Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
Quantified Facial Rejuvenation Utilizing High Intense Focus Ultrasound with Multiple Penetrative Depths
Authors Lio ML, Chang CC, Chuang ADC, Tsai LC , Chen CC
Received 30 November 2021
Accepted for publication 10 February 2022
Published 19 March 2022 Volume 2022:15 Pages 489—496
DOI https://doi.org/10.2147/CCID.S350556
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Man-Lok Lio,1 Chang-Cheng Chang,2-5 Andy Deng-Chi Chuang,6 Li-Cheng Tsai,7 Chien-Chou Chen8
1Department of General Surgery, China Medical University Hospital, Taichung City, Taiwan; 2Division of Plastic and Reconstructive Surgery, Department of Surgery, China Medical University Hospital, Taichung, Taiwan; 3Department of Cosmeceutics and Graduate Institute of Cosmeceutics, China Medical University, Taichung, Taiwan; 4School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan; 5Institute of Imaging and Biomedical Photonics, National Yang Ming Chiao Tung University, Tainan, Taiwan; 6Department of Plastic and Reconstructive Surgery, Chang Gung Memorial Hospital at Keelung, Keelung, Taiwan; 7Department of Dermatology, China Medical College Hospital, Taichung, Taiwan; 8Department of Dermatology, Joe Chen Beauty Skin Clinic, Taichung City, Taiwan
Correspondence: Chang-Cheng Chang, China Medical University Hospital, No. 2, Yude Rd, North District, Taichung City 404, Taiwan, Email [email protected]
Background: Multiple penetration depths of high-intensity focused ultrasound (HIFU) treatment for facial rejuvenation have not been quantified.
Methods: We enrolled 12 participants (n=24) to undergo one session of HIFU rejuvenation between January 1, 2019, and January 10, 2020. We used a 2-, 4.5-, and 6-mm focal depth transducer on the upper and middle face. We evaluated efficacy on days 60 and 90 by using our specific assessment system.
Results: The average eyebrow peak and pupil–eyebrow peak angles significantly increased by 2° (p < 0.0005) and decreased by 1° (p < 0.0001), respectively, at day 90. The shortened eyebrow–iris length indicated that the forehead tissues had lifted and moved medially to the central face. Supraorbital tissues were also vertically elevated, marked by the eyebrow–orbital (p = 0.0016) and vertical palpebral fissure lengths (p = 0.0052), which both exhibited a 0.8-cm elevation. For the midface, the increased canthus–oral–nasal angle (p = 0.5881) and decreased tragus–oral length (p = 0.5881) indicated that laxity had been corrected through lifted oral commissure, though the data were not statistically significant. No serious side effects were observed.
Conclusion: HIFU treatment with multiple depths quantitatively improved both upper-facial rejuvenation and midface rejuvenation after a single session.
Keywords: HIFU, high-intensity focused ultrasound, facial aging, facial periorbital rejuvenation, midface rejuvenation
Introduction
Facial aging results in changes to the various anatomic layers of the skin, subcutaneous adipose tissue, muscles, retaining ligaments, and skeleton.1 Facial rejuvenation tightens the affected facial connective tissues through collagen regeneration and recontouring. Surgical lifting and ablative resurfacing effectively treat moderate to severe laxity.3 However, because of the relatively prevalent side effects and prolonged recovery time, nonablative skin rejuvenation has become a popular choice.4 Modalities including laser-based treatment (eg NdYac or Alexandrite picosecond laser, and intense pulsed light) radiofrequency, and high-intensity focused ultrasound (HIFU) are used for skin rejuvenation through controlled thermal injury within the dermal region to trigger collagen remodeling; of these methods, HIFU is the only one that reaches the deep dermal and fibromuscular layer.2,3
HIFU eyebrow-lifting technology was approved by the Food and Drug Administration in 2009.5 The acoustic energy generates heat ranging from 60° to 70 °C, targeting the deep dermis and superficial musculoaponeurotic system (SMAS), the so-called coagulation zone, which leads to collagen denature, new collagen synthesis, skin tightening, and elevation.5,6 Anatomically, the thicknesses of facial skin layers vary slightly; thus, the depths of the targeted treatment layers must be adjusted accordingly. After adjustment of the deposited short pulse within 50 to 200 ms, the megahertz frequency, and the low energy within 0.5 to 1.5 J, HIFU can precisely target these programmed dermal depths with controlled source power for effective facial rejuvenation.6,8
Although many studies have evaluated the efficacy and safety of HIFU for use on the face, neck and other body regions,2,6,7,9 the applied exposure parameters (source power, exposure area, and focal depth) have not been well described. Because programmed depth transducers are evolving, with new models being introduced on the market,4 we assessed the efficacy of multiple depth transducers applied regionally to the upper and midface.
Our study introduced a single session of treatment for facial rejuvenation with multiple penetration depths (2, 4.5, and 6 mm) on the forehead, anterior and posterior temporal lobes, and zygomatic arches according to the depth of targeted tissue. We applied the treatment with UlTRAFORMER III (Classys, Seoul, Korea) novel transducers and evaluated its effectiveness by using our specific quantitative assessments based on anatomical landmarks.22
Materials and Methods
Ethical Statement
The study was approved by the institutional review board of China Medical University Hospital in Taichung (Reference No CMUH109-REC1-137). All participants provided written informed consent for the trial, including consent for publication, and all procedures were conducted in accordance with the Declaration of Helsinki.
Study Sample
Twelve participants between the ages of 20 and 60 years (2 men and 10 women; median age: 49.75 years) with Fitzpatrick skin type III–V were enrolled in our retrospective clinical review. All participants provided written informed consent for the trial. They received the HIFU treatment for facial rejuvenation between January 1, 2019, and January 10, 2020, and had not undergone any other aesthetic treatment. Individuals were excluded if they had undergone plastic surgery (eg, facelift, tissue augmentation, or blepharoplasty) before or between the aforementioned dates; treatments with fillers, or laser resurfacing; had scars, an infection, or a bleeding diathesis; or did not consent to the publication of their images.
Procedures and Devices
During preparation, topical anesthetic (Sincaine cream 5%, with Lidocaine 25 mg, Prilocaine 25 mg per gm) was applied to the participants’ forehead, temporal, and cheek regions for 20 minutes. One session of HIFU treatment was conducted, during which the ULTRAFORMER III targeted the forehead, temporal lobes, and zygomatic arches (see Supplementary Figure S1, figures, which outline the HIFU treatment lines, exposure parameters, and the expected consequential lifting effects) using the following three transducers:
- MF2; 5.5 MHz, 2-mm focal depth, applied at 0.3–0.4 J per line to the forehead.
- L4-4.5; 4 MHz, 4.5-mm focal depth, applied at 0.7 J per line to the anterior temporal lobes and zygomatic arches.
- W2-6.0; 2 MHz, 6-mm focal depth, applied at 1.0–1.2 J per line to the posterior temporal lobes.
Each treatment line was 25 mm, the standard interval between each thermal coagulation zone was 1.5 mm, and every treatment line contained 17 thermal coagulation zones. The entire procedure was conducted by the same physician, and transducers were applied perpendicularly, uniformly, and firmly to the skin surface. Treatment lines were adjacent and parallel to one another and approximately 3–5 mm apart. During treatment, 20, 10, 30, and 60 lines were applied to the zygomatic arches, anterior and posterior temporal lobes, and half of the forehead, respectively. The procedure was then repeated on the collateral side. In total, each participant received 240 exposure lines. One treatment session lasted 15–20 min. The total energy applied to the face was 138–162 J.
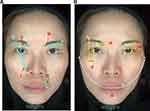
Standardized advanced imaging photographs (OBSERV A+, Myguard, Taoyuan, Taiwan) of the frontal (0°) were obtained pretreatment and on day 60 and 90 posttreatment. Participants were fixed in position under a standard OBSERV A+ lightening system. We assessed the efficacy of the treatment by comparing the designated angles and lengths before and after treatment (Figure 1).22
Efficacy Measurement: Objective Outcomes
Thirteen landmarks (see Supplementary Table S1, table, which explains the exact anatomies), four angular and five linear, were designed (Figure 1A and B). When eyebrow lifting is significantly improved, the eyebrow peak (E-peak) and eyebrow tail (E-tail) angles are increased. Elevated eyebrow peaks tend to move medially to the central side, resulting in a smaller pupil–eyebrow peak (P-E peak) angle (Table 1).
 |
Table 1 Movement of the Linear and Angular Assessments When Rejuvenation Present After Treatment |
Three vertical lines and one horizontal line present the restoration of eyelid ptosis. When the superior orbital rim (Os) is set as an immobile landmark, the elevation of supraorbital tissues causes the eyebrow to lift, as indicated by a greater eyebrow–orbital (E-O) length. When the skin is tightened at the upper and lower eyelid, the length of the vertical palpebral fissure (VPF) increases. The flattening and tightening of the upper eyelid skin causes the orbital–upper eyelid length to decrease. According to the Westmore model, the ideal brow position is above the lateral limbus,10 and when the eyebrow is lifted, the horizontal eyebrow–iris (E-I) length decreases (Table 1).
In terms of the midface, the distance between the bilateral tragi (Tr) passing through the oral commissure (Oc), so called the tragus–oral (T-O) length, should decrease if the sagging lower face is restored by rejuvenative procedures. These measurements were collected in the same manner collaterally.
Statistical Analyses
GraphPad Prism 6 software26 was used for statistical analyses. Statistical comparisons before and after the treatment were performed using paired t-tests. Data were presented as the mean ± standard deviation, and p values < 0.05 were considered statistically significant.
Results
The mean values of the eyebrow-peak and E-tail angles were increased at days 60 and 90 (Table 2) (see Supplementary Figure S2, figures, which present the results of the angular assessment in a boxplot). The E-peak angle increased from 25.958° ± 4.554° on day 0 to 28.208° ± 3.9232° at the day 90 follow-up, constituting a statistically significant improvement of 2° (p = 0.0003), approximately. The mean of the E-tail angle on day 90 was 4.250° ± 4.306°, which also constitutes an increase of approximately 1° compared with baseline, though the result was not statistically significant (p = 0.2011). The P-E peak angle was 4.000° ± 2.414° at baseline. The lifted and contracted supraorbital and forehead tissues caused the eyebrow peak to move medially to the central side, resulting in a significant, approximate 1° decrease in P-E peak angle on day 90 follow-up (2.833° ± 2.057°, p < 0.0001). Regarding the periorbital region, the means of both the E-O and VPF lengths were significantly higher at days 60 and 90, with an approximate 0.8 mm improvement (p = 0.0016; p = 0.0052, respectively) (Table 3) (see Supplementary Figure S3, figures, which present the results of the linear assessment in a boxplot).
 |
Table 2 Means of the Assessment Results for 12 Patients Along with the Angles, Standard Deviations, and p values < 0.05 Were Considered Statistically Significant |
 |
Table 3 Means of the Assessment Results for 12 Patients Along with the Lines, Standard Deviations, and p values < 0.05 Were Considered Statistically Significant |
The mean of the orbital–upper eyelid length decreased from 7.204 ± 2.208 mm to 6.588 ± 1.909 mm at day 90 (p = 0.0352). All data were statistically significant. According to horizontal linear measurements, the E-I length was shorter at day 90 (6.633 ± 2.463 mm) than at baseline (6.813± 2.663 mm), though the difference was not statistically significant (p = 0.5440).
For the midface, the average canthus–oral–nasal (C-O-N) angle was 29.625° ± 5.037° at baseline and exhibited a 0.3° increase to 29.958° ± 4.573° at day 90. The average tragus–oral (T-O) length decreased from 169.893 ± 26.617 mm at baseline to 168.852 ± 25.354 mm at day 90, representing a decrease of approximately 1 mm (Table 3). The data indicate that laxity of the midface was corrected and oral commissure was lifted, though not to a statistically significant level (p = 0.5881, p = 0.4943).
Side Effects
Pain and mild erythema in the treatment area were noted for 6 patients during treatment. These effects were soon resolved after treatment and did not last longer than 2 days. No serious side effects were reported during the study.
Discussion
HIFU treatment for facial rejuvenation is in high demand because it is minimally invasive, does not cause any epidermal damage, and can reach targeted skin layers at various depths with penetrating probes. Our current understanding of aging suggests that facial aging is not simply a result of the atrophy of subcutaneous fat but rather fatty hypertrophy, especially in the infraorbital, lateral temporal cheek, and submental region.18,21 In 2007, Gliklich et al and White et al studied the propagation of HIFU energy in cadaveric tissues to demonstrate that the formation of thermal injury zones, mainly in the SMAS layer, leads to thermal collagen denaturation and subsequent synthesis.12,17 Other in vivo studies have reported that collagen and elastic fibers develop after HIFU treatment primarily in the reticular and deep dermis.8,11,16,17 At a deeper tissue matrix, HIFU transducers thermally modify collagen and ablate adipocytes, thereby causing shrinkage and collagen remodeling within the tissue matrix and eventually reenforcing the attenuated ligaments and muscles. The depths of facial retaining ligaments and subdermal fascia vary because the thickness of anatomical components, such as superficial fat compartments and dermal tissue, tend to increase with age.16,17,20,21 Hence, the application of more than one transducer in HIFU treatment was vital in our study. To our knowledge, a 1.5-mm transducer is commonly used for superficial dermis, a 3-mm transducer is used for deeper dermis, and a 4.5-mm transducer targets the SMAS layers.4 Transducers sized 6 mm and above are often used in body recontouring for areas such as the abdomen and thighs.8,9
In our study, we applied a novel 2-mm transducer as a superficial transducer on the forehead (generated energy was 36–48 J). After one session of treatment, significant eyebrow lifting was observed at day 90 of follow-up. Additionally, the forehead tissue had contracted and moved supraorbital tissue medially to the central face. The lifting of the periorbital tissues was evidenced by an increase in mean E-O and VPF lengths, which indicated that the supraorbital ligamentous attachments had also thermally contracted and lifted (Figures 2A and B).
Our study is the first to report the use of a 6-mm deep transducer in facial rejuvenation, especially on the hair-bearing region of the temporal area, which is typically used on other body regions.12,14 Kwon et al proved a 6-mm transducer has benefits for tightening and rejuvenation of the area with unwanted fat.23 Because both the skin and fat of the lateral temporal and cheek regions are relatively thick, 4.5- and 6-mm transducers were employed to target the SMAS or deeper layers. We applied the MF6 (6 mm, 2 MHz, 1.0–1.2 J) to the posterior temporal lobes (generated energy was 60–72 J), extended the treatment site further to the hair-bearing region and scalp, in order to target the temporal fat pad in between the superficial and deep layers of the deep temporal fascia, which create a resonance between these two temporal fascia layers. For the concern of hair root injury, Jimenez et al24 studied the morphometric analysis of scalp hair and stated the mean length of human scalp hair follicle is 4.16mm, the data of Vogt et al25 reviewed the mean length of hair follicle is 3.86 mm; our applied 6-mm transducer targeted even deeper layers of the scalp, and no reports of epilation was noted in the post-treatment visits.
The increased E-tail angle and decreased E-I length indicated that the entire fascia of the temporal compartment contracted and subsequently lifted. Rejuvenation was also extended to the midface, as evidenced by the increase in the C-O-N angle and decrease in T-O length; therefore, laxity of the midface was restored and the oral commissure was lifted.
Some authors compared the aesthetic improvements of HIFU at two focal depths with improvements at a single focal depth. Baumann et al concluded that treatment with two focal depths is superior that with a single focal depth on the neck and lower face.13 However, research demonstrating the efficacy of multiple transducers on more than two regional uses is limited. The application of HIFU transducers to the upper to midface is also limited to only one or two focal depths.14 Suh et al11 reported clinical and histologic improvements in a study on 22 Korean participants after treatment with a single HIFU transducer on the forehead (3 mm, 0.3–0.35 J), temples (3 mm, 0.35 J), and malar areas. Park et al5 recorded a significant tightening of infraorbital laxity in seven patients treated with 1.5-mm (0.2 J) and 3-mm (0.45 J) focal depth transducers (with a total of 30 treatment lines). Recently, Kwon et al23 studied the efficacy of multiple transducers (3, 4.5 and 6.5 mm) applied on submental for reduction of unwanted submental fat. Our study design integrated the application of more transducers (2, 4.5 and 6 mm) on a single session of treatment. We validated the effectiveness quantitatively by using multiple penetration depths and transducers with deep focal depths for upper-facial and midfacial rejuvenation.
Thus far, no consensus has been reached on the ideal objective measurements for aesthetics. Traditional assessment tools, such as the Global Aesthetic Improvement Scale (GAIS) and wrinkle severity rating scale (WSRS), completed by both patients and physicians before and after treatment, are commonly used to assess HIFU treatment,14 but these 5-point scales cannot accurately represent treatment efficacy.14,15 Alam et al19 also evaluated the outcomes of HIFU treatment in eyebrow lifting by using fixed landmarks but measuring only linear changes and not employing anatomical landmarks on the lower face. In order to determine the cosmetic effects and quantity of skin lifting, our study employed a standard measurement of 13 facial landmarks, measuring the changes to four angles and five lines, according to which the efficacy of facial lifting was determined objectively.
This study has some limitations. First, we did not have a control group and it was almost impossible to hold a prospective, randomized clinical trial based on the personal heterogeneities, such as the degree of aging among people. Second, we did not compare the efficacy with a single transducer and the sample size was small and only analyzed the skin type of Asian, it is hard to determine which age group gave the best results. Third, the effects of repeated sessions were undetermined. Long-term adverse effects that may have occurred after the 90 days follow-up period were still not observed.
Conclusion
We assessed and quantified the efficacy of using multiple penetration depth transducers in HIFU treatment for facial rejuvenation. In our study, the results were favorable after one treatment session, and the side effects were transient and minimal. We confirmed that facial rejuvenation at the upper face and midface can be achieved through the use of transducers with multiple penetration depths (2, 4.5, and 6 mm). The variety of penetrative depths and sessions can potentially achieve even more effective results.
Acknowledgments
The authors wish to acknowledge the help of Li, Chia-wei in clinical investigation and Chen, Shih-ting for helping in the data collection for this study. We also acknowledge the Wallace Academic Editing for the English language editing.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cotofana S, Fratila AA, Schenck TL, et al. The anatomy of the aging face: a review. Facial Plast Surg. 2016;32(3):253–260. doi:10.1055/s-0036-1582234
2. Kim KH, Geronemus RG. Nonablative laser and light therapies for skin rejuvenation. Arch Facial Plast Surg. 2004;6(6):398–409. doi:10.1001/archfaci.6.6.398
3. Herne KB, Zachary CB. New facial rejuvenation techniques. Semin Cutan Med Surg. 2000;19(4):221–231. doi:10.1053/sder.2000.18362
4. Ko EJ, Hong JY, Kwon TR, et al. Efficacy and safety of non-invasive body tightening with high-intensity focused ultrasound (HIFU). Skin Res Technol. 2017;23(4):558–562. doi:10.1111/srt.12371
5. Pak CS, Lee YK, Jeong JH, et al. Safety and efficacy of ulthera in the rejuvenation of aging lower eyelids: a pivotal clinical trial. Aesthetic Plast Surg. 2014;38(5):861–868. doi:10.1007/s00266-014-0383-6
6. Suh DH, Oh YJ, Lee SJ, et al. A intense-focused ultrasound tightening for the treatment of infraorbital laxity. J Cosmet Laser Ther. 2012;14(6):290–295. doi:10.3109/14764172.2012.738912
7. Sasaki G, Tevez A. Microfocused ultrasound for nonablative skin and subdermal tightening to the periorbitum and body sites: preliminary report on eighty-two patients. J Cosmet Dermatol Sci Appl. 2012;2(2):108–116. doi:10.4236/jcdsa.2012.222022
8. Suh DH, Park HJ, Lee SJ, et al. Superficial intense focused ultrasound on periorbital wrinkle. J Cosmet Laser Ther. 2019;21(7–8):412–416. doi:10.1080/14764172.2019.1689272
9. Alster TS, Tanzi EL. Noninvasive lifting of arm, thigh, and knee skin with transcutaneous intense focused ultrasound. Dermatol Surg. 2012;38(5):754–759. doi:10.1111/j.1524-4725.2012.02338.x
10. Yalçınkaya E, Cingi C, Söken H, et al. Aesthetic analysis of the ideal eyebrow shape and position. Eur Arch Otorhinolaryngol. 2016;273(2):305–310. doi:10.1007/s00405-014-3356-0
11. Suh DH, Shin MK, Lee SJ, et al. Intense focused ultrasound tightening in Asian skin: clinical and pathologic results. Dermatol Surg. 2011;37(11):1595–1602. doi:10.1111/j.1524-4725.2011.02094.x
12. White WM, Makin IRS, Barthe PG, et al. Selective creation of thermal injury zones in the superficial musculoaponeurotic system using intense ultrasound therapy: a new target for noninvasive facial rejuvenation. Arch Facial Plast Surg. 2007;9(1):22–29. doi:10.1001/archfaci.9.1.22
13. Baumann L, Zelickson B. Evaluation of micro-focused ultrasound for lifting and tightening neck laxity. J Drugs Dermatol. 2016;15(5):607–614.
14. Ayatollahi A, Gholami J, Saberi M, et al. Systematic review and meta-analysis of safety and efficacy of high-intensity focused ultrasound (HIFU) for face and neck rejuvenation. Lasers Med Sci. 2020;35(5):1007–1024. doi:10.1007/s10103-020-02957-9
15. Hersant B, Abbou R, SidAhmed-Mezi M, et al. Assessment tools for facial rejuvenation treatment: a review. Aesthetic Plast Surg. 2016;40(4):556–565. doi:10.1007/s00266-016-0640-y
16. Lu PH, Yang CH, Chang YC. Quantitative analysis of face and neck skin tightening by microfocused ultrasound with visualization in Asians. Dermatol Surg. 2017;43(11):1332–1338. doi:10.1097/DSS.0000000000001181
17. Gliklich RE, White WM, Slayton MH, et al. Clinical pilot study of intense ultrasound therapy to deep dermal facial skin and subcutaneous tissues. Arch Facial Plast Surg. 2007;9(2):88–95. doi:10.1001/archfaci.9.2.88
18. Knize D. The Forehead and Temporal Fossa. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:45.
19. Alam M, White LE, Martin N, et al. Ultrasound tightening of facial and neck skin: a rater-blinded prospective cohort study. J Am Acad Dermatol. 2010;62(2):262–269. doi:10.1016/j.jaad.2009.06.039
20. Alghoul M, Codner MA. Retaining ligaments of the face: review of anatomy and clinical applications. Aesthet Surg J. 2013;33(6):769–782. doi:10.1177/1090820X13495405
21. Wan D, Amirlak B, Rohrich R, et al. The clinical importance of the fat compartments in midfacial aging. Plast Reconstr Surg Glob Open. 2014;1(9):e92. doi:10.1097/GOX.0000000000000035
22. Tsai LC, Lin ET, Chang CC, et al. Quantitative and objective measurements of facial aging process with anatomical landmarks. J Cosmet Dermatol. 2021. doi:10.1111/jocd.14221
23. Kwon HH, Yang SH, Choi M, et al. Tightening and reduction of unwanted submental fat using triple-layer high-intensity focused ultrasound: clinical and 3-dimensional imaging analysis. Dermatol Surg. 2021;47(12):1595–1600. doi:10.1097/DSS.0000000000003241
24. Jimenez F, Izeta A, Poblet E. Morphometric analysis of the human scalp hair follicle: practical implications for the hair transplant surgeon and hair regeneration studies. Dermatol surg. 2011;37(1):58–64. doi:10.1111/j.1524-4725.2010.01809.x
25. Vogt A, Hadam S, Heiderhoff M, et al. Morphometry of human terminal and vellus hair follicles. Exp Dermatol. 2007;16(11):946–950. doi:10.1111/j.1600-0625.2007.00602.x
26. Mavrevski R, Traykov ME, Trenchev IV, Trencheva MI. Approaches to modeling of biological experimental data with GraphPad Prism software. WSEAS Trans Syst Control. 2018;13:242–247.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.