integrity (Figure 7D). Additionally, PDA@MF NPs were mainly accumulated in the lung, liver, and kidney but negligible in other organs (such as the heart and spleen), suggesting the potential of PDA in the treatment of lung and liver diseases as well.161 These results show that PDA also has the potential to play roles in lung and liver diseases.
Conclusion and Prospect
In conclusion, PDA is a versatile material with a wide range of functions and immense potential in wound and tissue regeneration. Its diverse properties and abilities offer promising avenues for designing more sophisticated and intelligent tissue repair materials.
Powerful Bonding and Adhesion Allow for a Wide Range of PDA Applications
In recent years, PDA has been frequently utilized as an auxiliary material to complement the properties of the primary materials in tissue repair designs. Its strong bonding capabilities enable seamless integration with various types of materials without compromising their individual performance. PDA’s exceptional binding and adhesion properties make it a versatile component, facilitating its combination with a diverse range of materials in various tissue repair applications. Despite the array of materials available for tissue repair, PDA stands out for its ability to modify these materials and fulfill its role by simply integrating with them.
First and foremost, PDA can serve as a surface modifier for other non-biologically active materials, such as PEEK and metal. Through PDA modification, the surfaces of these materials can be improved, enhancing their surface properties.169,170 Secondly, the incorporation of PDA also opens up opportunities to develop drug release systems. By utilizing PDA as a carrier or modifier, controlled drug release can be achieved, enhancing the therapeutic efficacy of wound repair materials. Thirdly, the versatility of PDA allows it to be combined with various materials, enabling the creation of multi-layered structures and the design of more intricate wound repair materials. Fourthly, materials combined with PDA demonstrate robust self-healing capabilities, making them better suited to withstand the challenges of complex wound environments. Incorporating PDA in the design of new materials holds the promise of harnessing its beneficial properties for tissue repair applications.
PDA Can Be Used for the Design of Drug-Controlled Release Systems
Silver ions are a powerful antimicrobial material, but they also have some cytotoxicity. Controlling their release is currently the key to balancing the antimicrobial activity and toxicity of silver-based materials. The combination of materials such as PDA and MXene can provide more design ideas for controlling silver ion release systems.171 The strategy of combining PDA and metal ion materials is also applied to the disinfection of water bodies.172,173 The design ideas of materials in different fields may bring new inspiration to the design of wound antimicrobial materials.
The PTT capability of PDA enables the design of light-controlled drug release materials. By converting near-infrared (NIR) light energy into heat energy, PDA enhances drug release capacity and provides control over the drug release process. Moreover, PDA can be combined with temperature-responsive materials, like hot-melt materials, which melt at elevated temperatures, facilitating drug release concurrently. Additionally, PDA’s pH responsiveness enables it to control drug release in response to changes in pH levels. These versatile strategies offer promising avenues for designing intelligent and precise drug release systems for tissue repair applications.
PDA Can Be Used for in vivo Organ Repair
The application of drugs to open injuries in organs is relatively straightforward, but using repair materials on visceral tissues has posed challenges. PDA, with its potential for intravenous administration, can accumulate in organs such as the lung, liver, and kidney. Thus, PDA holds promise for addressing tissue damage in these organs. Additionally, local injection of PDA shows potential for treating neurological disorders like SCI. However, the safety of PDA for repairing visceral organ damage needs further validation. Questions regarding the degradation of PDA, potential embolism formation, and the possibility of new complications arising from its presence in the body remain to be addressed through comprehensive studies.
Prospect
It has been few decades that mussel-inspired materials come into scientists’ sight. While a few mussel-inspired materials, like mussel adhesive protein, have found their way into daily skin care and superficial clinical applications, their widespread adoption is hindered by production limitations and material complexity. Extracting MAP from natural sources or producing it through biological fermentation yields relatively low quantities, making it impractical for large-scale applications. Additionally, the intricate nature of mussel-inspired biomaterials for tissue repair and regeneration poses challenges for manufacturing and real-world clinical use. PDA, on the other hand, emerges as a promising alternative due to its ease of production and low cost. Its potential extends beyond that of natural mussel-inspired materials, making it a viable replacement in certain areas. Scientific research often explores the realm of possibilities, while medical products must prioritize practicality, production feasibility, and extensive clinical trials. With hundreds of published studies on PDA, there is ample reason to believe that with sufficient time and investment, PDA could revolutionize clinical treatments for a wide range of patients.
Abbreviations
PDA, Polydopamine; DOPA, 3,4-dihydroxy-l-phenylalanine; DA, Dopamine; NPs, Nanoparticles; PTT, Photothermal; HA, Hyaluronic acid; GO, Graphene oxide; CMCHm-PDA, Carboxymethyl chitin microspheres with PDA; BMP-2, Bone Morphogenetic Protein-2; ROS, Reactive oxygen species; PDAH, PDA with heparin; PEEK, Polyetheretherketone; TA, Tannic acid; LUT, Luteolin; NIR, Near infrared; TSLs, Thermosensitive liposomes; PCM, Phase-change material; Ag, Sliver; PDT, Photodynamic therapy; TCPP, Tetrakis(4-carboxyphenyl)porphyrin; PES, Pifithrin-μ; ZIF-8, Zeolite-based imidazole framework; LBL, Layer-by-layer; HDPE, High-density polyethylene; EPL, ε-Polylysine; COL1, Type I collagen; CCS, Carboxymethyl chitosan; BML, BML-284; PPy, Polypyrrole; PLLA, Poly(l-lactide); PCL, Polycaprolactone; RA, Rheumatoid arthritis; Rapa, Rapamycin; SCI, Spinal cord injury; AKI, Acute kidney injury; MF, Manganese ferrite.
Acknowledgement
This work was supported by grants from National Natural Science Foundation of China (No. 82172206), Zhejiang Provincial Medical and Healthy Science Foundation of China (No. 2023RC183 and 2024KY110). We thank Xiaoli Hong and Chao Bi from the Core Facilities, Zhejiang University School of Medicine for their technical support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Deng X, Gould M, Ali MA. A review of current advancements for wound healing: biomaterial applications and medical devices. J Biomed Mater Res B Appl Biomater. 2022;110(11):2542–2573. doi:10.1002/jbm.b.35086
2. Babilotte J, Guduric V, Le Nihouannen D, Naveau A, Fricain JC, Catros S. 3D printed polymer-mineral composite biomaterials for bone tissue engineering: fabrication and characterization. J Biomed Mater Res B Appl Biomater. 2019;107(8):2579–2595. doi:10.1002/jbm.b.34348
3. Jiang BG, Han N, Rao F, Wang YL, Kou YH, Zhang PX. Advance of peripheral nerve injury repair and reconstruction. Chin Med J. 2017;130(24):2996–2998. doi:10.4103/0366-6999.220299
4. Zhang Q, Liu Y, Li J, Wang J, Liu C. Recapitulation of growth factor-enriched microenvironment via BMP receptor activating hydrogel. Bioact Mater. 2023;20:638–650. doi:10.1016/j.bioactmat.2022.06.012
5. Zhang W, Yu M, Cao Y, et al. An anti-bacterial porous shape memory self-adaptive stiffened polymer for alveolar bone regeneration after tooth extraction. Bioact Mater. 2023;21:450–463. doi:10.1016/j.bioactmat.2022.08.030
6. Chen Q, Nan Y, Yang Y, et al. Nanodrugs alleviate acute kidney injury: manipulate RONS at kidney. Bioact Mater. 2023;22:141–167. doi:10.1016/j.bioactmat.2022.09.021
7. Jin J, Liu Y, Jiang C, et al. Arbutin-modified microspheres prevent osteoarthritis progression by mobilizing local anti-inflammatory and antioxidant responses. Mater Today Bio. 2022;16:100370. doi:10.1016/j.mtbio.2022.100370
8. Liu Z, Tang Q, Liu RT, et al. Laponite intercalated biomimetic multilayer coating prevents glucocorticoids induced orthopedic implant failure. Bioact Mater. 2023;22:60–73. doi:10.1016/j.bioactmat.2022.09.013
9. Taghizadeh A, Taghizadeh M, Yazdi MK, et al. Mussel-inspired biomaterials: from chemistry to clinic. Bioeng Transl Med. 2022;7(3):e10385. doi:10.1002/btm2.10385
10. Cavallini C, Vitiello G, Adinolfi B, et al. Melanin and melanin-like hybrid materials in regenerative medicine. Nanomaterials. 2020;10(8):1518. doi:10.3390/nano10081518
11. Miller DR, Spahn JE, Waite JH. The staying power of adhesion-associated antioxidant activity in mytilus californianus. J R Soc Interface. 2015;12(111):20150614. doi:10.1098/rsif.2015.0614
12. Kord Forooshani P, Lee BP. Recent approaches in designing bioadhesive materials inspired by mussel adhesive protein. J Polym Sci a Polym Chem. 2017;55(1):9–33. doi:10.1002/pola.28368
13. Liu Y. Design of Robust Hydrogel Based on Mussel-Inspired Chemistry. Michigan Technological University; 2017.
14. Haining RL, Achat-Mendes C. Neuromelanin, one of the most overlooked molecules in modern medicine, is not a spectator. Neural Regen Res. 2017;12(3):372–375. doi:10.4103/1673-5374.202928
15. d’Ischia M, Wakamatsu K, Cicoira F, et al. Melanins and melanogenesis: from pigment cells to human health and technological applications. Pigm Cell Melanoma Res. 2015;28(5):520–544. doi:10.1111/pcmr.12393
16. Danner EW, Kan Y, Hammer MU, Israelachvili JN, Waite JH. Adhesion of mussel foot protein Mefp-5 to mica: an underwater superglue. Biochemistry. 2012;51(33):6511–6518. doi:10.1021/bi3002538
17. Kalia S, Zhao J, Zeng H, McLean D, Kollias N, Lui H. Melanin quantification by in vitro and in vivo analysis of near-infrared fluorescence. Pigm Cell Melanoma Res. 2018;31(1):31–38. doi:10.1111/pcmr.12624
18. Ou-Yang H, Stamatas G, Kollias N. Spectral responses of melanin to ultraviolet A irradiation. J Invest Dermatol. 2004;122(2):492–496. doi:10.1046/j.0022-202X.2004.22247.x
19. Liu Y, Ai K, Ji X, et al. Comprehensive insights into the multi-antioxidative mechanisms of melanin nanoparticles and their application to protect brain from injury in ischemic stroke. J Am Chem Soc. 2017;139(2):856–862. doi:10.1021/jacs.6b11013
20. Panzella L, Gentile G, D’Errico G, et al. Atypical structural and pi-electron features of a melanin polymer that lead to superior free-radical-scavenging properties. Angew Chem Int Ed Engl. 2013;52(48):12684–12687. doi:10.1002/anie.201305747
21. Zucca FA, Segura-Aguilar J, Ferrari E, et al. Interactions of iron, dopamine and neuromelanin pathways in brain aging and Parkinson’s disease. Prog Neurobiol. 2017;155:96–119. doi:10.1016/j.pneurobio.2015.09.012
22. Hong S, Zhang QL, Zheng DW, et al. Enzyme mimicking based on the natural melanin particles from human hair. iScience. 2020;23(1):100778. doi:10.1016/j.isci.2019.100778
23. Roy S, Rhim J-W. Agar-based antioxidant composite films incorporated with melanin nanoparticles. Food Hydrocoll. 2019;94:391–398. doi:10.1016/j.foodhyd.2019.03.038
24. Ma H, Zhou Q, Chang J, Wu C. Grape seed-inspired smart hydrogel scaffolds for melanoma therapy and wound healing. ACS Nano. 2019;13(4):4302–4311. doi:10.1021/acsnano.8b09496
25. Lee H, Dellatore SM, Miller WM, Messersmith PB. Mussel-inspired surface chemistry for multifunctional coatings. Science. 2007;318(5849):426–430. doi:10.1126/science.1147241
26. Pennisi P, Salehinejad MA, Corso AM, Merlo EM, Avenanti A, Vicario CM. Delay discounting in parkinson’s disease: a systematic review and meta-analysis. Behav Brain Res. 2023;436:114101. doi:10.1016/j.bbr.2022.114101
27. Wang Y, Chen L, Ren DY, et al. Mussel-inspired collagen-hyaluronic acid composite scaffold with excellent antioxidant properties and sustained release of a growth factor for enhancing diabetic wound healing. Mater Today Bio. 2022;15:100320. doi:10.1016/j.mtbio.2022.100320
28. Yuan Z, Lin C, Dai L, et al. Near-infrared light-activatable dual-action nanoparticle combats the established biofilms of methicillin-resistant Staphylococcus aureus and its accompanying inflammation. Small. 2021;17(13):e2007522. doi:10.1002/smll.202007522
29. Ma K, Dong P, Liang M, Yu S, Chen Y, Wang F. Facile assembly of multifunctional antibacterial nanoplatform leveraging synergistic sensitization between silver nanostructure and vancomycin. ACS Appl Mater Interfaces. 2020;12(6):6955–6965. doi:10.1021/acsami.9b22043
30. Zeng WN, Wang D, Yu QP, et al. Near-infrared light-controllable multifunction mesoporous polydopamine nanocomposites for promoting infected wound healing. ACS Appl Mater Interfaces. 2022;14(2):2534–2550. doi:10.1021/acsami.1c19209
31. Yazdi MK, Zare M, Khodadadi A, et al. Polydopamine biomaterials for skin regeneration. ACS Biomater Sci Eng. 2022;8(6):2196–2219. doi:10.1021/acsbiomaterials.1c01436
32. Tolabi H, Bakhtiary N, Sayadi S, et al. A critical review on polydopamine surface-modified scaffolds in musculoskeletal regeneration. Front Bioeng Biotechnol. 2022;10:1008360. doi:10.3389/fbioe.2022.1008360
33. Zheng D, Huang C, Zhu X, Huang H, Xu C. Performance of polydopamine complex and mechanisms in wound healing. Int J Mol Sci. 2021;22(19). doi:10.3390/ijms221910563
34. Chen CT, Martin-Martinez FJ, Jung GS, Buehler MJ. Polydopamine and eumelanin molecular structures investigated with ab initio calculations. Chem Sci. 2017;8(2):1631–1641. doi:10.1039/c6sc04692d
35. Saiz-Poseu J, Mancebo-Aracil J, Nador F, Busque F, Ruiz-Molina D. The chemistry behind catechol-based adhesion. Angew Chem Int Ed Engl. 2019;58(3):696–714. doi:10.1002/anie.201801063
36. Wheat JC, Wolf JS Jr. Advances in bioadhesives, tissue sealants, and hemostatic agents. Urol Clin North Am. 2009;36(2):265–75, x. doi:10.1016/j.ucl.2009.02.002
37. Radosevich M, Goubran HI, Burnouf T. Fibrin sealant: scientific rationale, production methods, properties, and current clinical use. Vox Sang. 1997;72(3):133–143. doi:10.1046/j.1423-0410.1997.7230133.x
38. Joch C. The safety of fibrin sealants. Cardiovasc Surg. 2003;11:23–28. doi:10.1016/S0967-2109(03)00068-1
39. Ennker J, Ennker IC, Schoon D, et al. The impact of gelatin-resorcinol glue on aortic tissue - a histomorphologic evaluation. J Vasc Surg. 1994;20(1):34–43. doi:10.1016/0741-5214(94)90173-2
40. Furst W, Banerjee A. Release of glutaraldehyde from an albumin-glutaraldehyde tissue adhesive causes significant in vitro and in vivo toxicity. Ann Thorac Surg. 2005;79(5):1522–1529. doi:10.1016/j.athoracsur.2004.11.054
41. Fan C, Fu J, Zhu W, Wang DA. A mussel-inspired double-crosslinked tissue adhesive intended for internal medical use. Acta Biomater. 2016;33:51–63. doi:10.1016/j.actbio.2016.02.003
42. Chen W, Wang R, Xu TT, et al. A mussel-inspired poly(gamma-glutamic acid) tissue adhesive with high wet strength for wound closure. J Mater Chem B. 2017;5(28):5668–5678. doi:10.1039/c7tb00813a
43. Pandey N, Soto-Garcia L, Yaman S, et al. Polydopamine nanoparticles and hyaluronic acid hydrogels for mussel-inspired tissue adhesive nanocomposites. Biomater Adv. 2022;134:112589. doi:10.1016/j.msec.2021.112589
44. Leng F, Chen F, Jiang X. Modified porous carboxymethyl chitin microspheres by an organic solvent-free process for rapid hemostasis. Carbohydr Polym. 2021;270:118348. doi:10.1016/j.carbpol.2021.118348
45. Zhang X, Sun GH, Tian MP, et al. Mussel-inspired antibacterial polydopamine/chitosan/temperature-responsive hydrogels for rapid hemostasis. Int J Biol Macromol. 2019;138:321–333. doi:10.1016/j.ijbiomac.2019.07.052
46. Liu C, Yao W, Tian M, Wei J, Song Q, Qiao W. Mussel-inspired degradable antibacterial polydopamine/silica nanoparticle for rapid hemostasis. Biomaterials. 2018;179:83–95. doi:10.1016/j.biomaterials.2018.06.037
47. Li G, Liang Y, Xu C, et al. Polydopamine reinforced hemostasis of a graphene oxide sponge via enhanced platelet stimulation. Colloids Surf B Biointerfaces. 2019;174:35–41. doi:10.1016/j.colsurfb.2018.10.074
48. Shin M, Park S-G, Oh B-C, et al. Complete prevention of blood loss with self-sealing haemostatic needles. Nat Mater. 2017;16(1):147–152. doi:10.1038/nmat4758
49. Liu C, Liu X, Liu C, et al. A highly efficient, in situ wet-adhesive dextran derivative sponge for rapid hemostasis. Biomaterials. 2019;205:23–37. doi:10.1016/j.biomaterials.2019.03.016
50. Sigal A, Martin A, Ong A. Availability and use of hemostatic agents in prehospital trauma patients in pennsylvania translation from the military to the civilian setting. Open Access Emerg Med. 2017;9:47–52. doi:10.2147/OAEM.S134657
51. Liang Y, Xu C, Liu F, Du S, Li G, Wang X. Eliminating heat injury of zeolite in hemostasis via thermal conductivity of graphene sponge. ACS Appl Mater Interfaces. 2019;11(27):23848–23857. doi:10.1021/acsami.9b04956
52. Zhang H, Fan T, Chen W, Li Y, Wang B. Recent advances of two-dimensional materials in smart drug delivery nano-systems. Bioact Mater. 2020;5(4):1071–1086. doi:10.1016/j.bioactmat.2020.06.012
53. Gong M, Liu C, Liu C, et al. Biomimetic hydroxyapate/polydopamine composites with good biocompatibility and efficiency for uncontrolled bleeding. J Biomed Mater Res B Appl Biomater. 2021;109(11):1876–1892. doi:10.1002/jbm.b.34849
54. Kozen BG, Kircher SJ, Henao J, Godinez FS, Johnson AS. An alternative hemostatic dressing: comparison of CELOX, HemCon, and QuikClot. Acad Emerg Med. 2008;15(1):74–81. doi:10.1111/j.1553-2712.2007.00009.x
55. Cao S, Yang Y, Zhang S, Liu K, Chen J. Multifunctional dopamine modification of green antibacterial hemostatic sponge. Mater Sci Eng C Mater Biol Appl. 2021;127:112227. doi:10.1016/j.msec.2021.112227
56. Li M, Zhang Z, Liang Y, He J, Guo B. Multifunctional tissue-adhesive cryogel wound dressing for rapid nonpressing surface hemorrhage and wound repair. ACS Appl Mater Interfaces. 2020;12(32):35856–35872. doi:10.1021/acsami.0c08285
57. Hu J, Ding Y, Tao B, et al. Surface modification of titanium substrate via combining photothermal therapy and quorum-sensing-inhibition strategy for improving osseointegration and treating biofilm-associated bacterial infection. Bioact Mater. 2022;18:228–241. doi:10.1016/j.bioactmat.2022.03.011
58. Dong Q, Liang X, Chen F, et al. Injectable shape memory hydroxyethyl cellulose/soy protein isolate based composite sponge with antibacterial property for rapid noncompressible hemorrhage and prevention of wound infection. Int J Biol Macromol. 2022;217:367–380. doi:10.1016/j.ijbiomac.2022.07.051
59. Guo Z, Zhang Z, Zhang N, et al. A Mg(2+)/polydopamine composite hydrogel for the acceleration of infected wound healing. Bioact Mater. 2022;15:203–213. doi:10.1016/j.bioactmat.2021.11.036
60. Deng Y, Shi J, Chan YK, et al. Heterostructured metal-organic frameworks/polydopamine coating endows polyetheretherketone implants with multimodal osteogenicity and photoswitchable disinfection. Adv Healthc Mater. 2022;11(14):e2200641. doi:10.1002/adhm.202200641
61. Li X, Li B, Liu R, Dong Y, Zhao Y, Wu Y. Development of pH-responsive nanocomposites with remarkably synergistic antibiofilm activities based on ultrasmall silver nanoparticles in combination with aminoglycoside antibiotics. Colloids Surf B Biointerfaces. 2021;208:112112. doi:10.1016/j.colsurfb.2021.112112
62. Sun H, Dong J, Wang YYF, et al. Polydopamine-Coated Poly(L-lactide) nanofibers with controlled release of VEGF and BMP-2 as a regenerative periosteum. Acs Biomater Sci Eng. 2021;7(10):4883–4897. doi:10.1021/acsbiomaterials.1c00246
63. Chen J, Wu J, Mu J, et al. An antioxidative sophora exosome-encapsulated hydrogel promotes spinal cord repair by regulating oxidative stress microenvironment. Nanomedicine. 2023;47:102625. doi:10.1016/j.nano.2022.102625
64. Eawsakul K, Tancharoen S, Nasongkla N. Combination of dip coating of BMP-2 and spray coating of PLGA on dental implants for osseointegration. J Drug Deliv Sci Tec. 2021;61. doi:10.1016/j.jddst.2020.102296
65. Hettiaratchi MH, O’Meara MJ, Teal CJ, Payne SL, Pickering AJ, Shoichet MS. Local delivery of stabilized chondroitinase ABC degrades chondroitin sulfate proteoglycans in stroke-injured rat brains. J Control Release. 2019;297:14–25. doi:10.1016/j.jconrel.2019.01.033
66. Shadish JA, Benuska GM, DeForest CA. Bioactive site-specifically modified proteins for 4D patterning of gel biomaterials. Nat Mater. 2019;18(9):1005–1014. doi:10.1038/s41563-019-0367-7
67. Pearson HB, Mason DE, Kegelman CD, et al. Effects of bone morphogenetic protein-2 on neovascularization during large bone defect regeneration. Tissue Eng Part A. 2019;25(23–24):1623–1634. doi:10.1089/ten.TEA.2018.0326
68. Agarwal R, Garcia AJ. Biomaterial strategies for engineering implants for enhanced osseointegration and bone repair. Adv Drug Deliv Rev. 2015;94:53–62. doi:10.1016/j.addr.2015.03.013
69. Kim S, Kim J, Gajendiran M, et al. Enhanced skull bone regeneration by sustained release of BMP-2 in interpenetrating composite hydrogels. Biomacromolecules. 2018;19(11):4239–4249. doi:10.1021/acs.biomac.8b01013
70. Schoonraad SA, Trombold ML, Bryant SJ. The effects of stably tethered BMP-2 on MC3T3-E1 preosteoblasts encapsulated in a PEG hydrogel. Biomacromolecules. 2021;22(3):1065–1079. doi:10.1021/acs.biomac.0c01085
71. Wu Y, Li X, Sun Y, et al. Multiscale design of stiffening and ROS scavenging hydrogels for the augmentation of mandibular bone regeneration. Bioact Mater. 2023;20:111–125. doi:10.1016/j.bioactmat.2022.05.021
72. Pike DB, Cai S, Pomraning KR, et al. Heparin-regulated release of growth factors in vitro and angiogenic response in vivo to implanted hyaluronan hydrogels containing VEGF and bFGF. Biomaterials. 2006;27(30):5242–5251. doi:10.1016/j.biomaterials.2006.05.018
73. Pellegrini L, Burke DF, von Delft F, Mulloy B, Blundell TL. Crystal structure of fibroblast growth factor receptor ectodomain bound to ligand and heparin. Nature. 2000;407(6807):1029–1034. doi:10.1038/35039551
74. Lund J, Sondergaard MT, Conover CA, Overgaard MT. Heparin-binding mechanism of the IGF2/IGF-binding protein 2 complex. J Mol Endocrinol. 2014;52(3):345–355. doi:10.1530/JME-13-0184
75. Kim S, Cui ZK, Kim PJ, Jung LY, Lee M. Design of hydrogels to stabilize and enhance bone morphogenetic protein activity by heparin mimetics. Acta Biomater. 2018;72:45–54. doi:10.1016/j.actbio.2018.03.034
76. Hettiaratchi MH, Krishnan L, Rouse T, Chou C, McDevitt TC, Guldberg RE. Heparin-mediated delivery of bone morphogenetic protein-2 improves spatial localization of bone regeneration. Sci Adv. 2020;6(1):eaay1240. doi:10.1126/sciadv.aay1240
77. Zhang X, Li J, Chen J, et al. Enhanced bone regeneration via PHA scaffolds coated with polydopamine-captured BMP2. J Mater Chem B. 2022;10(32):6214–6227. doi:10.1039/d2tb01122k
78. Gao YK, Yuan ZY, Yuan XJ, et al. Bioinspired porous microspheres for sustained hypoxic exosomes release and vascularized bone regeneration. Bioact Mater. 2022;14:377–388. doi:10.1016/j.bioactmat.2022.01.041
79. Zhu H, Ji X, Guan H, et al. Tantalum nanoparticles reinforced polyetheretherketone shows enhanced bone formation. Mater Sci Eng C Mater Biol Appl. 2019;101:232–242. doi:10.1016/j.msec.2019.03.091
80. Hu W, Lu S, Ma Y, et al. Poly(dopamine)-inspired surface functionalization of polypropylene tissue mesh for prevention of intra-peritoneal adhesion formation. J Mater Chem B. 2017;5(3):575–585. doi:10.1039/c6tb02667b
81. Wardani AK, Ariono D, Subagjo Wenten IG, et al. Hydrophilic modification of polypropylene ultrafiltration membrane by air-assisted polydopamine coating. Polym Adv Technol. 2019;30(4):1148–1155. doi:10.1002/pat.4549
82. Jia L, Han F, Wang H, et al. Polydopamine-assisted surface modification for orthopaedic implants. J Orthop Translat. 2019;17:82–95. doi:10.1016/j.jot.2019.04.001
83. Gao C, Wang Y, Han F, et al. Antibacterial activity and osseointegration of silver-coated poly(ether ether ketone) prepared using the polydopamine-assisted deposition technique. J Mater Chem B. 2017;5(47):9326–9336. doi:10.1039/c7tb02436c
84. Deng Z, Shang B, Peng B. Polydopamine based colloidal materials: synthesis and applications. Chem Rec. 2018;18(4):410–432. doi:10.1002/tcr.201700051
85. Ford Versypt AN, Pack DW, Braatz RD. Mathematical modeling of drug delivery from autocatalytically degradable PLGA microspheres--A review. J Control Release. 2013;165(1):29–37. doi:10.1016/j.jconrel.2012.10.015
86. Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478). doi:10.1126/science.aau6977
87. Silva AKA, Perretta S, Perrod G, et al. Thermoresponsive gel embedded with adipose stem-cell-derived extracellular vesicles promotes esophageal fistula healing in a thermo-actuated delivery strategy. ACS Nano. 2018;12(10):9800–9814. doi:10.1021/acsnano.8b00117
88. Bei HP, Hung PM, Yeung HL, Wang S, Zhao X. Bone-a-petite: engineering exosomes towards bone, osteochondral, and cartilage repair. Small. 2021;17(50):e2101741. doi:10.1002/smll.202101741
89. Fan J, Lee CS, Kim S, Chen C, Aghaloo T, Lee M. Generation of small RNA-modulated exosome mimetics for bone regeneration. ACS Nano. 2020;14(9):11973–11984. doi:10.1021/acsnano.0c05122
90. Li LM, Zhang Y, Mu JF, et al. Transplantation of human mesenchymal stem-cell-derived exosomes immobilized in an adhesive hydrogel for effective treatment of spinal cord injury. Nano Lett. 2020;20(6):4298–4305. doi:10.1021/acs.nanolett.0c00929
91. Mol EA, Lei ZY, Roefs MT, et al. Injectable supramolecular ureidopyrimidinone hydrogels provide sustained release of extracellular vesicle therapeutics. Adv Healthc Mater. 2019;8(20). doi:10.1002/adhm.201900847
92. Swanson WB, Gong T, Zhang Z, et al. Controlled release of odontogenic exosomes from a biodegradable vehicle mediates dentinogenesis as a novel biomimetic pulp capping therapy. J Control Release. 2020;324:679–694. doi:10.1016/j.jconrel.2020.06.006
93. Hu ZA, Ma C, Rong X, Zou SJ, Liu XH. Immunomodulatory ECM-like microspheres for accelerated bone regeneration in diabetes mellitus. Acs Appl Mater Inter. 2018;10(3):2377–2390. doi:10.1021/acsami.7b18458
94. Lee CS, Kim S, Fan JB, Hwang HS, Aghaloo T, Lee M. Smoothened agonist sterosome immobilized hybrid scaffold for bone regeneration. Sci Adv. 2020;6(17). doi:10.1126/sciadv.aaz7822
95. Su N, Hao YY, Wang F, Hou WD, Chen HF, Luo Y. Mesenchymal stromal exosome-functionalized scaffolds induce innate and adaptive immunomodulatory responses toward tissue repair. Sci Adv. 2021;7(20). doi:10.1126/sciadv.abf7207
96. Fan L, Guan PF, Xiao CR, et al. Exosome-functionalized polyetheretherketone-based implant with immunomodulatory property for enhancing osseointegration. Bioact Mater. 2021;6(9):2754–2766. doi:10.1016/j.bioactmat.2021.02.005
97. Sun YH, Qin HS, Yan ZQ, Zhao CQ, Ren JS, Qu XG. Combating biofilm associated infection in vivo: integration of quorum sensing inhibition and photodynamic treatment based on multidrug delivered hollow carbon nitride sphere (vol 29, 1808222, 2019). Adv Funct Mater. 2020;30(9). doi:10.1002/adfm.201909740
98. Farhood B, Mortezaee K, Goradel NH, et al. Curcumin as an anti-inflammatory agent: implications to radiotherapy and chemotherapy. J Cell Physiol. 2019;234(5):5728–5740. doi:10.1002/jcp.27442
99. Chen T, Zhuang B, Huang Y, et al. Inhaled curcumin mesoporous polydopamine nanoparticles against radiation pneumonitis. Acta Pharm Sin B. 2022;12(5):2522–2532. doi:10.1016/j.apsb.2021.10.027
100. Li B, Webster TJ. Bacteria antibiotic resistance: new challenges and opportunities for implant-associated orthopedic infections. J Orthop Res. 2018;36(1):22–32. doi:10.1002/jor.23656
101. Sun X, Li L, Zhang H, et al. Near-infrared light-regulated drug-food homologous bioactive molecules and photothermal collaborative precise antibacterial therapy nanoplatform with controlled release property. Adv Healthc Mater. 2021;10(16):e2100546. doi:10.1002/adhm.202100546
102. Chiang WL, Lin TT, Sureshbabu R, et al. A rapid drug release system with a NIR light-activated molecular switch for dual-modality photothermal/antibiotic treatments of subcutaneous abscesses. J Control Release. 2015;199:53–62. doi:10.1016/j.jconrel.2014.12.011
103. Li M, Sun X, Zhang N, et al. NIR-activated polydopamine-coated carrier-free ”nanobomb” for in situ on-demand drug release. Adv Sci. 2018;5(7):1800155. doi:10.1002/advs.201800155
104. Fiorica C, Palumbo FS, Pitarresi G, et al. Ciprofloxacin releasing gellan gum/polydopamine based hydrogels with near infrared activated photothermal properties. Int J Pharm. 2021;610:121231. doi:10.1016/j.ijpharm.2021.121231
105. Che L, Wang Y, Sha D, et al. A biomimetic and bioactive scaffold with intelligently pulsatile teriparatide delivery for local and systemic osteoporosis regeneration. Bioact Mater. 2023;19:75–87. doi:10.1016/j.bioactmat.2022.03.023
106. Allen TM, Cullis PR. Liposomal drug delivery systems: from concept to clinical applications. Adv Drug Deliv Rev. 2013;65(1):36–48. doi:10.1016/j.addr.2012.09.037
107. Kong G, Braun RD, Dewhirst MW. Characterization of the effect of hyperthermia on nanoparticle extravasation from tumor vasculature. Cancer Res. 2001;61(7):3027–3032.
108. Wang Y, Shim MS, Levinson NS, Sung HW, Xia Y. Stimuli-responsive materials for controlled release of theranostic agents. Adv Funct Mater. 2014;24(27):4206–4220. doi:10.1002/adfm.201400279
109. Jung WK, Koo HC, Kim KW, Shin S, Kim SH, Park YH. Antibacterial activity and mechanism of action of the silver ion in Staphylococcus aureus and Escherichia coli. Appl Environ Microbiol. 2008;74(7):2171–2178. doi:10.1128/AEM.02001-07
110. Smetana AB, Klabunde KJ, Marchin GR, Sorensen CM. Biocidal activity of nanocrystalline silver powders and particles. Langmuir. 2008;24(14):7457–7464. doi:10.1021/la800091y
111. Samavedi S, Whittington AR, Goldstein AS. Calcium phosphate ceramics in bone tissue engineering: a review of properties and their influence on cell behavior. Acta Biomater. 2013;9(9):8037–8045. doi:10.1016/j.actbio.2013.06.014
112. Zhang Z, Zhang J, Zhang B, Tang J. Mussel-inspired functionalization of graphene for synthesizing Ag-polydopamine-graphene nanosheets as antibacterial materials. Nanoscale. 2013;5(1):118–123. doi:10.1039/c2nr32092d
113. Xie X, Mao C, Liu X, et al. Tuning the bandgap of photo-sensitive polydopamine/Ag3PO4/graphene oxide coating for rapid, noninvasive disinfection of implants. ACS Cent Sci. 2018;4(6):724–738. doi:10.1021/acscentsci.8b00177
114. Yang Y, Zhou X, Chan YK, et al. Photo-activated nanofibrous membrane with self-rechargeable antibacterial function for stubborn infected cutaneous regeneration. Small. 2022;18(12):e2105988. doi:10.1002/smll.202105988
115. Wang L, He S, Wu X, et al. Polyetheretherketone/nano-fluorohydroxyapatite composite with antimicrobial activity and osseointegration properties. Biomaterials. 2014;35(25):6758–6775. doi:10.1016/j.biomaterials.2014.04.085
116. Yan J, Yang L, Lin MF, Ma J, Lu X, Lee PS. Polydopamine spheres as active templates for convenient synthesis of various nanostructures. Small. 2013;9(4):596–603. doi:10.1002/smll.201201064
117. Zhang R, Jiang G, Gao Q, et al. Sprayed copper peroxide nanodots for accelerating wound healing in a multidrug-resistant bacteria infected diabetic ulcer. Nanoscale. 2021;13(37):15937–15951. doi:10.1039/d1nr04687j
118. Lin A, Liu Y, Zhu X, et al. Bacteria-responsive biomimetic selenium nanosystem for multidrug-resistant bacterial infection detection and inhibition. ACS Nano. 2019;13(12):13965–13984. doi:10.1021/acsnano.9b05766
119. Lynge ME, van der Westen R, Postma A, Stadler B. Polydopamine--a nature-inspired polymer coating for biomedical science. Nanoscale. 2011;3(12):4916–4928. doi:10.1039/c1nr10969c
120. Pan H, Shen X, Tao W, Chen S, Ye X. Fabrication of polydopamine-based curcumin nanoparticles for chemical stability and pH-responsive delivery. J Agric Food Chem. 2020;68(9):2795–2802. doi:10.1021/acs.jafc.9b07697
121. Liu Y, Ai K, Lu L. Polydopamine and its derivative materials: synthesis and promising applications in energy, environmental, and biomedical fields. Chem Rev. 2014;114(9):5057–5115. doi:10.1021/cr400407a
122. Ran P, Zheng H, Cao WX, et al. On-demand changeable theranostic hydrogels and visual imaging-guided antibacterial photodynamic therapy to promote wound healing. Acs Appl Mater Inter. 2022;14(43):49375–49388. doi:10.1021/acsami.2c15561
123. Peng D, Liu G, He Y, et al. Fabrication of a pH-responsive core-shell nanosystem with a low-temperature photothermal therapy effect for treating bacterial biofilm infection. Biomater Sci. 2021;9(22):7483–7491. doi:10.1039/d1bm01329g
124. Wang X, Wang CP, Wang XY, Wang YT, Zhang Q, Cheng YY. A polydopamine nanoparticle-knotted Poly(ethylene glycol) hydrogel for on-demand drug delivery and chemo-photothermal therapy. Chem Mater. 2017;29(3):1370–1376. doi:10.1021/acs.chemmater.6b05192
125. Yin J, Zhong J, Wang J, et al. 3D-printed high-density polyethylene scaffolds with bioactive and antibacterial layer-by-layer modification for auricle reconstruction. Mater Today Bio. 2022;16:100361. doi:10.1016/j.mtbio.2022.100361
126. Wu M, Chen F, Liu H, et al. Bioinspired sandwich-like hybrid surface functionalized scaffold capable of regulating osteogenesis, angiogenesis, and osteoclastogenesis for robust bone regeneration. Mater Today Bio. 2022;17:100458. doi:10.1016/j.mtbio.2022.100458
127. Yuan R, Yang N, Fan S, et al. Biomechanical motion-activated endogenous wound healing through LBL self-powered nanocomposite repairer with pH-responsive anti-inflammatory effect. Small. 2021;17(50):e2103997. doi:10.1002/smll.202103997
128. Xiong F, Wei S, Sheng H, et al. Three-layer core-shell structure of polypyrrole/polydopamine/poly(l-lactide) nanofibers for wound healing application. Int J Biol Macromol. 2022;222(Pt B):1948–1962. doi:10.1016/j.ijbiomac.2022.09.284
129. Zheng Z, Li M, Shi P, et al. Polydopamine-modified collagen sponge scaffold as a novel dermal regeneration template with sustained release of platelet-rich plasma to accelerate skin repair: a one-step strategy. Bioact Mater. 2021;6(8):2613–2628. doi:10.1016/j.bioactmat.2021.01.037
130. Zhu Z, Gao Q, Long Z, et al. Corrigendum to ”polydopamine/poly(sulfobetaine methacrylate) co-deposition coatings triggered by CuSO4/H2O2 on implants for improved surface hemocompatibility and antibacterial activity” [Bioactive materials 6 (2021) 2546–2556]. Bioact Mater. 2022;17:195–196. doi:10.1016/j.bioactmat.2022.01.037
131. Xu X, Li Y, Wang L, et al. Triple-functional polyetheretherketone surface with enhanced bacteriostasis and anti-inflammatory and osseointegrative properties for implant application. Biomaterials. 2019;212:98–114. doi:10.1016/j.biomaterials.2019.05.014
132. Decher G. Fuzzy nanoassemblies: toward layered polymeric multicomposites. Science. 1997;277(5330):1232–1237. doi:10.1126/science.277.5330.1232
133. de Villiers MM, Otto DP, Strydom SJ, Lvov YM. Introduction to nanocoatings produced by layer-by-layer (LbL) self-assembly. Adv Drug Deliv Rev. 2011;63(9):701–715. doi:10.1016/j.addr.2011.05.011
134. Yang Z, Xi Y, Bai J, et al. Covalent grafting of hyperbranched poly-L-lysine on Ti-based implants achieves dual functions of antibacteria and promoted osteointegration in vivo. Biomaterials. 2021;269:120534. doi:10.1016/j.biomaterials.2020.120534
135. Wasilewska M, Adamczyk Z, Ocwieja M, Wojnar D, Zeliszewska P. Silver nanoparticle/fibrinogen bilayers - mechanism of formation and stability determined by in situ electrokinetic measurements. J Colloid Interface Sci. 2018;513:170–179. doi:10.1016/j.jcis.2017.11.019
136. Tian L, Zhang Z, Tian B, Zhang X, Wang N. Study on antibacterial properties and cytocompatibility of EPL coated 3D printed PCL/HA composite scaffolds. RSC Adv. 2020;10(8):4805–4816. doi:10.1039/c9ra10275b
137. Pajorova J, Bacakova M, Musilkova J, et al. Morphology of a fibrin nanocoating influences dermal fibroblast behavior. Int J Nanomed. 2018;13:3367–3380. doi:10.2147/IJN.S162644
138. Zhang Y, Wang F, Huang Q, et al. Layer-by-layer immobilizing of polydopamine-assisted epsilon-polylysine and gum Arabic on titanium: tailoring of antibacterial and osteogenic properties. Mater Sci Eng C Mater Biol Appl. 2020;110:110690. doi:10.1016/j.msec.2020.110690
139. Zhao Y, Bai L, Zhang Y, et al. Type I collagen decorated nanoporous network on titanium implant surface promotes osseointegration through mediating immunomodulation, angiogenesis, and osteogenesis. Biomaterials. 2022;288:121684. doi:10.1016/j.biomaterials.2022.121684
140. Zhao X, Zhou L, Li Q, Zou Q, Du C. Biomimetic mineralization of carboxymethyl chitosan nanofibers with improved osteogenic activity in vitro and in vivo. Carbohydr Polym. 2018;195:225–234. doi:10.1016/j.carbpol.2018.04.090
141. Feng L, Shi W, Chen Q, et al. Smart asymmetric hydrogel with integrated multi-functions of NIR-triggered tunable adhesion, self-deformation, and bacterial eradication. Adv Healthc Mater. 2021;10(19):e2100784. doi:10.1002/adhm.202100784
142. Yang F, Murugan R, Ramakrishna S, Wang X, Ma YX, Wang S. Fabrication of nano-structured porous PLLA scaffold intended for nerve tissue engineering. Biomaterials. 2004;25(10):1891–1900. doi:10.1016/j.biomaterials.2003.08.062
143. Shim IK, Jung MR, Kim KH, et al. Novel three-dimensional scaffolds of poly(L-lactic acid) microfibers using electrospinning and mechanical expansion: fabrication and bone regeneration. J Biomed Mater Res B Appl Biomater. 2010;95(1):150–160. doi:10.1002/jbm.b.31695
144. Wu S, Peng H, Li X, Streubel PN, Liu Y, Duan B. Effect of scaffold morphology and cell co-culture on tenogenic differentiation of HADMSC on centrifugal melt electrospun poly (L‑lactic acid) fibrous meshes. Biofabrication. 2017;9(4):044106. doi:10.1088/1758-5090/aa8fb8
145. Zhou Q, Xie J, Bao M, et al. Engineering aligned electrospun PLLA microfibers with nano-porous surface nanotopography for modulating the responses of vascular smooth muscle cells. J Mater Chem B. 2015;3(21):4439–4450. doi:10.1039/c5tb00051c
146. Mao X, Cheng R, Zhang H, et al. Self-healing and injectable hydrogel for matching skin flap regeneration. Adv Sci. 2019;6(3):1801555. doi:10.1002/advs.201801555
147. Li L, Yan B, Yang J, Huang W, Chen L, Zeng H. Injectable self-healing hydrogel with antimicrobial and antifouling properties. Acs Appl Mater Inter. 2017;9(11):9221–9225. doi:10.1021/acsami.6b16192
148. Rao KM, Narayanan KB, Uthappa UT, Park PH, Choi I, Han SS. Tissue adhesive, self-healing, biocompatible, hemostasis, and antibacterial properties of fungal-derived carboxymethyl chitosan-polydopamine hydrogels. Pharmaceutics. 2022;14(5):1028. doi:10.3390/pharmaceutics14051028
149. Yi J, Nguyen KT, Wang W, et al. Mussel-inspired adhesive double-network hydrogel for intraoral ultrasound imaging. ACS Appl Bio Mater. 2020;3(12):8943–8952. doi:10.1021/acsabm.0c01211
150. Zhang G, Chen S, Peng Z, et al. Topologically enhanced dual-network hydrogels with rapid recovery for low-hysteresis, self-adhesive epidemic electronics. ACS Appl Mater Interfaces. 2021;13(10):12531–12540. doi:10.1021/acsami.1c00819
151. Chen T, Chen Y, Rehman HU, et al. Ultratough, self-healing, and tissue-adhesive hydrogel for wound dressing. ACS Appl Mater Interfaces. 2018;10(39):33523–33531. doi:10.1021/acsami.8b10064
152. Mourya VK, Inamdara N, Ashutosh Tiwari N. Carboxymethyl chitosan and its applications. Adv Mater Lett. 2010;1(1):11–33. doi:10.5185/amlett.2010.3108
153. Dai S, Yue S, Ning Z, Jiang N, Gan Z. Polydopamine nanoparticle-reinforced near-infrared light-triggered shape memory polycaprolactone-polydopamine polyurethane for biomedical implant applications. ACS Appl Mater Interfaces. 2022;14(12):14668–14676. doi:10.1021/acsami.2c03172
154. Gong T, Zhao K, Liu X, Lu L, Liu D, Zhou S. A dynamically tunable, bioinspired micropatterned surface regulates vascular endothelial and smooth muscle cells growth at vascularization. Small. 2016;12(41):5769–5778. doi:10.1002/smll.201601503
155. Gogoi S, Karak N. Biobased biodegradable waterborne hyperbranched polyurethane as an ecofriendly sustainable material. ACS Sustain Chem Eng. 2014;2(12):2730–2738. doi:10.1021/sc5006022
156. Daraghmeh DN, King C, Wiese MD. A review of liquid biopsy as a tool to assess epigenetic, cfDNA and miRNA variability as methotrexate response predictors in patients with rheumatoid arthritis. Pharmacol Res. 2021;173:105887. doi:10.1016/j.phrs.2021.105887
157. Mondelo-Macía P, Castro-Santos P, Castillo-García A, Muinelo-Romay L, Diaz-Peña R. Circulating free DNA and its emerging role in autoimmune diseases. J Pers Med. 2021;11(2):151. doi:10.3390/jpm11020151
158. Liang H, Peng B, Dong C, et al. Cationic nanoparticle as an inhibitor of cell-free DNA-induced inflammation. Nat Commun. 2018;9(1):4291. doi:10.1038/s41467-018-06603-5
159. Wang Y, Ma X, Ding C, Jia L. pH-responsive deoxyribonucleic acid capture/release by polydopamine functionalized magnetic nanoparticles. Anal Chim Acta. 2015;862:33–40. doi:10.1016/j.aca.2015.01.009
160. Chen Y, Wang Y, Jiang X, et al. Dimethylamino group modified polydopamine nanoparticles with positive charges to scavenge cell-free DNA for rheumatoid arthritis therapy. Bioact Mater. 2022;18:409–420. doi:10.1016/j.bioactmat.2022.03.028
161. Zheng B, Deng G, Zheng J, et al. Self-polymerized polydopamine-based nanoparticles for acute kidney injury treatment through inhibiting oxidative damages and inflammatory. Int J Biochem Cell Biol. 2022;143:106141. doi:10.1016/j.biocel.2021.106141
162. Saita M, Kaneko J, Sato T, et al. Novel antioxidative nanotherapeutics in a rat periodontitis model: reactive oxygen species scavenging by redox injectable gel suppresses alveolar bone resorption. Biomaterials. 2016;76:292–301. doi:10.1016/j.biomaterials.2015.10.077
163. Wei Y, Fu J, Wu W, et al. Quercetin prevents oxidative stress-induced injury of periodontal ligament cells and alveolar bone loss in periodontitis. Drug Des Devel Ther. 2021;15:3509–3522. doi:10.2147/DDDT.S315249
164. Bao X, Zhao J, Sun J, Hu M, Yang X. Polydopamine nanoparticles as efficient scavengers for reactive oxygen species in periodontal disease. ACS Nano. 2018;12(9):8882–8892. doi:10.1021/acsnano.8b04022
165. Fu Y, Zhang J, Wang Y, et al. Reduced polydopamine nanoparticles incorporated oxidized dextran/chitosan hybrid hydrogels with enhanced antioxidative and antibacterial properties for accelerated wound healing. Carbohydr Polym. 2021;257:117598. doi:10.1016/j.carbpol.2020.117598
166. Li Y, Yang L, Hou Y, et al. Polydopamine-mediated graphene oxide and nanohydroxyapatite-incorporated conductive scaffold with an immunomodulatory ability accelerates periodontal bone regeneration in diabetes. Bioact Mater. 2022;18:213–227. doi:10.1016/j.bioactmat.2022.03.021
167. Sohrabi Y, Lagache SMM, Schnack L, et al mTOR-dependent oxidative stress regulates oxLDL-induced trained innate immunity in human monocytes. Front Immunol. 2018;9:3155. doi:10.3389/fimmu.2018.03155
168. Shi H, Jin L, Li J, et al. Mesoporous polydopamine nanoparticles for sustained release of rapamycin and reactive oxygen species scavenging to synergistically accelerate neurogenesis after spinal cord injury. J Mater Chem B. 2022;10(33):6351–6359. doi:10.1039/d2tb00841f
169. Wei X, Zhou W, Tang Z, et al. Magnesium surface-activated 3D printed porous PEEK scaffolds for in vivo osseointegration by promoting angiogenesis and osteogenesis. Bioact Mater. 2023;20:16–28. doi:10.1016/j.bioactmat.2022.05.011
170. Wu HY, Lin YH, Lee AK, Kuo TY, Tsai CH, Shie MY. Combined effects of polydopamine-assisted copper immobilization on 3d-printed porous Ti6Al4V scaffold for angiogenic and osteogenic bone regeneration. Cells. 2022;11(18):1.
171. Liu G, Xiong Q, Xu Y, et al. Magnetically separable MXene@Fe3O4/Au/PDA nanosheets with photothermal-magnetolytic coupling antibacterial performance. Appl Surf Sci. 2022;590:153125. doi:10.1016/j.apsusc.2022.153125
172. Fang Q, Wang J, Wu S, Leung KC, Xu Y, Xuan S. NIR-induced improvement of catalytic activity and antibacterial performance over AuAg nanorods in Rambutan-like Fe(3)O(4)@AgAu@PDA magnetic nanospheres. J Hazard Mater. 2023;445:130616. doi:10.1016/j.jhazmat.2022.130616
173. Fang Q, Wang J, Xiong Q, et al. Anisotropic α-Fe2O3/AgAu/Polydopamine nanostructures for photothermally enhanced antibacterial applications. ACS Appl Nano Mater. 2023;6(7):6423–6434. doi:10.1021/acsanm.3c01068
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
