Back to Journals » International Medical Case Reports Journal » Volume 16
Rare Unilateral Twin Ectopic Pregnancy After Frozen Embryo Transfer: A Case Report and Literature Review
Authors Zhang Y, Lu X, Wang X, Wu X, Jing X, Cui X
Received 2 September 2023
Accepted for publication 4 November 2023
Published 13 November 2023 Volume 2023:16 Pages 731—737
DOI https://doi.org/10.2147/IMCRJ.S409492
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Yuxia Zhang,1 Xiaobing Lu,1 Xianping Wang,1 Xueqing Wu,1 Xuan Jing,2 Xiangrong Cui1
1Reproductive Medicine Center, the Affiliated Children’s Hospital of Shanxi Medical University, Children’s Hospital of Shanxi, Shanxi Maternal and Child Health Hospital, Taiyuan, 030001, People’s Republic of China; 2Clinical Laboratory, Shanxi Provincial People’s Hospital (Fifth Hospital) of Shanxi Medical University, Taiyuan, 030001, People’s Republic of China
Correspondence: Xiangrong Cui; Xuan Jing, Email [email protected]; [email protected]
Background: Unilateral twin ectopic pregnancy is extremely rare in natural pregnancy, with an incidence rate of only 1 in 200,000– 2,500,000, represents a major health risk for reproductive-aged women, leading to even life-threatening complications. There is a lack of data on the prevalence of this rare disease after in-vitro fertilization-embryo transfer (IVF-ET) cycles.
Case Report: We present a case of a 51-year-old woman with rare unilateral twin ectopic pregnancy after frozen embryo transfer treated with bilateral salpingectomy, followed by a review of the literature.
Conclusion: Twin ectopic pregnancy is a very rare type of pregnancy that requires a high index of suspicion to diagnose and treat early to prevent complications and maternal death.
Keywords: twin ectopic, pregnancy, unilateral, rare condition, assisted reproductive technology
Introduction
In-vitro fertilization-embryo transfer (IVF-ET) is an important component of assisted fertility technology, and ectopic pregnancy (EP) is one of the common complications of IVF-ET.1 The incidence of ectopic pregnancy in ART cycle is 1% ~ 5%, which is more than 2 times higher than that in natural cycle.2 Unilateral twin ectopic pregnancy is extremely rare in natural pregnancy, with an incidence rate of only 1 in 200,000–2,500,000, represents a major health risk for reproductive-aged women, leading to even life-threatening complications.3,4 Since the first case of unilateral twin tubal pregnancy was reported by De Ott in 18915, an average of one case per year is reported in the literature.6 Assisted reproductive technology (ART) is responsible for the increase in twin tubal pregnancy.7 The misdiagnosis or delayed diagnosis of EP leads to severe bleeding, hypovolemic shock, and other complications, which are related to the maternal incidence rate and mortality. Fallopian tube destruction due to tubal surgery or inflammation, especially chlamydia infection, is a major risk factor for tubal pregnancy. The quantity and quality of transferred embryos, the control of ovarian stimulation (COS) programs, laboratory conditions, and transfer technologies are considered as possible factors for EP after IVF-embryo transfer (ET).8 The accurate management strategy for patients at risk of ectopic pregnancy after IVF-ET has not been established.8 This report describes a case of 51-year-old patient with unilateral twin ectopic pregnancy that occurred after embryo transfer.
Case Report
A 51-year-old woman with an 11-year history of secondary infertility was referred to the IVF program. During her first marriage, she gave birth to a baby girl in 1998 and a baby boy in 2001, and had abortions in 2005 and 2008, respectively. She remarried in 2012 and had a salpingography in 2015, which showed that bilateral fallopian tubes were patency. She had no history of abdomino/pelvic surgery or dilation and curettage.
In this treatment cycle, antagonist protocol and recombinant follicle-stimulating hormone (rFSH) stimulation starting from day 3 of the menstrual cycle were used for ovulation induction. Follicular development was monitored by plasma estradiol (E2) and transvaginal ultrasonography (TVUSG). On the 13th day of the cycle, with follicles over 18mm and estradiol levels of 1052 ng/mL, 8000 IU of human chorionic gonadotropin (hCG) was administered. Eight oocytes were retrieved by transvaginal sonographic aspiration 36 hours after hCG. On day 3 of culture, three embryos of the 4- to 8-cell stages were transferred. The procedure was done atraumatically and clearly demonstrated ustrasonographically. The embryos were transferred in a total of 25 μL of culture medium and the patient received luteal support. Ten days after the transfer of the embryos, the serum β-hCG values are 114.2 U/L. Serial monitoring of serum β-hCG values are shown in Figure 1.
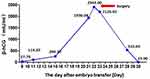 |
Figure 1 The β-HCG changes after embryo transfer and surgery. |
The patient’s vital signs were unstable at the emergency room: blood pressure, 76/55mmHg; pulse rate, 77 beats/min. Despite the increase in β-hCG values during the hospital follow-up, 29 days after the embryo transfer, the β-hCG levels were 2408 U/L and the serum progesterone (P4) level was 13.30 ng/mL. Transvaginal ultrasonography revealed no gestational sac in the uterine cavity but 2 gestational sacs with 2 yolk sacs at the left adnexa, the endometrial thickness was 9.5mm, and an unilateral twin ectopic pregnancy was diagnosed (Figure 2). The presence of approximately 9×8mm hypoechoic nodules between the anterior uterine wall muscles suggests the possibility of uterine fibroids (Figure 2). Operative findings showed that there was a 4-cm ectopic mass with active bleeding in the ampulla of the left fallopian tube. She underwent bilateral salpingectomy, and the postoperative course was uncomplicated. Gross pathologic and histologic assessments confirmed the 2 distinct pregnancies at the same tube. The twins were dichorionic and diamniotic (Figure 3). The patient had an uneventful recovery. The levels of β-hCG had returned to below 50 U/L at the 3rd postoperative week (Figure 1).
Discussion
Ectopic pregnancy refers to implantation of the embryo outside the endometrial cavity, with an incidence of 1–2% in all pregnancy types.9 The incidence of ectopic pregnancy accounts for 2.1–9.4% of all clinical pregnancies after IVF.10 The most common implantation site outside the endometrial cavity is the fallopian tube, accounting for more than 90%.11 Other implantation sites include ovaries, cervix, abdominal cavity, cesarean section scar, or stroma.12
Twin ectopic pregnancy occurs in 1:20,000 up to 1:125,000 pregnancies of ectopic pregnancy, and it is an extremely rare condition, which is the implantation of both embryos outside of the endometrial lining.12 It can usually be implanted on the fallopian tubes, but double ectopic implantation of ovaries, abdomen, cesarean section scars, corneas, and cervix have also been reported.13 In the cases of twin tubal pregnancies, most were reported to be bilateral ectopic pregnancy, while a few were unilateral tubal pregnancies. In the present report, the implantation was on the left side of the uterine tube after IVF.
The incidence of ectopic pregnancy appears to increase after IVF-ET treatment compared to natural pregnancies. As the number of IVF procedures continues to increase, the incidence of ectopic pregnancy and bilateral ectopic pregnancy may also rise.14 Unilateral or bilateral tubal pathology, past pelvic surgery, and pelvic infection are associated with EP. Recent studies have shown that pelvic inflammation and subsequent blockage of the fallopian tubes have been described as risk factors for EP after natural and assisted conception.15 In addition, risk factors for ectopic pregnancy after IVF include advanced maternal age, pre-existing fallopian tube disease, transferring multiple embryos, poor embryo quality, and loading embryos in high-volume media. According to the theory of “spray effect”, the volume of transport medium should not exceed 20 μL.16 In addition to transferring two embryos, poor embryo quality and advanced maternal age were predisposing risk factors for ectopic pregnancy in our present patient.17 It has also been reported that the use of gonadotropin-releasing hormone (GnRH) analogues may be associated with higher EP rates in the IVF population. In the process of ovulation induced by gonadotropin, high levels of estrogen affect peristaltic movement of fallopian tube and migration of embryos.18 Some rare ectopic pregnancies in assisted reproduction, such as intrauterine and extrauterine pregnancies, bilateral tubal pregnancies, cervical pregnancies, and ovarian pregnancies, are significantly higher than natural pregnancies.19
Unilateral tubal twin pregnancies (Table 1) after ICSI-ET have only been reported in a small number of cases.20–38 The most reliable technique for diagnosing EP is TVUSG. Intrauterine pregnancy sac loss with elevated β-hCG levels is consistent with abnormal pregnancy.20 Continuous β-hCG levels can also be used for diagnosis. In viable intrauterine pregnancies, the minimum elevation of β-hCG within 2 days is 53%.1 The minimum reduction in spontaneous abortion within 2 days is 21% to 35%, depending on the initial level.1 A rise or fall in β-hCG values below these values indicates an ectopic pregnancy.
 |
Table 1 Recent Cases for Unilateral Twin Ectopic Pregnancy |
In this case, an initial rapid rise in β-hCG levels was observed, possibly caused by two sources of hormone production (unilateral twin ectopic pregnancy). This also led to the misconception that it was an intrauterine pregnancy. The combined use of ultrasound, pelvic examination, and follow-up of serum β-hCG levels is a key factor in the appropriate management of current cases. Close follow-up with ultrasound and physical examination helped us to diagnose and treat this case early. Moreover, dual gestational sac trophoblastic activity results in a higher β-hCG than a single gestational sac, which may confuse the clinician’s decision. Delay in diagnosing tubal ectopic pregnancy might lead to severe intraabdominal bleeding and even maternal death. However, in our case, accurate follow-up by expert doctors enabled us to successfully manage patients and clinical doctors in the early stages.
Conclusions
In conclusion, ectopic pregnancy, including unilateral twin ectopic pregnancy, is a known risk of IVF. Women who experience irregular vaginal bleeding and lower abdominal pain during the process of abortion after assisted reproductive technology should promptly seek medical treatment and physical examination at a hospital with good conditions, including gynecological examination, quantitative determination of blood and urine HCG, and high-definition color ultrasound examination to determine the clinical pregnancy situation. If no intrauterine pregnancy is found, in order to make a clear diagnosis as soon as possible for patients with indications, appropriate timing for laparoscopic examination can be chosen. This case report highlights the importance of maintaining a high index of suspicion in patients with an acute abdomen and the need for close monitoring and timely surgical intervention. Further research and clinical reports are warranted to improve our understanding of this uncommon condition and optimize its management.
Ethics Approval and Consent to Participate
The protocol was approved by the Ethics Committee of Shanxi Maternal and Child Health Care Hospital (IRB-KY-2017).
Consent for Publication
The patient’s written consent has been obtained for publication.
Funding
This study was supported by National Natural Science Foundation of China (grant no. 82000722 and 82000302), Natural Science Foundation of Shanxi (grant no. 201901D211519 and 201901D211546), Research Project Supported by Shanxi Scholarship Council of China (grant no. HGKY2019092), China Postdoctoral Science Foundation (grant no. 2020 M670703), Initial Scientific Research Fund of PhD in Shanxi Provincial People’s Hospital (grant no. b201635), Fund Program for the Scientific Activities of Selected Returned Overseas Professionals in Shanxi Province (grant no. 20200033 and 20220050), Key Research and Development Projects of Shanxi Province (grant no. 188821) and Medical and Technological Innovation Team of Shanxi (grant no. 2020TD19).
Disclosure
The authors declare that they have no competing interests.
References
1. Wang S, Qi L, Liu Y, et al. Suitable endometrial thickness on embryo transfer day may reduce ectopic pregnancy rate and improve clinical pregnancy rate. BMC Pregnancy Childbirth. 2023;23(1):517. doi:10.1186/s12884-023-05837-6
2. Liu Z, Jing C. A Case Report of Retroperitoneal Ectopic Pregnancy After in vitro Fertilization-Embryo Transfer and Literature Review. Int J Womens Health. 2023;15:679–693. doi:10.2147/IJWH.S408319
3. Ozturk E, Akturk H. Sonographically Positive Fetal Heartbeat in Unilateral Tubal Twin Pregnancy as a Rare Case With Literature Review. Cureus. 2023;15(5):e39697. doi:10.7759/cureus.39697
4. Gure Eticha T. Unilateral Twin Ectopic Pregnancy: a Case Report from the Eastern Part of Ethiopia, Harar. Int Med Case Rep J. 2022;15:521–527. doi:10.2147/IMCRJ.S382708
5. De Los Rios JF, Castaneda JD, Miryam A. Bilateral ectopic pregnancy. J Minim Invasive Gynecol. 2007;14(4):419–427. doi:10.1016/j.jmig.2007.01.011
6. Lategan HE, Gillispie VC. Spontaneous Unilateral Tubal Twin Ectopic Pregnancy. Ochsner J. 2019;19(2):178–180. doi:10.31486/toj.17.0110
7. Elsayed S, Farah N, Anglim M. Heterotopic Pregnancy: case Series and Review of Diagnosis and Management. Case Rep Obstet Gynecol. 2023;2023:2124191. doi:10.1155/2023/2124191
8. Hashemi S, Arabipoor A, Kohestani S, et al. The Predictive Value of Serum ss-HCG Levels in The Detection of Ectopic Pregnancy Sixteen Days after Embryo Transfer: a Cross-Sectional Study. Int J Fertil Steril. 2023;17(3):181–186. doi:10.22074/ijfs.2022.546087.1247
9. Wang YN, Zheng LW, Fu LL, Xu Y, Zhang XY. Heterotopic pregnancy after assisted reproductive techniques with favorable outcome of the intrauterine pregnancy: a case report. World J Clin Cases. 2023;11(3):669–676. doi:10.12998/wjcc.v11.i3.669
10. Cirillo F, Paladino I, Ronchetti C, et al. Ectopic pregnancy risk factors in infertile patients: a 10-year single center experience. Sci Rep. 2022;12(1):20473. doi:10.1038/s41598-022-24649-w
11. Shen Y-T, Yang -Y-Y, Zhang P-G, et al. Tubal ectopic pregnancy: a retrospective cohort study on clinical characteristics, treatment options and reproductive outcomes within 5 years. Arch Gynecol Obstet. 2022;306(6):2055–2062. doi:10.1007/s00404-022-06690-2
12. Garg N, Milad MP. Female sterilization reversal in the era of in-vitro fertilization. Curr Opin Obstet Gynecol. 2022;34(4):244–249. doi:10.1097/GCO.0000000000000802
13. Naredi N, Tripathy SR, Sharma R. Transvaginal Ultrasound-Guided Methotrexate Instillation for Failed Medical Management of Ectopic Pregnancies in Subfertile Women. J Hum Reprod Sci. 2022;15(1):90–95. doi:10.4103/jhrs.jhrs_1_22
14. Luo X, Li L, Lin N, et al. Low Endogenous LH on the COS Initiation Day of a GnRH-Agonist Regimen Increases the Risk of Early Pregnancy Loss and Adverse ART Outcomes. Front Endocrinol (Lausanne). 2022;13:830567. doi:10.3389/fendo.2022.830567
15. Anh ND, Hai NX, Ha N-TT, et al. Retroperitoneal ectopic pregnancy after in vitro fertilization: a case report of a patient with bilateral salpingectomy. Radiol Case Rep. 2022;17(3):721–724. doi:10.1016/j.radcr.2021.12.011
16. Kong M, Paramesparan K, Keshvala C, Shah A. Acute abdomen or life-threatening heterotopic pregnancy with tubal rupture: where does imaging play a role? BMJ Case Rep. 2020;13(12):e239178. doi:10.1136/bcr-2020-239178
17. Tan Y, Bu ZQ, Shi H, Song H, Zhang YL. Risk Factors of Recurrent Ectopic Pregnancy in Patients Treated With in vitro Fertilization Cycles: a Matched Case-Control Study. Front Endocrinol (Lausanne). 2020;11:552117. doi:10.3389/fendo.2020.552117
18. Osada H, Teramoto S, Kaijima H, et al. Managing Ectopic Pregnancies by Targeting Chorionic Villi with a Transvaginal Injection of Ethanol into the Lacunar Space. Biomedicines. 2020;8(7):202. doi:10.3390/biomedicines8070202
19. Xu H, Feng G, Wei Y, et al. Predicting Ectopic Pregnancy Using Human Chorionic Gonadotropin (hCG) Levels and Main Cause of Infertility in Women Undergoing Assisted Reproductive Treatment: retrospective Observational Cohort Study. JMIR Med Inform. 2020;8(4):e17366. doi:10.2196/17366
20. Kasum M. Unilateral twin tubal pregnancy and subsequent heterotopic pregnancy in a patient following in vitro fertilization. Acta Clin Croat. 2009;48:451–454.
21. Rolle CJ, Wai CY, Bawdon R, Santos-Ramos R, Hoffman B. Unilateral twin ectopic pregnancy in a patient with a history of multiple sexually transmitted infections. Infect Dis Obstet Gynecol. 2006;2006:10306. doi:10.1155/IDOG/2006/10306
22. Urunsak I, Kadayifci O, Atay Y, Demir S, Guzel AB. A unilateral tubal twin pregnancy. Ann Saudi Med. 2006;26(4):333. doi:10.5144/0256-4947.2006.333
23. Goker EN, Tavmergen E, Ozcakir HT, Levi R, Adakan S. Unilateral ectopic twin pregnancy following an IVF cycle. J Obstet Gynaecol Res. 2001;27(4):213–215. doi:10.1111/j.1447-0756.2001.tb01253.x
24. Gualandi M, Steemers N, de Keyser JL. First reported case of preoperative ultrasonic diagnosis and laparoscopic treatment of unilateral, twin tubal pregnancy. Rev Fr Gynecol Obstet. 1994;89(3):134–136.
25. Sur SD, Reddy K. Spontaneous unilateral tubal twin pregnancy. J R Soc Med. 2005;98(6):276. doi:10.1177/014107680509800612
26. Pattanasuttinont S. Rupture of unilateral twin tubal pregnancy. J Med Assoc Thai. 2008;91(2):249–252.
27. Summa B, Meinhold-Heerlein I, Bauerschlag DO, et al. Early detection of a twin tubal pregnancy by Doppler sonography allows fertility-conserving laparoscopic surgery. Arch Gynecol Obstet. 2009;279(1):87–90. doi:10.1007/s00404-008-0648-x
28. Karadeniz RS, Dilbaz S, Ozkan SD. Unilateral twin tubal pregnancy successfully treated with methotrexate. Int J Gynaecol Obstet. 2008;102(2):171. doi:10.1016/j.ijgo.2008.03.012
29. Dede M, Gezginç K, Yenen M, et al. Unilateral tubal ectopic twin pregnancy. Taiwan J Obstet Gynecol. 2008;47(2):226–228. doi:10.1016/S1028-4559(08)60089-3
30. Arikan DC, Kiran G, Coskun A, Kostu B. Unilateral tubal twin ectopic pregnancy treated with single-dose methotrexate. Arch Gynecol Obstet. 2011;283(2):397–399. doi:10.1007/s00404-010-1449-6
31. Longoria TC, Stephenson ML, Speir VJ. Live unilateral twin ectopic pregnancy in a fallopian tube remnant after previous ipsilateral salpingectomy. J Clin Ultrasound. 2014;42(3):169–171. doi:10.1002/jcu.22074
32. Vohra S, Mahsood S, Shelton H, Zaedi K, Economides DL. Spontaneous live unilateral twin ectopic pregnancy - A case presentation. Ultrasound. 2014;22(4):243–246. doi:10.1177/1742271X14555565
33. Ghanbarzadeh N, Nadjafi-Semnani M, Nadjafi-Semnani A, Nadjfai-Semnani F, Shahabinejad S. Unilateral twin tubal ectopic pregnancy in a patient following tubal surgery. J Res Med Sci. 2015;20(2):196–198.
34. Kim CI, Lee TY, Park ST, Kim HB, Park SH. A rare case of spontaneous live unilateral twin tubal pregnancy with both fetuses presenting with heart activities and a literature review. Obstet Gynecol Sci. 2018;61(2):274–277. doi:10.5468/ogs.2018.61.2.274
35. Betti M, Vergani P, Damiani GR, et al. Unilateral twin tubal pregnancy: a case report and review of the literature. Acta Biomed. 2018;89(3):423–427. doi:10.23750/abm.v89i3.6915
36. Seak CJ, Goh ZNL, Wong AC, Seak JC, Seak CK. Unilateral live twin tubal ectopic pregnancy presenting at 12 weeks of gestation: a case report. Medicine (Baltimore). 2019;98(38):e17229. doi:10.1097/MD.0000000000017229
37. Martin A, Balachandar K, Bland P. Management of a spontaneously conceived live unilateral twin ectopic pregnancy in Australia: a case report. Case Rep Womens Health. 2021;30:e00300. doi:10.1016/j.crwh.2021.e00300
38. Samha R, AlAwad Y, Wardeh AM, Ibrahem AM, Abo Moughdeb AK. A unilateral twin ectopic pregnancy in the fallopian tube: a rare case report. Int J Surg Case Rep. 2023;111:108833. doi:10.1016/j.ijscr.2023.108833
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


