Back to Journals » Clinical Ophthalmology » Volume 14
Rapid Structural and Functional Improvements with the 0.19 mg Fluocinolone Acetonide Intravitreal Implant for Patients with DME and Low Visual Acuity: 6-Month Data from the UAE
Authors Elbarky AM
Received 15 November 2019
Accepted for publication 28 January 2020
Published 16 March 2020 Volume 2020:14 Pages 823—830
DOI https://doi.org/10.2147/OPTH.S238740
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ahmed Mohammed Elbarky1,2
1Vitreoretinal consultant, Sheikh Khalifa Medical City, Abu Dhabi, United Arab Emirates; 2Department of Ophthalmology, Benha Faculty of Medicine, Benha University, Benha, Egypt
Correspondence: Ahmed Mohammed Elbarky Email [email protected]
Purpose: The 0.19 mg fluocinolone acetonide (FAc) intravitreal implant is approved in the United Arab Emirates (UAE) for treating diabetic macular edema (DME) in patients previously treated with a course of corticosteroids and that did not have a clinically significant rise in intraocular pressure (IOP). This ongoing study is assessing its effectiveness and safety in pseudophakic patients with DME in clinical practice from a single center in the UAE.
Methods: A retrospective, ongoing 6-month audit study (NCT03590587), in which 22 eyes from 22 patients were treated with a single FAc intravitreal implant after treatment with a prior course of corticosteroids. Outcomes assessed included mean changes in best-corrected visual acuity (BCVA), central macular thickness (CMT), and IOP. Six-month follow-up data are presented.
Results: After FAc implantation, mean BCVA improved rapidly, increasing by 25.4 ± 3.0 letters (mean±SEM) from baseline to Month 6 (p< 0.0001). At 6 months, BCVA had improved by 15 letters or more in 91% of eyes (n=20/22). Mean CMT decreased by 267.0 ± 20.1 μm from baseline to Month 6 (p< 0.0001). Over 85% of eyes (n=19/22) had a CMT less than 300 μm at 6 months. Mean IOP increased by 2.9 ± 0.7 mmHg from baseline to Month 6 (p< 0.001). All eyes except 2 had an IOP of 21 mmHg or lower. At Month 6, five eyes (23%) needed IOP-lowering therapy.
Conclusion: Injection of the FAc intravitreal implant rapidly and significantly improved BCVA and CMT within 6 months. These rapid and significant improvements exceed those reported in other real-world studies. Safety signals were consistent with corticosteroid class effects. The FAc implant may be a useful treatment option for patients in the UAE, particularly those with sight threatening DME requiring rapid functional improvements.
Keywords: diabetic macular edema, fluocinolone acetonide intravitreal implant, clinical evidence
Introduction
Diabetic macular edema (DME) is associated with retinal thickening of the central area of the retina, known as the macula, caused by accumulation of fluid leading to development of edema or swelling, and is linked with severity of diabetic retinopathy.1 Estimates suggest that the prevalence of DME in patients with diabetic retinopathy increases with the duration of diabetes.2,3
DME is the leading cause of vision loss among patients with diabetic retinopathy2 and significantly impacts a patient’s quality of life. That includes poor visual functioning, restricted social and psychological well-being, and the inability to perform daily activities.4
If left untreated, swelling in the macula can cause vision problems that worsen over time, and can lead to an irreversible vision loss.5 Early diagnosis and effective treatment of DME are, therefore, essential to prevent visual impairment and avoid declines in vision-related quality of life as a result of declining visual acuity.6 Current treatment guidelines for DME generally recommend anti-vascular endothelial growth factor (anti-VEGF) therapy first line and corticosteroid therapy second line.7–9
First-line intravitreal anti-VEGF injections, such as ranibizumab, rapidly and effectively reduce edema and substantially improve visual acuity and anatomical outcomes.10 Not all patients with DME respond, however, with up to half showing some persistent edema after anti-VEGF treatment alone.11 Furthermore, the frequency and burden of anti-VEGF injections limits patients’ adherence, presenting a major challenge to delivering effective patient care.11
For patients whose DME is considered insufficiently responsive to anti-VEGF injections, second-line treatment with intravitreal injections of corticosteroids, such as triamcinolone, has been shown to be beneficial.12,13 Corticosteroids reduce the expression of VEGF and other factors involved in vascular leakage, and suppress the influx of inflammatory cells into the retina.10 Treatment with systemic steroids is not feasible for DME due to their potential to cause harmful side effects.10 This, and the desire to reduce the clinical and patient burden of repeated injections and clinic visits, led to the development of two intravitreal corticosteroid implants: dexamethasone and fluocinolone acetonide (FAc).
Both dexamethasone (OZURDEX® 700 µg; Allergan Ltd, Marlow, Buckinghamshire, UK) and FAc implant (ILUVIEN® 190 µg; Alimera Sciences Inc., Atlanta, GA, USA) are licensed in Europe and the USA for the treatment of DME that persists or recurs despite treatment.14,15 Both implants are effective in the treatment of DME,10,16–18 with the FAc implant offering improved convenience and a reduced clinical burden compared with the dexamethasone due to the longer duration of action of a single intravitreal injection. While the latter is short-acting (its effects lasting for around 6 months before re-injection is required), the FAc implant is designed to deliver inflammation-suppressing FAc over a period of up to 3 years, with a daily release rate of 0.2 µg.10
The United Arab Emirates (UAE) Health Authority approved reimbursement for the FAc intravitreal implant in October 2016 for patients with DME who have previously received a course of corticosteroids and did not have a significant rise in intraocular pressure (IOP).19 A number of multicenter real-world studies including the Medisoft audit in the UK,20 the USER study in the USA,21 the IRISS study in Germany, Portugal and the UK,22 and the RESPOND study in Portugal,23 have confirmed the safety and effectiveness profile previously demonstrated in clinical trials. To our knowledge, no study has yet examined the effectiveness and safety of the FAc intravitreal implant in clinical practice in a UAE population.
The objective of the current study is to assess the effectiveness and safety of the FAc intravitreal implant in patients with DME and a pseudophakic lens, and treated in clinical practice in the UAE.
Materials and Methods
Study Design
This is a retrospective, single-center 6-month (September 2017–March 2018) audit study, in patients with a pseudophakic lens and DME that persisted or recurred despite treatment. Patients were treated at the Sheikh Khalifa Medical City in Abu Dhabi, UAE, and received the FAc implant after having previously received a course of corticosteroid treatment. The trial is registered with ClinicalTrials.gov (NCT03590587).24 Data for the first 6 months of the study are presented. The study was approved by the ethical committee of the Sheikh Khalifa Medical City in Abu Dhabi, UAE. All patients gave their written informed consent, and procedures were performed according to the ethical standards of the 1964 Declaration of Helsinki and its later amendments,25 the International Conference on Good Clinical Practice guidelines,26 and all applicable country-specific regulatory requirements.
Patients and Study Procedures
For inclusion in the study, patients were required to be pseudophakic, have DME (duration ≥6 months and DME that persisted or recurred despite treatment), and had received a prior course of corticosteroid treatment during therapy. Patients were excluded if they had any maculopathy, macular edema not related to diabetes, or history of posterior uveitis. A single FAc intravitreal implant (ILUVIEN) was injected into the affected eye according to product labeling.19
Outcomes
Outcomes were analyzed at baseline and then at Months 1, 3, and 6 after receiving the FAc intravitreal implant. Effectiveness evaluations were mean changes in best-corrected visual acuity (BCVA; measured using the Early Treatment Diabetic Retinopathy Study [ETDRS] scale) and central macular thickness (CMT). Safety was evaluated in terms of mean change in IOP.
Data and Statistical Analysis
Student’s paired t-tests were used to assess changes from baseline, and to establish significance between paired samples. A p-value of <0.05 was defined as statistically significant. Data are reported as mean ± standard error of the mean (SEM) unless otherwise stated.
Results
Patient Population
Patient demographics and baseline characteristics are shown in Table 1. In total, 22 pseudophakic eyes from 22 patients were included in the study. The patients’ mean age was 67 (range: 51–79) years, and half were female (n=11; 50%). Duration of DME was more than 6 months in all eyes of which the majority (n=17; 77%) had non-proliferative diabetic retinopathy. All eyes had received at least one prior anti-VEGF treatment (mean of 6.8 ranibizumab intravitreal injections and 2.8 of aflibercept in eyes that were treated) for DME (ranibizumab was the most common [n=21; 95%]). For inclusion, all patients had received prior treatment with a dexamethasone implant.
 |
Table 1 Patient Demographics and Baseline Characteristics |
Effectiveness
Best-Corrected Visual Acuity
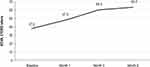
At baseline, mean BCVA was 37.6 ± 3.3 ETDRS letters. After FAc implantation, mean BCVA improved rapidly, increasing by 10.4 ± 2.0 letters from baseline to Month 1, by 22.8 ± 2.9 letters at Month 3, and by 25.4 ± 3.0 letters at Month 6 (p<0.0001 versus baseline; Figure 1). The mean BCVA after 6 months of FAc treatment was 63.0 ± 3.5 letters, although most eyes achieved rapid increases in the first few months of treatment. By Month 3, almost two-thirds (n=15/22; 68%) of eyes had already achieved 80% of the mean gain in BCVA at 6 months (data not shown).
One month after FAc implantation, BCVA had already improved by 5 or more letters in 77% of eyes (n=17/22). This rose to 91% of eyes (n=20/22) by Month 3. Similarly, after 1 month, BCVA had improved by 15 letters or more in more than half of the eyes (n=13/22; 59%), which rose to 86% of eyes (n=19/22) after 3 months and 91% (n=20/22) after 6 months (Figure 2).
After 6 months, BCVA had improved from baseline in all eyes except 2. In these eyes, BCVA decreased by 11.1 and 0 letters from baseline to 6 months. After 6 months, 14 eyes (64%) had a BCVA of more than 65 letters, and 5 eyes (23%) had a BCVA of more than 70 letters.
Central Macular Thickness
At baseline, mean CMT was 534.3 ± 19.4 µm (Table 1). After FAc implantation, CMT decreased by 171.5 ± 15.5 µm, 240.9 ± 15.8 µm, and 267.0 ± 20.1 µm from baseline to Months 1, 3, and 6, respectively (p<0.0001 versus baseline; Figure 3). The mean CMT after 6 months of FAc treatment was 267.3 ± 7.4 µm, but rapid reductions were seen in the first few months of treatment. Almost 1 in 5 eyes (18%; n=4/22) had achieved 80% of this value after just 1 month, and almost three-quarters of eyes (91%; n=20/22) had achieved 80% of this value by 3 months (data not shown).
 |
Figure 3 Mean change from baseline in CMT at 1, 3, and 6 months after FAc implantation. Abbreviations: CMT, central macular thickness; FAc, fluocinolone acetonide. |
One month after FAc implantation, all eyes had achieved CMT reductions of 50 µm or more, and 86% had CMT reductions of 100 µm or more (n=19/22). By 3 months, all eyes had CMT reductions of at least 100 µm, and 86% (n=19/22) and 55% (n=12/22) had achieved reductions of 150 µm and 250 µm or more, respectively. After 6 months, 3 eyes (14%) had CMT reductions of more than 350 µm (Figure 4). Over 85% of eyes (n=19/22) had a CMT less than 300 µm at 6 months.
Safety
Intraocular Pressure
At baseline, mean IOP was 15.1 ± 0.6 mmHg (Table 1). After FAc implantation, mean IOP increased slightly: by 1.3 mmHg, 2.5 mmHg, and 2.9 mmHg from baseline at Months 1, 3, and 6, respectively (p>0.05 for Month 1, p<0.001 for Months 3 and 6 versus baseline). Mean IOP after 6 months was 18.0 ± 0.8 mmHg (Figure 5).
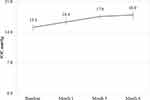 |
Figure 5 Error bars represent standard error of the mean for all eyes at each timepoint (n=22). Abbreviations: FAc, fluocinolone acetonide; IOP, intraocular pressure. |
After 6 months, the mean increase in IOP was 2.9 mmHg. After 6 months, fewer than a quarter of eyes (n=5/22; 23%) experienced an increase in IOP of more than 5 mmHg, and only 1 eye showed an increase of more than 10 mmHg (an increase of 14.0 mmHg; data not shown). During the 6-month period, 5 eyes (23%) experienced increases in IOP of ≥21 mmHg and required IOP-lowering therapy (dorzolamide hydrochloride alone or in combination with tafluprost/travoprost and brimonidine). None of these eyes required surgery to manage IOP. Further, by Month 6, 20 of the 22 eyes had an IOP below 21 mmHg and the remaining two eyes were being managed with IOP-lowering therapy.
Other Findings
Supplemental Therapy
During the study period, only one eye required supplemental therapy and a single intravitreal injection of ranibizumab was administered at Month 6.
Vitrectomy
A prior vitrectomy had been conducted in two eyes prior to therapy with the FAc intravitreal implant and outcomes were similar to the study group. In these two eyes, BCVA improved rapidly, increasing by 34.9 letters (from a baseline of 35.0 letters) and 19.9 letters (from 50.1 letters) at Month 6. In these two eyes, ≥15 letters were achieved after 1 and 3 months, respectively. These changes were accompanied by decreases in CMT of 305.0 µm (from 538.0) and 142.0 µm (from 396.0 µm) at Month 6. The time taken to achieve a CMT below 300 µm ranged between 1 and 3 months. In both eyes, IOP remained below 21 mmHg at Month 6 and one of the eyes was being managed with IOP-lowering therapy, which was started at Month 3.
Discussion
In this retrospective real-world study in the UAE, the injection of a single FAc intravitreal implant rapidly and significantly improved BCVA and CMT outcomes within 6 months, in pseudophakic patients with DME after a prior course of corticosteroid therapy. Safety signals were consistent with corticosteroid class effects: small elevations in IOP were controlled with IOP-lowering medications when necessary. While the effectiveness and safety of the FAc implant in both phakic and pseudophakic patients has been shown previously in both real-world studies and clinical trials.17,27,28 The results reported here show rapid improvements in BCVA and CMT that exceed those reported previously. To the auhtor's knowledge, this is the first study in patients from the Middle East.
In the current study, mean BCVA improved rapidly and significantly within the first 6 months after FAc implantation. Remarkably, after just 6 months, mean BCVA had increased by more than 25 ETDRS letters from baseline, and over 90% of eyes had achieved an improvement of 15 letters or more. The speed of these improvements is consistent with those reported in the pivotal Phase III FAME studies, which also found rapid improvements in BCVA in the first 3 and 6 months after FAc implantation.10,27 The magnitude of the BCVA improvements seen in the current study is, however, much higher than those in FAME, possibly because this study reports data from 22 patients who were not randomized or prospectively enrolled. This is in contrast to the FAME study which was a Phase III randomized multicenter study with a large sample size. This study also included only pseudophakic patients, whose vision is not impaired by cataract formation, and patients with lower BCVA at baseline.
As with BCVA, mean CMT also improved rapidly and significantly in this study. Mean CMT decreased by almost 270 µm, and all patients had achieved reductions of at least 100 µm by 3 months. These rapid and significant improvements in CMT are greater than those observed in FAME and some real-world studies, including the UK multicenter Medisoft audit,20 but are in line with those reported in others; for example, the Portuguese RESPOND study reported mean reductions in central subfield thickness (CST) of more than 290 µm after 12 months of FAc therapy, with significant and rapid decreases in the first week.23 In the current study, a dry macula, with a CMT less than 300 µm, was achieved in over 85% of eyes by 6 months. This is consistent with the findings of the USER study, in which the percentage of patients achieving a dry macula significantly increased after FAc implantation.21 It should be noted, however, that the follow-up period in the USER study was longer than in the current study.
Data from clinical real-world studies have established the safety profile of the FAc intravitreal implant in patients with DME that persists or recurs despite treatment, and the current study revealed no new safety findings. Indeed, patients previously exposed to a course of corticosteroids appear to have fewer IOP elevations after FAc implantation than those who have not been exposed to prior course of corticosteroids,20,21 and the IOP increases that were observed in this study are in line with previously reported findings.
The limitations of this study include its retrospective design, which increases the potential for selection bias and confounding, and the small study sample, which limits the generalizability of the results and statistical power. Consequently, while the rapid and substantial improvements in BCVA and CMT observed in this study are quite marked, larger studies will be needed to confirm these findings. In addition, this study had a short follow-up period, so whether the improvements observed are sustained in the long term remains to be seen; however, larger studies have already shown that the FAc implant remains effective for up to 36 months in patients in clinical trials and real-world practices,27,28 and it would be interesting to confirm these results in this UAE population.
Conclusions
The FAc intravitreal implant is effective in UAE patients who have pseudophakic eyes and DME previously treated with a course of corticosteroids. In this patient population, the FAc implant rapidly and significantly improved BCVA and CMT, with no new safety signals. It may, therefore, be a useful treatment option for patients in the UAE, particularly those with sight threatening DME requiring rapid functional improvements.
Data Sharing Statement
The BCVA, CMT and IOP data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
Editorial support in the development of this manuscript was provided by Hayward Medical Communications and funded by Alimera Sciences in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Funding
The author received no financial support for the research, authorship, and/or publication of this article.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Musat O, Cernat C, Labib M, et al. Diabetic macular edema. Rom J Ophthalmol. 2015;59(3):133–136.
2. Browning DJ, Stewart MW, Lee C. Diabetic macular edema: evidence-based management. Indian J Ophthalmol. 2018;66(12):1736–1750. doi:10.4103/ijo.IJO_1240_18
3. Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond). 2015;2:17. doi:10.1186/s40662-015-0026-2
4. Cooper OAE, Taylor DJ, Crabb DP, Sim DA, McBain H. Psychological, social and everyday visual impact of diabetic macular oedema and diabetic retinopathy: a systematic review. Diabetic Medicine. 2019. doi:10.1111/dme.14125
5. Ferris FL
6. Gonder JR, Walker VM, Barbeau M, et al. Costs and quality of life in diabetic macular edema: Canadian burden of diabetic macular edema observational study (C-REALITY). J Ophthalmol. 2014;2014:939315.
7. Royal College of Ophthalmologists (RCO). Diabetic retinopathy guidelines. 2012. Available from: https://www.rcophth.ac.uk/wp-content/uploads/2014/12/2013-SCI-301-FINAL-DR-GUIDELINES-DEC-2012-updated-July-2013.pdf.
8. International Council of Ophthalmology (ICO). ICO guidelines for diabetic eye care. 2017. Available from: http://www.icoph.org/downloads/ICOGuidelinesforDiabeticEyeCare.pdf.
9. Schmidt-Erfurth U, Garcia-Arumi J, Bandello F, et al. Guidelines for the management of diabetic macular edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica. 2017;237(4):185–222. doi:10.1159/000458539
10. Campochiaro PA, Brown DM, Pearson A, et al. Long-term benefit of sustained-delivery fluocinolone acetonide vitreous inserts for diabetic macular edema. Ophthalmology. 2011;118(4):626–35 e2. doi:10.1016/j.ophtha.2010.12.028
11. Eichenbaum DA, Buznego C, Weng CY, Dhoot DS, Wykoff CC, Sheth VS. When and how to incorporate steroids for persistent diabetic macular edema: a discussion of real-world treatment optimization strategies. Ophthalmic Surg Lasers Imaging Retina. 2018;49(7):S5–S15. doi:10.3928/23258160-20180621-01
12. Gillies MC, Sutter FK, Simpson JM, Larsson J, Ali H, Zhu M. Intravitreal triamcinolone for refractory diabetic macular edema: two-year results of a double-masked, placebo-controlled, randomized clinical trial. Ophthalmology. 2006;113(9):1533–1538. doi:10.1016/j.ophtha.2006.02.065
13. Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002;109(5):920–927. doi:10.1016/S0161-6420(02)00975-2
14. Chawan-Saad J, Wu M, Wu A, Wu L. Corticosteroids for diabetic macular edema. Taiwan Journal of Ophthalmology. 2019;9(4):233–242. doi:10.4103/tjo.tjo_68_19
15. Zur D, Iglicki M, Loewenstein A. The role of steroids in the management of diabetic macular edema. Ophthalmic Research. 2019;62(4):231–236. doi:10.1159/000499540020.
16. Cunha-Vaz J, Ashton P, Iezzi R, et al. Sustained delivery fluocinolone acetonide vitreous implants: long-term benefit in patients with chronic diabetic macular edema. Ophthalmology. 2014;121(10):1892–1903. doi:10.1016/j.ophtha.2014.04.019
17. Pessoa B, Coelho J, Correia N, Ferreira N, Beirao M, Meireles A. Fluocinolone acetonide intravitreal implant 190 mug (ILUVIEN(R)) in vitrectomized versus nonvitrectomized eyes for the treatment of chronic diabetic macular edema. Ophthalmic Res. 2018;59(2):68–75. doi:10.1159/000484091
18. Rehak M, Busch C, Unterlauft JD, Jochmann C, Wiedemann P. Outcomes in diabetic macular edema switched directly or after a dexamethasone implant to a fluocinolone acetonide intravitreal implant following anti-VEGF treatment. Acta Diabetologica. 2019. [Online ahead of print]. doi:10.1007/s00592-019-01439-x
19. Alimera Sciences. Press release, 26 October 2016: alimera sciences begins selling ILUVIEN in the Middle East. 2016 Available from: https://investor.alimerasciences.com/news-releases/news-release-details/alimera-sciences-begins-selling-iluvienr-middle-east.
20. Bailey C, Chakravarthy U, Lotery A, Menon G, Talks J, Medisoft Audit G. Real-world experience with 0.2 mug/day fluocinolone acetonide intravitreal implant (ILUVIEN) in the United Kingdom. Eye (Lond). 2017;31(12):1707–1715. doi:10.1038/eye.2017.125
21. Eaton A, Koh SS, Jimenez J, Riemann CD. The USER study: a chart review of patients receiving a 0.2 microg/day fluocinolone acetonide implant for diabetic macular edema. Ophthalmol Ther. 2018;8:51–62.
22. Chakravarthy U, Taylor SR, Koch FHJ, Castro de Sousa JP, Bailey C. Changes in intraocular pressure after intravitreal fluocinolone acetonide (ILUVIEN): real-world experience in three European countries. Br J Ophthalmol. 2018. doi:10.1136/bjophthalmol-2018-312284
23. Figueira J, Henriques J, Amaro M, Rosas V, Alves D, Cunha-Vaz J. A nonrandomized, open-label, multicenter, phase 4 pilot study on the effect and safety of ILUVIEN(R) in chronic diabetic macular edema patients considered insufficiently responsive to available therapies (RESPOND). Ophthalmic Res. 2017;57(3):166–172. doi:10.1159/000455235
24. National Institutes of Health: ClinicalTrials.gov. Rapid structural and functional improvements in following 0.19 mg fluocinolone acetonide (FAc) implant in diabetic macular edema patients with poor visual acuity: 12-month audit results from United Arab Emirates [NCT03590587]. 2018. Available from: https://clinicaltrials.gov/ct2/show/NCT03590587.
25. World Medical Association. WMA Declaration of Helsinki – ethical principles for medical research involving human subjects. 2013 Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
26. International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH Harmonised Tripartite Guideline – guideline for Good Clinical Practice E6(R1). 1996 Available from: https://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R1_Guideline.pdf.
27. Campochiaro PA, Brown DM, Pearson A, et al. Sustained delivery fluocinolone acetonide vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology. 2012;119(10):2125–2132. doi:10.1016/j.ophtha.2012.04.030
28. Singh P, Chedid A, Deuchler SK, Kohnen T, Muller M, Koch FH. The efficacy and safety outcomes of the 0.19 mg fluocinolone acetonide implant after prior treatment with the 0.7 mg dexamethasone implant in patients with diabetic macular edema. Int Med Case Rep J. 2018;11:265–269. doi:10.2147/IMCRJ.S174461
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.