Back to Journals » Clinical Ophthalmology » Volume 17
Randomized Trial Comparing Prediction Accuracy of Two Swept Source Optical Coherence Tomography Biometers
Authors Multack S, Plummer N, Smits G, Hall B
Received 7 February 2023
Accepted for publication 3 August 2023
Published 17 August 2023 Volume 2023:17 Pages 2423—2428
DOI https://doi.org/10.2147/OPTH.S407538
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sam Multack,1 Nellie Plummer,1 Gerard Smits,2 Brad Hall3
1Multack Eye Care, Frankfort, IL, USA; 2CSC, Inc., Santa Barbara, CA, USA; 3Sengi, Penniac, NB, Canada
Correspondence: Sam Multack, Multack Eye Care, 22200 Wolf Road, Frankfort, IL, 60423, USA, Tel +1 815-889-3333, Email [email protected]
Purpose: To compare the prediction accuracy of the Argos biometer using standard keratometry to the prediction accuracy of the IOLMaster 700 biometer using Total Keratometry.
Methods: This was a randomized, prospective, single surgeon study of 80 right eyes of 80 patients that had preoperative biometry with both the Argos and IOLMaster 700 devices, followed by cataract surgery and intraocular lens (IOL) implantation. Prediction errors (directional and absolute) for each device were determined from the 1 month postoperative manifest refraction.
Results: The directional prediction error was 0.07 ± 0.32 D for the Argos and 0.08 ± 0.34 D for the IOLMaster 700. The mean of the difference in prediction error (directional) was 0.02 D, which was not statistically significant (p > 0.05). The absolute prediction error was 0.21 ± 0.25 D for the Argos and 0.25 ± 0.24 D for the IOLMaster 700. The mean of the difference in absolute prediction error was 0.04 D, which was statistically significant (p < 0.004) but not clinically significant. The percentage of eyes with absolute prediction error ≤ 0.5 D was 91% (73 eyes) for the Argos and 88% (70 eyes) for the IOLMaster 700. This difference was not statistically significant.
Conclusion: The prediction accuracies were similar between the Argos and IOLMaster 700 in eyes with normal axial length. There was a significant difference in mean absolute prediction error between devices; however, this was not clinically meaningful.
Keywords: Argos, IOLMaster 700, swept source optical coherence tomography, SS-OCT, cataract surgery, biometry
Plain Language Summary
Cataract surgery is a common procedure, which involves removing the opaque natural lens and replacing it with an artificial intraocular lens (IOL). To select a lens with the appropriate power, preoperative measurements are taken prior to surgery using a device called a biometer. There many different types of these devices available, and each biometer may use different optical technologies or different mathematical formulas to determine the most appropriate IOL power. The purpose of this study was to compare the prediction accuracy of a biometer than uses standard keratometry to the prediction accuracy of another biometer that uses Total Keratometry. The results of this study suggest that the prediction accuracies were similar between the devices.
Introduction
Achieving the refractive target in cataract surgery is important for good clinical outcomes for patients. Many preoperative formulas have been developed to aid in selecting the appropriate intraocular lens (IOL) power, but these formulas are dependent on accurate preoperative biometry measurements. Optical biometers were first available with partial coherence interferometry (PCI), which measured keratometry (K), axial length (AL), and anterior chamber depth (ACD).1 Other technologies include optical low coherence reflectometry (OLCR),2 optical low coherence interferometry (OLCI),3 and swept-source optical coherence tomography (SS-OCT).4,5 However, biometers utilizing SS-OCT have better optical penetration.6
The first available SS-OCT biometer was the IOLMaster 700 (Carl Zeiss Meditec AG). Using a refractive index of 1.3375 and a wavelength of 1050 nm, it can measure K, AL, ACD, lens thickness (LT), central corneal thickness (CCT), and white-to-white (WTW).7 For keratometry, the IOLMaster 700 uses 3 rings for 18 spots. The IOLMaster 700 is also able to assess Total Keratometry (TK), which is a direct measure of both the anterior and posterior corneal surfaces.8 Using TK may allow for better outcomes in eyes that would benefit from accurate corneal surface measurement (such as eyes with a history of corneal refractive surgery or eyes with significant astigmatism).9,10 Studies have reported that the use of the IOLMaster 700 generally leads to good clinical outcomes after cataract surgery.8,11–13
A relatively new SS-OCT biometer is the Argos (Movu, a Santec Company). It also measures K, AL, ACD, LT, CCT, and WTW, but uses a wavelength of 1060 nm and refractive indices of 1.376, 1.410, and 1.336 for the cornea, lens, and aqueous and vitreous, respectively.14 A sum of these segments is used to calculate axial length, and adjustments to axial length can be made from variability in the lengths of any of these segments.15,16 The retinal thickness is defined as 300 μm. The Argos uses standard keratometry (using a single ring of 16 spots), which does not directly measure the posterior corneal surface, however the Barrett toric calculator can use an estimated value for preoperative IOL calculations. Previous studies of the Argos have also reported good clinical outcomes.12,17
To date, there are minimal data comparing the refractive outcomes between the Argos and IOLMaster 700 biometers. The purpose of this study was to compare the prediction accuracy of the Argos device using standard keratometry to the prediction accuracy of the IOLMaster device using Total Keratometry in eyes with normal axial length.
Methods
This was a randomized, cross-over, prospective, single-surgeon study of the prediction accuracy of two SS-OCT biometers. The study was reviewed and approved by an Institutional Review Board (Salus IRB; Approval #64989743). Written informed consent was obtained from all subjects. The study followed the tenets of the Declaration of Helsinki, Good Clinical Practice, and International Harmonization (ICH) guidelines.
The inclusion criteria for this study were adults 50–85 years old, clinically significant cataracts, and planned implantation with the AcrySof IQ (SN60WF) IOL (Alcon Vision LLC). Subjects were excluded if they had central corneal thickness less than 490 mm and greater than 600 mm, history of contact lens use within 2 months of cataract surgery, severe dry eye, or corneal, retinal, or systemic disease. Subjects were also excluded if they had measured axial length less than 22.00 mm or greater than 26.00 mm, as the purpose of this study was to compare the prediction accuracies in eyes with normal axial length. Eyes with corneal astigmatism greater than 1.00 D were excluded to eliminate astigmatism as a confounding factor. Prior corneal refractive surgery creates challenges for IOL power calculation,18 thus subjects were excluded if they had prior corneal refractive surgery.
Two SS-OCT biometers were used to assess all subject eyes preoperatively, the Argos and the IOLMaster 700. Subjects were randomized as to the order of biometry measurements. Group 1 subjects first had measurements with the Argos device follow by the IOLMaster 700 device. Group 2 subjects first had measurements with the IOLMaster 700 device, followed by the Argos device. The right eyes of each subject were included for data analysis. For preoperative planning, the Barrett Universal Formula II “K” was used with the Argos device, and the Barrett Universal II TK formula was used with the IOLMaster 700 device. Plano was targeted for all eyes. If the suggested IOL power by each biometer was not the same, the IOL power suggested by the Argos device was selected. One experience surgeon performed all cataract surgeries (SM). Incisions (2.4 mm) were made temporally, followed by manual capsulorhexis. Refractive and visual outcomes were measured 28 to 42 days postoperatively. Subjective refractions were performed by the same optometrist who was blinded to the biometry data.
The primary endpoint for the study was mean absolute prediction error of each SS-OCT biometer. Absolute prediction error was calculated as the absolute difference between the predicted spherical equivalent refraction from preoperative planning and the measured spherical equivalent refraction (manifest). Secondary endpoints included median absolute prediction error, and the percentage of eyes with less than or equal to 0.25 D and 0.5 D absolute prediction error.
Statistical analyses were performed using SAS software (Version 9.4, SAS Institute, Inc). Normality was assessed using the Shapiro–Wilks test. Parametric variables were compared using a paired t-test, while non-parametric variables were compared using a Wilcoxon signed-rank test. A margin of 0.5 D was used for non-inferiority testing. Percentages of eyes within 0.5 D were compared using McNemar tests. Sample size calculations with SAS proc power revealed that 68 subjects would be required to establish non-inferiority with 90% power, assuming a within subject standard deviation of 0.25 D and an alpha of 0.05. This was increased to 80 subjects to account for any dropouts.
Results
A total of 80 right eyes of 80 subjects were enrolled in this study. Of the 80 eyes, 30 were from male subjects and 50 were from female subjects. The mean age of subjects was 72.2 ± 6.9 years (range 56 to 87).
Table 1 summarizes the prediction errors for each biometer. The Argos and IOLMaster 700 devices had similar prediction errors (directional) of 0.07 D and 0.08 D respectively. The mean of the difference was 0.02 D and was not statistically significant. The absolute prediction errors were 0.21 D and 0.25 D for the Argos and IOLMaster devices, respectively. A paired t-test was performed, and inferiority was rejected with a t statistic of 28.35 (p < 0.0001). After the non-inferiority test, a superiority test was performed, again using a paired t-test. The results showed that Argos had numerically smaller absolute error of 0.04 D than the IOLMaster 700, which was statistically significant (p=0.04), but not clinically significant. It should be noted that a non-parametric test confirmed that the difference was statistically significant (p = 0.0043).
 |
Table 1 Summary of Prediction Errors |
Refractive outcomes are summarized in Table 2. Overall, postoperative manifest refraction spherical equivalent was excellent, with 94% of eyes (75/80) within ± 0.5 D. Residual astigmatism was also good with 69% of eyes (55/80) having ≤ 0.5 D of residual astigmatism postoperatively. Figure 1 shows the distribution of absolute prediction error for the Argos and IOLMaster 700 biometers. Both biometers had similar percentages of eyes with absolute prediction errors ≤ 0.5 D, at 91% (73/80) for the Argos and 88% (70/80) for the IOLMaster 700. This difference was not statistically significant.
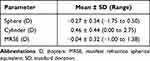 |
Table 2 Postoperative Refractive Outcomes |
 |
Figure 1 Absolute prediction error for spherical equivalent (n = 80 eyes). Abbreviation: D, diopters. |
Discussion
In general, cataract surgeons may be hitting the refractive target (± 0.5 D) in only 73% of cases.19 Good refractive outcomes will depend on accurate preoperative measurements. Advances in optical biometry may offer improved outcomes, however it is important for clinicians to know how optical biometers perform, especially compared to each other. Studies comparing PCI to SS-OCT biometers have reported comparable or improved preoperative measurements with SS-OCT biometers.12,13 In this study, we compared the predictive accuracy of the Argos and IOLMaster 700, with the Argos device using standard keratometry and the IOLMaster device using Total Keratometry.
We observed small differences in the prediction of spherical equivalent between the Argos and IOLMaster 700, which were not clinically relevant. Fabian and Wehner20 reported that the mean difference absolute prediction error between standard keratometry (Barrett Universal II formula) and Total Keratometry (Barrett Universal II TK formula) was 0.02 D (K – TK; compared to −0.04 D in our study). The mean difference reported by Fabian and Wehner also appears to be clinically irrelevant, however their study used only the IOLMaster 700 and included eyes with more astigmatism than our study. Choi et al21 observed minimal differences in mean absolute prediction error between the Argos and IOLMaster 700 (0.40 D and 0.36 D respectively) when implanting a trifocal IOL in patients with a history of corneal refractive surgery (using the Barrett True-K formula). A retrospective study by Yang et al5 also reported minimal differences in mean absolute prediction error between the Argos and IOLMaster 700 (0.35 D and 0.42 D respectively) with the Haigis formula. Tamaoki et al22 observed no significant differences in directional prediction error among short, medium, and long eyes between the Argos and IOLMaster 700 (using the Haigis formula), but did report significant differences within each of the three axial length groups. It would appear that, based on our results and those reported in other studies, that the prediction accuracies between the Argos and IOLMaster 700 are similar.
We also observed minimal differences in the percentage of eyes with an absolute prediction error ≤ 0.5 D between the Argos (91%) and IOLMaster 700 (88%). Fabian and Wehner20 reported that the percentage of eyes with an absolute prediction error ≤ 0.5 D between standard keratometry and Total Keratometry was 84% and 86%, respectively (using the Barrett Universal II and Barrett Universal II TK formulas). Omoto et al17 also observed minimal differences in the percentage of eyes with absolute prediction error ≤ 0.5 D between the Argos and IOLMaster 700 across short, medium, and long axial lengths. However, the percentages reported by Omoto et al17 were lower (70% or less with the Barrett Universal II formula) than those in our study. Tamaoki et al22 also investigated the differences in the percentage of eyes with absolute prediction error ≤ 0.5 D between the Argos and IOLMaster 700 across short, medium, and long axial lengths. They reported minimal differences between the Argos (80%) and IOLMaster 700 (83%) with the Haigis formula. In a retrospective study, Yang et al5 observed the same (73%) percentage of eyes with absolute prediction error ≤ 0.5 D between the Argos and IOLMaster 700 with the Haigis formula. Choi et al21 also observed the same (76%) percentage of eyes with absolute prediction error ≤ 0.5 D between the Argos and IOLMaster 700 using the Barrett True-K formula to implant a trifocal IOL. The results of our study and others indicate that the percentage of eyes with absolute prediction error ≤ 0.5 D are similar between the Argos and IOLMaster 700 devices.
Randomizing the biometer measurement order was intended to minimize dry eye or fatigue bias for each biometer reading. However, using the same eye to calculate the prediction error for each device is a limitation of this study, given that when the suggested powers differed between the devices, the Argos suggested power was preferred. This could introduce bias for better performance with the Argos. However, with the clinical insignificance of the differences observed in this study and others, our results appear robust. Another limitation of this study is that we are evaluating refractive outcomes only and there are not comparisons for K, AL, ACD, WTW, or LT measurements. However, other studies have reported comparisons of preoperative biometry.5,12,17,20–22
In conclusion, the prediction accuracies were similar between the Argos and IOLMaster 700 in eyes with normal axial length. There was a significant difference in mean absolute prediction error between devices, however this was not clinically relevant.
Funding
This study was supported with an investigator-initiated study grant (64989743) from Alcon Vision, LLC, Fort Worth, TX, USA.
Disclosure
Sam Multack reports consulting fees from Alcon Vision LLC, EyeCheck LLC, and EyeDX LLC. Gerard Smits reports consulting fees from Carl Zeiss Meditec. Brad Hall reports consulting fees from Ace Vision Group. The authors report no other conflicts of interest in this work.
References
1. Vogel A, Dick BH, Krummenauer F. Reproducibility of optical biometry using partial coherence interferometry: intraobserver and interobserver reliability. J Cataract Refract Surg. 2001;27:1961–1968. doi:10.1016/S0886-3350(01)01214-7
2. Hoffer KJ, Shammas HJ, Savini G. Comparison of 2 laser instruments for measuring axial length. J Cataract Refract Surg. 2010;36:644–648. doi:10.1016/j.jcrs.2009.11.007
3. Hoffer KJ, Shammas HJ, Savini G, Huang J. Multicenter study of optical low-coherence interferometry and partial-coherence interferometry optical biometers with patients from the United States and China. J Cataract Refract Surg. 2016;42:62–67. doi:10.1016/j.jcrs.2015.07.041
4. Montes-Mico R, Pastor-Pascual F, Ruiz-Mesa R, Tana-Rivero P. Ocular biometry with swept-source optical coherence tomography. J Cataract Refract Surg. 2021;47:802–814. doi:10.1097/j.jcrs.0000000000000551
5. Yang CM, Lim DH, Kim HJ, Chung TY. Comparison of two swept-source optical coherence tomography biometers and a partial coherence interferometer. PLoS One. 2019;14:e0223114. doi:10.1371/journal.pone.0223114
6. Lee HK, Kim MK. Comparison of a new swept-source optical biometer with a partial coherence interferometry. BMC Ophthalmol. 2018;18:269. doi:10.1186/s12886-018-0936-6
7. Srivannaboon S, Chirapapaisan C, Chonpimai P, Loket S. Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. J Cataract Refract Surg. 2015;41:2224–2232. doi:10.1016/j.jcrs.2015.03.019
8. Akman A, Asena L, Gungor SG. Evaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500. Br J Ophthalmol. 2016;100:1201–1205. doi:10.1136/bjophthalmol-2015-307779
9. Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38:2080–2087. doi:10.1016/j.jcrs.2012.08.036
10. Chen X, Yuan F, Wu L. Metaanalysis of intraocular lens power calculation after laser refractive surgery in myopic eyes. J Cataract Refract Surg. 2016;42:163–170. doi:10.1016/j.jcrs.2015.12.005
11. Rocha-de-Lossada C, Rodriguez-Vallejo M, Rachwani-Anil R, Burguera N, Fernandez J. Predicted refraction variability due to reliability of nine optical biometers for intraocular lens power calculation. J Refract Surg. 2022;38:120–127. doi:10.3928/1081597X-20211122-01
12. Montes-Mico R. Evaluation of 6 biometers based on different optical technologies. J Cataract Refract Surg. 2022;48:16–25. doi:10.1097/j.jcrs.0000000000000690
13. Higashiyama T, Mori H, Nakajima F, Ohji M. Comparison of a new biometer using swept-source optical coherence tomography and a conventional biometer using partial coherence interferometry. PLoS One. 2018;13:e0196401. doi:10.1371/journal.pone.0196401
14. Shammas HJ, Ortiz S, Shammas MC, Kim SH, Chong C. Biometry measurements using a new large-coherence-length swept-source optical coherence tomographer. J Cataract Refract Surg. 2016;42:50–61. doi:10.1016/j.jcrs.2015.07.042
15. Wang Q, Chen M, Ning R, et al. The precision of a new anterior segment optical coherence tomographer and its comparison with a swept-source OCT-based optical biometer in patients with cataract. J Refract Surg. 2021;37:616–622. doi:10.3928/1081597X-20210610-02
16. Shammas HJ, Taroni L, Pellegrini M, et al. Accuracy of newer intraocular lens power formulas in short and long eyes using sum-of-segments biometry. J Cataract Refract Surg. 2022;48:1113–1120. doi:10.1097/j.jcrs.0000000000000958
17. Omoto MK, Torii H, Masui S, Ayaki M, Tsubota K, Negishi K. Ocular biometry and refractive outcomes using two swept-source optical coherence tomography-based biometers with segmental or equivalent refractive indices. Sci Rep. 2019;9:6557. doi:10.1038/s41598-019-42968-3
18. Savini G, Hoffer KJ. Intraocular lens power calculation in eyes with previous corneal refractive surgery. Eye Vis. 2018;5:18. doi:10.1186/s40662-018-0110-5
19. Lundstrom M, Dickman M, Henry Y, et al. Risk factors for refractive error after cataract surgery: analysis of 282 811 cataract extractions reported to the European registry of quality outcomes for cataract and refractive surgery. J Cataract Refract Surg. 2018;44:447–452. doi:10.1016/j.jcrs.2018.01.031
20. Fabian E, Wehner W. Prediction accuracy of total keratometry compared to standard keratometry using different intraocular lens power formulas. J Refract Surg. 2019;35:362–368. doi:10.3928/1081597X-20190422-02
21. Choi JY, Choi A, Kwon H, Jeon S. Accuracy of IOL power calculation formulas for quadrifocal AcrySof IQ PanOptix TFNT implantation in patients with previous corneal refractive surgery: comparison of SS-OCT-based biometers. J Refract Surg. 2021;37:836–841. doi:10.3928/1081597X-20210812-02
22. Tamaoki A, Kojima T, Hasegawa A, et al. Clinical Evaluation of a New Swept-Source Optical Coherence Biometer That Uses Individual Refractive Indices to Measure Axial Length in Cataract Patients. Ophthalmic Res. 2019;62:11–23. doi:10.1159/000496690
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
