Back to Journals » Risk Management and Healthcare Policy » Volume 14
Quality Assurance of Personal Radiation Shield for Kilovoltage Photon: A Multicentre Experience
Authors Bawazeer O
Received 28 December 2020
Accepted for publication 11 March 2021
Published 24 March 2021 Volume 2021:14 Pages 1263—1270
DOI https://doi.org/10.2147/RMHP.S298783
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Omemh Bawazeer
Medical Physics Department, Umm Al-Qura University, Mecca, Saudi Arabia
Correspondence: Omemh Bawazeer
Medical Physics Department, Umm Al-Qura University, Mecca, Saudi Arabia
Tel +966 563349226
Email [email protected]
Purpose: To optimize the maintenance of radiation shields, this study aims to analyze annual inspection files to assess the integrity of radiation shields and their associated factors with regard to defects in radiation shields in clinical settings.
Methods: A multicenter cross-sectional study was conducted at hospitals in Saudi Arabia. The data from annual inspection files of 1019 clinical lead radiation shields were analyzed. The factors of shield shape, unit where a shield is used, shield thickness, short-term use and number of users were examined. In addition to the inspection file analysis, radiation attenuation measurements were obtained for a subset of shields to compare newly purchased shields with older shields. Statistical analyses were performed using Fisher’s exact test and a t-test.
Results: The results show that the highest percentage of failing shields were found in the emergency unit, fluoroscopy unit and operation room with a failure of approximately 7.14%, 5.61%, and 3.98%, respectively, of these shields. Fluoroscopy and operation room units were statistically significantly associated with shield defects. There was no association between shield damage and shape of shield, shield thickness, short-term use or number of users. Radiation attenuation measurements were similar for new and older shields.
Conclusion: As fluoroscopy units and operating rooms have a higher percentage of damaged shields, it is recommended that the shields employed in these units should be regularly inspected more frequently than once a year. The study highlights that the shields’ age, transmission measurements that confirm that the correct shields are purchased according to the required kVp, physical appearance, and cleanliness should be recorded in annual inspection files. This study highlights the need for uniform inspection files of radiation shields across hospitals. National and international organizations may apply these findings to develop appropriate recommendations.
Keywords: radiation shield, lead shield, body apron
Introduction
Radiation shields have an important role in the safety of employees who operate radiation equipment and in preventing patients’ exposure to radiation. Lead shields are widely utilized in clinical practice to protect staff and patients from secondary radiation. Protective shields may have different shapes, including a one-piece full-body apron, a jacket, and a skirt. Typically, lead is embedded in rubber and fabric, or a mix of lead and rubber or lead and vinyl is used. Newer shields may also be lead free and made of a composite of lighter materials, such as bismuth or antimony, which may function as an equivalent to lead. Lead shields should include a protective layer with a minimum thickness of 0.25 mm of lead for X-rays up to 100 kV and a minimum thickness of 0.35 mm lead for X-rays greater than 100 kV.1
These shields are employed in different units in hospitals, including diagnostics, operating rooms, nuclear medicine, and dental clinics. In clinical practice, shields are subject to damage, which may include cracks, holes, or tears. Damage can also occur when shields are not properly handled or stored.2 Therefore, during clinical use, protective shields should be examined to check their integrity. There is no standard protocol for shield inspection, although some manufacturers may make recommendations. Shields should also be examined if a safety issue is suspected or if the shield is present on the ground. In many hospitals, shields are inspected once a year.2–4 Inspections may be conducted visually or via palpation, but neither of these methods can detect internal damage. It was reported that 54.50% of damaged radiation shields (as determined via imaging) passed a visual inspection.5 In another study, visual inspections and physical palpation indicated no damage in 77.78% of aprons that were shown to be damaged via imaging.7 Imaging inspection may use a computed tomography (CT) scan,5,6 fluoroscopy6,8 or a general X-ray.9
Existing research on radiation shields examines the transmission measurements of clinical shields,7,10 clinical practice using lead-free materials,11,12 and the development of nano shields.13–15 Few studies with a limited number of samples have reported the integrity of radiation shields. A study at the University of Basel emphasizes the requirement of quality checks of X-ray protection clothing.6 Of 85 lead aprons that were examined, 58 were found to be defective, due to either damage such as cracks or to radiation permeability.9 A new practical method was suggested to assess the integrity of shields by determining the maximum tear length.16 However, research on the effect of shield shape, thickness, and unit, number of users, and duration of use on shield defects is lacking. Therefore, to optimize the integrity of clinical radiation shields, this study analyzed the data from annual inspections of clinical radiation shields to investigate the impact of these factors on the integrity of radiation shields.
Method
This paper presents a multicenter cross-sectional study that was conducted in Saudi Arabia. Ethical approval was obtained from ethical committee, Approval number (HAPO-02-K-012-2020-09-444). We analyzed inspection data for 1019 radiation shields that are actively used in four hospitals. The annual inspection data for the radiation shields were compiled and statistically analyzed. To maintain anonymity, the hospitals are referred to as hospitals 1, 2, 3, and 4. All the radiation shields investigated in this study use shield-based lead for radiation protection.
Radiation shields are inspected by an institution’s radiation safety office or by a hospital’s medical physics. Regarding clinical protocol, the integrity of the internal structure of shields is inspected regularly (once a year) using fluoroscopy imaging. Each shield was identified by serial number, shape, unit where it was collected, and inspection results, which consisted of pass (no damage to shield) or fail (shield is damaged). The criteria for acceptance of the pass or rejection of a shield is demonstrated in a study conducted by Lambert and McKeon,3 and certain clinical protocols and manufacture protocols followed this criterion. They assessed the rejection criteria based on the radiation dose received by a worker from a defect and the cost of replacing a lead protective shield. Aprons will be rejected (fail) and replaced if the sum of the areas of defects exceeds 15 mm2 unless the defect is not located over a critical organ. Lesser rejection criteria will be applied if defects are detected on the back of the lead apron, along the seam and overlapped areas; these areas will be rejected if the area defect exceeds 670 mm2. If the defect is located over the testes and thyroid, the shields should be rejected and replaced when the sum of the areas of defects exceeds 11 mm2.
The data from annual inspection files were collected from all four hospitals. We reorganized the data files for compatibility with a statistical program. The radiation shields were classified by shape, unit, thickness, short-term use (two years), and number of users. For the thickness of shields, only one hospital reported the thickness, so the number of shields in regard to thickness was classified for 147 shields. In addition, for short-term usage (two years), data were collected from two hospitals. The number of users was estimated from the number of staffs in the radiology departments. Two hospitals were classified as having a large number of users, and another two hospitals were classified as smaller number of users.
In addition to the data collected from annual inspection files, radiation attenuation measurements were conducted on a subset of shields (forty shields). These shields are classified as new punches shield and old shield. Although there is no specific age registered in the inspection files, the older shields were confirmed by the radiation safety office and estimated to have an age range of approximately 3 to 6 years. The X-ray attenuation measurements were carried out by separately positioning each shield at 60 cm from the focal spot and ionization chamber with 0.2 cm2 for soft X-ray (PIW, Germany). X-ray attenuation measurements were performed using a tube voltage of 70 kV. A tube current-time product of 10 mAs was applied. Measurements were conducted with and without an apron present in the radiation field.
Attenuation was calculated with the following equation:
Statistical analyses were performed using the social sciences software (SPSS version 16.0, Chicago, Illinois, USA). Fisher’s exact test was conducted to test the independence of each group. These comparisons identify whether any group is a differential factor. A 95% confidence interval, that is, a p-value less than 0.05, was considered statistically significant. P-values greater than 0.05 indicate insignificant differences, implying that the tested grouping is not an influential factor. For comparison, the attenuation measurements t-test was applied, and statistical significance was set at a P value of less than 0.05.
Results
A total of 1019 radiation shields were examined in this study. Figure 1 represents the percentage of passing and failure rate of the annual inspections for clinical shields by unit where the shields are utilized. Radiation shields are used in 13 units in the included hospitals. Of these shields, 98.46% passed the annual inspection (no damage), while 2.11% failed the inspection (damage detected). The highest percentage of failing shields was employed in the emergency unit; approximately 7.14% of these shields were damaged. The next highest rate of damage occurred in the fluoroscopy unit, where 5.61% or six of 101 shields were damaged, followed by the operating theater, where 3.98% or ten of 241 shields were damaged. General X-rays had a low failure rate of 2.35%; the dental unit had a failure rate of only 0.95%. The remaining units (breast biopsy, pain clinic, catheterization laboratory (cath lab), intensive care unit (ICU), endoscopy, nuclear medicine, lithotripsy, and CT) had no failing shields.
 |
Figure 1 Percentages (%) of the annual inspection test for clinical shields in each department. |
To investigate the impact of individual units on shield damage, Fisher’s exact test was performed to obtain a comparison between the number of shields that pass or fail in each department and the sum of the shields in the other departments (Figure 2). The operating room had the highest use of radiation shields: 251 shields. For the remaining units, 233 shields were used in the cath lab, 178 shields were utilized in general X-rays, 107 shields in fluoroscopy, and 105 in dental clinics. The most significant unit association with shield defects is fluoroscopy, with a p-value of 0.01. The operating room also significantly impacted shield damage, with a p-value of 0.02. The p-value for the relationships of all other units with shield damage was greater than 0.05.
 |
Figure 2 Number of shields in each department compared to the total number of shields in the other departments, and Fisher’s exact test results. |
The data by shield shape are shown in Figure 3. This study includes eleven different shapes for radiation shields; failing shields were most common among thyroid and body apron shields. These shapes failed at comparable rates: 2.79% and 2.47% for thyroid shields and body apron shields, respectively. No damage was detected for other shapes. The most common shape in hospitals is a body apron (486 shields). The next most common shape was thyroid protection (358 shields). Lead gloves, body aprons with collars, and shield skirts were less common. The results of Fisher’s exact test indicated no relationship between damage and shield shape, as the p-value was greater than 0.05 for all shapes (Figure 4).
 |
Figure 3 Percentages (%) of the annual inspection test classified based on shield shape. |
 |
Figure 4 Number of shields for each shape compared to the total number of the shields for other shapes, and Fisher’s exact test results. |
The shields were also categorized based on the lead thicknesses of 147 shields, as shown in Figure 5. No failing rate was reported for a lead thickness of 0.35 and 0.3 mm. No significant relationship was found between lead thickness and shield damage. Fisher’s exact test yielded P-values greater than 0.05 for lead thicknesses of 0.5 mm, 0.35 mm, and 0.3 mm.
 |
Figure 5 Number of shields for each thickness compared to the total number of the shields for other thickness, and Fisher’s exact test results. |
The relationship between shield damage and short-term use is demonstrated in Figure 6, which shows the results of the annual shield inspections at hospitals 1 and 2 over two years. For the two years, there is no significant difference among the inspection results of each year (p-value > 0.05) in hospital 1. However, during the following two years in hospital 2, the difference became significant. In 2019, no shield damage was reported.
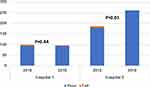 |
Figure 6 Relationship between shield damage and short-term use, and Fisher’s exact test results. |
The relationship between shield damage and number of users is represented in Figure 7. The results of Fisher’s exact test revealed that there is no relation between shield damage and number of users.
 |
Figure 7 Comparison between number of users and damage, and Fisher’s exact test results. |
The comparison attenuation measurements between newly purchased shields and older shields for the subset of data are shown in Figure 8. The results of the t test show that the mean of radiation attenuation is approximately 97.1% and that there is no significant difference in attenuation ability between new shields and older shields.
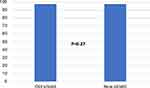 |
Figure 8 Radiation attenuation measurements by new and older shields, and t test results. |
Discussion
To the best of our knowledge, this paper is the first assessment of annual inspection files of clinical shields with 11 shield shapes, 13 units of use, 3 shield thicknesses, short-term shield duration of use, and number of users. The results of this investigation of the integrity of a shield as well as the information in current clinical inspection files can be used to improve radiation protection for both staff and patients and optimize radiation protection in radiology departments. The results will also improve cost-effectiveness since radiation shields are expensive, and excellent maintenance will increase the lifespan of clinical shields, thereby reducing the budget for replacing damaged shields.
First, the analysis of inspection files from different hospitals revealed the need for uniform inspection files of radiation shields across hospitals. National and international organizations may use these findings to develop appropriate recommendations for quality assurance tests. Second, of the clinical units investigated here, fluoroscopy and operating rooms are significantly more likely to have defective shields (p-value < 5) due to radiation damage. These findings have clinical relevance as it is possible that staff and patients might use shields with internal structural damage if inspections are conducted only once a year. This limitation cloud be increasing the risk of radiation exposure for patients and staff. Fluoroscopy in particular is considered a high-dose source of radiation.17 Therefore, shields used in fluoroscopy and operating rooms should undergo specific quality checks more frequently than once a year. Perhaps staff working in these units should undergo training on proper shield maintenance, use, hinge, and storage. In addition, if damage occurs during the year, the additional personal staff dose could be evaluated and added to the annual dose received. Stam et al16 proposed an equation to calculate the additional dose to give to staff if holes were detected in a shield. The additional dose is a function for many factors, such as radiation energy, size and location of tears or holes in a shield, and thickness of a shield (single or double layers).
This study also demonstrated that body aprons and thyroid shields were more likely than other shapes to be damaged (Figures 3 and 4), but this difference was not statistically significant. For the thickness of a shield, it was also expected that thinner shields might be more likely to undergo damage due to folding or bending. However, the results indicated that all thicknesses of lead shields (0.5 mm, 0.35 mm, and 0.3 mm) were damaged at similar rates. At the international level, the results for shape and thickness of a shield could be adapted since the examined shields are purchased from different international companies. In regard to the thickness of a radiation shield, previous studies have recommended that the radiation transmission of new radiation shields under different levels of kV should be measured prior to use. Manufacturer labels usually report measurement using one beam quality with a narrow beam setup.7,8 In response to this finding and based on our analyses of annual inspection files, we recommend adding transmission measurements based on shield thickness to the diagnostic clinical ranges for new shields. These transmission measurement data can be used to confirm that the right shields are purchased according to the required kVp.
We also examined the relationship between short-term shield use and the integrity of a shield. Figure 6 shows the results of annual inspections for short-term usage at two hospitals. At hospital 1, there was no significant difference in the percentage of damaged shields over two consecutive years (p-value > 0.05). However, at hospital 2, shield duration of use had a significant association with shield damage when two consecutive years were compared. In 2018, 3.76% of shields were damaged. However, no shields were damaged in 2019. A radiation officer at that hospital explained that this difference may have occurred because a large number of shields were replaced in 2018. It should be noted, however, that this study has only a limited ability to accurately assess the relationship between shield integrity and duration of use because no information about shield age was included in the annual inspection files. On the topic of shield age, two points emerge from this study. First, shield age should be included in the annual inspection files to help illuminate any existing relationship between integrity and shield age. This inclusion would also help management determine when to purchase new radiation shields and select a company that manufactures a shield with a long life. For the number of users, the results show that there is no significant difference between shield damage and number of users.
The annual inspection files analyzed in this study include neither any criteria for regularly cleaning the surface of shields nor any descriptions of the physical appearance of shields. However, a recent study reported that 63% of radiation shields have dust on exterior surfaces, which correlates with the physical appearance of a shield.18 This dust may be a hazard as lead-based dust is a well-known source of lead exposure. Lead dust can be absorbed by the blood either by inhalation or inadvertent ingestion, causing elevated levels of lead in the blood. More recently, bacterial contamination on protective shields was reported.19,20 We therefore recommend, in accordance with recent international highlights, that a description of the physical appearance of shields and surface cleaning procedures should be included in the annual inspection files.
Conclusion
This study has analyzed the annual inspection files for 1019 radiation shields that are currently in use in four hospitals. The study has demonstrated that the fluoroscopy and operating units are more likely to have defective shields than other hospital units. In response to this finding, we have recommended that radiation shields used in fluoroscopy and operating rooms should be inspected for damage more frequently than once a year. We found no association between shield integrity and shape of shield, shield thickness, short-term use, or number of users. This study has also identified some limitations in annual inspection data, which should (in addition to existing data) include descriptions of inspected shields’ physical appearance, age, cleanliness, and transmission measurements for new shields to assure that an appropriate shield will be used for a specific kV value. This study highlights the need for uniform inspection files of radiation shields across hospitals. National and international organizations may use these findings to improve the quality assurance of personnel protective radiation shielding.
Ethics Approval
This study was approved by the biomedical Ethics Committee in Umm Al-Qura University (approval number: HAPO-02-K-012-2020-09-444).
Disclosure
The author declares that they have no conflicts of interest for this work.
References
1. Institute of Physics and Engineering in Medicine. Medical and Dental Guidance Notes: A Good Practice Guide on All Aspects of Ionising Radiation Protection in the Clinical Environment. York: Institute of Physics and Engineering in Medicine; 2002.
2. Michel R, Zorn MJ. Implementation of an X-ray radiation protective equipment inspection program. Health Phys. 2002;82(2 Suppl):S51–S53. doi:10.1097/00004032-200202001-00012
3. Lambert K, McKeon T. Inspection of lead aprons: criteria for rejection. Health Phys. 2001;80:S67–S69. doi:10.1097/00004032-200105001-00008
4. Australian/New Zealand Standard™. Occupational Protective Gloves. Part 1: Selection, Use and Maintenance. 2000. AS/NZS 2161.1.
5. Matsuda M, Suzuki T. Evaluation of lead aprons and their maintenance and management at our hospital. J Anesth. 2016;30(3):518–521. doi:10.1007/s00540-016-2140-2
6. Oppliger-Schäfer D, Roser HW. Quality assurance of X-ray protection clothing at the university hospital basel. In:
7. Uche CH, Chimuanya UD, Okeji MC, Onwugalu E. How efficient are the lead aprons used for radiation protection in our hospitals. Indian j Appl Res. 2018;8(2).
8. Livingstone RS, Varghese A. A simple quality control tool for assessing integrity of lead equivalent aprons. Indian J Radiol Imaging. 2018;28(2):258. doi:10.4103/ijri.IJRI_374_17
9. Oyar O, Kislalioglu A. How protective are the lead aprons we use against ionizing radiation? Diagn Intervent Radiol. 2012;18(2):147.
10. Murphy PH, Wu Y, Glaze SA. Attenuation properties of lead composite aprons. Radiology. 1993;186(1):269–272. doi:10.1148/radiology.186.1.8416577
11. Papadopoulos N, Papaefstathiou C, Kaplanis PA, et al.. Comparison of lead-free and conventional x-ray aprons for diagnostic radiology. In:
12. McCaffrey JP, Shen H, Downton B, Mainegra‐Hing E. Radiation attenuation by lead and nonlead materials used in radiation shielding garments. Med Phys. 2007;34(2):530–537. doi:10.1118/1.2426404
13. Aghaz A, Faghihi R, Mortazavi S, Haghparast A, Mehdizadeh S, Sina S. Radiation attenuation properties of shields containing micro and Nano WO3 in diagnostic X-ray energy range. Int J Radiat Res. 2016;14(2):127. doi:10.18869/acadpub.ijrr.14.2.127
14. Botelho MZ, Künzel R, Okuno E, Levenhagen RS, Basegio T, Bergmann CP. X-ray transmission through nanostructured and microstructured CuO materials. Appl Radiat Isot. 2011;69(2):527–530. doi:10.1016/j.apradiso.2010.11.002
15. Cho JH, Kim MS, Rhim JD. Comparison of radiation shielding ratios of nano-sized bismuth trioxide and molybdenum. Radiat Effe Defects Solids. 2015;170(7–8):651–658. doi:10.1080/10420150.2015.1080703
16. Stam W, Pillay M. Inspection of lead aprons: a practical rejection model. Health Phys. 2008;95(2):S133–S136. doi:10.1097/01.HP.0000314763.19226.86
17. Stahl CM, Meisinger QC, Andre MP, Kinney TB, Newton IG. Radiation risk to the fluoroscopy operator and staff. Am J Roentgenol. 2016;207(4):737–744. doi:10.2214/AJR.16.16555
18. Burns KM, Shoag JM, Kahlon SS, et al. Lead aprons are a lead exposure hazard. J Am Coll Radiol. 2017;14(5):641–647. doi:10.1016/j.jacr.2016.10.024
19. Ang L, Almasoud A, Palakodeti S, Mahmud E. Bacterial contamination of lead aprons in a high-volume cardiac catheterization laboratory and disinfection using an automated ultraviolet-c radiation system. J Invasive Cardiol. 2018;30:416–420.
20. McAleese T, Broderick JM, Stanley E, Curran R. Thyroid radiation shields: a potential source of intraoperative infection. J Orthopaedics. 2020;22:300–303. doi:10.1016/j.jor.2020.06.010
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.