Back to Journals » Clinical Ophthalmology » Volume 15
Real-World Anti-Vascular Endothelial Growth Factor Therapy Outcomes in Myopic Choroidal Neovascularization
Authors Bhatia D, Mehta A, DaCosta J , Crothers O, Talks JS
Received 22 March 2021
Accepted for publication 27 May 2021
Published 25 June 2021 Volume 2021:15 Pages 2753—2758
DOI https://doi.org/10.2147/OPTH.S311816
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Devangna Bhatia, Alexander Mehta, Joanna DaCosta, Oonagh Crothers, James Stephen Talks
Newcastle Eye Centre, Royal Victoria Infirmary, Newcastle upon Tyne, UK
Correspondence: Devangna Bhatia
Newcastle Eye Centre, Royal Victoria Infirmary, Newcastle upon Tyne, UK
Email [email protected]
Aim: Evaluation of real-world outcomes of intravitreal anti-vascular endothelial growth factor (anti-VEGF) therapy in the primary treatment of choroidal neovascularization (CNV) secondary to pathological myopia.
Patients and Methods: A retrospective cohort analysis of treatment naive patients with myopic CNV who received treatment with either intravitreal ranibizumab or aflibercept over a 12-year period from September 2007 to May 2020 was performed. Baseline features, treatment factors and outcomes were compared between younger and older patients and final visual outcome was assessed for associated factors.
Results: Thirty-seven eyes of 36 patients (24 females, 12 males) were included. Mean age was 58 years (range=26– 89 years). Of these patients, 11/36 (31%) were ≤ 50 years of age and 25/36 (69%) were ≥ 51 years of age. Seventy-three percent (27/37) of eyes were phakic. One patient received bilateral treatment for myopic CNV. Median spherical equivalent was − 8.50 diopters. Seventy percent (26/37) of eyes commenced primary treatment with ranibizumab, and 11/37 (30%) eyes commenced treatment with aflibercept. There were no significant differences between treatment factors and outcomes of younger and older patients. Median number of injections was 3 over a median follow-up period of 24.6 months. Mean CRT decreased by 126μm and median visual improvement was +6 letters. Analysis showed that younger age (p=0.022) and fewer injections (p=0.004) were associated with better visual outcomes.
Conclusion: Myopic CNV requires less frequent anti-VEGF intravitreal therapy over a shorter follow-up period than both neovascular age-related macular degeneration and diabetic macular edema. Increased frequency of administration of intravitreal anti-VEGF treatment did not improve vision. Younger age is associated with a better final visual outcome. These findings may help to advise patients about the prognosis of treatment and help guide treatment decisions.
Keywords: myopia, pathological myopia, choroidal neovascularization, anti-VEGF intravitreal injection
Introduction
High myopia, also termed pathological myopia, is projected to increase in prevalence over time.1 Geographical variation in prevalence rates has been noted. Vitale et al reported an eight-fold increase in high myopia over a 30-year period in the United States, from 0.2% to 1.6%.2
High myopia occurs at considerably higher rates in Asian populations. Lin et al reported that the proportion of myopia attributable to high myopia increased from 10.9% to 21% of Taiwanese students from 1983 to 2000.3 The etiology of high myopia is generally considered to result from a complex interaction between hereditary and environmental factors.
Pathological myopia may be defined as an axial length over 26.5mm and a refractive error greater than −6.00 diopter sphere.4 Associated chorio-retinal abnormalities in these patients such as lacquer cracks, chorioretinal atrophy, pigmentary degeneration, and lattice degeneration have been described.5
Choroidal neovascularization (CNV) occurs in 5–11% of patients with pathological myopia.6 Progressive pathological myopia leads to axial elongation of the eye. This causes structural stretching of chorio-retinal tissue, leading to subsequent thinning. This process together with associated chorio-retinal abnormalities leads to thinned tissue which is relatively ischemic, and upregulation of vascular endothelial growth factor (VEGF) is postulated to occur causing myopic CNV to develop.
Myopic CNV, if untreated, has a poor visual prognosis, leading to progressive irreversible loss of vision and blindness.7 An estimated 89% of patients have marked visual impairment within 5 years of CNV onset.8
Clinical trials have demonstrated the efficacy of anti-vascular endothelial growth factor (anti-VEGF) drugs in the treatment of myopic CNV.9,10 Most studies have reported results over short to medium term follow-up intervals and comparing a younger and older age groups.11,12
The aim of this study was to report the functional and anatomical outcome of intravitreal anti-VEGF therapy in the primary treatment of CNV secondary to pathological myopia in a real-world setting.
Patients and Methods
A retrospective review was conducted of a consecutive series of patients with CNV secondary to myopia who received intravitreal anti-VEGF intravitreal injection treatment between September 2007 and May 2020 in the ophthalmology department of the Royal Victoria Infirmary, Newcastle upon Tyne, UK.
Inclusion criteria were treatment naive patients who received either ranibizumab or aflibercept for myopic CNV. Patients with prior treatment for CNV, including photodynamic therapy and laser photocoagulation, or other causes of CNV, such as neovascular age-related macular degeneration (nAMD), trauma, or angioid streaks, were excluded. Eyes with ocular co-pathology, such as amblyopia, diabetic retinopathy, and glaucoma, and clinically significant cataract to warrant surgical intervention were excluded. Eyes with prior refractive surgery were excluded. All pseudophakic patients underwent their cataract surgery prior to treatment for the myopic CVN. Data collected included patient demographics such as age, gender, and mean spherical equivalent of patients’ habitual correction. Optical coherence tomography (OCT, Heidelberg, Germany) central macular thickness (CRT) at baseline before initiation of treatment, after the third injection and at the last recorded visit was collected. Early treatment diabetic retinopathy (ETDRS) vision at 2 meters with patients’ habitual correction was recorded rather than refracted visual acuity in alignment with the real-world setting of this study. We defined visual stability as maintenance of ETDRS vision ± 5 letters from baseline vision.
Data apart from OCT measurements was recorded in an electronic medical record (Medisoft Ophthalmology, Medisoft Limited, Leeds, UK). The lead clinician and Caldicott Guardian at the hospital gave written permission for anonymized data extraction. Anonymized data analysis of this type does not require ethical approval as it is viewed as audit or service evaluation. This study was conducted in accordance with the principles of the Declaration of Helsinki and the UK Data Protection Act.
Statistical analysis was performed using SPSS (Version 26, Armonk, NY: IBM Corp). Patient demographics, clinical features, treatment measures and outcomes were compared between age groups (≤50 years and ≥51 years). Independent t-test/Mann–Whitney U-tests were used to compare continuous variables depending on normality of distribution (assessed using Kolmogorov–Smirnov and Shapiro–Wilk tests). Associations between categorical variables were analysed using chi-square test/Fisher’s exact probability. To assess factors influencing visual outcome via a multiple regression model at a power of at least 80%, a minimum of 108 observations would have been required.13 Instead, an exploratory correlation analysis was performed across the entire population to determine the effects of baseline BCVA, age, spherical equivalent, duration of treatment and number of injections on final visual outcome. A p-value of <0.05 was considered as statistically significant.
Results
The data set included 37 eyes of 36 patients (24 females, 12 males). The mean age was 58 years (range=26–89 years). Of these patients, 11/36 (31%) were aged ≤50 years and 25/36 (69%) were aged ≥51 years. Seventy-three percent (27/37) of eyes were phakic. One patient received bilateral treatment for myopic CNV. The median spherical equivalent was −8.50 diopters.
Primary treatment with ranibizumab was started in 26/37 (70%) eyes, and in 11/37 (30%) eyes aflibercept was used. The mean number of injections was 4 over a median follow-up period of 24.6 months. For our data set, the mean CRT decreased by 126μm and median visual improvement was +6 letters. Twenty-seven eyes received ≤5 injections over a treatment duration of up to 15 months.
Baseline comparison by age (≤50 years vs ≥51 years) is shown in Table 1. There was a significant difference in lens status (p=0.018) and spherical equivalent (0.011) between age groups. No significant differences were found in comparison of treatment factors and outcomes by age group (Table 2).
 |
Table 1 Baseline Demographics and Clinical Features of Myopic Choroidal Neovascularization Patients by Age Group |
 |
Table 2 Treatment Factors and Outcomes for Myopic Choroidal Neovascularization Patients by Age Group |
Correlation analysis for final BCVA (Table 3) showed that younger age (p=0.044), fewer injections (p<0.001), shorter duration (p<0.001) and higher baseline BCVA (p=0.035) were associated with better visual outcomes. The only significant intercorrelation found was between number of injections and duration of treatment (coefficient 0.903; p<0.001).
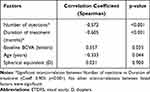 |
Table 3 Analysis of Factors Contributing to Final Visual Acuity in Myopic Choroidal Neovascularization Patients |
Discussion
Our study shows that myopic CNV requires less frequent anti-VEGF intravitreal therapy over a shorter follow-up period than other pathologies such as neovascular age-related macular degeneration and diabetic macular edema. The focus of therapy for neovascular age-related macular degeneration has changed to consideration of the optimal dosing regimen to reduce treatment burden. Regimens such as a treat and extend protocol have been shown to maintain vision with slightly fewer injections when compared to monthly treatments.14 Elman et al, in a 5-year randomized controlled trial of ranibizumab plus prompt or deferred laser therapy for diabetic macular oedema, showed that visual gain (mean gain +7.2 letters in prompt laser group and +9.8 in deferred group) was achieved with a diminished median number of injections in subsequent years, 13 injections over 5 years in prompt laser group and 17 in the deferred laser group.15 In our study, analysis showed that the factors influencing final visual outcome were number of injections (p<0.001), baseline BCVA (p=0.035) and age (p=0.044). A shorter duration of treatment was also significant (p<0.001) but highly correlated to fewer injections. Baseline vision and CRT did not differ between patients younger than or over the age of fifty. All pseudophakic patients underwent their cataract surgery prior to treatment for the myopic CNV.
Our results show that younger patients had better visual outcomes than older patients (p= 0.044). This result is in agreement with similar studies by Bruè et al,12 which suggest that with time the natural progression of myopia leads to chorioretinal atrophy and degeneration, which negatively affects visual outcome in the older age group. Despite the difference in lens status between our age groups (Table 1), the relationship between age and final visual outcome did not differ between phakic and pseudophakic patients.
As this is real-world data collection, our results are affected by varying clinical decisions, diversity of the patient group, and possible variation of the service to provide treatment as planned over time.
In our study, the mean gain in vision at year 1 with myopic CNV was +9 letters. This result is similar to that of Wecker et al,14 who examined 5-year outcomes and injection patterns with pro re nata (PRN, treat as required) treatment regimens for nAMD, DME, RVO and myopic CNV. They found a mean visual gain in year 1 with myopic CNV of +7.2 letters. Their PRN study design limited data collection and analysis to patients with active disease or undergoing follow-up at indicated time points.
We found that an average of 3.88 ranibizumab injections and 2.45 aflibercept injections was needed for maintaining visual stability. This is in agreement with the median number of 3 injections required in the REPAIR9 study which examined 12-month outcomes of ranibizumab in CNV secondary to myopia. REPAIR demonstrated a mean 13.8 letter gain in best corrected visual acuity (BCVA). We did not record a 12-month BCVA due to the real-world setting of our study so may have underestimated gain in visual improvement.
MYRROR10 was a Phase III randomized controlled trial conducted in Asia that demonstrated aflibercept was effective for the treatment of myopic CNV. Patients who received aflibercept gained 13.5 letters and required a median of 3 injections compared to the placebo group with 3.9 letters gained. Our results are similar, in that the patients who received aflibercept gained 15.3 letters after 3 injections compared to an 8.5-letter gain in the ranibizumab group.
Unlike AMD, in which visual acuity outcomes are usually better with more injections,16 we found that more injections (or a longer duration of treatment) were associated with a worse outcome (p<0.001), presumably because patients requiring more injections had more advanced chorioretinal atrophy associated with pathological myopia.
In our study, aflibercept was used less frequently than ranibizumab in the treatment of myopic CNV. The National Institute of Health and Clinical Excellence (NICE) approves treatment for use in the National Health Service (NHS) in the UK. Ranibizumab was approved by NICE for the treatment of myopic CNV in November 2013 and aflibercept in 2017, hence more patients in our study were initially commenced on treatment with ranibizumab.17,18 Aflibercept is a vascular endothelial growth factor (VEGF) inhibitor, which binds two isoforms of VEGF, VEGF-A and VEGF-B, together with placental growth factor (PGF). This is in contrast to ranibizumab which binds VEGF and not PGF. Therefore, aflibercept may be more efficacious at inhibiting the growth of new blood vessels in the choriocapillaris, which promote development of choroidal neovascularization.
Other treatment options for myopic CNV include laser photocoagulation, photodynamic therapy (PDT) and surgical removal. None of these treatments have been proven to maintain visual stability in the long term. Laser photocoagulation poses a risk to the fovea and therefore visual acuity, especially in juxtafoveal cases due to the expansion of the laser scar over time.
The Verteporfin in Photodynamic Therapy (VIP) study19 has shown verteporfin photodynamic therapy (vPDT) to be better than the natural course of the disease or placebo at stabilizing vision loss (<8-letter loss) at 24 months. However, with the emergence of anti-VEGF agents, they have become the more popular option for treatment of myopic CNVs. Their superiority has been proven in the RADIANCE (Ranibizumab And PDT [verteporfIn] evAluation iN myopic Choroidal nEovascularization) study,20 which was a randomized control phase III trial. It compared the efficacy and safety of ranibizumab to vPDT. There was an average BCVA gain of more than 10 ETDRS letters following treatment with ranibizumab compared to approximately 2 ETDRS letters for vPDT. We included treatment naïve patients only in this study and all patients received monotherapy with anti-VEGF agents. We were therefore unable to determine whether a combination treatment regimen with other modalities may be a more or less effective treatment for myopic CNV in this study.
There are potential risks associated with administration of anti-VEGF treatment. In terms of safety, our series had no cases of endophthalmitis, retinal tear or detachment following anti-VEGF injection for myopic CNV. Myopes in general are at a higher risk of developing retinal detachments and tears following an intravitreal injection.21 We did not record any patients with lattice degeneration in our series; however, in such patients, consideration of laser treatment prior to intravitreal injections may be warranted. In pathological myopia, the result of treatment of CNV with intravitreal anti-VEGF agents may induce contraction of the CNV with the resultant development of chorioretinal structural changes leading to fibrosis and atrophy, which may lead to poor visual prognosis.14
A recent retrospective study22 of 96 eyes comparing real-world outcomes of intravitreal anti-VEGF therapies in patients with myopic CNV demonstrated no significant difference in visual improvement after 1 year of treatment between bevacizumab, ranibizumab and aflibercept. By year 3, visual improvement was not significant in the ranibizumab and bevacizumab groups. No difference in the number of injections between the three groups was recorded. Our results differ in that we did not include any patients treated with bevacizumab in our series as this is not a licensed or NICE approved treatment in the UK. Patients ≥51 years required more ranibizumab injections than those ≤50 years and were followed for a longer period.
Our study is limited by its small cohort size. In particular, differences in lens status and refractive correction with younger individuals more likely to wear contact lenses will have influenced visual outcomes. Furthermore, the small sample size introduces a source of bias into interpretation of visual outcomes due to outliers. We did not record axial length as a parameter to define pathological myopia. These factors are important limitations to our study and therefore our results must be interpreted with caution and may not be directly comparable to large scale prospective randomized controlled trials. However, this is a reflection of the real-world nature of our study and our results are useful as a guide to inform patients on likely outcomes for myopic choroidal neovascularization in a practical setting.
We found that myopic CNV requires less frequent anti-VEGF intravitreal therapy over a shorter follow-up period than both neovascular age-related macular degeneration and diabetic macular edema. Increased frequency of administration of intravitreal anti-VEGF treatment did not improve vision. Younger age is associated with a better final visual outcome. These findings may help to advise patients about the prognosis of treatment and help guide treatment decisions.
Further research in terms of real-world studies and the efficacy of newer anti-VEGF agents will optimize current treatment strategies for myopic CNV.
Acknowledgments
The abstract of this paper was presented at the ARVO Annual Meeting 2019, as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Investigative Ophthalmology & Visual Science, July 2019, Vol. 60, 5007: https://iovs.arvojournals.org/article.aspx?articleid=2744416.
Disclosure
Miss Joanna DaCosta reports travel grants from Alimera, outside the submitted work. Mr James Stephen Talks reports personal fees for advisory board and/or research from Bayer, Novartis, and Roche, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi:10.1016/j.ophtha.2016.01.006
2. Vitale S, Sperduto RD, Ferris FL. Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Arch Ophthalmol. 2009;127(12):1632–1639. doi:10.1001/archophthalmol.2009.303
3. Lin L, Shih Y, Hsiao C, Chen C. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore. 2004. Available from: https://pubmed.ncbi.nlm.nih.gov/15008558/.
4. Neelam K, Cheung CMG, Ohno-Matsui K, Lai TYY, Wong TY. Choroidal neovascularization in pathological myopia. Prog Retin Eye Res. 2012;31(5):495–525. doi:10.1016/j.preteyeres.2012.04.001
5. Saw SM, Gazzard G, Shin-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25(5):381–391. doi:10.1111/j.1475-1313.2005.00298.x
6. Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol. 2014;157(1):9–25.e12. doi:10.1016/j.ajo.2013.08.010
7. Holash J, Davis S, Papadopoulos N, et al. VEGF-Trap: a VEGF blocker with potent antitumor effects. Proc Natl Acad Sci U S A. 2002;99(17):11393–11398. doi:10.1073/pnas.172398299
8. Chan NSW, Teo K, Cheung CMG. Epidemiology and diagnosis of myopic choroidal neovascularization in Asia. Eye Contact Lens. 2016;42(1):48–55. doi:10.1097/ICL.0000000000000201
9. Tufail A, Narendran N, Patel PJ, et al. Ranibizumab in myopic choroidal neovascularization: the 12-month results from the Repair Study. Ophthalmology. 2013;120(9):1944–1946. doi:10.1016/j.ophtha.2013.06.010
10. Ikuno Y, Ohno-Matsui K, Wong TY, et al. Intravitreal aflibercept injection in patients with myopic choroidal neovascularization: the MYRROR Study. Ophthalmology. 2015;122(6):1220–1227. doi:10.1016/j.ophtha.2015.01.025
11. Karagiannis D, Kontadakis GA, Kaprinis K, et al. Treatment of myopic choroidal neovascularization with intravitreal ranibizumab injections: the role of age. Clin Ophthalmol. 2017;11:1197–1201. doi:10.2147/OPTH.S135174
12. Bruè C, Pazzaglia A, Mariotti C, Reibaldi M, Giovannini A. Aflibercept as primary treatment for myopic choroidal neovascularisation: a Retrospective Study. Eye. 2016;30(1):139–145. doi:10.1038/eye.2015.199
13. Green SB. How many subjects does it take to do a regression analysis? Multivariate Behav Res. 1991;26(3):499–510. doi:10.1207/s15327906mbr2603_7
14. Wecker T, Ehlken C, Bühler A, et al. Five-year visual acuity outcomes and injection patterns in patients with pro-re-nata treatments for AMD, DME, RVO and myopic CNV. Br J Ophthalmol. 2017;101(3):353–359. doi:10.1136/bjophthalmol-2016-308668
15. Elman MJ, Ayala A, Bressler NM, et al. Intravitreal ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: 5-year randomized trial results. Ophthalmology. 2015;122(2):375–381. doi:10.1016/j.ophtha.2014.08.047
16. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. doi:10.1056/nejmoa054481
17. NICE. Overview. Ranibizumab for treating choroidal neovascularisation associated with pathological myopia. Guidance. NICE; 2013.
18. NICE. Overview. Aflibercept for treating choroidal neovascularisation. Guidance. NICE; 2017.
19. Blinder KJ, Blumenkranz MS, Bressler NM, et al. Verteporfin therapy of subfoveal choroidal neovascularization in pathologic myopia: 2-year results of a randomized clinical trial–VIP report no. 3. Ophthalmology. 2003;110(4):667–673. doi:10.1016/S0161-6420(02)01998-X
20. Wolf S, Balciuniene VJ, Laganovska G, et al. RADIANCE: a randomized controlled study of ranibizumab in patients with choroidal neovascularization secondary to pathologic myopia. Ophthalmology. 2014;121(3):682–692.e2. doi:10.1016/j.ophtha.2013.10.023
21. Karabag RY, Parlak M, Cetin G, Yaman A, Osman Saatci A. Retinal tears and rhegmatogenous retinal detachment after intravitreal injections: its prevalence and case reports. Digit J Ophthalmol. 2015;21(1):8–10. doi:10.5693/djo.01.2014.07.001
22. Corazza P, Kabbani J, Soomro T, Alam MMR, D’Alterio FM, Younis S. Three-year real-world outcomes of intravitreal anti-VEGF therapies in patients affected by myopic choroidal neovascularization. Eur J Ophthalmol. 2020;112067212096345. doi:10.1177/1120672120963455
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
