Back to Journals » OncoTargets and Therapy » Volume 11
Real-world usage and clinical outcomes of alectinib among post-crizotinib progression anaplastic lymphoma kinase positive non-small-cell lung cancer patients in the USA
Authors DiBonaventura MD, Wong W, Shah-Manek B, Schulz M
Received 27 June 2017
Accepted for publication 10 November 2017
Published 22 December 2017 Volume 2018:11 Pages 75—82
DOI https://doi.org/10.2147/OTT.S144960
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Geoffrey Pietersz
Marco D DiBonaventura,1 William Wong,2 Bijal Shah-Manek,3,4 Mathias Schulz2
1Ipsos Healthcare, Global Evidence, Value & Access, New York, NY, 2Genentech, US Medical Affairs, San Francisco, CA, 3Ipsos Healthcare, Global Evidence, Value & Access, San Francisco, CA, 4College of Pharmacy, Touro University California, CA, USA
Background: Alectinib is an approved treatment for anaplastic lymphoma kinase (ALK)-positive patients with advanced non-small-cell lung cancer. Despite positive supporting clinical data, there is a lack of real-world information on the usage and patient outcomes of those treated with alectinib post-crizotinib progression.
Methods: Participating oncologists (N=95) in the USA were recruited from an online physician panel to participate in a retrospective patient chart review. Physicians randomly selected eligible patients (ie, patients who progressed on crizotinib as their first ALK inhibitor and were treated with alectinib as their second ALK inhibitor), collected demographics and clinical history from their medical charts, and entered the data into an online data collection form.
Results: A total of N=207 patient charts were included (age: 60.1±10.4 years; 53.6% male). The patients in our sample were older (median age of 60 vs 53 years), were more likely to be current smokers (12% vs 1%), had better performance status (45% vs 33% had an Eastern Cooperative Oncology Group [ECOG] of 0), and were less likely to have an adenocarcinoma histology (83% vs 96%) relative to published clinical trials. The objective response rate was higher than in clinical trials (67.1% vs 51.3%, respectively) as was the disease control rate (89.9% vs 78.8%, respectively), though it varied by race/ethnicity, ECOG, and prior treatment history. Discontinuation (0.0%) and dose reductions (3.4%) due to adverse events were uncommon in alectinib.
Conclusion: Patients using alectinib post-crizotinib in clinical practice are older, more racially/ethnically and histologically diverse than patients in published trials. Real-world response rates were high and similar to those reported in clinical studies, though there is some variation by patient characteristics. Alectinib was well tolerated in clinical practice as reflected by the rates of discontinuation, dose reductions, and dose interruptions.
Keywords: alectinib, anaplastic lymphoma kinase, non-small-cell lung cancer, treatment patterns, outcomes, ALK inhibitor, ALK+
Introduction
An estimated 220,000 adults were diagnosed with lung and bronchus cancer in the USA in 2015, representing 13% of all new cancer cases.1 Non-small-cell lung cancer (NSCLC) accounts for ~80%–85% of all cases of lung cancer, and is the most common cause of death in men and second only to breast cancer in women.2 Prognosis is poor for patients with metastatic disease, with the median survival <1 year because of delays in diagnosis.3,4
Treatment of NSCLC is guided by disease stage, histology, and mutation status. Surgery is the most common treatment for early-stage localized disease, whereas multimodal therapy remains the norm for patients with locally advanced disease.5 Approximately 40% of patients with NSCLC present with metastatic or locally advanced disease, underscoring the importance of identifying therapeutic regimens that may benefit this large patient population. Combination chemotherapy, usually platinum-based, has historically been the first-line therapy of choice for advanced NSCLC among patients without driver mutations.6–8 Newer agents, such as programmed cell death-1 and programmed cell death ligand-1 inhibitors, have been more recently evaluated in clinical trials for the treatment of NSCLC and several other types of cancer.9–11
Over the last decade, a variety of targeted therapies have been developed for the treatment of advanced or metastatic NSCLC in patients with driver mutations. Indeed, anaplastic lymphoma kinase (ALK) inhibitors represent a promising potential target for antitumor therapy,12–14 with ~2%–7% of patients with NSCLC being ALK positive.7,15 Crizotinib was identified as the first potent inhibitor of ALK in experimental cancer models;16 clinical data have suggested superior response and longer progression-free survival for patients treated with crizotinib relative to chemotherapy.17–20
Despite these efficacy results, almost all patients ultimately develop resistance to crizotinib within 1–2 years, with the central nervous system (CNS) being a frequent site of progression.21–24 The recently available second-generation ALK inhibitors (eg, ceritinib, alectinib, brigatinib) and third-generation ALK inhibitors (eg, lorlatinib) have been found to provide significant benefits for patients who experience crizotinib progression.25,26 Of the second-generation ALK inhibitors, alectinib is the only one that is not exported out of the CNS because of it not being a p-glycoprotein substrate,25–27 and several clinical studies28–31 have shown alectinib to be highly active, especially in patients with brain metastases and CNS disease. Further, alectinib is well tolerated among crizotinib-resistant patients.28–31 However, little real-world data exist on the usage and outcomes of patients treated with alectinib after crizotinib progression. The aim of the present study is to examine the real-world treatment patterns and clinical outcomes of patients with ALK+ NSCLC who have progressed on crizotinib and were treated with alectinib as their second ALK inhibitor.
Methods
Data source
A retrospective patient chart review study was conducted to meet the objectives described above. Participating oncologists were recruited from the Medefield physician panel (http://www.medefield.com/). The Medefield panel is an opt-in panel in which physicians join with the understanding that they will complete periodic surveys. All panel physicians in the USA have their credentials validated with American Medical Association.
Potential physician respondents were emailed an invitation to participate in the study. Physicians who provided informed consent were screened for eligibility. Physicians’ inclusion criteria include board-certified or board-eligible oncologist, in practice for at least 5 years but no more than 25 years, personally involved in the treatment decisions of patients with NSCLC, and have seen at least 1 NSCLC ALK+ patient in the past year. Physicians who met inclusion criteria were then asked to select between 1 and 5 of their patient charts that met the following eligibility criteria: ≥18 years, diagnosed with ALK+ NSCLC (tumors harboring a rearranged ALK gene/fusion protein), and experienced disease progression while on crizotinib (as their first ALK inhibitor). ALK+ status was determined by the responding physician based on results available in the patient chart. It was desired to have a minimum of 12-month follow-up from time of initial disease progression on crizotinib or until death (if <12 months of follow-up exist). Patients who participated in an NSCLC-related clinical trial prior to crizotinib and alectinib were excluded.
Using the data available from each medical chart, the physician collected the demographics, health history, health care resource use, and treatment information for each patient. Data were pulled from notes from physical examinations, laboratory data, imaging data, prescription data, and nurse records, as appropriate.
Ethics
The study protocol and data collection form were reviewed by an independent institutional review board (Pearl IRB, Indianapolis, IN; Protocol #: 16-033202) and the study was granted exemption status. The IRB reviewed the documents submitted for exemption determination in accordance to the US Food and Drug Administration 21 CFR 56.104 and the Department of Health and Human Services 45 CFR 46.101 regulations.. The exemption was approved under the exempt review category 45 CFR 46.101(b) category 4.
Patient written informed consent to review the medical records was not required by the IRB as no personally identifiable patient information was collected. Only anonymous patient data were collected and results were only reported in aggregate. Physicians provided consent for participating in the study and written informed consent was required from each responding physician, before participating in the study.
Study sample
Data from a total of N=207 patient charts who used alectinib as their second ALK inhibitor were collected from N=95 physicians.
Study measures
Physician demographics: Physicians provided information as to their age, sex, and practice characteristics (years in practice, setting, and patient load).
Patient demographics: Physicians provided information related to the age, sex, and employment status of each patient.
General health history: Height and weight (to convert to body mass index [BMI] category), smoking history, and comorbidities (to calculate a Charlson comorbidity index) were assessed.
NSCLC history: The date of diagnosis, stage at diagnosis, histology, current performance status (Eastern Cooperative Oncology Group [ECOG]), and the number/location/date of metastases were captured.
Treatment history: Treatments used prior to and after crizotinib, including their duration, were captured. Reasons for discontinuation of each therapy were captured along with the presence and reasons for dose modifications. The presence of adverse events was captured along with treatments related to brain/CNS metastases.
Clinical outcomes: Best response (complete response [CR], partial response [PR], stable disease [SD], or progression) was captured for each treatment based on the interpretation of the treating physician using the data contained within the medical chart. The study did not mandate that any specific criteria, such as RECIST v1.1, were to be used in this assessment. For the purposes of this study, objective response rate (ORR) was defined as the proportion of patients achieving a best response of CR or PR. Disease control rate (DCR) was defined as the proportion of patients achieving a best response of CR, PR, or SD.
Health care resource use: The number of hospitalizations, emergency room visits, and office visits was captured. Health care resource use specific to adverse events was also assessed.
Statistical analysis
Physician and patient characteristics, response rates, and safety/tolerability were reported descriptively using frequencies and percentages for categorical variables and means and standard deviations for continuous variables. Differences in response rates across patient characteristic strata were compared using chi-square tests.
Results
Physician characteristics
A total of N=95 physicians contributed patient charts; N=47 (49.5%) specialized in hematology/oncology and N=48 (50.5%) specialized in medical oncology (Table 1). Physicians were predominantly male (81.1%), with a mean of 14.6 years (SD =6.4) in practice. The most common practice setting was private practice (46.3%) followed by an academic hospital/medical center (35.8%).
  | Table 1 Characteristics of the physician sample treating patients with alectinib post-crizotinib progression (N=95) |
Real-world vs clinical trial patient characteristics
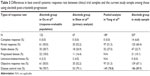
Descriptive comparisons were then made between our study and available clinical trial results (Table 2).28,29 Key differences observed between our study and clinical trial populations included age (median age of 60 vs 53 for our study and the pooled clinical trial samples, respectively), gender (54% vs 44% male, respectively), and performance status (45% vs 33% had an ECOG of 0). Both our study and clinical trial samples had similar percentages of Asian patients (18% vs 19%). Patients in our study were more likely to be a current smoker (12% vs 1%), less likely to have an adenocarcinoma histology (83% vs 96%), and were less likely to have presented with brain metastases (12% vs 60%) relative to clinical trial samples.
Comparisons were also made between alectinib best overall responses rates in our study and clinical trial data (Table 3). Among the full sample (N=207 alectinib patients), the ORR was higher than in clinical trials (67.1% vs 51.3%, respectively) as was the DCR (89.9% vs 78.8%, respectively).
Best overall response rates in the overall alectinib subsample were then compared across various patient characteristic strata (Table 4). As reported above, best overall response rates were consistent, and in some cases higher than those reported in prior clinical trials.28,29 Although response did not differ by physician characteristics or patient age, ORR was highest among Asian respondents (89.2%) vs 47.4% among non-Asian/non-White respondents (P<.05). These findings are consistent with those reported in clinical trials.28,29 Former/passive/never smokers exhibited higher response rates relative to current smokers (ORR =68.3% vs 58.3%) but this difference was not significant (P=0.07). No differences were observed by level of BMI (P=0.81). Better functional status, as assessed by ECOG performance score, was associated with better response (ORR =71.6% for ECOG 0–1 vs 30.0% for ECOG 2+; P<0.05). Finally, ORR was similar between those with and without prior chemotherapy (65.9% vs 67.5%, respectively); however, rates of SD were higher (25.8% vs 11.4%) and rates of PD were lower (6.7% vs 22.7%) for those without prior chemotherapy (P<0.05).
Dose modifications
The median dose for the patients in this study was 600 mg twice daily. Discontinuations were the most common category of dosage modification. Among those who used alectinib, 14.0% of patients (N=29) discontinued the drug, whereas only 4.3% (N=9) had their dose reduced; and only one patient experienced a dose interruption (N=1; 0.5% [Table 5]). Of the dose discontinuations, N=12 (41.4%) were due to disease progression, 9 (31.0%) were due to death, N=5 (17.2%) were due to patient request, and N=3 (10.3%) were due to other reasons (none were due to adverse events).
  | Table 5 Frequency and reasons for dosage modification among patients using alectinib post-crizotinib progression (N=207) |
Safety and tolerability
There were no dose discontinuations or dose reductions due to adverse events among the patients in this study. Of the dose reductions, N=7 (3.38%) were due to adverse events; specific adverse events included fatigue (N=4), hepatotoxicity (N=2), bradycardia (N=1), and edema (N=1).
Discussion
The objectives of this study were to examine the real-world usage and clinical outcomes among patients with ALK+ NSCLC who were treated with alectinib after progressing on crizotinib as their first ALK inhibitor. The sample characteristics of our study patients vs those of clinical trials patients emphasize the differences between these two environments. The alectinib sample in our study was ~10 years older, had fewer Asian respondents, more African-American and Hispanic respondents, had a more diverse histology (clinical trials were almost exclusively adenocarcinoma), had more current smokers, and had poorer functional status based on ECOG measures than clinical trial samples.28,29 Additionally, many alectinib patients were managed by a hematologist/oncologist and in the private practice setting. Although not alectinib specific, recent real-world data studies of ALK+ NSCLC patients suggested similar demographic (age, sex) and health history (smoking status) findings as reported here.32,33 These results suggest that the patients prescribed alectinib immediately after crizotinib progression are more demographically diverse than those enrolled in clinical trials, which could have implications for clinical outcomes and experiences with safety/tolerability events.
Rates of brain metastases in our study vis-à-vis published literature deserve specific comment. Some real-world studies have reported brain metastatic rates over 50%,34 which is similar to that reported in clinical studies.28–30 However, other real-world studies have estimated rates closer to 20%–30%.33,35–37 These numbers are still higher than those reported in our sample in which 12% of patients had brain metastases at the end of crizotinib/initiation of alectinib. Although it is unknown what could cause the discrepancy, there are several possibilities. First, the follow-up time (as well as the timeframe that constituted “baseline”) was slightly shorter in the present study (eg, relative to Betts et al33); thus, there was less time for a brain metastasis to manifest. Secondly, our patient population was generally older than the available clinical data, and research has suggested that the incidence of brain metastases in older patients is lower than that in younger patients.38 Recent studies have suggested that only 47% of brain metastases are symptomatic39 representing a possible source of underdiagnosis of brain metastases that is disproportionately more common in smaller practices than larger academic centers. Most of the patients in this study were treated in smaller private practices, which could have contributed to the lower rates of brain metastasis. Undoubtedly, more research is necessary, though substantial clinical data suggest the importance of brain metastases in the ALK+ NSCLC patient population.24,40
The observed response rates were generally similar in our study to clinical trial results and, to a certain degree, even more favorable.28–30 However, in some cases these response rates differed significantly by the characteristics of the patients. Asian patients (vs non-Asian/non-White patients), former/passive/never smokers (vs current smokers), and patients with better functional status (vs patients with poorer functional status), all reported better response rates. Nevertheless, it should be noted that for all strata, response rates were objectively high and, due to small sample sizes, caution should be exercised when interpreting the comparisons across groups. Further, the RECIST criteria were not used to define response in this real-world study; rather, the oncologist determined response based on information in the patient’s chart.
Finally, the results suggest that alectinib was well tolerated in real-world clinical practice. Discontinuation was relatively uncommon over the study period (14%) and when it occurred it was mostly due to disease progression; no discontinuation due to adverse events was observed. Dosage reductions and dosage interruptions were even less common. Fatigue was the most common safety/tolerability event that led to dose modifications. However, it should be noted that the observation time for our study (due to the recent availability of alectinib) was less than that in clinical trials (14–20 months for randomized controlled trials vs 10 months for our study; Table 2).
Limitations
Most of the research questions were descriptive in nature, without clear threats to internal validity. However, the method and the nature of the sample source may be a threat to the external validity. Only members of an Internet panel were eligible to join; these physicians (and, by extension, perhaps their patients) may differ from broader oncologist population. The selected panel did have a large representation with the intent to minimize this bias. Another threat to validity was the chart selection method. Although physicians were asked to select their most recent patients, physicians could have selected charts preferentially, which may have biased the sample of patients. Finally, the RECIST criteria were not used to determine response to treatment in this real-world study.
Conclusions
This retrospective chart review study is the first to document the real-world usage and clinical outcomes of patients with ALK+ NSCLC who are treated with alectinib after experiencing progression on crizotinib as their first ALK inhibitor. Substantial differences were observed between the real-world sample and the samples of alectinib clinical trials; our study suggested (consistent with other real-world data studies on ALK+ NSCLC patients more broadly31,32) that patients using alectinib in clinical practice are older, more racially/ethnically and histologically diverse than those samples in published trials. Nevertheless, response rates are generally high and similar to those reported in clinical studies, though there is some variation by patient characteristics. In addition, alectinib was well tolerated in clinical practice with no discontinuations or dose interruptions and very few dose reductions due to adverse events.
Acknowledgment
Funding was provided by Genentech.
Disclosure
Marco D DiBonaventura was employed by Ipsos Healthcare at the time of the study and Bijal Shah-Manek is employed by Ipsos Healthcare, a health care consulting company. William Wong and Mathias Schulz are employed by Genentech (a subsidiary of Roche Holding AG). Mathias Schulz and William Wong hold shares from Roche Holding AG. The authors report no other conflicts of interest in this work.
References
National Cancer Institute. SEER stat fact sheets: Lung and bronchus cancer. Available from: http://seer.cancer.gov/statfacts/html/lungb.html. Accessed November 18, 2015. | ||
Ramalingam S. Belani C. Systemic chemotherapy for advanced non-small cell lung cancer: recent advances and future directions. Oncologist. 2008;13(Suppl 1):5–13. | ||
O’Bryant CL, Wenger SD, Kim M, Thompson LA. Crizotinib: a new treatment option of ALK-positive non-small cell lung cancer. Ann Pharmacother. 2013;47(2):189–197. | ||
Radzikowska E, Roszkowski-Sliz K, Chabowski M, Glaz P. Influence of delays in diagnosis and treatment on survival in small cell lung cancer patients. Adv Exp Med Biol. 2013;788:355–362. | ||
Dempke WC. Targeted therapy for NSCLC-A double-edged Sword? Anticancer Res. 2015;35(5):2503–2512. | ||
Shepherd F. Second-line chemotherapy for non-small cell lung cancer. Expert Rev Anticancer Ther. 2003;3(1):435–442. | ||
Scagliotti GV, Parikh P, von Pawel J, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naïve patients with advanced-stage non-small cell lung cancer. J Clin Oncol. 2008;26(21):3543–3451. | ||
Dempke WC, Suto T, Reck M. Targeted therapies for non-small cell lung cancer. Lung Cancer. 2010;67(3):257–274. | ||
Ma W, Gilligan BM, Yuan J, Li T. Current status and perspectives in translational biomarker research for PD-1/PD-L1 immune checkpoint blockade therapy. J Hematol Oncol. 2016;9(1):47. | ||
Dholaria B, Hammond W, Shreders A, Lou Y. Emerging therapeutic agents for lung cancer. J Hematol Oncol. 2016;9(1):138. | ||
Diggs LP, Hsueh EC. Utility of PD-L1 immunohistochemistry assays for predicting PD-1/PD-L1 inhibitor response. Biomark Res. 2017;5(1):12. | ||
Minguet J, Smith KH, Bramlage P. Targeted therapies for treatment of non-small cell lung cancer – recent advances and future perspectives. Int J Cancer. 2016;138(11):2549–2561. | ||
Solomon B, Varella-Garcia M, Camidge DR. ALK gene rearrangements: a new therapeutic target in a molecularly defined subset of non-small cell lung cancer. J Thorac Oncol. 2009;4(12):1450–1454. | ||
Gainor JF, Varghese AM, Ou SH, et al. ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: an analysis of 1,683 patients with non-small cell lung cancer. Clin Cancer Res. 2013;19(15):4273–4281. | ||
Casaluce F, Sgambato A, Maione P, et al. ALK inhibitors: a new targeted therapy in the treatment of advanced NSCLC. Targ Oncol. 2013;8(1):55–67. | ||
Christensen JG, Zou HY, Arango ME, et al. Cytoreductive antitumor activity of PF-2341066, a novel inhibitor of anaplastic lymphoma kinase and c-Met, in experimental models of anaplastic large-cell lymphoma. Mol Cancer Ther. 2007;6(12 Pt 1):3314–3322. | ||
Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363(18):1693–1703. | ||
Camidge DR, Bang YJ, Kwak EL, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol. 2012;13(10):1011–1019. | ||
Shaw AT, Kim DW, Nakagawa K, et al. Crizotinib vs chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368:2385–2394. | ||
Solomon BJ, Mok T, Kim DW, et al; PROFILE 1014 Investigators. First-line crizotinib vs chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371(213):2167–2177. | ||
Toyokawa G, Seto T. ALK inhibitors: what is the best way to treat patients with ALK+ non-small-cell lung cancer? Clin Lung Cancer. 2014;15(5):313–319. | ||
Katayama R, Shaw AT, Khan TM, et al. Mechanisms of acquired crizotinib resistance in ALK-rearranged lung cancers. Sci Transl Med. 2012;4(120):120ra17. | ||
Doebele RC, Pilling AB, Aisner DL, et al. Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer. Clin Cancer Res. 2012;18(5):1472–1482. | ||
Weickhardt AJ, Scheier B, Burke JM, et al. Local ablative therapy of oligoprogressive disease prolongs disease control by tyrosine kinase inhibitors in oncogene addicted non-small cell lung cancer. J Thorac Oncol. 2012;7(12):1807–1814. | ||
Wu J, Savooji J, Liu D. Second- and third-generation ALK inhibitors for non-small cell lung cancer. J Hematol Oncol. 2016;9:19. | ||
Iragavarapu C, Mustafa M, Akinleye A, et al. Novel ALK inhibitors in clinical use and development. J Hematol Oncol. 2015;8:17. | ||
Kodama T, Hasegawa M, Takanashi K, Sakurai Y, Kondoh O, Sakamoto H. Antitumor activity of the selective ALK inhibitor alectinib in models of intracranial metastases. Cancer Chemother Pharmacol. 2014;74(5):1023–1028. | ||
Ou SH, Ahn JS, De Petris L, et al. Alectinib in crizotinib-refractory ALK-rearranged non-small-cell lung cancer: a Phase II Global Study. J Clin Oncol. 2016;34(7):661–668. | ||
Shaw AT, Gandhi L, Gadgeel S, et al; study investigators. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multicentre, phase 2 trial. Lancet Oncol. 2016;17(2):234–242. | ||
Yang JC, Ou SI, De Petris L, et al. Pooled systemic efficacy and safety data from two phase II studies (NP28673 and NP28761) of alectinib in ALK-positive non-small-cell lung cancer (NSCLC). J Thorac Oncol. 2017;12(10):1552–1560. | ||
Gadgeel SM, Gandhi L, Riely GJ, et al. Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): results from the dose-finding portion of a phase 1/2 study. Lancet Oncol. 2014;15(10):1119–1128. | ||
Bendaly E, Sasane M, Zhang J, Swallow E, Macalalad AR, Patel D. Diverse characteristics of the ALK+ NSCLC patients in the United States. Poster presented at: The 16th World Conference on Lung Cancer; September 2015; Denver, CO. | ||
Betts K, Song J, Guo J, Wong W, Ravelo A, Schulz M. Real-world treatment patterns and brain metastases development in ALK-positive non-small cell lung cancer. Poster presented at: The Association of Managed Care Pharmacist (AMCP) Annual Managed Care and Specialty Pharmacy Annual Meeting; April 2016; San Fransisco, CA. | ||
Guérin A, Sasane M, Zhang J, et al. Brain metastases in patients with ALK+ non-small cell lung cancer: clinical symptoms, treatment patterns and economic burden. J Med Econ. 2015;18(4):312–322. | ||
Doebele RC, Lu X, Sumey C, et al. Oncogene status predicts patterns of metastatic spread in treatment-naïve nonsmall cell lung cancer. Cancer. 2012;118(18):4502–4511. | ||
Rangachari D, Yamaguchi N, VanderLaan PA, et al. Brain metastases in patients with EGFR-mutated or ALK-rearranged non-small-cell lung cancers. Lung Cancer. 2015;88(1):108–111. | ||
Toyokawa G, Seto T, Takenoyama M, Ichinose Y. Insights into brain metastasis in patients with ALK+ lung cancer: is the brain truly a sanctuary? Cancer Metastasis Rev. 2015;34(4):797–805. | ||
Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the metropolitan detroit cancer surveillance system. J Clin Oncol. 2004;22(14):2865–2872. | ||
Jena A, Taneja S, Talwar V, Sharma JB. Magnetic resonance (MR) patterns of brain metastasis in lung cancer patients: correlation of imaging findings with symptom. J Thorac Oncol. 2008;3(2):140–144. | ||
Baik CS, Chamberlain MC, Chow LQ. Targeted therapy for brain metastases in EGFR-mutated and ALK-rearranged non-small-cell lung cancer. J Thorac Oncol. 2015;10(9):1268–1278. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.