Back to Journals » Cancer Management and Research » Volume 13
Radiation Oncologists’ Approach to Internal Mammary Lymph Node Radiotherapy in Breast Cancer: The Turkish Society for Radiation Oncology Breast Cancer Study Group (TROD 06-005 Survey Study)
Received 5 July 2021
Accepted for publication 10 September 2021
Published 16 September 2021 Volume 2021:13 Pages 7203—7212
DOI https://doi.org/10.2147/CMAR.S327666
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Yong Teng
Ayfer Ay Eren,1 Mehmet Fuat Eren2
1Radiation Oncology Clinic, Kartal Dr. Lütfi Kırdar City Hospital, Istanbul, 34890, Turkey; 2Radiation Oncology Clinic, Marmara University Pendik Education and Research Hospital, Istanbul, 34899, Turkey
Correspondence: Mehmet Fuat Eren
Marmara University Pendik Education and Research Hospital, Radiation Oncology Clinic, Istanbul, 34899, Turkey
Tel +90 530 690 05 04
Email [email protected]
Background: This study aimed to examine the practice patterns of radiation oncologists in Turkey regarding radiotherapy to the regional lymph nodes, including internal mammary lymph nodes (IMNs), and identify the factors influencing their clinical decisions in breast cancer patients.
Methods: A nationwide, 19-point questionnaire was sent to the physician members of the Turkish Society for Radiation Oncology (TROD).
Results: In total, 165 radiation oncologists completed the survey, corresponding to a 27% response rate. Regional radiotherapy was used in 64.2% of the patients with 1– 3 axillary lymphatic involvement and unfavorable prognostic factors. In contrast, 61.2% of the respondents indicated that IMN should be included in the target volume for regional radiotherapy when the patient had one positive node after axillary lymph node dissection (ALND) in the inner quadrant and central region tumors. However, 71.5% of the respondents chose to include the IMN in the non-inner quadrant and non-central region tumors for patients with four or more positive nodes after ALND. The decision to offer internal mammary lymph node radiotherapy (IMNRT) varied widely and significantly among respondents, years in practice, and the rates of dedicating their clinical time to patients with breast cancer.
Conclusion: The results of this survey revealed significant national variation in attitudes regarding the treatment of IMN. Thus, this study may also help document the impact of future studies on clinical practice.
Keywords: survey, breast cancer, internal mammary lymph nodes, regional nodal irradiation, radiotherapy
Introduction
Since the recent publication of randomized controlled trials, regional nodal irradiation (RNI), including the supra-/infraclavicular and IMNs, has become the standard treatment in adjuvant radiotherapy (RT) node-positive breast cancer.1,2 RT aims to eradicate the microscopic residual disease in the lymphatic drainage system after breast cancer surgery. EORTC 22922/10925 (1) and MA.20 (2) have shown that RNI and breast RT increase local control, distant metastasis-free survival, and disease-free survival in patients with breast cancer. In contrast, the addition of IMNRT may be associated with increased pulmonary and cardiac toxicities.3–5 Therefore, before the publication of the European Organisation for Research and Treatment of Cancer (EORTC) 22922/10925 and MA.20, IMNRT is generally not recommended in clinical practice. In addition to the results of the two randomized studies, a Danish multicenter prospective cohort study also showed that including IMNRT in RNI significantly increased survival in medial and central breast tumors.6 Although current evidence suggests that IMNs are a significant pathway of lymphatic drainage, the management of IMN in breast cancer remains controversial.
Although worldwide variation in the use of IMNRT has been shown in previous studies,7–10 there are no specific data concerning actual Turkish practice. More importantly, the selection of nodal regions that should be included is unknown. Therefore, we conducted a survey among radiation oncologists in Turkey. The objectives were: (a) to report the tendencies in the practice of RNI and IMNRT in Turkey, (b) to identify the factors that influence the decision to offer radiotherapy to the IMNs, and (c) to support the need for new evidence-based guidelines and future studies.
Materials and Methods
A survey questionnaire regarding IMNRT in breast cancer was developed and confirmed after consultation with radiation oncologists experienced in breast cancer radiotherapy. The Institutional Ethics Committee approved the study protocol and survey of Kartal Dr. Lütfü Kırdar City Hospital (No. 2017/514/120/12, 26.12.2017). Study respondents had given a consent form to have their data published. The survey was conducted between November 2017 and January 2018. The questionnaire comprised 19 questions and four main sections: (1) general information of the participants; (2) indications; (3) treatment technique and the dose fractionated regimen; and (4) literature review. All questions were designed as multi-choice questions, allowing multiple answers and free responses to missing options. The questionnaire was sent to all TROD members via e-mail. In addition, the questionnaire was sent to the respondents through WhatsApp and SMS and sent over e-mail to increase the participation rate. Participation in the survey was achieved at the congresses and meetings held during the study. Statistical analyses were carried out using IBM SPSS Statistics software version 23. Frequency distributions (numbers and percentages) were calculated for the categorical variables. The chi-square test was used to examine the correlations between categorical variables. Statistical significance was set at P ≤ 0.05.
Results
General Information
Six hundred five radiation oncologists (ROs) registered in the TROD, and the survey reached 165 ROs, which resulted in a 27% response rate. The questions and answers are summarized in Table 1. Most respondents were 50 years old and younger (73.3%). In addition, % 27.2 of respondents (associate professors and professors were 13.9% and 13.3%, respectively) worked in an academic environment. The vast majority of respondents (66.7%) had experienced radiation oncology who had worked in the RT field for ≥ five years, and the remaining respondents (6.1%) were residents in radiation oncology. The rates of respondents working in university and training and research hospitals were similar, with 41.4% and 39.6%, respectively. Nineteen percent of the respondents were working in private hospitals. Finally, the respondents were divided based on the rates of dedicating their clinical time to patients with breast cancer. With 37 (22.4%) less than 5% of clinical time dedicated to breast cancer, 47 (28.5%) 5% to 25% of clinical time dedicated to breast cancer, 63 (38.2%) 25% to 75% of clinical time dedicated to breast cancer, and 18 (10.9%) more than 75% of clinical time dedicated to breast cancer. The respondents were also divided according to the number of years they had been practicing as radiation oncologists, with 44 (26.7%) practicing for more than 20 years, 65 (39.4%) practicing for 10–20 years, 40 (24.2%) practicing for 5–10 years, and 16 (9.7%) practicing for less than five years.
 |
Table 1 Survey Items and Results Obtained from Turkish Radiation Oncologists |
Indication for Lymph Node Irradiation
In patients with 1–3 axillary lymphatic involvement and the presence of unfavorable prognostic factors (aggressive biology, tumor diameter >3 cm, lymphovascular invasion, grade 3, young age (premenopausal), surgical margin adjacent), respondents were more likely to use regional radiotherapy when compared with four or more axillary lymphatic involvement (64.2% to 57%). In addition, 64.2% of the respondents also performed RNI in patients with ALND negative and IMN positive on PET-CT and CT. However, there was more variation in the inclusion of regional nodal irradiation. The proportion of respondents who included this region ranged from 15.8 to 64.2%, depending on the scenario (Table 2). As shown in Table 3, responses varied widely and significantly among respondents, years in practice, and the rates of dedicating their clinical time to patients with breast cancer. Most residents treated the RNI in all patients with 1–3 axillary lymphatic involvement, and professors infrequently treated the RNI (p=0.011). In contrast, RNI rates were significantly higher for professors than for residents with unfavorable prognostic factors in patients with 1–3 axillary lymphatic involvement and patients with four or more positive axillary involvement (p=0.023 and p=0.016, respectively). In addition, respondents with over 20 years of radiation oncology practice compared to those with 5–10 years of practice, there was a significantly higher rate in all patients with four or more axillary lymphatic involvement and patients with 50% or more positive lymph nodes removed after axillary dissection (p=0.006 and p=0.009, respectively).
 |
Table 2 Regional Nodal Irradiation Scenarios |
 |
Table 3 Responses Regarding RT to Regional Lymph Nodes in Breast Cancer Radiotherapy for Several Scenarios |
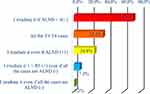
The questionnaire listed potential reasons for IMNRT, and the participants were asked about the situation in which they would perform IMNRT. The results are presented in Figure 1. The majority of respondents performed IMNRT in case of IMN positive on PET-CT and planning CT (81.8%). 71.5% of the respondents performed IMNRT in patients with four or more positive axillary involvement for tumors located in the non-inner quadrant and non-central (Figure 2), and 61.2% of the respondents performed IMNRT in case of one node-positive after ALND with tumors located in the inner quadrant and central (Figure 3). The indications for IMNRT recommended by the guidelines are any part of the axillary bed for greater than or equal to four positive nodes. However, 61.2% of respondents agreed that the internal mammary region should always be treated when one node-positive after ALND with tumors located in the inner quadrant and central region. In addition, 49% of the respondents stated that additional cardiac toxicity was the most critical reason for not performing IMNRT. The IMNRT rate of residents was significantly higher than that of specialists in the inner quadrant, central tumors, non-inner quadrant, and non-central tumors, even if there was one axillary lymph node involvement (p=0.015). In addition, the IMNRT rate of physicians who had a practice of 5 years and fewer for inner quadrant and central tumors, even if all the cases were axillary negative but with one or more negative prognostic factors, was significantly lower than that of the physicians who practiced ten years or more. However, the axillary lymph node involvement rate was significantly higher (p=0.038 and p=0.046, respectively).
 |
Figure 1 Responses regarding radiotherapy to the internal mammary node for several scenarios. In which situations do you irradiate the IMN? |
Details of Radiation Techniques for IMNRT
The most frequently used dose regimens for lymph node irradiation were 50 Gy in 25 fractions (65%) and 46 Gy in 23 fractions (33%). Regarding IMNRT, 52.1% of respondents treated their patients with 3D conformal radiotherapy using tangential fields. In contrast, only 5% of the respondents used hypofractionated regimens (42.5 Gy in 16 fractions). The proportion of respondents who applied photons, electrons, and combined photons and electrons was 34.5%, 5.5%, and 60%, respectively. Of the respondents, 41.2% used the breath-hold technique only for patients with left-sided breast cancer. After the MA20 and EORTC 22922 randomized trials, 55.2% of the respondents changed the IMNRT indications and reduced the clinical target volume (CTV)/planning target volume (PTV) margins for IMNRT.
Discussion
This study assessed the current Turkish radiation oncologists’ preferences and views regarding indications for IMNRT in patients with breast cancer. To our knowledge, this is the first nationwide survey of IMNRT endorsed by the TROD. The guideline recommendations for IMNRT cannot be applied in daily practice; the intervention and indications differ according to the axilla after positive sentinel lymph node dissection or ALND.
The MA.20 and EORTC 22922/10925 trials highlighted the current practice of RNI.1,2 Both the MA.20 trial and EORTC concluded that the addition of RNI to the IMN and the upper axillary nodes, including the supraclavicular region, reduced regional and distant breast cancer recurrence in patients with breast cancer. In MA.20, regional recurrences were reduced from 2.7% to 0.7%, and distant recurrences were reduced from 17.3% to 13.4% with the addition of nodal radiotherapy. According to the 10-year outcomes of the EORTC 22922/10925, RNI reduced the rate of regional and distant recurrences by 4.2 to 2.7% and 19.6 to 15.9%, respectively. However, the 15-year outcomes of EORTC were similar to the 10-year outcomes.11 In the subgroup analysis, breast cancer recurrence and mortality were reduced in the group with IMN and medial supraclavicular lymph nodes (MSN). The breast cancer recurrence rate was 23.4% in the IMN-MSN arm and 26.2% in the control arm.11 In the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) meta-analysis, 8135 patients from 22 trials concluded that the addition of RNI could reduce both regional and distant recurrences in patients with breast cancer.12 In contrast, in our survey, only 11 participants (6.7%) experienced IMN recurrence in IMNRT intervention during follow-up, while 44 participants (27%) experienced IMN recurrence in cases without IMNRT intervention.
Based on these results, the 2021 National Comprehensive Cancer Network (NCCN) guidelines strongly recommend irradiation of the IMN when delivering RNI for patients with four or more positive nodes (category 1) and patients with 1–3 positive node involvement (category 2A).13 RNI is not recommended in node-negative cases by the NCCN panel.13 Nevertheless, as shown in our survey, we observed significant variability in the practice patterns of IMNRT. About 61.2% of respondents reported treating IMN when only one lymph node was involved after ALND with tumors located in the inner quadrant and central, but 71.5% reported treatment if there were four or more positive nodes after ALND in patients with tumors located in the non-inner quadrant and non-central. This proportion increased to one-third in scenarios involving four or more lymph nodes. Thus, the tendency for an increasing number of respondents to report the use of RT to the IMN with increased pathologic lymph node involvement was present for the non-inner quadrant and non-central tumors.
Similarly, in a recent survey from Germany, Borm et al investigated the RNI differences among physicians and reported that participants performed RNI at a rate of 72% in the presence of 1–3 positive lymph nodes and risk factors, and 85% in the presence of three or more lymph nodes or supraclavicular lymph node involvement.7 In a Danish cohort study, additional IMNRT increased overall survival in patients with risk factors, including increased tumor size, an increasing number of involved axillary nodes, higher tumor grade, and medially located primary tumors.6 Only the French randomized trial, including 1334 patients, showed no survival benefit with the addition of IMNRT during post-mastectomy irradiation.4,5 From the NCCN guidelines, irradiation to the IMN is recommended category 1 in patients with greater than or equal to 4 positive lymph nodes. However, as shown in our survey, 61.2% of the participants treated IMN, even if one node (+) after ALND.
In a recently published survey conducted on ROs in German-speaking countries, radiotherapy techniques with cardiac protection were preferred in patients with breast cancer who underwent IMRT by 42.1%.14 In our survey, IMRT was preferred for cardiac protection by 47.9% in IMNRT, and half of the participants stated that they might have to compromise on IMNRT when they could not provide the cardiac doses they aimed at. However, IMNRT increases the cardiac dose during postoperative RT for left breast cancer.5 Many studies in which modern cardiac toxicity was not encountered independently of laterality in breast cancer irradiation with modern RT techniques.15,16 In the 10-year long-term outcomes of the MA.20, French, and Danish Breast Cancer Cooperative Group IMN studies, they strongly supported IMNRT. In the 15-year outcomes of EORTC, no remarkable cardiac risk increase was reported with IMNRT. In another study with a median follow-up of 9.3 years, the correlation between IMNRT and ischemic cardiac events could not be shown because of modern RT techniques.17 Modern RT techniques indicate that cardiac toxicity is not as prominent in IMNRT. Although the NCCN recommends including IMNRT in the area in most RNI irradiations, the standard rate of IMNRT of ROs in all patients who underwent elective RNI was 17% in our survey. Borm et al reported that IMNRT was not preferred because of its toxicity and unclear efficacy. Although guidelines recommend IMNRT more since the development of modern techniques (deep-inhalation breath-hold [DIBH], wide tangents, IMRT) allows for better protection of risk organs, in our study, the rate of applying “deep breath-hold” to each case of IMNRT intervention was 8.5%, and it was not preferred by half of the participants (50.3%). However, side effects are known to decrease with the reduction of cardiac and lung doses in IMNRT using the DIBH technique.18
We did not investigate the aspect in our survey regarding the treatment approach to regional nodal irradiation in patients who underwent neoadjuvant chemotherapy (NAC). Although this topic was not addressed in the survey, it was discussed regarding similar studies have been conducted. Patients with locally advanced breast cancer do not undergo primary surgery; instead, they are sent to the NAC and subsequent surgery. In this clinical scenario, the role, indication, and treatment radiation volumes can change dramatically. No randomized studies have evaluated the role of postoperative RT after NAC. The ongoing NSABP B-51/RTOG 1304 Phase III clinical study investigated the necessity of breast/chest wall radiotherapy and RNI after mastectomy and breast-conserving surgery in ypN0 after NAC T1-3N1.19 The study by Gregucci et al showed that the complete pathological response to NAC is a predictive prognostic factor, and it influences the indication to the chest wall, and the ipsilateral lymph node irradiation after NAC is the extension of the disease at diagnosis (cT3-T4 and/or cN2-N3).20 A recently published review also demonstrated that adjuvant radiotherapy including RNI after NAC should be based on pre-treatment investigations.21
The selection of radiotherapy techniques is essential to decrease the complications associated with IMNRT. The conformal technique is the preferred option. In our survey, while the conformal technique was used by 52.1% of participants, intensity-modulated radiation therapy (IMRT) was performed by 47.9%. Most of the participants delivered a total dose of 50 Gy with a 2-Gy dose/fraction. Only 4.8% of the participants used hypofractionated schemes because of the late toxicity data. However, in 2019, Wang et al recently published a randomized trial showing that conventional fractionation was not superior to hypofractionation in RNI, and the side effects were similar.22
There were some limitations to our study. First, we used a survey to present a cross-section of the IMNRT in Turkey. Unfortunately, none of the eligible ROs in Turkey answered the questionnaire. Although some practice surveys were conducted in other countries, the response rate was only 27.2%. This may have resulted in biased sampling. Second, some questions in the questionnaire concerning the details of techniques may have had a lower probability of response because of the low rate of participants (18%) with breast cancer experience. Therefore, future studies should address these limitations.
Conclusion
This is the first nationwide survey to summarize the current clinical practices of IMNRT in Turkey. The results showed a wide variation in IMNRT. Respondents, years in practice, and the rates of dedicating their clinical time to patients with breast cancer affected the decision to offer IMNRT. The current NCCN guideline recommendations for IMN have not been adequately implemented. This study and future surveys may also help document the impact of future studies on clinical practice.
Abbreviations
IMN, Internal mammary lymph node; TROD, Turkish Society for Radiation Oncology; ALND, Axillary lymph node dissection; IMNRT, Internal mammary lymph node radiotherapy; RNI, Regional nodal irradiation; RT, Radiotherapy; EORTC, European Organisation for Research and Treatment of Cancer; ROs, Radiation oncologists; CTV, Clinical target volume; PTV, Planning target volume; MSN, Medial supraclavicular lymph nodes; EBCTCG, Early Breast Cancer Trialists’ Collaborative Group; NCCN, National Comprehensive Cancer Network; DIBH, Deep-inhalation breath-hold.
Ethics Approval
The Institutional Ethics Committee approved the study protocol and survey of Kartal Dr. Lütfü Kırdar City Hospital (No. 2017/514/120/12, 26.12.2017).
Acknowledgments
The authors are grateful to all participants that replied to the questionnaire for their effort and time. The authors would like to thank Nuran Beşe and Zeynep Özsaran for their contributions to this survey. The authors would also like to thank Duygu Gedik, Halil Akbörü, Melis Gültekin, Cenk Umay, Eda Erdiş, Banu Atalar, Pelin Altınok, Gül Alço, Ayşe Altınok, Seda Eröz for assistance with the data collecting.
Author Contributions
Both authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The authors received no specific financial support for the research, authorship, and/or publication of this article.
Disclosure
Mehmet Fuat Eren and Ayfer Ay Eren declare that they have no conflicts of interest for this work.
References
1. Poortmans PM, Collette S, Kirkove C, et al.; EORTC Radiation Oncology and Breast Cancer Groups. Internal mammary and medial supraclavicular irradiation in breast cancer. N Engl J Med. 2015;373(4):317–327. PMID: 26200978. doi:10.1056/NEJMoa1415369
2. Whelan TJ, Olivotto IA, Parulekar WR, et al.; MA.20 Study Investigators. Regional nodal irradiation in early-stage breast cancer. N Engl J Med. 2015;373(4):307–316. doi:10.1056/NEJMoa1415340.
3. Shah C, Badiyan S, Berry S, et al. Cardiac dose sparing and avoidance techniques in breast cancer radiotherapy. Radiother Oncol. 2014;112(1):9–16. PMID: 24813095. doi:10.1016/j.radonc.2014.04.009
4. Meattini I, Guenzi M, Fozza A, et al. Overview on cardiac, pulmonary and cutaneous toxicity in patients treated with adjuvant radiotherapy for breast cancer. Breast Cancer. 2017;24(1):52–62. PMID: 27025498. doi:10.1007/s12282-016-0694-3.
5. Thorsen LB, Thomsen MS, Berg M; et al., Danish Breast Cancer Cooperative Group Radiotherapy committee. CT-planned internal mammary node radiotherapy in the DBCG-IMN study: benefit versus potentially harmful effects. Acta Oncol. 2014;53:1027–1034. doi:10.3109/0284186X.2014.925579
6. Thorsen LB, Offersen BV, Danø H, et al. DBCG-IMN: a population-based cohort study on the effect of internal mammary node irradiation in early node-positive breast cancer. J Clin Oncol. 2016;34(4):314–320. doi:10.1200/JCO.2015.63.6456
7. Borm KJ, Kessel K, Devecka M, et al. variability in lymph node irradiation in patients with breast cancer-results from a multi-center survey in German-speaking countries. Strahlenther Onkol. 2020;196(1):15–22. doi:10.1007/s00066-019-01537-3
8. Roumeliotis M, Long K, Phan T, Graham D, Quirk S. Including internal mammary lymph nodes in radiation therapy for synchronous bilateral breast cancer: an international survey of treatment technique and clinical priorities. Breast Cancer Res Treat. 2018;171(2):471–475. doi:10.1007/s10549-018-4848-1
9. Taghian A, Jagsi R, Makris A, et al. Results of a survey regarding irradiation of internal mammary chain in patients with breast cancer: practice is culture driven rather than evidence based. Int J Radiat Oncol Biol Phys. 2004;60(3):706–714. doi:10.1016/j.ijrobp.2004.04.027
10. Clavel S, Roy I, Carrier JF, Rousseau P, Fortin MA. Adjuvant regional irradiation after breast-conserving therapy for early stage breast cancer: a survey of canadian radiation oncologists. Clin Oncol (R Coll Radiol). 2010;22(1):39–45. doi:10.1016/j.clon.2009.09.026
11. Poortmans PM, Weltens C, Fortpied C, et al. Internal mammary and medial supraclavicular lymph node chain irradiation in stage I-III breast cancer (EORTC 22922/10925): 15-year results of a randomized, phase 3 trial [published correction appears in Lancet Oncol. 2021 Jan;22(1):e5]. Lancet Oncol. 2020;21(12):1602–1610. doi:10.1016/S1470-2045(20)30472-1
12. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomized trials. Lancet. 2011;378:1707–16. 34. doi:10.1016/S0140-6736(11)61629-2
13. Gradishar WJ, Moran MS, Abraham J, et al. NCCN guidelines® insights: breast cancer, version 4.2021. J Natl Compr Canc Netw. 2021;19(5):484–493. doi:10.6004/jnccn.2021.0023
14. Duma MN, Münch S, Oechsner M, et al. Heart-sparing radiotherapy in patients with breast cancer: what are the techniques used in the clinical routine? A pattern of practice survey in the German-speaking countries. Med Dosim. 2017;42(3):197–202. doi:10.1016/j.meddos.2017.03.002
15. Rutter CE, Chagpar AB, Evans SB. Breast cancer laterality does not influence survival in a large modern cohort: implications for radiation-related cardiac mortality. Int J Radiat Oncol Biol Phys. 2014;90(2):329–334. doi:10.1016/j.ijrobp.2014.06.030
16. Boero IJ, Paravati AJ, Triplett DP, et al. Modern radiation therapy and cardiac outcomes in breast cancer. Int J Radiat Oncol Biol Phys. 2016;94(4):700–708. doi:10.1016/j.ijrobp.2015.12.018
17. Dess RT, Liss AL, Griffith KA, et al. Ischemic cardiac events following treatment of the internal mammary nodal region using contemporary radiation planning techniques. Int J Radiat Oncol Biol Phys. 2017;99(5):1146–1153. doi:10.1016/j.ijrobp.2017.06.2459
18. Ranger A, Dunlop A, Hutchinson K, et al. A dosimetric comparison of breast radiotherapy techniques to treat locoregional lymph nodes including the internal mammary chain. Clin Oncol (R Coll Radiol). 2018;30(6):346–353. doi:10.1016/j.clon.2018.01.017
19. Mamounas EP, White JR, Bandos H, et al. NSABP B-51/ RTOG 1304: randomized phase III clinical trial evaluating the role of postmastectomy chest wall and regional nodal XRT (CWRNRT) and post-lumpectomy RNRT in patients with documented positive axillary (Ax) nodes before neoadjuvant chemotherapy (NC) who convert to pathologically negative Ax nodes after NC. JCO. 2014;32(15 supp):tps1141.
20. Gregucci F, Fozza A, Falivene S, et al.; Italian Society of Radiotherapy and Clinical Oncology (AIRO) Breast Group. Present clinical practice of breast cancer radiotherapy in Italy: a nationwide survey by the Italian Society of Radiotherapy and Clinical Oncology (AIRO) Breast Group. Radiol Med. 2020;125(7):674–682. doi:10.1007/s11547-020-01147-5
21. Fozza A, Giaj-Levra N, De Rose F, et al. Lymph nodal radiotherapy in breast cancer: what are the unresolved issues? Expert Rev Anticancer Ther. 2021;21(8):827–840. doi:10.1080/14737140.2021.1917390
22. Wang SL, Fang H, Song YW, et al. Hypofractionated versus conventional fractionated postmastectomy radiotherapy for patients with high-risk breast cancer: a randomised, non-inferiority, open-label, phase 3 trial. Lancet Oncol. 2019;20(3):352–360. doi:10.1016/S1470-2045(18)30813-1
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.