Back to Journals » Clinical Ophthalmology » Volume 17
Quality of Vision in Eyes with Chronic Dacryocystitis After Endoscopic Dacryocystorhinostomy
Authors Meng Z , Chen R , Cao S, Yu X, Liu S, Hu Y, Li J, Chen M, Wang K, Liang X
Received 12 October 2023
Accepted for publication 21 November 2023
Published 6 December 2023 Volume 2023:17 Pages 3729—3737
DOI https://doi.org/10.2147/OPTH.S441094
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ziwei Meng,1,* Rongxin Chen,1,* Shujuan Cao,2,* Xinyue Yu,1 Shu Liu,3 Yu Hu,1 Jing Li,1 Meiqing Chen,1 Kerui Wang,1 Xuanwei Liang1
1State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Sun Yat-sen University, Guangzhou, 510060, People’s Republic of China; 2Ophthalmologic Center, The Affiliated Kashi Hospital of Sun Yat-sen University, The First People’s Hospital of Kashi Prefecture, Kashi, 844000, People’s Republic of China; 3Department of Pharmacy, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Sun Yat-sen University Cancer Center, Guangzhou, 510060, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xuanwei Liang; Rongxin Chen, State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Sun Yat-sen University, 54 South Xianlie Road, Guangzhou, 510060, People’s Republic of China, Email [email protected]; [email protected]
Purpose: To assess the quality of vision (QOV) of patients with chronic dacryocystitis and explore the impact of endoscopic dacryocystorhinostomy (En-DCR) on patients’ QOV, with the aim of increasing clinicians’ attention to the potential QOV changes in patients with chronic dacryocystitis.
Patients and Methods: Chronic dacryocystitis patients who attended the Department of Oculoplastics, Zhongshan Ophthalmic Center, Sun Yat-sen University from January 2022 to June 2022 and had En-DCR were included. The QOV was evaluated preoperatively and postoperatively using the Quick-contrast sensitivity function test (qCSF) and the OPD ScanIII comprehensive visual quality analyser, and the contrast sensitivity function (CSF), higher-order aberrations (HOAs), and modulation transfer function (MTF) data were recorded.
Results: Thirty-eight patients with chronic dacryocystitis were included. QOV analysis of those with monocular chronic dacryocystitis revealed that HOAs were significantly higher in affected eyes than in contralateral eyes (P < 0.05), and CSF and MTF were significantly lower in affected eyes than in contralateral eyes (P < 0.05). One month after En-DCR, patients’ HOAs, CSF, and MTF were significantly improved (P < 0.05), and there was no statistically significant difference in the effect of intraoperative combined silicone intubation versus no intubation on QOV (P > 0.05).
Conclusion: Chronic dacryocystitis can significantly affect the QOV of patients. Successful En-DCR significantly improves the CSF, HOAs and MTF, which can effectively improve the QOV.
Keywords: chronic dacryocystitis, contrast sensitivity function, higher-order aberrations, modulation transfer function, endoscopic dacryocystorhinostomy
Introduction
Quality of vision (QOV) is a concept at a higher level than visual acuity. It not only reflects the degree of resolution of the human eye to subtle targets, but also includes indicators such as contrast, comfort, and stability. With the development of the information age, people’s requirements for QOV have gradually increased, for example, the previous therapeutic cataract surgery has gradually grown into a refractive surgery that pursues QOV. High visual quality is of great significance for improving the quality of life.
Tear film plays an important role in maintaining QOV. Since the tear film is the first refractive surface of the eye, the optical quality of the eye is highly dependent on its homogeneity. When the tear quantity is significantly insufficient or excessive, the stability of the tear film may be reduced.1 As a representative disease of tear insufficiency, numerous studies have shown that dry eye can lead to a decrease in QOV, which is manifested as (1) decreased functional visual acuity;2 (2) reduced contrast sensitivity function (CSF);3 and (3) increased wavefront aberration.4 When lacrimal duct obstruction occurs, patients will present with excessive tear quantity, which is known as epiphora and, in turn, destroys the stability of the surface tear film while also possibly reducing the patient’s QOV.1 A study of patients with epiphora caused by unilateral lacrimal duct obstruction revealed that the CSF of the affected eye was significantly lower than that of the contralateral eye.5 Chronic dacryocystitis is one of the most common infections of the lacrimal duct and is associated with partial and total obstruction of the nasolacrimal duct. The most notable common signs and symptoms of chronic dacryocystitis are persistent epiphora and increased secretions. It is generally believed that chronic dacryocystitis is a nonblinding eye disease and does not cause a decrease in visual acuity. However, patients often complain of blurred vision associated with excessive tear quantity. The potential impact of the disease on the patient’s QOV has not received enough attention.
The results of previous studies have shown that lacrimal passage intubation plays a positive role in improving the QOV of patients with lacrimal duct obstruction.6,7 Endoscopic dacryocystorhinostomy (En-DCR) has been widely used in clinical practice and has become the main surgical method for the treatment of chronic dacryocystitis,8 but its effect on QOV of patients has not been quantified. It is of interest to have an in-depth understanding of the potential QOV changes in patients to supplement the traditional treatment strategy with appropriate ocular surface intervention to better improve the treatment effect of chronic dacryocystitis, thereby improving the quality of life. Thus, in this study, subjective and objective examinations were used to evaluate the QOV of patients with chronic dacryocystitis and the effect of En-DCR.
Materials and Methods
The study was designed as a prospective case series. The project conformed to the tenets of the Declaration of Helsinki, and ethical approval was obtained from the Institutional Review Board of Zhongshan Ophthalmic Center (2021KYPJ100). All patients voluntarily participated in the study and signed informed consent forms.
Study Population
Patients with chronic dacryocystitis who received primary En-DCR from January 2022 to June 2022 at Zhongshan Ophthalmic Center were considered for enrolment. The inclusion criteria were as follows: (1) age between 30 and 60 years old; (2) emmetropia (less than −0.50D to +1.00D) or low-to-moderate myopia (−0.50 to −6.00 D inclusive), with best-corrected distance visual acuity (BCVA) of 20/20 or better; and (3) clear clinical symptoms (including varying degrees of epiphora symptoms and eye secretions). The exclusion criteria were as follows: (1) chronic dacryocystitis caused by trauma, radiotherapy or chemotherapy, or congenital factors; (2) a history of other ocular diseases that seriously affect vision or any history of ocular surface surgery; and (3) patients with central cortical or nuclear cataract and intraocular lens eye.
Preoperative Examination
Routine medical history collection, standard ophthalmic examination (including BCVA, intraocular pressure, slit lamp examination, etc.) and irrigation of the lacrimal passage were performed in all patients.
Assessment of CSF
The Quick-contrast sensitivity function test (qCSF) was used to measure CSF. Developed by Lesmes et al9 this detection method combines the latest Bayesian adaptive algorithms and information theory tools to measure CSF quickly and accurately, stimuli were presented on a gamma-corrected 46-inch LCD monitor (NEC LCD P463). The examination was performed in a dark room with the patient sitting at a distance of 4 m from the monitor, and before the examination was started, the patient had five minutes for dark adaptation. Myopia patients wore eyeglasses to correct their visual acuity based on the optometry results, ensuring that all patients’ eyes were measured in their best corrected state, right eye first and then left eye. In each stimulus, the monitor presented three consecutive filtered digits of the same size but with decreasing contrast. The patient was asked to report verbally to the examiner the numbers presented on the monitor, and the examiner entered the reported answers with the computer keyboard, recording them as “correct” or “incorrect” or an “I don’t know” response. After all answers had been entered, this stimulus disappeared, and a new stimulus was started 500 ms later. At the end of the examination, the program automatically calculated the area under log contrast sensitivity function (AULCSF), and the AULCSF of both eyes of the patient was recorded separately for statistical analysis.
Assessment of HOAs and MTF
The OPD ScanIII comprehensive visual quality analyser (Nidek Co., Ltd., Gamagori, Japan) was used to assess the QOV, which includes automatic optometry, automatic keratometry, wavefront aberrometry, and Placido ring corneal topography. The environment for this instrument measurement also requires a dark room. The patient was instructed to keep both eyes flat, look at the measurement window, and try to open the eyes as wide as possible after one natural blink. In this study, measurements were performed in OPD/CT mode, and the examiner turned the lever clockwise or counterclockwise to obtain the best focal position for photo imaging by the screen instructions. After completing all measurements, the OK button was clicked, and the instrument automatically saved and analysed the data. The OPD Scan III comprehensive visual quality analyser could objectively and quantitatively display each order of aberration with the root mean square (RMS), measured in microns (um).
The following data were recorded by an OPD Scan III comprehensive visual quality analyser for analysis: (1) corneal higher-order aberrations (HOAs) at 4.0 mm pupil diameters (high RMS, coma RMS, trefoil RMS, and sph RMS) and (2) high-order modulation transfer function (HO MTF). Both eyes were measured three times, and the average was taken for statistical analysis.
Surgical Technique
All surgeries were performed by the same surgeon (XL). Operations were carried out under general anaesthesia with the patient in the supine position. Local submucosal injection with lidocaine and epinephrine hydrochloride over the preconceived rhinostomy site was followed by filling the nasal cavity with cotton pledgets infiltrated with the above mixture to provide sufficient topical vasoconstriction. Under endoscopic (Stryker Surgical, Kalamazoo, MI, USA) guidance, at the anterior edge of the middle turbinate axil, with the anterior edge of the uncinate process as the base and the attachment point of the inferior turbinate as the lower limit, the nasal mucoperiosteum was cut longitudinally and fully separated under the mucoperiosteum, and part of the mucoperiosteal flap was cut off to fully expose the lacrimal sac area and the lateral bone wall of the upper nasolacrimal duct. Bone-biting forceps were used, and a 12 mm×10 mm bony ostium was created. After the medial sac wall of the lacrimal sac was exposed, a Bowman probe was used to pass through the superior canaliculus into the lacrimal sac and tent up the medial sac wall of the lacrimal sac. The lacrimal sac wall was cut in full thickness to make the lacrimal sac flap, and 7–0 Vicryl sutures (Ethicon, USA) were used to suture the nasal mucoperiosteal flap and the lacrimal sac flap. Then, the anastomotic situation was used to decide whether to perform silicone intubation. A suitable expansive sponge was placed at the osteotomy site at the conclusion of surgery.
Postoperative Examination
All patients were reviewed at 1 month postoperatively, and success of En-DCR was defined as anatomical success and functional success.10 The BCVA, qCSF, and OPD Scan III comprehensive visual quality analysis examinations were required at the time of review, and the same QOV evaluation data as preoperative were recorded. For patients with silicone tubes placed during surgery, the tubes were removed after completing the above examinations one month after surgery as appropriate. All examinations were performed by the same skilled ophthalmologist, and the examination steps were completed strictly according to the preoperative requirements.
Statistical Analysis
The statistical analysis was performed using IBM SPSS software (Version 25.0; SPSS Inc., Chicago, IL, USA). Data are described as the mean ± standard deviation (mean ± SD) or quartile (P25, P75). Normally distributed data were compared using paired samples T-test and independent samples T-test, data that were not normally distributed were compared using paired samples Wilcoxon signed-rank test and independent samples Mann–Whitney U-test. All probabilities quoted were two-sided and considered statistically significant at P<0.05.
Results
A total of 38 patients with chronic dacryocystitis participated in this study, and the average age of the patients was 42.05±8.752 years, including 35 female patients and 3 male patients. The average duration of symptoms was 52.26±47.193 months, ranging from 2 to 156 months. There were 29 patients with monocular chronic dacryocystitis and 9 patients with bilateral disease. All patients underwent monocular surgery, of which 25 eyes were treated with En-DCR alone, and 13 eyes were treated with En-DCR combined with silicone intubation.
Preoperative Comparison of QOV Between Affected and Contralateral Eyes
By analysing the preoperative QOV data of 29 patients with monocular chronic dacryocystitis, it was found that the BCVA was comparable for both eyes (P > 0.05), while the AULCSF of the affected eye was significantly lower in the affected eye than in the contralateral eye. The high RMS, coma RMS, trefoil RMS, and Sph RMS of the affected eye were all higher than those of the contralateral eye, and the HO MTF of the affected eye was significantly lower than that of the contralateral eye (Table 1).
 |
Table 1 Preoperative Comparison of QOV Between Affected and Contralateral Eyes |
Effect of En-DCR on QOV
Comparison of QOV Before and After En-DCR
Anatomic success and functional success of En-DCR were achieved in all 38 patients at the one-month postoperative follow-up. There was no significant difference in BCVA in either eye compared to the preoperative BCVA (P > 0.05). The differences in HOAs were statistically significant in the operated eyes compared to preoperative (P < 0.05), and the postoperative AULCSF and HO MTF were significantly improved in the operated eyes compared to preoperative AULCSF and HO MTF (P < 0.001) as shown in Figure 1.
There were no significant differences in AULCSF, HOAs and HO MTF in nonoperated eyes compared with those before surgery (AULCSF t=−1.560, P=0.127; High RMS Z=−1.40, P=0.162; Coma RMS Z=−0.355, P=0.722; Trefoil RMS Z=−0.746, P=0.455; Sph RMS t=0.329, P=0.744; HO MTF Z=−1.305, P=0.192).
Postoperative Comparison of QOV Between Affected and Contralateral Eyes
There was no significant difference in AULCSF, HOAs and HO MTF between the affected eye and the contralateral eye in 26 patients with monocular chronic dacryocystitis after En-DCR (P > 0.05) as shown in Table 2.
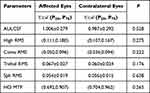 |
Table 2 Postoperative Comparison of QOV Between Affected and Contralateral Eyes |
Effect of Lacrimal Silicone Intubation on QOV
Patients were divided into with or without silicone intubation group according to whether combined with silicone intubation intraoperatively. Comparing the differences in AULCSF, HOAs and HO MTF changes between the two groups, we found no statistically significant differences between the groups with and without silicone intubation in terms of QOV changes (Table 3).
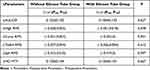 |
Table 3 Effect of Lacrimal Silicone Tube on QOV |
Discussion
In this study, the QOV of patients with chronic dacryocystitis was quantitatively evaluated from both subjective and objective perspectives. It was confirmed that chronic dacryocystitis can lead to a decrease in QOV and the utility of En-DCR in improving visual quality.
Since cataracts can affect the QOV, which can be manifested by reduced CSF and increased aberrations,11,12 the degree of lens opacity and vision loss in both eyes may vary. Therefore, the enrolment criteria of BCVA ≥ 1.0 were set in this study to more accurately evaluate the effect of chronic dacryocystitis on the QOV of patients.
The lacrimal drainage system is composed of lacrimal puncta, lacrimal canaliculus, lacrimal sac and nasolacrimal duct. This system maintains the proper distribution and drainage of tear components, safeguarding the health of the ocular surface and tear film, which is vital to the health of the ocular surface. When the nasolacrimal duct is narrowed or even blocked, the tear drainage ability is reduced, and the patient will exhibit epiphora. As two multifactorial diseases characterized by tear film instability, dry eye and epiphora can cause a variety of symptoms and even visual disturbances. However, for both diseases, patients can obtain better best-corrected visual acuity even if they have vision-related subjective symptoms, so it is difficult to detect changes in QOV using conventional visual acuity examinations.2 With the development of technology and equipment in ophthalmic clinical practice, different methods have been used in various studies to assess QOV in dry eye patients, including CSF measurement as well as quantitative optical sampling methods, such as measuring corneal topography data or wavefront aberration; the results have confirmed that the instability of the tear film in patients with dry eye has a direct visual impact and that this change in QOV is directly related to increased optical HOAs and increased light diffusion phenomena caused by tear film irregularities.3,4,13 Study results have also indicated that the QOV of dry eye patients will improve after treatment, and CSF and HOAs have shown varying degrees of improvement after artificial tear treatment.14,15 Therefore, for chronic dacryocystitis, which also causes decreased tear film stability, quantitative assessment of QOV is crucial for better understanding and treatment of the disease.
The CSF test is more sensitive than the conventional visual acuity test and can capture the QOV at medium and low spatial frequencies.16 It has been reported that activities related to quality of life, including reading speed,17 walking speed,18 and driving,19 are related to CSF. Therefore, the evaluation of CSF can help ophthalmologists better understand the symptoms and related QOV of patients with lacrimal duct obstruction diseases such as chronic dacryocystitis. The traditional method of measuring CSF is relatively time-consuming, and its low contrast level greatly limits the range and resolution of the test grating stimulation. In this study, a qCSF instrument was used to evaluate the CSF of patients; using the instrument enables more comprehensive evaluation of the changes in CSF under more contrast and spatial frequency combinations and shortens the time required for examination. It is often used to evaluate the visual training effect of amblyopia and the QOV of patients with age-related macular degeneration.20 It can also be used to screen the visual quality of patients without obvious visual impairment, such as the change in visual quality after refractive surgery.21 By comparing the binocular AULCSF of patients with monocular chronic dacryocystitis in this study, we found that the CSF of the affected eye was significantly lower than that of the contralateral side, which was consistent with the results of Tasaki et al5 on the CSF of patients with monocular lacrimal duct obstruction. This indicates that the blurred vision felt by patients with chronic dacryocystitis in the daily environment is likely to be the result of reduced CSF, which leads to a decrease in the ability of patients to distinguish subtle differences such as colour or shape.
The wavefront aberrations of dry eye patients who receive lacrimal punctum embolus implantation have been measured in previous studies, and the results indicated that corneal coma aberration increased after the implantation of lacrimal punctum embolus. This suggests that the function of the lacrimal duct system to drain tears is blocked, resulting in excessive retention of tears on the ocular surface and an asymmetric distribution of tear film thickness, which in turn causes the increase of corneal coma aberration.22 In this study, we detected that the HOAs of the cornea in patients with chronic dacryocystitis were significantly higher, which again verified that when the lacrimal drainage system was abnormal, excessive tear retention could lead to an increase in HOAs; the existence of aberrations could cause the light to deviate from the ideal optical path after passing through the human eye optical system, resulting in a decrease in QOV. In addition, since the OPD ScanIII comprehensive visual quality analyser can provide three-part aberration data of whole-eye HOAs, corneal HOAs, and intraocular HOAs, we also recorded the patient’s whole-eye HOA data in the early stage. Through analysis, it was found that the whole-eye HOAs exhibited the same change trend as the corneal HOAs, indicating that the increase in corneal HOAs caused by the irregular change in the corneal surface is the main source of aberration change in the whole eye. Therefore, the results of this study only show the change in corneal HOAs.
En-DCR has become a recognized surgical method for the treatment of chronic dacryocystitis. By creating a channel between the lacrimal sac and the nasal cavity, we allow the tears pass through the lacrimal sac to bypass the blocked nasolacrimal duct and directly flow into the nasal cavity, thereby improving the patient’s symptoms, such as epiphora and increased secretions. The results of this study demonstrate the effectiveness of successful En-DCR in improving QOV in patients with chronic dacryocystitis, and the QOV of affected eyes in monocular patients can be restored to the level of contralateral eyes after En-DCR, indicating that En-DCR can improve the ocular surface tear film irregularity caused by chronic dacryocystitis to a certain extent. Preoperative and postoperative QOV assessments can help ophthalmologists understand the recovery of visual quality in patients. For patients with QOV who do not notably improve, further ocular surface intervention can be considered. At present, there is controversy about whether the combination of silicone intubation is needed in En-DCR. In some studies, researchers have shown that there is no difference in the success rate of surgery between silicone intubation and nonintubation,10,23 while other scholars believe that silicone intubation can play a continuous and effective role in supporting the anastomosis, thereby improving the success rate of En-DCR. In the surgical treatment of this study, for patients with complicated conditions such as a small lacrimal sac or lacrimal sac mucosa with scar hyperplasia, silicone intubation was performed in combination with En-DCR. Previous studies have revealed that silicone intubation can markedly improve the CSF and HOAs of patients with lacrimal duct obstruction.6,7 In addition, silicone intubation is associated with complications such as irritation of the ocular surface, secondary infection, and ocular surface inflammation.24 Therefore, in this study, we compared the QOV improvement of patients who received or did not receive silicone intubation; we found no differences in CSF, HOAs and MTF between the two groups, which indicated that the impact of En-DCR on the visual quality of patients mainly depended on the opening of the anastomotic stoma.
This study had some limitations. The subjective feelings of patients with chronic dacryocystitis towards QOV and the severity of symptoms were not assessed. Subsequently, QOV-related questionnaires were considered to further assess this issue, such as the Lac-Q questionnaire and the NEI VFQ-25 questionnaire. Another limitation was the short follow-up time in this study. Long term postoperative assessment of QOV after En-DCR is needed in future studies.
Conclusion
Chronic dacryocystitis can affect the QOV of patients, and successful En-DCR significantly improves the CSF, HOAs and MTF, which can effectively improve the QOV. This study provides new insights for optimizing the diagnosis and treatment of chronic dacryocystitis, suggesting that ophthalmologists should pay more attention to the potential QOV changes in patients with chronic dacryocystitis.
Data Sharing Statement
The data used for the analysis are available from the corresponding author upon reasonable request.
Ethical Approval
The study followed the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University (Approved ID: 2021KYPJ100).
Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas, with Ziwei Meng, Rongxin Chen, Shujuan Cao and Xuanwei Liang served as the main leaders in the process of drafting, revising or critically reviewing the article. All named authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was partly supported by Zhongshan Ophthalmic Center Clinical Specialty Construction Project (No. 3030901010071), Natural Science Foundation of Guangdong Province (No. 2021A1515012043), Xinjiang Uygur Autonomous Region Innovation Environment (Talents, Bases) Special Project (Tianshan Youth Project) Funding Project (No. 2019Q145), and the Pearl River Scholar Tianshan Talent Cooperation’s Expert Studio Innovation Team (No. KDYY202018).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Koh S, Tung CI, Inoue Y, Jhanji V. Effects of tear film dynamics on quality of vision. Br J Ophthalmol. 2018;102(12):1615–1620. doi:10.1136/bjophthalmol-2018-312333
2. Goto E, Yagi Y, Matsumoto Y, Tsubota K. Impaired functional visual acuity of dry eye patients. Am J Ophthalmol. 2002;133(2):181–186. doi:10.1016/S0002-9394(01)01365-4
3. Ridder WH
4. Montés-Micó R, Cáliz A, Alió JL. Wavefront analysis of higher order aberrations in dry eye patients. J Refract Surg. 2004;20(3):243–247. doi:10.3928/1081-597X-20040501-08
5. Tasaki K, Hoshi S, Hiraoka T, Oshika T, Madigan M. Deterioration of contrast sensitivity in eyes with epiphora due to lacrimal passage obstruction. PLoS One. 2020;15(5):e0233295. doi:10.1371/journal.pone.0233295
6. Koh S, Inoue Y, Ochi S, Takai Y, Maeda N, Nishida K. Quality of vision in eyes with epiphora undergoing lacrimal passage intubation. Am J Ophthalmol. 2017;181:71–78. doi:10.1016/j.ajo.2017.06.022
7. Hoshi S, Tasaki K, Hiraoka T, Oshika T. Improvement in contrast sensitivity function after lacrimal passage intubation in eyes with epiphora. J Clin Med. 2020;9(9):2761. doi:10.3390/jcm9092761
8. Ali MJ, Psaltis AJ, Bassiouni A, Wormald PJ. Long-term outcomes in primary powered endoscopic dacryocystorhinostomy. Br J Ophthalmol. 2014;98(12):1678–1680. doi:10.1136/bjophthalmol-2014-305510
9. Lesmes LA, Lu ZL, Baek J, Albright TD. Bayesian adaptive estimation of the contrast sensitivity function: the quick CSF method. J Vis. 2010;10(3):
10. Chong KK, Lai FH, Ho M, Luk A, Wong BW, Young A. Randomized trial on silicone intubation in endoscopic mechanical dacryocystorhinostomy (SEND) for primary nasolacrimal duct obstruction. Ophthalmology. 2013;120(10):2139–2145. doi:10.1016/j.ophtha.2013.02.036
11. Shandiz JH, Derakhshan A, Daneshyar A, et al. Effect of cataract type and severity on visual acuity and contrast sensitivity. J Ophthalmic Vis Res. 2011;6(1):26–31.
12. Faria-Correia F, Lopes B, Monteiro T, Franqueira N, Ambrósio R Jr. Scheimpflug lens densitometry and ocular wavefront aberrations in patients with mild nuclear cataract. J Cataract Refract Surg. 2016;42(3):405–411. doi:10.1016/j.jcrs.2015.10.069
13. Koh S, Maeda N, Ikeda C, et al. The effect of ocular surface regularity on contrast sensitivity and straylight in dry eye. Invest Ophthalmol Vis Sci. 2017;58(5):2647–2651. doi:10.1167/iovs.17-21894
14. Zhang Y, Potvin R, Gong L. A study of the short-term effect of artificial tears on contrast sensitivity in patients with Sjögren’s syndrome. Invest Ophthalmol Vis Sci. 2013;54(13):7977–7982. doi:10.1167/iovs.13-11798
15. Huang FC, Tseng SH, Shih MH, Chen FK. Effect of artificial tears on corneal surface regularity, contrast sensitivity, and glare disability in dry eyes. Ophthalmology. 2002;109(10):1934–1940. doi:10.1016/S0161-6420(02)01136-3
16. Richman J, Spaeth GL, Wirostko B. Contrast sensitivity basics and a critique of currently available tests. J Cataract Refract Surg. 2013;39(7):1100–1106. doi:10.1016/j.jcrs.2013.05.001
17. Crossland MD, Culham LE, Rubin GS. Predicting reading fluency in patients with macular disease. Optom Vis Sci. 2005;82(1):11–17.
18. Donoghue OA, Ryan H, Duggan E, et al. Relationship between fear of falling and mobility varies with visual function among older adults. Geriatr Gerontol Int. 2014;14(4):827–836. doi:10.1111/ggi.12174
19. Ni W, Li X, Hou Z, Zhang H, Qiu W, Wang W. Impact of cataract surgery on vision-related life performances: the usefulness of real-life vision test for cataract surgery outcomes evaluation. Eye. 2015;29(12):1545–1554. doi:10.1038/eye.2015.147
20. Hou F, Huang CB, Lesmes L, et al. qCSF in clinical application: efficient characterization and classification of contrast sensitivity functions in amblyopia. Invest Ophthalmol Vis Sci. 2010;51(10):5365–5377. doi:10.1167/iovs.10-5468
21. Gao H, Miles TP, Troche R, Murdoch DM, Koefoed VF, Cason JB. Quality of vision following LASIK and PRK-MMC for treatment of myopia. Mil Med. 2022;187(9–10):e1051–e1058. doi:10.1093/milmed/usab071
22. Koh S, Maeda N. Wavefront sensing and the dynamics of tear film. Cornea. 2007;26(9 Suppl 1):S41–S45. doi:10.1097/ICO.0b013e31812f69e8
23. Smirnov G, Tuomilehto H, Teräsvirta M, Nuutinen J, Seppä J. Silicone tubing is not necessary after primary endoscopic dacryocystorhinostomy: a prospective randomized study. Am J Rhinol. 2008;22(2):214–217. doi:10.2500/ajr.2008.22.3132
24. Fayers T, Dolman PJO. Bicanalicular silicone stents in endonasal dacryocystorhinostomy: results of a randomized clinical trial. Ophthalmology. 2016;123(10):2255–2259. doi:10.1016/j.ophtha.2016.06.026
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

