Back to Journals » Drug Design, Development and Therapy » Volume 12
Randomized trial of betahistine mesilate tablets as augmentation for oxcarbazepine and carbamazepine in treating vestibular paroxysmia
Authors Xue H, Xiang W, Yu Y, Liu G, Chong Y, Zhou J
Received 5 December 2017
Accepted for publication 14 February 2018
Published 12 April 2018 Volume 2018:12 Pages 837—843
DOI https://doi.org/10.2147/DDDT.S158888
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Georgios Panos
Hui Xue,1,2 Wenping Xiang,2 Yichuan Yu,3 Guorong Liu,2 Yi Chong,2 Jiying Zhou1
1Department of Neurology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China; 2Department of Neurology, Baotou Central Hospital, Inner Mongolia, Baotou, China; 3Department of Emergency, Yongchuan Hospital of Chongqing Medical University, Chongqing, China
Background: Vestibular paroxysmia (VP) is a rare episodic peripheral vestibular disorder. This study was conducted to compare the efficacy and acceptability of carbamazepine (CBZ) plus betahistine mesilate tablets (BMT) (CBZ+BMT) and oxcarbazepine (OXC) plus BMT (OXC+BMT) in treating VP, and investigated whether the synergistic effect could be increased along with the increased dose of BMT.
Methods: VP patients were recruited and randomly assigned to receive CBZ+BMT or OXC+BMT. The doses of CBZ and OXC were set to 200 and 300 mg/time, twice daily, respectively. The doses of BMT were set to 12 and 18 mg/time, twice daily. Half of the patients in each group received BMT 12 mg/time and the other half received BMT 18 mg/time. The treatment was continued for 12 weeks. The vertigo frequency, vertigo score, vertigo duration, response rate, and drug-related side effects were analyzed.
Results: In total, 92 patients in the CBZ+BMT group and 93 patients in the OXC+BMT group completed this trial. After 12 weeks of treatment, the two groups had similar average vertigo frequency, average vertigo score, average vertigo duration, and response rate. But the incidence of side effects was significantly higher in the CBZ+BMT group than in the OXC+BMT group (p=0.04). Subgroup analysis found that patients receiving BMT (18 mg) had greater reductions in average vertigo frequency, average vertigo duration, and average vertigo score, and higher response rates than patients receiving BMT (12 mg).
Conclusion: These results demonstrated that OXC+BMT may be suitable as an alternative method in VP patients with CBZ hypersensitivity, and the synergistic effect could be increased along with the increased dose of BMT.
Keywords: vestibular paroxysmia, betahistine mesilate tablets, carbamazepine, oxcarbazepine
Introduction
Vestibular paroxysmia (VP) is a rare episodic peripheral vestibular disorder, which can seriously affect the quality of life of patients. The main symptoms of VP include spontaneous, recurrent, short attacks of spinning, or non-spinning vertigo that usually continue for less than 1 min and happen more than 30 times/day.1 These symptoms are generally caused by direct pulsatile compression with ephaptic discharges. The pathogenesis of VP is still unclear, although many researchers believe that the demyelination of nerve fibers caused by vascular compression of the vestibulocochlear nerve is the main cause of VP.2,3 Partly because of the unclear pathogenesis, there are no objective laboratory-based diagnostic methods for VP. In clinical practice, the diagnosis of VP still relies on the symptom clusters and vestibular function assessment.
Currently, carbamazepine (CBZ) is viewed as the first line drug treatment for VP.4 The recommended dose of this drug is 200–600 mg/day.5 However, there is a strong association between CBZ-induced Stevens–Johnson syndrome (SJS) and human leukocyte antigen (HLA)-B*1502 in Han Chinese.6 Thus, clinicians have to check for HLA*B1502 before prescribing CBZ. In addition, the oral absorption of CBZ is relatively slow. To circumvent these limitations, another fast sodium channel blocker, oxcarbazepine (OXC), has been developed. A randomized controlled trial showed that OXC could reduce the days with vertigo for VP patients compared to placebo.7 The recommended dose of OXC is 300–900 mg/day.8 There is very limited evidence for the use of topiramate, baclofen, lamotrigin, or non-antiepileptic drugs, although these drugs have been tried in trigeminal neuralgia.9–11
A Chinese study reported that betahistine mesilate tablets (BMT) could significantly improve the efficacy of CBZ in treating VP.12 BMT is a microcirculation-improving agent, which could reduce the vertigo symptoms induced by vestibular or other inner ear dysfunctions. Our retrospective review found that the response rates in both the CBZ+BMT group and the OXC+BMT group were higher compared to the CBZ-alone group, which indicated that BMT could provide effective augmentation for CBZ and OXC in treating VP.13 In our previous study, we also found that CBZ+BMT and OXC+BMT had similar efficacy and acceptability.13 But this finding needs to be assessed in further research, for the following two reasons: 1) our previous study was not a randomized controlled trial; and 2) the doses of CBZ, OXC, and BMT are different in different patients. Therefore, this randomized controlled trial was conducted to evaluate whether CBZ+BMT and OXC+BMT had similar efficacy and acceptability in treating VP, and to investigate whether the synergistic effect could be increased along with the increased dose of BMT.
Methods
Patients recruited
This study was reviewed and approved by the Ethical Committee of the First Affiliated Hospital of Chongqing Medical University. Prior to treatment, written informed consent was obtained from all the included patients. Two experienced clinicians were in charge of recruiting VP patients according to the criteria described by Hüfner et al in 2008:14 1) vertigo lasts from a few seconds to a few minutes before treatment; 2) vertigo occurs at rest or with certain head positions; 3) vertigo has at least one of the following characteristics when occurring: no accompanying symptoms, postural instability, unstable gait, unilateral tinnitus, unilateral ear stuffiness or numbness, and unilateral hearing loss; 4) patients meet at least one of the following auxiliary diagnostic criteria: magnetic resonance imaging shows vascular compression of the nerve, a hyperventilation test induces nystagmus, electronystagmography shows worsening vestibular dysfunction, and patients respond to antiepileptic drug treatment; and 5) the above-mentioned symptoms cannot be explained by other diseases. The number of vertigo of VP patients was at least five in each month before treatment. Patients with positive HLA-B*1502 were excluded.
Intervention methods
The included VP patients were randomly assigned to receive CBZ+BMT or OXC+BMT. According to the average dose of CBZ and OXC used in our previous study,13 the doses of CBZ and OXC used in this study were set to 200 and 300 mg/time, twice daily, respectively. In order to study whether the different doses of BMT had the different effects in improving the efficacy of CBZ and OXC, the doses of BMT used in this study were set to 12 and 18 mg/time, twice daily. Half of the patients in each group received BMT 12 mg/time, and the other half received BMT 18 mg/time. The treatment was continued for 12 weeks, and would be terminated if serious side effects occurred. The patients, investigators, and data analysts were blinded to the intervention methods.
Outcome assessment
The vertigo frequency, vertigo score, and vertigo duration were assessed before and after treatment. The vertigo frequency referred to the number of episodes of vertigo occurring in 1 month, which was recorded by each patient or his or her family. The vertigo score was calculated using the scale in the previous study.15 The scale scores ranged from 0 to 10, where “0” represented “no pain” and “10” represented “the worst imaginable pain.” The respondents were asked to report their pain intensity in the past 24 h or current pain intensity using a number on the scale. The unit of vertigo duration was seconds (s). To make the interpretation of the results easier for clinicians,16 the response rate was also reported, which was calculated as the number of complete recoveries (CRs) and partial recoveries (PRs) divided by the total number of patients. The CR and PR were defined, respectively, as the total and partial disappearance of vertigo and its accompanying symptoms; if the vertigo and its accompanying symptoms showed no improvement after treatment, then this was defined as no relief (NR). Drug-related side effects were recorded during the whole treatment period to evaluate the acceptability of these two intervention methods.
Statistical analysis
All analyses were performed using SPSS version 19.0 (IBM Corp, Armonk, NY, USA). The chi-squared test and Student’s t-test were used to check whether the demographic data were similar between the two groups. Analysis of vertigo frequency, vertigo score, and vertigo duration was performed using analysis of covariance (ANCOVA). The ANCOVA evaluated the effect of treatment methods on the parameters’ values at the end of the trial, while statistically controlling for the effects of each parameter’s initial value.17 This statistical method can increase the statistical power by reducing the within-group error variance. The response rate was analyzed using the chi-squared test. A p-value less than 0.05 indicated a statistically significant difference between the two groups.
Results
Baseline data
According to the results of our retrospective review,13 we found that the statistical power was 0.8 when each group had 90 patients. Considering a withdrawal rate of about 10% of patients, the number of patients in each group was set to 100. In total, 200 VP patients were recruited from our hospital and several community hospitals. The first participant was randomized in May 2015 and the last clinic visit occurred in June 2017. Finally, 92 patients in the CBZ+BMT group and 93 patients in the OXC+BMT group completed this trial. The demographic data were similar between the two groups. Detailed information is presented in Table 1. The reasons for withdrawal included: 1) four patients had economic problems; 2) five patients could not tolerate the treatments; 3) three patients did not take their medications as prescribed; and 4) three patients could not be contacted.
  | Table 1 Baseline data of patients in the two groups |
Vertigo frequency
Before treatment, the average vertigo frequencies were similar between the two groups. After treatment, the average vertigo frequency was significantly decreased to 4.16±5.75 episodes/month in the CBZ+BMT group (p<0.00001) and 5.25±6.32 episodes/month in the OXC+BMT group (p<0.00001). The CBZ+BMT group had a greater reduction. But the result of the ANCOVA showed that compared to the OXC+BMT group, the CBZ+BMT group had a non-statistically significantly lower average vertigo frequency (p=0.21) (Figure 1). Subgroup analysis found that compared to the CBZ+BMT (12 mg) group, the CBZ+BMT (18 mg) group had a significantly lower average vertigo frequency (p=0.01); compared to the OXC+BMT (12 mg) group, the OXC+BMT (18 mg) group had a significantly lower average vertigo frequency (p=0.03) (Figure 1).
  | Figure 1 Vertigo frequency in the two groups before and after treatment. |
Vertigo duration
Before treatment, the average vertigo durations were similar between the two groups. After treatment, the average vertigo duration was significantly decreased to 22.27±35.06 s in the CBZ+BMT group (p<0.00001) and 29.91±43.66 s in the OXC+BMT group (p<0.00001). The CBZ+BMT group had a greater reduction. But the result of the ANCOVA showed that compared to the OXC+BMT group, the CBZ+BMT group had a non-statistically significantly lower average vertigo duration (p=0.19) (Figure 2). Subgroup analysis found that compared to the CBZ+BMT (12 mg) group, the CBZ+BMT (18 mg) group had a significantly lower average vertigo duration (p=0.03); compared to the OXC+BMT (12 mg) group, the OXC+BMT (18 mg) group had a significantly lower average vertigo duration (p=0.01) (Figure 2).
  | Figure 2 Vertigo duration in the two groups before and after treatment. |
Vertigo score
Before treatment, the average vertigo scores were similar between the two groups. After treatment, the average vertigo score was significantly decreased to 1.85±2.09 in the CBZ+BMT group (p<0.00001) and 2.05±2.00 in the OXC+BMT group. The CBZ+BMT group had a greater reduction. But the result of the ANCOVA showed that compared to the OXC+BMT group, the CBZ+BMT group had a non-statistically significantly lower average vertigo score (p=0.49) (Figure 3). Subgroup analysis found that compared to the CBZ+BMT (12 mg) group, the CBZ+BMT (18 mg) group had a significantly lower average vertigo score (p=0.03); compared to the OXC+BMT (12 mg) group, the OXC+BMT (18 mg) group had a significantly lower average vertigo score (p=0.02) (Figure 3).
  | Figure 3 Vertigo score in the two groups before and after treatment. |
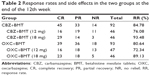
Response rate
After treatment, 45 patients, 33 patients, and 14 patients met the criteria of CR, PR, and NR, respectively, in the CBZ+BMT group; and 39 patients, 36 patients, and 18 patients met the criteria of CR, PR, and NR, respectively, in the OXC+BMT group (Table 2). The response rates were similar between the CBZ+BMT group and the OXC+BMT group (84.78% vs 80.64%, p=0.45). Subgroup analysis found that compared to the CBZ+BMT (12 mg) group, the CBZ+BMT (18 mg) group had a significantly higher response rate (p=0.02); compared to the OXC+BMT (12 mg) group, the OXC+BMT (18 mg) group had a significantly higher response rate (p=0.04) (Table 2).
Drug-related side effects
During the whole treatment period, the following drug-related side effects were recorded in the CBZ+BMT group: drowsiness (n=6), dry mouth (n=2), double vision (n=2), headache (n=4), dizziness (n=3), ataxia (n=4), nausea (n=4), vomiting (n=3), mild liver dysfunction (n=1), and mild renal dysfunction (n=1); the following drug-related side effects were recorded in the OXC+BMT group: drowsiness (n=2), dry mouth (n=2), double vision (n=3), fatigue (n=2), headaches (n=2), dizziness (n=3), nausea (n=2), and difficulty concentrating (n=2). The incidence of side effects was significantly higher in the CBZ+BMT group (32.61%) than in the OXC+BMT group (19.35%) (p=0.04). Subgroup analysis found that the incidence of side effects was similar between the CBZ+BMT (12 mg) group and the CBZ+BMT (18 mg) group; the incidence of side effects was also similar between the OXC+BMT (12 mg) group and the OXC+BMT (18 mg) group. The drug-related side effects were mild and needed no special treatment.
Discussion
This study recruited and assigned VP patients to receive CBZ+BMT or OXC+BMT. After treatment, the vertigo frequency, vertigo score, and vertigo duration were significantly decreased in both groups, which demonstrated that BMT could provide effective augmentation for CBZ and OXC in treating VP. Compared to the OXC+BMT group, the CBZ+BMT group had non-statistically significantly lower average vertigo frequency, lower average vertigo duration, and lower average vertigo score. The response rates were similar between the two groups. The incidence of drug-related side effects was significantly higher in the CBZ+BMT group than in the OXC+BMT group, although these side effects were mild and acceptable. These results indicate that the efficacy of CBZ+BMT was non-statistically significantly better than that of OXC+BMT, which is consistent with the findings of our previous retrospective review.13 Therefore, OXC+BMT may be a highly effective alternative method in treating VP.
Subgroup analysis found that compared to the CBZ+BMT (12 mg) group, the CBZ+BMT (18 mg) group had significantly lower average vertigo frequency, lower average vertigo duration, and lower average vertigo score; the response rate was significantly higher in the CBZ+BMT (18 mg) group than in the CBZ+BMT (12 mg) group. Similar results were also found between the OXC+BMT (12 mg) group and the OXC+BMT (18 mg) group. Moreover, the incidence of side effects was similar between the patients receiving BMT 18 mg and the patients receiving BMT 12 mg. These results indicate that the synergistic effect could be increased along with the increased dose of BMT, and the high BMT dose did not cause more side effects. Therefore, the high BMT dose (18 mg) is preferred over the low BMT dose (12 mg) when using it as augmentation for CBZ or OXC in treating VP. As this study is limited by the small number of samples in each subgroup, future studies are needed to further validate and support these findings.
Hüfner et al reported that both CBZ (average dose of 568 mg/day) and OXC (average dose of 870 mg/day) were effective in treating VP, with significant reductions in vertigo frequency to about 10% of baseline, in vertigo duration to about 10%, and in vertigo score to about 15%.14 Here, we used lower doses of CBZ (average dose of 400 mg/day) and OXC (average dose of 600 mg/day) to obtain similar results. This phenomenon could be explained by the following two reasons: 1) the different ethnicity and the lower body weight of our recruited patients and 2) BMT being used as augmentation for CBZ and OXC in our study. The addition of BMT could also reduce the incidence of drug-related side effects. A previous study reported that the incidences of side effects on the digestive system and urinary system among patients receiving CBZ alone were 15% and 3.3%, respectively.18 But in our study, these incidences were only 6.5% and 1.1% among patients receiving CBZ+BMT. In addition, the incidences of drug-related side effects in both the CBZ+BMT group and the OXC+BMT group were higher in the present study than in our previous study.13 This may be because our previous study was a retrospective study, which included some VP patients who had no or incomplete records about their drug-related side effects.
OXC is inactive on its own, but behaves as prodrug to licarbazepine in the liver to produce its therapeutic effect.19 It is a structural derivative of CBZ, but with fewer drug-related side effects. In general, OXC could be used to treat the same conditions as CBZ. Consistent with these conclusions, both this study and our previous study found that compared to the patients receiving CBZ, patients receiving OXC had fewer drug-related side effects and similar therapeutic effects.13 But one point should be noticed. Since the structure of OXC is similar to CBZ, and SJS caused by CBZ is significantly more common in patients with positive HLA-B*1502,6 there is also a consideration for genetic testing in Asian patients with VP prior to prescribing OXC, owing to the higher frequency of HLA-B*1502 in these patients.20
Limitations of this study should be mentioned here. First, all patients with VP were recruited from the same place, which may influence the applicability of our conclusions.21 Second, whether the combined application of OXC or CBZ and higher doses of BMT could produce better efficacy than CBZ+BMT (18 mg) or OXC+BMT (18 mg) should be investigated in future studies. Third, only short-term effects were evaluated, future studies are needed to assess the long-term effects of these two treatment methods. Fourth, current diagnostic criteria to diagnose VP were published in 2016.22 These criteria include: 1) more than 10 attacks of spontaneous spinning or non-spinning vertigo; 2) <60 s duration; 3) stereotyped phenomenology in a particular patient; 4) response to CBZ or OXC; and 5) could not be better accounted for by another disease. The inclusion of patients in this study was performed before the publication of these criteria. Therefore, whether our conclusion was appropriate for those VP patients according to the current diagnostic criteria was unknown. Fifth, whether BMT (18 mg) could significantly reduce the CBZ or OXC doses to minimize the incidence of the SJS was not investigated here, and needs further research and discussion.
Conclusion
This study found that the BMT could significantly improve the efficacy and acceptability of CBZ and OXC in treating VP, and the synergistic effect could be increased along with the increased dose of BMT. After treatment, the CBZ+BMT and OXC+BMT groups had similar average vertigo frequency, average vertigo duration, average vertigo score, and response rates. The incidence of drug-related side effects was significantly higher in the CBZ+BMT group than in the OXC+BMT group. Therefore, OXC+BMT may be suitable as an alternative method in VP patients with CBZ hypersensitivity.
Disclosure
The authors declare no conflicts of interest in this work.
References
Brandt T, Strupp M, Dieterich M. Vestibular paroxysmia: a treatable neurovascular cross-compression syndrome. J Neurol. 2016;263(Suppl 1):S90–S96. | ||
Leal PR, Roch JA, Hermier M, Souza MA, Cristino-Filho G, Sindou M. Structural abnormalities of the trigeminal root revealed by diffusion tensor imaging in patients with trigeminal neuralgia caused by neurovascular compression: a prospective, double-blind, controlled study. Pain. 2011;152(10):2357–2364. | ||
Jannetta PJ, Møller MB, Møller AR. Disabling positional vertigo. N Engl J Med. 1984;310:1700–1705. | ||
Brandt T, Dieterich M. Vestibular paroxysmia: vascular compression of the eighth nerve? Lancet. 1994;343(8900):798–799. | ||
Brandt T, Huppert T, Hüfner K, Zingler VC, Dieterich M, Strupp M. Long-term course and relapses of vestibular and balance disorders. Restor Neurol Neurosci. 2010;28(1):69–82. | ||
Locharernkul C, Loplumlert J, Limotai C, et al. Carbamazepine and phenytoin induced Stevens-Johnson syndrome is associated with HLA-B*1502 allele in Thai population. Epilepsia. 2008;49(12):2087–2091. | ||
Strupp M, Zwergal A, Feil K, Bremova T, Brandt T. Pharmacotherapy of vestibular and cerebellar disorders and downbeat nystagmus: translational and back-translational research. Ann N Y Acad Sci. 2015;1343:27–36. | ||
Brandt T, Zwergal A, Strupp M. Medical treatment of vestibular disorders. Expert Opin Pharmacother. 2009;10:1537–1548. | ||
Zakrzewska JM, McMillan R. Trigeminal neuralgia: the diagnosis and management of this excruciating and poorly understood facial pain. Postgrad Med J. 2011;87:410–416. | ||
Wang QP, Bai M. Topiramate versus carbamazepine for the treatment of classical trigeminal neuralgia: a meta-analysis. CNS Drugs. 2011;25:847–857. | ||
Yang M, Zhou M, He L, Chen N, Zakrzewska JM. Non-antiepileptic drugs for trigeminal neuralgia. Cochrane Database Syst Rev. 2011;(1):CD004029. | ||
Li JH. Efficacy of carbamazepine combined with mestilate in treatment of vestibular paroxysmia. Chinese Journal of Trauma and Disability Medicine. 2013;21(10):41–42. | ||
Yi C, Wenping X, Hui X, et al. Efficacy and acceptability of oxcarbazepine vs. carbamazepine with betahistine mesilate tablets in treating vestibular paroxysmia: a retrospective review. Postgrad Med. 2016;128(5):492–495. | ||
Hüfner K, Barresi D, Glaser M, et al. Vestibular paroxysmia: diagnostic features and medical treatment. Neurology. 2008;71(13):1006–1014. | ||
Chen Y, Zhao Z, Zhuang J, Yin Y, Ji Z, Li Y. The efficiency of carbamazepine in treatment of vestibular paroxysmia. Journal of Apoplexy and Nervous Diseases. 2011;28(3):242–243. | ||
Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS. Interpreting treatment effects in randomised trials. BMJ. 1998;316(7132):690–693. | ||
Kang R, He Y, Yan Y, et al. Comparison of paroxetine and agomelatine in depressed type 2 diabetes mellitus patients: a double-blind, randomized, clinical trial. Neuropsychiatr Dis Treat. 2015;11:1307–1311. | ||
Ming Z. [Common drug-related side-effects of carbamazepine in clinical practice]. Bei Fang Yao Xue. 2015;12(6):173. Chinese. | ||
Rogawski MA. Diverse mechanisms of antiepileptic drugs in the development pipeline. Epilepsy. 2006;69(3):273–294. | ||
He XJ, Jian LY, He XL, et al. Association between the HLA-B*15:02 allele and carbamazepine-induced Stevens-Johnson syndrome/toxic epidermal necrolysis in Han individuals of northeastern China. Pharmacol Rep. 2013;65(5):1256–1262. | ||
Chen JJ, Zhou CJ, Zheng P, et al. Differential urinary metabolites related with the severity of major depressive disorder. Behav Brain Res. 2017;332:280–287. | ||
Strupp M, Lopez-Escamez JA, Kim JS, et al. Vestibular paroxysmia: diagnostic criteria. J Vestib Res. 2016;26(5–6):409–415. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.